Summary
Background
While vaccination plays a critical role in the global response to the COVID-19 pandemic, vaccine rollout remains suboptimal in Nigeria and other Low- and Middle-income countries (LMICs). This study documents the level of hesitancy among health workers (HWs) during the initial COVID-19 vaccine deployment phase in Nigeria and assesses the magnitude and determinants of hesitancy across Nigeria.
Methods
A cross sectional study across all States in Nigeria was conducted with over 10,000 HWs interviewed between March and April 2021. Data were cleaned and analyzed with proportions and confidence intervals of hesitancy documented and stratification by HW category. We compared the level of confidence/acceptance to be vaccinated across Nigeria and documented the sources of negative information amongst HWs who refused the vaccine.
Findings
Among the 10 184 HWs interviewed, 9 369 [92% (95% CI= 91, 92)] were confident of the COVID-19 vaccines and were already vaccinated at the time of this survey. Compared to HWs who were less than 20 years old, those aged 50 – 59 years were significantly more confident of the COVID-19 vaccines and had been vaccinated (OR=3.8, 95% CI=2.3 – 6.4, p<0.001). Only 858 (8%) of the HWs interviewed reported being hesitant with 57% (479/858) having received negative information, with the commonest source of information from social media (43.4%.)
Interpretation
A vast majority of HWs who were offered COVID-19 vaccines as part of the first phase of national vaccine roll out were vaccinated and reported being confident of the COVID-19 vaccines. The reported hesitancy was due mainly to safety issues, and negative information about vaccines from social media. The issues identified remain a significant risk to the success of subsequent phases of the vaccine rollout in Nigeria.
Funding
None.
Keywords: COVID-19 vaccine, Vaccine hesitancy, Health workers, Nigeria
Research in context.
Evidence before this study
Vaccine hesitancy has a huge effect on health decisions by the wider populations. The term hesitancy is a spectrum between accepting and refusing all vaccines offered to individuals. Prior to the COVID-19 vaccine rollout in Africa, over 50% of the population have been reported by some studies to be hesitant about receiving the COVID-19 vaccines. However, the actual decisions before vaccines were deployed and after vaccine deployment may not be similar, hence the need to document real life decisions made following vaccine deployment.
Added value of this study
To the best of our knowledge, this is the first study performed after COVID-19 vaccines became available in Nigeria focusing on health workers (HWs) in Nigeria following the rollout of the COVID-19 vaccines, with over ten thousand respondents. Our study shows that over 90% of HWs who were offered the COVID-19 vaccines were confident about the vaccines and were already vaccinated at the time of this survey. Previous COVID-19 infection were strong determinants of vaccine acceptance. We also show that HWs >50 years old were more likely or willing to be vaccinated compared to HWs in their early 20’s. We have shown that issues around perceived COVID-19 vaccine safety are the main reasons for refusals, with the main source of negative information being social media.
Implications of all the available evidence
A very high proportion of the surveyed HWs were willing to, and already vaccinated during the phase 1 of the COVID-19 vaccination rollout in Nigeria. The national vaccine deployments must focus more on engaging with younger HWs and manage disinformation through social media to improve vaccination uptake.
Alt-text: Unlabelled box
Introduction
By early January 2021, the World Health Organization (WHO) had reported over 83 million cases of SARS-CoV-2 infection globally with 1.9 million of these in the African region.1 Majority of the cases in Africa were reported in South Africa, Algeria, Ethiopia, Nigeria, and Kenya. As of 13th May 2021, the Nigeria center for Disease Control (NCDC) – the country's public health institute had reported 161,515 confirmed COVID-19 cases and 2,065 deaths across the 36 States and the Federal Capital Territory(FCT) of Nigeria.2 Even as countries continue to implement various strategies to mitigate the impact of the pandemic on lives and livelihoods, vaccination is seen as a critical tool to accelerate this process.3
As part of the response to the COVID-19 pandemic, the COVID-19 Vaccines Global Access Facility(COVAX) shipped an initial 3.94 million doses of the AstraZeneca/Oxford vaccine to Nigeria on March 2, 2021, to commence COVID-19 vaccination in Nigeria and help contain the spread of the virus. As part of the roll-out of COVID-19 vaccination, Nigeria developed a four-phased National Deployment and Vaccination Plan (NDVP). This four-phase plan included an initial prioritization of Healthcare Workers (HWs) and other priority frontline workers, targeting about 2 million persons to be offered the first dose of the Oxford/AstraZeneca vaccines across all States and the Federal Capital Territory of Nigeria.4 The National Primary Health Care Development Agency (NPHCDA) trained healthcare workers and vaccination teams who were deployed to all districts within days of the formal launch of the vaccination campaign on the 5th of March 2021. Only the Oxford/Astra Zeneca (Serum Institute India) COVID-19 vaccine was deployed as part of the Phase 1 of the national vaccine deployment plan.
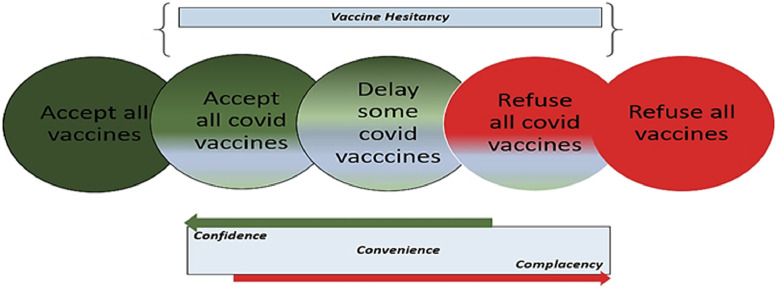
Vaccine hesitancy is a broad term describing a spectrum between acceptance of all vaccine types offered to persons and the rejection of all vaccines. This spectrum may include accepting all covid vaccines, delaying some covid vaccines and refusing all covid vaccines. Vaccine hesitancy in general and in this context is seen to be determined by confidence, convenience, and complacency5 (Figure 1). Vaccine hesitancy amongst HWs has been highlighted as a challenge to achieving global immunization targets.6 HWs remain a trusted and reliable source of information about the impact of vaccines on disease control and prevention. There is well documented evidence suggesting that the general population rely on HWs’ opinions and considers them important in making the decision to be vaccinated.7 The acceptance or rejection of COVID-19 vaccines among HWs can, thus, influence the acceptability of COVID-19 vaccines at the community level.8
Figure 1.
Schema showing continuum of vaccine hesitancy and vaccine hesitancy determinants. *Report of the SAGE working group on vaccine hesitancy Nov 12, 2014.
In Africa, pre-vaccine deployment surveys conducted across several countries found that more than 50 per cent of the general population were hesitant about receiving the COVID-19 vaccines if and when they are available.9, 10, 11 Other surveys exploring the intention to receive the COVID-19 vaccines also showed varying degrees of hesitancy across multiple social and demographic groups.12, 13, 14 A survey conducted to explore the intention to accept COVID-19 among doctors in Nigeria reported that only about 38 per cent of respondents were willing to accept the COVID-19 vaccination.15 To end the current pandemic, it is imperative that the factors driving COVID-19 vaccine hesitancy, especially among healthcare workers be explored after the actual vaccine deployment has commenced.
The currently available literature on COVID-19 vaccine hesitancy is based on studies reporting on the intention to accept vaccines if, and when they are deployed. The authors are not aware of any study reporting the ‘actual’ vaccine hesitancy or acceptance of subsequent doses after the deployment of COVID-19 vaccines in Nigeria. Generating contextual evidence around COVID-19 vaccine hesitancy, especially in LMIC is key to addressing future concerns around acceptance of the multiple new vaccines that would be deployed as part of the pandemic response. To bridge this gap, we assessed COVID-19 vaccine hesitancy and its determinants among healthcare workers during the phase 1 deployment of vaccines received through the COVAX facility in Nigeria as part of the National deployment and vaccination plan (NDVP). We hope that our study can provide evidence to guide policy decisions and improve strategy for subsequent phases of vaccine deployment in Nigeria and other countries in Africa.
Methods
Study design and study population
We conducted a cross-sectional national survey of healthcare workers in health facilities across all six geopolitical zones of Nigeria between March and April 2021. Nigeria, which is situated in west Africa, is the most populous country in Africa, and the sixth most populous country in the world with an estimated population of 211 million as of 2021.16 For ease of economic and political administration, Nigeria is divided into six geopolitical zones which comprise 36 states and the federal capital territory (FCT) as follows: North Central (Benue, FCT, Kogi, Kwara, Nasarawa, Niger, and Plateau States); North East (Adamawa, Bauchi, Borno, Gombe, Taraba, and Yobe States); North West (Jigawa, Kaduna, Kano, Katsina, Kebbi, Sokoto, and Zamfara States); South East (Abia, Anambra, Ebonyi, Enugu, and Imo States); South-South (Akwa Ibom, Bayelsa, Cross River, Delta, Edo, and Rivers States); South West (Ekiti, Lagos, Ogun, Ondo, Osun, and Oyo States). Nigeria's healthcare system consists of a network of primary, secondary, and tertiary facilities distributed across the 36 states and the FCT.
To ensure an efficient delivery of the vaccines, the National Primary Health Care Development Agency (NPHCDA) of Nigeria developed a phased NDVP with the first phase targeting frontline healthcare workers scheduled to commence in March 2021. The health workforce in Nigeria comprises a diverse group ranging from medical doctors, nurses, pharmacists, and laboratory scientists who provide care mainly at the tertiary and secondary levels, to the Community Health Workers who provide care at the primary and community levels. As of 2019, Nigeria had a health worker-to-population ratio of about 3.8 medical doctors per 10 000 population, 15 nursing and midwifery personnel per 10 000 population, and 116 454 Community Health Workers.17
Dataset
The dataset for this study was collected as part of a national survey using a purposive sampling method with the aim of gaining feedback from frontline HW who implemented the phase 1 of the vaccine deployment and had been offered the COVID-19 vaccine at facilities or temporary posts where the vaccine was being offered across Nigeria. As part of the routine and standard procedure to evaluate the introduction of new vaccines by the NPHCDA, this survey was conducted between weeks 4-7 of the commencement of phase 1 of the COVID-19 vaccination in Nigeria. As such, the National Health Research Ethics Committee (NHREC) of Nigeria considered the study exempt from formal ethics committee approval. Nevertheless, informed consent was sought from survey respondents, and confidentiality was maintained.
Study tools and procedures
The draft questionnaire was designed in English by the authors with inputs from the immunization and data management team of the NPHCDA with support from WHO to ensure clarity and to refine the questions and options for responses. The final survey was conducted by State Technical Assistants (STAs) deployed through the WHO Nigeria incident management system (IMS) support for COVID-19 vaccination through a computer-assisted personal interviewing technique. The in-person interviews were documented using the Open Data Kit (ODK) platform on encrypted handheld devices. The survey questionnaires (appendix 1) were pre-loaded on the handheld devices used by the interviewers. As part of the data quality enhancement process for the surveys, the data collection tool included validity constraints to ensure allowable answers for each question using skip logics during the interviews. Each interviewer conducted at least one interview per day and each interview was uploaded by the technical assistants in real-time after completion. The interviews were administered in English. An ICT team was on standby to provide remote technical support for field staff who encountered challenges with data collection or submission.
Each interview was completed after documentation of answers to the 22 questions on the questionnaire over a minimum duration of 15 minutes. The first ten questions captured the respondents’ State and Local Government Area of location, demographic data, profession, and type of health facility where they worked. Questions 11 to 16 asked if they had previously tested positive for COVID-19, if they had received the COVID-19 vaccine, and their knowledge of the currently available COVID-19 vaccines, and their willingness to offer the vaccine to their family and friends or to receive it if they were yet to. Questions 17 to 22 explored the reasons for refusal of the vaccine amongst those who were yet to receive the COVID-19 vaccine, and the sources and kinds of information which they had received which influenced their decision about the COVID-19 vaccine. For the purposes of this work,
Definition of COVID-19 vaccine confidence or hesitancy
For the purposes of this analysis, respondents were defined as COVID-19 vaccine-hesitant if they had delayed in accepting or had refused the COVID-19 vaccine despite its daily availability (for more than four weeks) at the designated vaccination posts or health facility where they worked. On the other hand, respondents were considered as COVID-19 vaccine confident if they had already received the COVID-19 vaccine which was offered them on or before the day of the survey.
Data analysis
The dataset was downloaded as an Excel® based spreadsheet, reviewed and cleaned to ensure the completeness and correctness of all required variables. We analyzed the data using descriptive statistics to assess level of vaccine hesitancy amongst healthcare workers in Nigeria at national, regional and State levels.
We calculated the proportion of respondents from each State (the equivalent of regions in some climes) who were not hesitant by dividing the number of respondents from each State who were not hesitant by the total number of respondents from each state. We weighted this analysis by the corresponding population of the 36 States and the Federal Capital Territory of Nigeria using programme data based on the country's 2021 COVID-19 National Deployment and Vaccine Plan. We calculated 95% confidence intervals around these estimates and used these to construct a thematic map of the vaccine confidence amongst the survey respondents in each State in Nigeria. We illustrated the point estimates and 95% CI of the proportion of non-hesitant subjects in each State from the least to the greatest in an ascending order in a forest plot, comparing them to the national estimate. We used binary logistic regression modelling to determine the predictors of hesitancy.
We calculated the proportion of respondents’ reasons for hesitancy, and sources of information regarding COVID-19 vaccination, and used these estimates to construct a bar chart and Tree map respectively. We defined negative information as any pieces of information which the respondents received from any source that might have influenced their decision to delay or refuse being vaccinated. Data analysis was performed using Microsoft Excel (Microsoft, Seattle, WA, USA), and STATA (16.1, StataCorp LLC, College Station, TX). Thematic map was created using QGIS® software (version 3.18.3), with administrative boundaries data from geoBoundaries.18
Ethical considerations
Programmatic data was used for this analysis. Data used was collected as part of the COVID-19 vaccination monitoring process. However, an application for exemption was also submitted to the National Human research ethics committee (NHREC).No personal details of respondents or identifiers is contained in this paper and so no consent was required for publication.
Role of the funding source
No grants were provided for the study design, data collection, data analysis, data interpretation, related to the development of this of this manuscript. TN, OW, EN had full access to all the data used in this study and all authors had final responsibility for the decision to submit for publication
Results
Background characteristics
Table 1 shows the background summary statistics of 10 184 HWs who responded to the survey across the 36 States and the Federal Capital Territory of Nigeria. The mean age of the respondents was 40.1 ± 9.8 years. The majority of survey respondents were females [65.5% (6 672/10 184)] and community health extension workers (CHEW) [50.5% (5 143/10 184)]. Most respondents worked in government public health facilities [89.1% (9 069/10 184)], while 76.5% (7 786/10 184) were in primary healthcare centres. There were 12.6% (1 288/10 184) of the survey respondents who had previously tested positive for COVID-19. Among those who had previously tested positive for COVID-19, 98% (1 262/1 288) were vaccinated compared with 91% (8,064/8,896) among those who had not previously tested positive.
Table 1.
Background characteristics of healthcare workers who responded to the survey across the 36 States and the Federal Capital Territory of Nigeria.
| Variable | Total (%) | Hesitant (%) | Not hesitant (%) |
|---|---|---|---|
| n = 10184 | n = 858 (8.4) | n = 9326 (91.6) | |
| Age, mean (SD) | 40.1 (9.8) | 36.3 (10.7) | 40.5 (9.7) |
| Age | |||
| <20 | 126 (1.2) | 21 (16.7) | 105 (83.3) |
| 20-29 | 1480 (14.5) | 236 (16.0) | 1244 (84.0) |
| 20-39 | 3001 (29.5) | 282 (9.4) | 2719 (90.6) |
| 40-49 | 5442 (53.4) | 208 (5.8) | 3388 (94.2) |
| 50-59 | 1846 (18.1) | 92 (5.0) | 1754 (95.0) |
| ≥60 | 135 (1.3) | 19 (14.1) | 116 (85.9) |
| Sex | |||
| Female | 6672 (65.5) | 633 (9.5) | 6039 (90.5) |
| Male | 3512 (34.5) | 225 (6.4) | 3287 (93.6) |
| Region | |||
| Northcentral | 1381 (13.6) | 176 (12.7) | 1205 (87.3) |
| Northeast | 1389 (13.6) | 99 (7.1) | 1290 (92.9) |
| Northwest | 1518 (14.9) | 62 (4.1) | 1456 (95.9) |
| Southeast | 863 (8.5) | 92 (10.7) | 771 (89.3) |
| South-South | 1090 (10.7) | 98 (9.0) | 992 (91.0) |
| Southwest | 3943 (38.7) | 331 (8.4) | 3612 (91.6) |
| Type of health workforce | |||
| CHEW | 5143 (50.5) | 307 (6.0) | 4836 (94.0) |
| Doctor | 302 (3.0) | 42 (13.9) | 260 (86.1) |
| Environmental health assistant | 1733 (17.0) | 165 (9.5) | 1568 (90.5) |
| Lab scientist | 227 (2.2) | 29 (12.8) | 198 (87.2) |
| Laboratory technologist | 272 (2.7) | 37 (13.6) | 235 (86.4) |
| Nurse/midwife | 2166 (21.3) | 273 (12.6) | 1893 (87.4) |
| Optometrist | 49 (0.5) | 1 (2.0) | 48 (98.0) |
| Pharmacist | 153 (1.5) | 26 (17.0) | 127 (83.0) |
| Pharmacy technician | 139 (1.4) | 16 (11.5) | 123 (88.5) |
| Level of healthcare facility | |||
| Community | 843 (8.3) | 126 (15.0) | 717 (85.0) |
| Primary | 7786 (76.5) | 531 (6.8) | 7255 (93.2) |
| Secondary | 985 (9.7) | 122 (12.4) | 863 (87.6) |
| Tertiary | 570 (5.6) | 79 (13.9) | 491 (86.1) |
| Type of facility | |||
| Private | 1115 (10.9) | 232 (20.8) | 883 (79.2) |
| Public | 9069 (89.1) | 626 (6.9) | 8443 (93.1) |
| Previously tested positive for COVID-19 | |||
| No | 8896 (87.4) | 832 (9.4) | 8064 (90.6) |
| Yes | 1288 (12.6) | 26 (2.0) | 1262 (98.0) |
| Willing to offer vaccine to family | |||
| No | 346 (3.4) | 118 (34.1) | 228 (65.9) |
| Yes | 9417 (92.5) | 577 (6.1) | 8840 (93.9) |
| Maybe | 421 (4.1) | 163 (38.7) | 258 (61.3) |
COVID-19 vaccine confidence
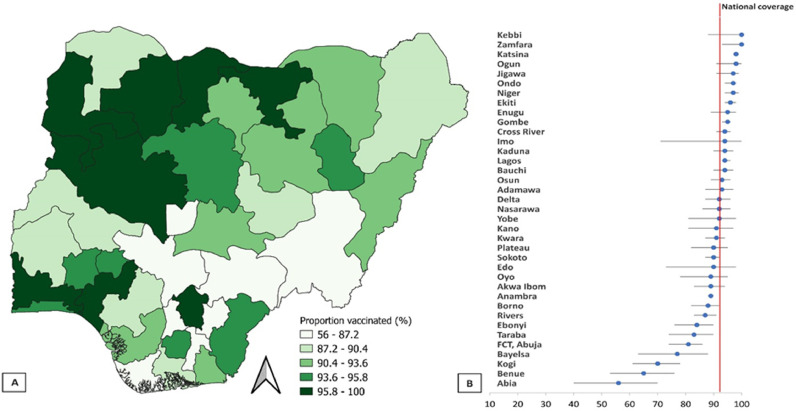
Overall, 92% (95% CI=91,92) of HW surveyed were confident of the COVID-19 vaccines and were already vaccinated at the time of this survey. Among survey respondents, those from the northeast of Nigeria were generally more confident of the COVID-19 vaccines. On the other hand, HWs in the north-central, and the southeast of Nigeria were less confident about the COVID-19 vaccines (Figure 2A). Specifically, healthcare workers in Kebbi, Zamfara, and Katsina States (all in the northeast of Nigeria) were the most confident of COVID-19 vaccines. Contrastingly, those in Kogi and Benue States (both in north-central Nigeria), and Abia State in southeast Nigeria were the least confident of the COVID-19 vaccines (Figure 2B). Supplementary Table 1 shows no significant difference between weighted and unweighted proportion (95% CI) of healthcare workers who were confident of the COVID-19 vaccines across the 36 States and the Federal Capital Territory of Nigeria.
Figure 2.
(a) Thematic map showing COVID-19 vaccine confidence among the survey respondents across the 36 States (2nd administrative unit) and the Federal capital Territory of Nigeria; (b) the proportion (95% CI) of survey respondents who have received (confident) the COVID-19 vaccines across the 36 States and the Federal Capital Territory of Nigeria compared to the national average.
Note: Weighted by the corresponding population of all the 36 States and the Federal Capital Territory of Nigeria.
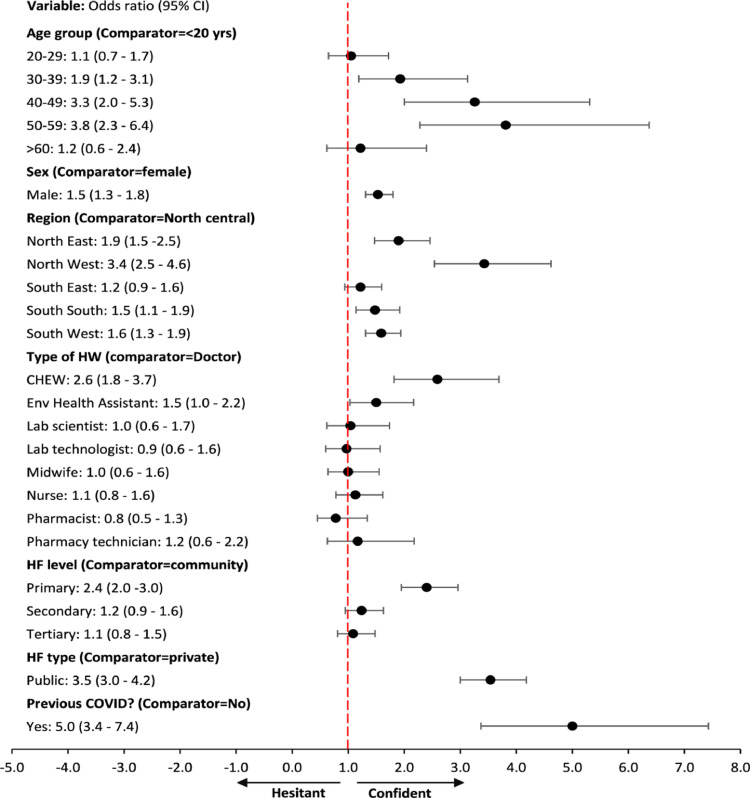
Determinants of COVID-19 vaccine refusals
There was a significant difference in the likelihood of accepting the COVID-19 vaccines between respondents who were aged 50 – 59 years old compared to those who were 20 years or less (OR=3.8, 95% CI=2.3 – 6.4, p<0.001) (Figure 3). The likelihood of respondents from States in the northwest of Nigeria refusing COVID-19 vaccination was lower compared to those from States in Northcentral Nigeria (OR=3.4, 95% CI=2.5 – 4.6, p<0.001). CHEW were 2.6 times less likely to refuse the COVID-19 vaccines compared to doctors, while healthcare workers in public facilities were 3.5 times less likely to refuse the COVID-19 vaccines compared to healthcare workers in private facilities. There was a significant difference in the likelihood of not refusing the COVID-19 vaccines between respondents who had previously tested positive for COVID-19 compared to those who have not previously tested positive (OR=5.0, 95% CI=3.4 – 7.4, p<0.001) (Figure 3).
Figure 3.
Forest plot (multivariate logistic regression) indicating the association between health worker characteristics and vaccine confidence.
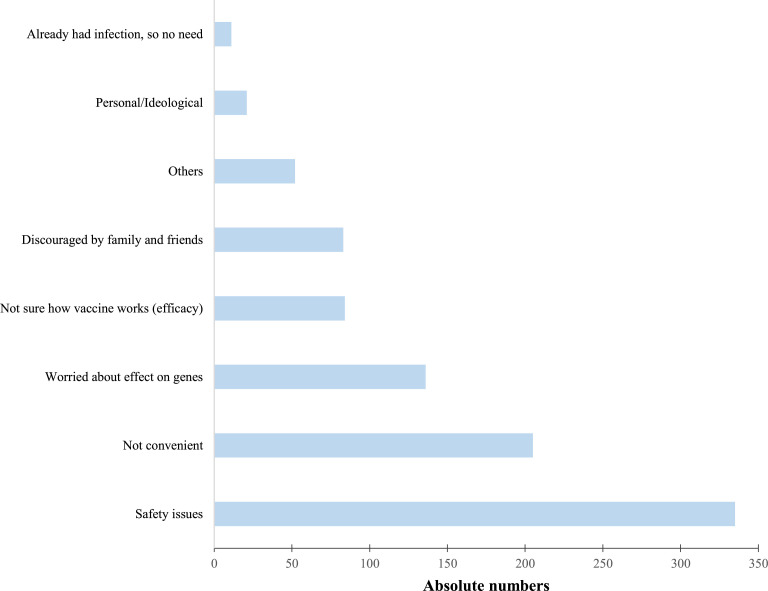
Figure 4 shows the reasons advanced for lack of confidence in the COVID-19 vaccines by the 858 surveyed healthcare workers who have been offered but have not received the COVID-19 vaccine. Safety-related issues, including fears that the vaccines would be harmful to them, their unborn babies (for those who were pregnant), or their breastfeeding infants were the commonest reasons [39% (335/858)] for lack of confidence in the vaccine. About fifteen percent (136/858) of survey respondents who were not confident in receiving the COVID-19 vaccine said that they were worried that the vaccine could alter their genes or genetic makeup. Personal ideology and having been previously infected by the virus were the least common reasons advanced for lack of confidence by the healthcare workers who were not confident in the COVID-19 vaccines.
Figure 4.
The reasons advanced by healthcare workers for lack for confidence in COVID-19 vaccines across the 36 States and the Federal Capital Territory of Nigeria (n=858).
*Multiple responses provided by survey respondents.
Sources of negative information about COVID-19 vaccines
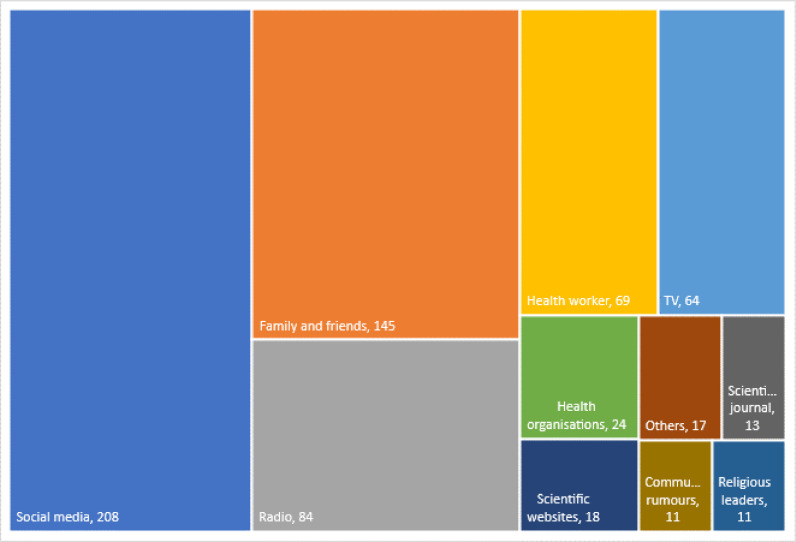
Among the survey respondents who were hesitant about the COVID-19 vaccines, 57% (479/858) agreed to having received negative pieces of information that influenced their decision not to be vaccinated. Of these, the commonest source [43.4% (208/479)] of negative information about COVID-19 vaccines was social media. Family or friends, and radio were also common sources of negative information about COVID-19 vaccines accounting for the second and third commonest source of negative information respectively (Figure 5). Community rumours and information by religious leaders were the least common sources of negative information about COVID-19 vaccines that influenced the decision to receive the vaccines.
Figure 5.
Sources of negative information about COVID-19 vaccines that contributed to lack of confidence in the COVID-19 vaccines among health workers across the 36 States and the Federal Capital Territory of Nigeria.
Note: 479 out of the 858 healthcare workers who were not confident in the COVID-19 vaccines agreed to having received negative information that influenced their decisions. Multiple responses were provided by survey respondents and absolute numbers are presented in the chart.
Discussion
Addressing vaccine hesitancy among HWs is critical in maintaining the successes of vaccination programs.8 This study assessed vaccine confidence and hesitancy among HWs during the initial phase of the COVID-19 vaccination roll-out in Nigeria. The study received responses from over 10 000 HWs across the 36 States and the Federal Capital Territory of Nigeria. While most HWs were confident and had already received the vaccine, confidence varied across the six-geo-political zone with the north-east and north-central regions recording the highest and lowest confidence, respectively. Also, previous history of COVID-19 infection/disease was found to be the strongest determinant of confidence and social media, was the most common source of negative information that influenced the decision not to be vaccinated.
We found that a vast majority of HWs with access to the COVID-19 vaccines were confident about receiving the vaccine offered in Nigeria and were already vaccinated. The high acceptance among HWs found in our study is in contrast with low acceptance observed in studies conducted among HWs in Nigeria, Ghana, Democratic Republic of Congo and Saudi Arabia prior to the availability of the vaccine.9,11,12,15,19 This high acceptance can be attributed to the availability of the vaccine in-country, and the priority given to vaccinating HWs in the initial phase.20 This high acceptance may also have been influenced by the already successfully vaccine deployments reported across Europe and the Americas prior to vaccine arrival in Nigeria. A study by Viswanath et al showed that those who felt that they were more susceptible to COVID-19 and that the consequences are likely to be severe were more willing to accept vaccines offered to them and people under their care. The health belief model theorizes that people's beliefs about whether they were susceptible to disease, and their perceptions of the benefits of trying to avoid it, influenced their readiness to act.21 Being at the coalface of the fight against COVID-19, and having seen first-hand, the devastating consequences of the virus, may have increased the willingness to vaccinate themselves.22 This may have also accounted for the over 5-fold difference in vaccine confidence amongst those with prior history of the coronavirus infection.
Majority of the HWs involved in the deployment of the COVID-19 vaccines in Nigeria were community-based health workers (referred to as CHEWs). Most of the vaccination points were at the primary health care centers compared to secondary and tertiary health facilities. This emphasizes the role of primary health care in achieving universal coverage and the role of primary health care in deployment of quick interventions to large populations as needed during situations like outbreaks and pandemics. This role of community health workers has also been emphasized by the African Center for disease control (Africa CDC) highlighting their role in improving vaccination coverage with examples from Rwanda.23,24 The PHC system in Nigeria and other countries in Africa remain an important vehicle for achieving the SDG health goal and other global targets including Immunization Agenda 2030 (IA2030) and the Addis declaration on Immunization. It is believed that a strong and robust PHC system is a key vehicle needed to drive countries towards the achievement of the WHO targets of vaccinating at least 70% of the population by Q2 2021.
In Nigeria, the geo-political zones represent distinct levels of development, socialization, religious and political situations. Although coverage of routine childhood vaccines is generally lowest in the Northwest and Northeast, and highest in the South-South of Nigeria,25,26 our findings were paradoxical. Compared to routine childhood vaccination, our study shows that confidence in COVID-19 vaccine varied across the six geo-political zones, however, coverage was paradoxically highest in Northwest and Northeast and lowest in the North-Central and Southeast of Nigeria. This apparent and paradoxical regional differences in COVID-19 vaccine confidence among HWs in Nigeria compared to routine immunization may be reflective of a broader developmental and socio-political context. Institutional mistrust has been shown to negatively impact the likelihood of getting vaccinated. Trust in government is strongly associated with vaccine acceptance and can contribute to public compliance with recommended actions.9,14,27 As countries push towards increased vaccination of its populace, it is important to note that gaps in trust between the citizenry and the those in position of authority may impede success as has been shown elsewhere.28
Consistent with several studies, safety-related issues were found to be the most common reason cited by HWs for a lack of confidence in COVDI-19 vaccines.9,11,15,29 It is important that safety concerns about the vaccine be addressed using targeted interventions among HWs. The national vaccine deployment plan should focus on improving safety surveillance and publicly publish national data to address any concerns the populace may have on the vaccines being used in Nigeria as against using data shared from other countries. The national expert community (NEC) must be strengthened to conduct causality assessments for all adverse effects following immunization (AEFI) reported after administration of the COVID-19 vaccines. Furthermore, our findings show that social media was the most common source of negative information which influenced the decision made about receiving the vaccine.30 While social media was used by global health bodies to share information during the pandemic, more action should be taken to curb the spread of fake news by identifying and removing disease trolls while ensuring that accurate information are easily accessible.31
Our findings should be interpreted with the following limitation in mind. First, due to the survey design, our study is prone to non-response bias because the included participants may have disproportionately possessed certain characteristics compared to the non-responders which could have affected the outcomes. The fact that we weighted the analysis based on the corresponding population of each States potentially mitigates for non-response bias. Secondly, because our study asked respondents to describe their attitude or behaviours towards the COVID-19 vaccines rather than an objective measurement, it may have been prone to self-reporting bias. This sample was targeted at health workers engaged as vaccinators at designated health facility and vaccination post by the Nigeria immunization team as part of the national deployment and vaccination plan. The vaccination posts were selected based on population at the subnational administrative levels. We believe that the weighing of the results also addressing this concern. The weighting we have done relates to Total population by state as against health worker distribution. This is so due to the challenges around availability of health worker distribution data at subnational levels in Nigeria Third, the survey was conducted in the early phase of the vaccine roll-out and gives a snapshot of the behaviour and attitude of HWs at that time point. Confidence in COVID-19 vaccines among HWs in Nigeria might have evolved as new information about the safety, adverse reactions and more vaccine options are made available. Despite these limitations, this study is based on responses from a large number of HWs during the initial phase of COVID-19 vaccination rollout in Nigeria and provides important information which could inform COVID-19 vaccination strategies going forward.
We documented COVID-19 vaccine confidence amongst HWs in Nigeria following the initial phase of its national vaccine deployment plan between March and April 2021. We found that a high proportion of HWs had been vaccinated with the vaccines offered them and were confident about the vaccines. The majority of the HWs were community health workers deployed to primary health centers with older workers more likely to be confident compared to younger health workers.
Gaps remain around an optimal vaccine deployment as almost one-tenth of the HWs were still hesitant and can negatively influence the willingness to access the COVID-19vaccines by the general population who rely on them for health information. The HWs hesitancy was driven by negative information around vaccine safety mainly accessed through the social media.
Efforts around the call for vaccine equity and access will only be strengthened when countries like Nigeria and other LMICs demonstrate capacity to deploy available vaccines quickly. The NVDPs must be revised and robust enough to address the misinformation on vaccine safety and increase uptake using the available primary health care system and its health care workers to ensure access of covid vaccines to all eligible Nigerians.
Contributors
TN, OW, EN, and NN conceptualized the study while. TN, OW, EN and SO developed the initial draft. OW and EN conducted the data analysis and generated the charts and figures. The revision of the drafts were done by TN, OW, EN, NO, ED and SO. TN, OW, EN, NN and ED completed the final drafts with supervision by JE, US, AE and WM. All authors have reviewed, read and approved the final draft of the manuscript. TN, OW, EN had full access to all the data used in this study and all authors had final responsibility for the decision to submit for publication.
Data sharing statement
Data used as part of this work are publicly available and may be shared upon reasonable request to the corresponding author.
Declaration of interests
All authors have declared no conflict of interest as relates to this body of work.
Acknowledgements
We acknowledge the efforts of the numerous health workers deployed as part of the vaccination role out during the response to the covid outbreak in Nigeria. We thank Daniel Oyaole for the tremendous work done in managing the questionnaires and developing the checklist on the server while remotely supporting the teams during the data collection.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2022.101499.
Appendix. Supplementary materials
References
- 1.WHO. Weekly epidemiological update - 5 January 2021. https://www.who.int/publications/m/item/weekly-epidemiological-update—5-january-2021. Accessed 5 April 2021.
- 2.Nigeria Centre for Disease Control NCDC coronavirus COVID-19 microsite. Freq Asked Quest. 2020 https://covid19.ncdc.gov.ng/ Accessed 13 May 2021. [Google Scholar]
- 3.Microbe The Lancet. COVID-19 vaccines: the pandemic will not end overnight. Lancet Microbe. 2021;2:e1. doi: 10.1016/S2666-5247(20)30226-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Organization World Health. World Heal Organ. 2020. Guidance on developing a national deployment and vaccination plan for COVID-19 vaccines: interim guidance. [Google Scholar]
- 5.SAGE Working Group on Vaccine Hesitancy. Report of the SAGE working group on Vaccine hesitancy 12 November 2014*. 10.4172/2155-9821.1000161 [DOI]
- 6.Leask J, Willaby HW, Kaufman J. The big picture in addressing vaccine hesitancy. Hum Vaccines Immunother. 2014 doi: 10.4161/hv.29725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization . World Heal Organ. 2021. The role of community health workers in COVID-19 vaccination. Implementation Support Guide.https://apps.who.int/iris/bitstream/handle/10665/340986/WHO-2019-nCoV-NDVP-%0ACHWs-role-2021.1-eng.pdf [Google Scholar]
- 8.Dubé E. Addressing vaccine hesitancy: the crucial role of healthcare providers. Clin Microbiol Infect. 2017;23:279–280. doi: 10.1016/j.cmi.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 9.Acceptability of COVID-19 Vaccination among Health Care Workers in Ghana. https://www.hindawi.com/journals/aph/2021/9998176/. Accessed 13 May 2021.
- 10.Nachega JB, Sam-Agudu NA, Masekela R, et al. Comment Addressing challenges to rolling out COVID-19 vaccines in African countries. 2021. 10.1016/S2214-109X(21)00097-8 [DOI] [PMC free article] [PubMed]
- 11.Ekwebene OC, Obidile VC, Azubuike PC, Nnamani CP, Dankano NE, Egbuniwe MC. COVID-19 vaccine knowledge and acceptability among healthcare providers in Nigeria. Int J Trop Dis Heal. 2021:51–60. [Google Scholar]
- 12.Qattan AMN, Alshareef N, Alsharqi O, Al Rahahleh N, Chirwa GC, Al-Hanawi MK. Acceptability of a COVID-19 vaccine among healthcare workers in the Kingdom of Saudi Arabia. Front Med. 2021;8 doi: 10.3389/fmed.2021.644300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Larson HJ, Broniatowski DA. Volatility of vaccine confidence. Science (80-.) 2021;371:1289. doi: 10.1126/science.abi6488. [DOI] [PubMed] [Google Scholar]
- 14.Lazarus JV., Ratzan SC, Palayew A, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27:225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nri-Ezedia CA, Okechukwu C, Ogochukwu OC, et al. Predictors of coronavirus disease-19 (COVID-19) vaccine acceptance among Nigerian medical doctors. SSRN Electron J. 2021 doi: 10.2139/ssrn.3820535. [DOI] [Google Scholar]
- 16.World Population Review Nigeria population 2021. World Popul Rev. 2021 https://worldpopulationreview.com/countries/nigeria-population Accessed 13 May 2021. [Google Scholar]
- 17.World Health Organization. Global health workforce statistics database. 2020. https://www.who.int/data/gho/data/themes/topics/health-workforce. Accessed 13 May 2021.
- 18.Runfola D, Anderson A, Baier H, et al. GeoBoundaries: a global database of political administrative boundaries. PLoS One. 2020;15(4) doi: 10.1371/journal.pone.0231866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kabamba Nzaji M, Kabamba Ngombe L, Ngoie Mwamba G, et al. Acceptability of vaccination against COVID-19 among healthcare workers in the Democratic Republic of the Congo. Pragmatic Obs Res. 2020;11:103–109. doi: 10.2147/POR.S271096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Odekunle FF, Odekunle RO. The impact of the US president's emergency plan for AIDS relief (PEPFAR) HIV and AIDS program on the Nigerian health system. Pan Afr Med J. 2016;25:143. doi: 10.11604/pamj.2016.25.143.9987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Cancer Institute . 2nd Ed. 2005. Theory at a Glance A Guide For Health Promotion Practice. [Google Scholar]
- 22.Viswanath K, Bekalu M, Dhawan D, Pinnamaneni R, Lang J, McLoud R. Individual and social determinants of COVID-19 vaccine uptake. BMC Public Health. 2021;21:1–10. doi: 10.1186/s12889-021-10862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization Regional Office for Africa. Community health worker programmes in the WHO African region: evidence and options policy brief. 2017. https://www.afro.who.int/sites/default/files/2017-07/. Community Health Worker Policy Brief - English_0.pdf. Accessed 1 Nov 2021.
- 24.Robson J, Bao J, Wang A, et al. Making sense of Rwanda's remarkable vaccine coverage success. Int J Healthc. 2020;6:56. [Google Scholar]
- 25.Adeloye D, Jacobs W, Amuta AO, et al. Coverage and determinants of childhood immunization in Nigeria: A systematic review and meta-analysis. Vaccine. 2017;35:2871–2881. doi: 10.1016/j.vaccine.2017.04.034. [DOI] [PubMed] [Google Scholar]
- 26.Wariri O, Nkereuwem E, Erondu NA, et al. A scorecard of progress towards measles elimination in 15 west African countries, 2001–19: a retrospective, multicountry analysis of national immunisation coverage and surveillance data. Lancet Glob Heal. 2021;9:e280–e290. doi: 10.1016/S2214-109X(20)30481-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stoop N, Hirvonen K, Maystadt JF. Institutional mistrust and child vaccination coverage in Africa. BMJ Glob Heal. 2021;6:4595. doi: 10.1136/bmjgh-2020-004595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nigeria's Political Leaders Need to Win Trust to Tackle COVID-19 | Chatham House – International Affairs Think Tank.
- 29.Verger P, Scronias D, Dauby N, et al. Attitudes of healthcare workers towards COVID-19 vaccination: a survey in France and French-speaking parts of Belgium and Canada, 2020. Eurosurveillance. 2021;26 doi: 10.2807/1560-7917.ES.2021.26.3.2002047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Burki T. Vaccine misinformation and social media. Lancet Digit Heal. 2019;1:e258–e259. [Google Scholar]
- 31.Garrett L. COVID-19: the medium is the message. Lancet. 2020;395:942–943. doi: 10.1016/S0140-6736(20)30600-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.