Abstract
The number of aesthetic procedures performed worldwide continues to grow together with an increase in the population seeking the restoration or preservation of a youthful appearance. Requests for non-surgical body rejuvenation are increasing. Patients are looking for safe and effective minimally invasive aesthetic procedures. Soft-tissue dermal fillers can meet these expectations. Based on the beneficial outcomes of these treatments in many facial areas, a new trend is developing to target body areas. Different dermal fillers are available and include collagen stimulators initially developed to restore facial volume. Furthermore, they are associated with long-lasting efficiency, a high level of patient satisfaction and a good safety profile, with mainly minor adverse events reported. In appropriate conditions of use, they are now used for body rejuvenation in clinical practice. Their use is expanding and allows addressing various issues including volume loss, skin laxity, cellulite, striae distensae and wrinkles. This review focuses on poly-L-lactic acid (PLLA), used in the first collagen stimulator and one of the most investigated in facial and in off-facial body applications. The available published data, although still limited, are presented by body area, neck and chest, buttocks, abdomen, upper arms, thighs, knees, and hands. Key features of the concerned zones and the main clinical signs affecting the body part as well as the injection modalities are provided along with the aesthetic results. This represents the state of the art on which to base further developments necessary for optimal and safe outcomes of treatment with the PLLA-based collagen stimulators and others in this class for body rejuvenation.
Keywords: poly-L-lactic acid, PLLA, volume augmentation, body contouring, dermal filler, collagen stimulator, buttocks, body rejuvenation, skin laxity, skin quality
Introduction
The number of patients seeking nonsurgical rejuvenation of the face and the body is continuing to increase due to a growing aging population concerned with physical appearance. Women wishing to maintain a younger-looking appearance and attractiveness represent 92% of all cosmetic procedures.1 Men are keen to maintain physical characteristics associated with virility.2 Millennials are also increasingly concerned with preserving their beauty and youth.3 Among the various treatment approaches, different minimally invasive techniques have been developed and dermal fillers currently come second after botulinum toxin type A (BTA).3 Their use is increasing worldwide. Dermal fillers allow the restoration of volume loss by filling the area concerned, to correct wrinkles, and to improve facial contours. The number of cosmetic procedures with dermal fillers has risen from 1.6 million in 2011 to 3.4 million in 2020.1
In the resorbable category of dermal fillers, cross-linked hyaluronic acids (HA) come first in the ranking followed by collagen stimulators characterized by their property of inducing natural collagen production. The latter are made of either polymers, polycaprolactone (PCL; Ellansé, 30% microspheres; Sinclair Pharmaceuticals, London, UK),4,5 Poly-L-lactic acid (PLLA, Sculptra 150 mg/vial; Galderma, La Tour-de-Peilz, Switzerland;6–9 other PLLA-based product, Lanluma V [210 mg /vial] and Lanluma X [630 mg/vial], Sinclair Pharmaceuticals, London, UK), and of ceramics, calcium hydroxylapatite (CaHA, Radiesse 30% microspheres; Merz Aesthetics, Frankfurt am Main, Germany;10–12 other CaHA-based product, Crystalys Luminera 55.7% microspheres; Allergan Aesthetics, an AbbVie group, USA). Besides their different compositions, formulations, product preparations and injection modalities, their main differences consist of their degradation kinetics, level of efficacy and duration of action. The aliphatic polyesters, PCL and PLLA, degrade slowly by hydrolysis of the ester bonds and have a long duration with PCL having the longest.4,13–16 CaHA degrades more rapidly by a different mechanism.10,12 Polymethyl methacrylate (PMMA, Bellafill 20% microspheres in bovine collagen, Suneva Medical, California, USA) is a permanent polymer, that had limited use in Europe given this characteristic.17 All these products were originally developed for facial indications. Their use in body rejuvenation, initially performed using invasive methods such as surgery or lipofilling, was considered later on with the use of lasers and dermal fillers, along with the increasing patients’ demand.18
PLLA is a biocompatible, biodegradable and bioresorbable polymer. It is an alpha hydroxy acid polymer of the lactic acid L-enantiomeric structure that has been safely used in many applications and in medicine for more than 30 years.19–22 PLLA-based fillers are supplied as a lyophilized powder to be reconstituted with sterile water according to specific conditions.19,23
PLLA filler (Sculptra) was approved in aesthetics in 1999 in Europe and in 2004 in Europe and in USA by the US Food and Drug administration (FDA) in the correction of fat loss associated with antiretroviral therapy-induced lipoatrophy in HIV patients, and in 2009 by the FDA for the correction of nasolabial fold deficiencies and other facial wrinkles in immunocompetent patients. Its use in these indications has expanded worldwide, associated with good long-term aesthetic results thanks to its biostimulatory-collagen effect.9
PLLA-based filler is the first collagen stimulator of long duration of action following several needed sessions of treatment. If one considers the first demonstrations of these key product characteristics, the collagen stimulatory properties were evidenced in human in subjects (n=14) who received PLLA injections (3 sessions, spaced 4 weeks apart) at the postauricular level by collagen histochemical determination on biopsies taken at different times. Increase of collagen type-I was shown at 3 and 6 months.9 This study opened the new class of collagen stimulators. The long duration of action was demonstrated in a first pivotal study comparing PLLA versus collagen (116/117 subjects, respectively); the long-term safety/efficacy was shown up to 25 months.14 The rationale for several sessions was first documented in a dedicated article;24 this modality allows the effect through collagen stimulation, a biological process to occur and avoids overcorrection. Numerous clinical studies were conducted on this basis both in aesthetics and HIV lipoatrophy, the two main indications. PLLA fillers are among the most clinically documented products.
Beyond its classical and long-term use in facial indications, PLLA is also currently used in body treatment for volume augmentation, body contouring, skin laxity, cellulite, scars, and striae distensae of off-face areas such as the neck and chest, buttocks, abdomen, arms, thighs, knees and hands.25–27 Recently, PLLA has been designed and is available in larger vials to conveniently treat large depressed areas like buttocks (Lanluma X) while Lanluma V is used for the other off-facial and facial areas. A recent survey reported that gluteal augmentation (42.4%) is the second most common usage of PLLA in the USA, following HIV lipoatrophy (46.8%), illustrating the importance of off-face treatments with PLLA.28
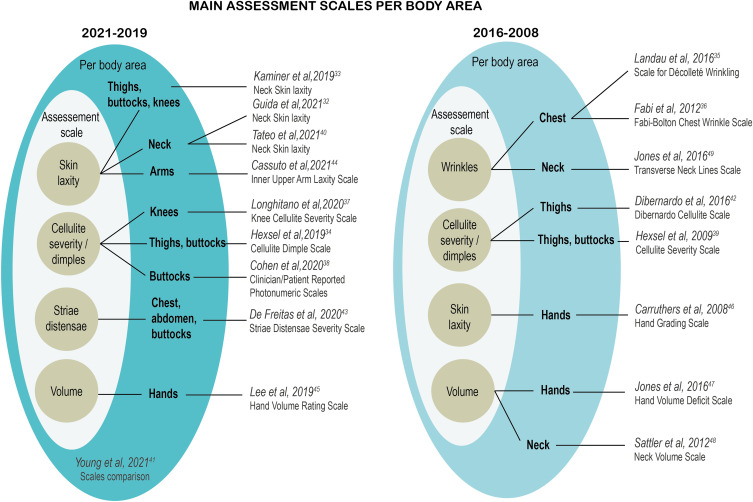
Considering the further increase in body applications and the various modalities in the use of PLLA according to the area treated,6,28–31 it appeared necessary to analyze all the available safety and efficacy results obtained so far from clinical data per area to improve the definition of optimal and safer treatment protocols. Several validated assessment scales developed in parallel to the growing use of PLLA in off-facial areas are presented (Figure 1).32–49
Figure 1.
Main aesthetic assessment scales per body area in 2021–2019 and 2016–2008. Scheme from MO Christen and O Granio 2022.
Note: During the review process some articles of interest have seen published including one by Hexsel et al145 scale on buttocks and Green et al146 scale on hands.
A literature review of the data available on PLLA in off-face areas is proposed. The data are discussed per area and gathered in tabulated summaries focused on efficacy, safety, and treatment protocols. The main and most recently published studies on the other collagen stimulators are cited per body area to assess the information available regarding this whole class of fillers and their increasing contribution to body treatment.
Methodology
Literature Search and Data Selection
A search was carried out on MEDLINE, PubMed, Cochrane Library databases and Google Scholar. The databases were searched since inception until July 5th, 2021. The search terms comprised PLLA and poly-L-lactic acid in aesthetics in body areas. Articles were selected for inclusion if they were published in English language and dealt with studies conducted on humans (clinical studies, case-reports, reviews, letters, and recommendations). Articles on PLLA facial treatment only were excluded. The search was extended to articles published in books. A total of 49 articles was included in the review. PLLA in body applications has opened the way to other collagen stimulators in these new areas. To document this practice, the main, recent publications on the use of those products for body treatment were selected from PUBMED, MEDLINE, Google Scholar and also based on the author’s awareness in the field (namely polycaprolactone [PCL], calcium hydroxylapatite [CaHa], polymethylmethacrylate [PMMA]). Publications are cited and referenced in the article in each body area chapter.
PLLA in the Neck and Chest
Nowadays more and more patients obtain a younger appearance through facial rejuvenation procedures,1 creating a sharp contrast with the closest areas, the neck and chest. As the most visible body part, the neck was the first off-face area to be treated and demand has been increasing.50
Both aging and behaviors (ultraviolet, infrared, and visible light or pollution exposure) affect the quality of the skin resulting in line/wrinkle formation, skin laxity, hyperpigmentation, erythema and telangiectasia. Different aesthetic procedures exist alone or in combination such as superficial chemical peels to improve skin texture, sclerotherapy to correct the presence of reticular veins, laser and light therapies to improve signs of photoaging (fine lines and wrinkles, hyperpigmentation and skin texture), BTA, HAs and collagen-stimulators PCL, CaHA and PLLA to correct wrinkles and improve skin texture and skin quality.12,26,27,51–54 Hyperdiluted CaHA used was shown to be effective in tightening skin in these areas.12,55–58 The benefits of combining treatments was evidenced with CaHA combined with microfocused ultrasound in particular59 and PCL filler with HA and PLLA threads.51 Given their long-lasting biostimulatory properties, PLLA fillers, Sculptra and Lanluma V, used alone or in combination, are a good option for treating lines and wrinkles of the neck and chest.26,27,52,53,60–65
It is important to note that the skin of the chest area is thin, and that the distribution of subcutaneous fat varies from one patient to another. The superficial chest wall is composed of skin, subcutaneous fat, pectoralis major, fat, pectoralis minor and ribs.50 For the neck, PLLA is injected between the deep dermis and subcutaneous tissue in the anterolateral region.61,62 For the chest, PLLA is injected into the subcutaneous tissue plan over the platysma between the breast and then laterally in the plane of subcutaneous fat at an angle of 60°, at equidistant 1.0-cm points.61,62 The treatment area is between the suprasternal notch, the midclavicular line and the fourth rib.22,50,66
PLLA for neck and chest rejuvenation demonstrated a favorable efficacy and a good safety profile in studies including facial and off-face areas together with studies dedicated to those areas (Table 1). In a large European retrospective study conducted on 2131 subjects, 64 patients received PLLA to treat the neck and chest (1–2.5 vials/session; 5mL/vial). Treatment yielded impressive results in the case of extreme concavities, such as the pectus excavatum. Globally, 95% of the patients were satisfied with a duration of treatment benefit of up to 30 months.67 In photographic analysis, PLLA treatment was associated with 81% to 100% improvement depending on the evaluator in 21 patients after receiving an average of 1.8 treatment session (1.0 and 2.38 for patients with moderate and severe signs of photoaging, respectively); more than 90% of patients were satisfied.61 In another study on 568 subjects with 162 treated for the neck and 72 for the chest, good results assessed with the DGS score (definitive graduated score) were obtained with PLLA (up to 7.5 and 7.8 for the neck and chest, respectively) after a median number of sessions of 3.68 A prospective study on 25 patients with moderate- to-severe crepiness and wrinkles showed an improvement in 90% of patients 6 months post-treatment after 3 treatment sessions (1 vial/session; 9mL/vial).64 Similar results were reported in 28 patients treated with PLLA for moderate-to-severe rhytids of the neck and chest after a mean of 2.3 treatment sessions (range, 1–7; 16mL/session; 16mL/vial); results were sustained up to 18 months.63 The best improvement was for patients who received at least 3 treatment sessions.63,66 Studies reported no or only mild transient adverse events; the most frequent were hematomas and ecchymoses at the injection site.62–64,66–68
Table 1.
Published Efficacy/Safety Data and Protocols on PLLA in Neck and Chest
| Reference (Nb of Patients) | Design/Objectives | Efficacy | Safety | Reconstitution/Vial | Session/Patient | Injection Technique/Device | Nb Vial** | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Volume/Time | Total Volume | Nb | Intervals (wks) | Per Session | Total | |||||
| Fabi 201566 Vanaman & Fabi 201550 (NR) | Clinical practice Wrinkles and lines |
Visual improvement (PA) | Common minor reaction disappearing rapidly: Pain, ecchymoses, edema, pruritus, hematoma, nodule | 7 mL* for 2–24h + L1% | 16 mL | 3–4 | 4 | Linear threading injection into the reticular dermis and subcutaneous tissue Needle/cannula 25G 1.5-inch |
1 | 3–4 |
| Zac & Da Costa 202062 (NR) | Technical publication Wrinkles and lines |
NR | Transient hematomas, ecchymoses | 8 mL for 24–48h + L2% | 20 mL | 1–4 | 4–8 | Injection between the deep dermis and subcutaneous tissue Needle 26G |
1 (12/20 mL) | 1–4 |
| Mazzuco & Hexsel, 200961 (N=36) | Clinical experience Skin laxity, atrophy and wrinkles F-U: 18 months |
81–100% GAIS improvement (n=21) Patients’ satisfaction: 91.6% (n=36) Effect maintained up to 18 months |
Transient hematomas, ecchymosis; early-onset subcutaneous nodule (n=1) | 10 mL for 48–72h + L2% | 11.9 mL | 1–4 | 4–6 | Injection between the deep dermis and the subcutaneous tissue Needle 27 G |
1 (4–7 mL) | 1–4 |
| Bolton et al 201163 (N=28) | Clinical practice, Retrospective study review Chest wrinkles scale F-U: 18 months |
1- to 2-point FBWS improvement Effect maintained up to 18 months |
No AE reported during the study period, no nodule formation | 14 mL* for > 2h-o/night + L1% | 16 mL | 1–7 | 4 | Needle 26G 1.5-in | 1 (16 mL) | 1–7 |
| Wilkerson & Golberg 201864 (N=25) | Prospective review Moderate-to severe crepiness and chest wrinkles F-U: 6 months |
90% of patients with ≥1-point FBWS improvement 6-month post treatment | No AE reported by investigators | 9 mL, incubation time NR | 9 mL | 3 | 8–12 | Intradermally injection Needle 27G |
1 | 3 |
| Peterson & Goldman 201152 (NR) | Clinical practice, retrospective review Chest rhytids |
Skin quality improvement (PA) | Ecchymoses, edema, pain, pruritus, inflammation, nodules, hematomas | 6 mL for 24h + L1% | 16 mL | 3–4 | 4 | Retrograde fanning injection in the subcutaneous tissue Needle 27G 1.5-in |
1 | 3–4 |
| Lorenc, 201222 (NR) | Clinical practice Volume loss |
Effective volume restoration (PA); High patient satisfaction (96%) | Safe | 5 mL > 2h + L1% | 24 mL | 1–2 | 6 | Tunneling injection in the supraperiostal plane Needle 27G 0.5-in |
NR | NR |
| Vleggaar, 200667 (N=64/2131) | Clinical practice Skin laxity F-U: 4–6 weeks post-treatment |
95.1% of patient satisfied | No serious AE; ecchymosis, transient soreness | 4 mL, 30 min - o/night + L2% | 5 mL | NR | 4–6 | Tunneling injection in the deep dermal subcutaneous plane Device NR |
NR | NR |
| Redaelli & Forte, 200968 (N=234/568) | Clinical practice Sin laxity F-U: 12 months |
DGS improvement of 7.5 to 7.8 | Few temporary AE, nodule formation (1%) | 6–8 mL 24–48h | 6–8 mL | NR | NR | Linear retrograde injection in the deep dermis/subcutis layer Needle 25–27G |
NR | NR |
Note: *Reconstitution in bacteriostatic water instead of sterile water for injection; **Volume injected when reported.
Abbreviations: AE, adverse event; DGS, definitive graduated score; FBWS, Fabi-Bolton 5-point wrinkle scale; GAIS, Global Aesthetic Improvement Scale with Grade 1, very much improved, Grade 2, much improved, Grade 3, improved, Grade 4, no change, Grade 5, worse; F-U, follow-up; L, lidocaine; NR, not reported; PA, photographic assessment.
The volume, duration of PLLA reconstitution and injection technique varied between studies (Table 1). In the first clinical use, the volume of PLLA reconstitution was 3–5 mL, as recommended, for a reconstitution time lasting overnight.67 Another study conducted on 234 patients utilized a reconstitution volume of 6–8 mL.68 In order to reduce the incidence of nodule formation, recommendations were given to increase the reconstitution volume of PLLA in general, as well as for neck and chest treatment.6 The volume of PLLA reconstitution increased from 5mL,67 6–8 mL,68 9 mL,64 12 mL,61,69 16 mL,6,52,63,66 20 mL62 to 24 mL.22 The duration of reconstitution varied from just prior to use,64 2–24h,22,50,63,66,67 24–48h,62,68,69 to 48–72h before administration.61 PLLA is injected with a 25G needle or a cannula,66 a 26G needle,62,63,68 or a 27G needle,22,52,61,64,68 using a retrograde linear threading52,66,68 or fanning technique.52,61,69 Most patients received 1 vial per session and the injected volume could represent all the reconstituted PLLA (16 mL),63 or a part of it.61,62 The total number of sessions ranged from 1 to 7, and 4–8 weeks apart.
PLLA and Buttocks
The gluteal region corresponds to the most common procedure in body (buttocks augmentation increased by 38.4% in 2019 and by 65.9% since 2015; buttocks lift by 25.5% in 2019 and by 77.6% since 2015).70 This area plays an important role in physical attractiveness and has always been considered as a criterion of female beauty linked to fecundity and health status.71 With aging, weight loss, or disease states, the skin loses its elasticity and a loss of gluteal subcutaneous fat leads to the decreased volume of the area and gluteal ptosis. The gluteal suspension system, a dense ligamentous connective tissue, becomes less firm leading to sagging buttocks.72 This process leads to impaired skin quality with the development of striae and cellulite-derived indentations that particularly affect the buttocks and thighs and a large majority of a large majority of women (80–90% are concerned by cellulite to some degree).73 Cellulite is characterized by topographic alterations of the surface relief of the skin with depressed areas due to thick subcutaneous septae and raised zones due to the projection of underlying fat to the surface of the skin. The association of the depressions, dimpling (indentations) with increased thickness of the fibrous septae was confirmed by MRI.74–76 This multifactorial condition is a real concern and the consequence is increased interest in buttock aesthetics.77 A waist-to-hip ratio of 0.6 to 0.65 for women78 and 0.85 for men79 are relevant indicators for physicians to define an aesthetic strategy. Other factors include the shape of the rounded, lifted posterior projection, the smooth, inward shape of the lumbar curvature (A-shaped, square shape, curvy, V-shaped and round-shaped) as well as the frame (fat, bone and skin) of the buttocks.73,80 The buttock area has been traditionally treated by surgery, including surgical lifting, alloplastic/silicone implants and autologous fat grafting known as the Brazilian lift.81–83 This has opened the way to buttock treatment and attracted attention to safety.84 Severe complications and even death by fat emboli were reported.84,85 However, recommendations have been published to limit complications.73 SubcisionTM, which can be manual, vacuum- or laser-assisted, is another modality of cellulite treatment. It allows cutting the fibrous bands, releasing tension and evenly redistributing the subcutaneous fat.86,87 The ideal patient candidates requesting buttock augmentation have a low body mass index (≤20 kg/m2) and a minimal excess fat, which contraindicates autologous fat transfer.22,73 Non-surgical treatments for buttocks augmentation with the use of HAs or collagen stimulators such as PCL,88 CaHA12 PMMA,89 are increasing with the advantage of their long-lasting effect1,70,90 and are indicated for those patients as well as for patients looking for improved contouring, reshaping, skin quality, striae distensae and cellulite appearance.76,91 Thanks to its biostimulatory properties, PLLA is increasingly used for gluteal augmentation and to treat contour irregularities.22,26–28,90,92–99 Its use to treat buttocks is the first off-facial application of the product according to a recent American survey.28 In this area, Lanluma, given its specific presentation, is well adapted for the patient and the physician. Very recently, expert recommendations for buttock contouring with PLLA have been published.100
A danger zone called the “danger triangle” must be properly identified.73 PLLA must be administered over the muscle within the subcutaneous layer.73,96 The upper and middle parts of the buttocks are the regions where most filler should be injected to achieve the most aesthetic and natural outcome for volume augmentation and the biostimulatory properties of the PLLA helps to lift the lower region.73,92 The lateral part contributed to the need for reshaping.
Good results with PLLA treatment were reported in case reports, retrospective reviews, clinical studies,97 and clinical practice, for buttock augmentation and reshaping/contouring22,92,98,99 to treat skin laxity/flaccidity,92,94–96 cellulite,92–97 scars and striae appearance94 providing gluteal augmentation, cellulite appearance improvement and natural looking-effect (Table 2). The first published cases showed for 2 subjects that PLLA is an effective option giving a natural looking effect for gluteal augmentation and the reduction of cellulite appearance.92 A recent randomized, double-blind, placebo-controlled clinical trial on 31 patients treated with PLLA (0.5–1 vial per session, 12mL/vial) combined with SubcisionTM in the buttocks and thighs, reported a significant GAIS improvement at 3 and 6 months post-treatment regarding cellulite appearance.97 In a study combining PLLA with SubcisionTM on 24 patients (buttocks, n=23) with a moderate-to-severe degree of cellulite according to Hexsel’s Cellulite Severity Scale,34 the SubcisionTM procedure was applied before the first session on the deep depressions in standing position and muscles relaxed, followed by PLLA treatment (0.5 to 1 vial per buttock per session, 12 mL/vial). Six to eight weeks later, a second PLLA injection was proposed only upon patient’s request. According to the GAIS assessed by 3 independent evaluators, 60% of the patients reached a great-to-excellent improvement with 92% of the patients satisfied or very satisfied.93
Table 2.
Published Efficacy/Safety Data and Protocols on PLLA in Buttocks
| Reference (Nb of Patients) | Design/Objectives | Efficacy | Safety | Reconstitution/Vial | Session/Patient | Injection Technique/Device | Nb Vial*** | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Volume/Time | Total Volume | Nb | Intervals (wks) | Per Session | Total | |||||
| Lorenc 201222 (NR) | Clinical practice | Effective gluteal augmentation (PA) | NR | 5 mL for > 2h + L1% | 12 mL | NR | 6 | Tunneling SC injection Needle or cannula 25G 1.5-in |
>2 | NR |
| Cunha et al 201695 (N=14) | Clinical practice Volume loss F-U: 6 months |
GAS: Improvement of the skin quality and laxity | Hematoma; no nodule formation | 9 mL for 48h + L | 11 mL | 2 | 6 | Injection in the deep dermis – superficial hypodermis | 2 | 4 |
| Mazzuco and Sadick 201692 (N=2) | Clinical practice Case report Skin laxity, volume loss, cellulite |
Effective gluteal augmentation (PA) | Mild bruising | 10 mL for 24h + L | 12 mL | 2–3 | 4 | Linear threading SC injection Needle 27G 1-in |
3–4 | 6–12 |
| Mazzuco et al 202094 (N=13 /45) | Clinical practice Body contour, skin laxity, cellulite, striae F-U: 2 months |
GAIS improvement (92.3–100%) | Pain during application and mild ecchymosis | 10 mL for 48–72h + L2% | 12 mL | 1–3 | 6–8 | Fanning injection Needle 26G½ or cannula 22G |
1/ 25 cm2 |
3–5 |
| Durairaj et al 202096 (N=52/60) | Retrospective clinical review Skin laxity, cellulite dimpling F-U: 20 weeks + 2 years |
GAIS improvement (skin/cellulite appearance) | Mild-moderate AE at the injection site (bruising, swelling, ecchymosis, soreness) | 5 mL for 24h | 10 mL | 1–3 | 4–6 | Cross-hatching injection in the SC deep dermis 21G needle |
1/ 24 cm2 2–12 |
4–42 |
| Sandoval 202099 (NR) | Technical publication Skin irregularities, volume loss F-U: 6 months |
Significant gluteal and skin quality improvement (PA) | No serious AE reported; transient bruising at injection sites | 8 mL for 24h + L2% | 20 mL | 2–3 | 4–6 | Linear threading or cross-hatching injection in SC deep dermis level Needle 26 G 1.5-in or 27G 1-in/cannula 22G |
NR | NR |
| Mazzuco 202093 (N=23/24) | Case series + SubcisionTM Cellulite, skin laxity F-U: 24 months |
60% of patients with GAIS 1–2 and 92% of patients satisfied/very satisfied 60 days post-treatment | Pain during procedure, transient bruising and ecchymosis | 10 mL for 48–96h + L2% | 12 mL | 1–3** | 6–8 | Injection in the superficial SC layer 26G ½ needle |
1–2 | <6 |
| Shridharani et al 202198 (N=16/20) | Clinical experience Volume loss, cellulite |
Improvement for 81.3% of patients (PA) | Bruising, oedema, tenderness, numbness; nodule (n=1) resolved spontaneously | 5–13 mL*for 2h + LEp1–2% | 10 mL (volume)/15 mL (cellulite) | 1–11 (2.5) | 4–24 | Linear threading or cross-hatching injection in the mid-to-deep dermis Needle 23–25 G 1.5-in |
1–40 (8) 7–15 mL |
25 |
| Swearingen et al 202196 (N=31) | Randomized, DB Placebo controlled + SubcisionTM Cellulite F-U: 6 months |
GAIS: Significant improvement 3- and 6-months post-treatment | No serious AE reported; bruising and erythema | 10 mL for 48–96h + L2% | 12 mL | 3 | 4 | Needle 26G ½ | 0.5–1 | 2–3 |
Notes: *Reconstitution in bacteriostatic water instead of sterile water for injection; **Combined with SubcisionTM for the first session; ***Left and right sides are counted separately.
Abbreviations: AE, adverse events; F-U, follow-up; GAIS, Global Aesthetic Improvement Scale with Grade 1, very much improved, Grade 2, much improved, Grade 3, improved, Grade 4, no change, Grade 5, worse; GAS, General appearance of the skin; NR, not reported; L, lidocaine; LEp, lidocaine +_i epinephrine; PA, Photographic assessment; SC, subcutaneous.
The results from 14 patients who received 2 PLLA treatments 6 weeks apart with 1 vial per buttock per session (10mL/vial) showed a high level of patient satisfaction with an 85% improvement for skin appearance and 71% for skin laxity.95 The amplitude of improvement was correlated with the number of PLLA vials administered. A retrospective clinical review including 60 patients showed that the best results with a GAIS of 1 (exceptional improvement) or 2 (very improved) was reached with 20 vials or more (10 vials/buttock side, 10mL/vial) whatever the age of the patient and the number of sessions.96 A study on 20 consecutive patients treated with PLLA (buttocks contouring, n=16; 4 vials/buttock side; volumization treatment, 10mL/vial; cellulite treatment 15mL/vial) reported that 81.3% of treatment sessions resulted in an improved volume and appearance of the buttocks.98
PLLA for buttock rejuvenation was generally well tolerated as associated with only mild transient adverse events localized at the injection sites, such as pain during procedure,93,95 hematoma/ecchymosis,95,96 edema,95,98 bruising92,96,98,99 and swelling.96 The main possible complications include asymmetry, contour irregularities, infection and necrosis, as recently described.73 A recent study reported one case of nodule in one patient that resolved spontaneously after 38 days.98 When combined to SubcisionTM, almost half of the patients reported mild-to-moderate hemosiderosis resolving within 3 months.93
PLLA is reconstituted in 10 to 20 mL of sterile water plus lidocaine 2h,98 24 h,92,96,99 48h95,97 to 72h94 or 96h93,97 before administration (Table 2). For volume augmentation treatments, a more concentrated preparation of PLLA can be used (10 mL per vial) and a more diluted one to treat cellulite (15 mL per vial).98 Depending on the patients’ demand, the number of treatments varies from 1 to 11, 4–24 weeks apart.93,94,96–98 The product should be injected preferentially in the superior and lateral quadrants of the buttocks avoiding the “danger triangle”,73 with a linear threading or fanning technique using a cannula or a needle.27,73,98 A recent publication reported a description of PLLA administration in the buttocks.73 Post-treatment massages must be done by the physician and compression bandage applied for two days.
PLLA and Abdomen
The appearance of the abdomen plays a major role in the silhouette. For women and men, it reflects a healthy lifestyle and condition, self-awareness and vitality.101 The abdomen has critical roles in the protection of the internal organs, breathing and movements of the body. The anterolateral abdominal wall consists of 4 successive layers: skin, fascia, muscles, and peritoneum. With aging, pregnancy, gain/loss of weight, the muscles and the abdominal skin lose their firmness. In the case of moderate-to-severe abdominal skin laxity, surgery (abdominoplasty and liposuction) is usually proposed.83 For patients with mild skin laxity, non-invasive strategies are available like radiofrequency, ultrasound, shock waves and cryolipolysis which have demonstrated their efficiency in dermal remodeling.102 Some results have been obtained with CaHA.12,103,104 PLLA was investigated in this body area, but data are also limited (Table 3).26,27,94,98,101
Table 3.
Published Efficacy/Safety Data and Protocols on PLLA in Abdomen
| Reference (Nb of Patients) | Design/Objectives | Efficacy | Safety | Reconstitution/Vial | Session/Patient | Injection Technique/Device | Nb Vial | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Volume/Time | Total Volume | Nb | Intervals (wks) | Per Session | Total | |||||
| Mazzuco et al 202094 (N=6/45) | Case study Skin laxity, striae F-U: 2 months |
GAIS: improvement of 83.3–100% (PA) | Pain during application, mild ecchymosis, no nodule | 10 mL/48–72h + L2% | 12 mL | 1–3 | 6–8 | Fanning injection in small bolus in the superficial cutaneous layer Needle 26G ½ or cannula 22G |
1/ 25 cm2 |
1–3 |
| Sadick & Arruda 2017101 (N=5) | Case study Skin quality and texture, laxity F-U: 12 months |
PA: Improvement of abdominal contouring, skin laxity and quality High level of patients’ satisfaction |
Mild bruising at the injection sites, no serious AE reported | 10 mL/24h + L* | 12 mL | 1–2 | 3 | Retrograde linear threading injection in the superficial layer of the SC tissue (deep dermis) Needle 27G 1-in |
1–2 | 2–4 |
| Shridharani et al 202198 (N=3/20) | Clinical practice Skin laxity |
PA: improvement for 77.8% of patients | Bruising, oedema, tenderness and numbness, nodule (n=1) resolved spontaneously | 5–13 mL + LEp | 10–15 mL | 1–4 | 13–14 | Linear threading or cross-hatching injection in the deep dermal or subdermal planes Needle 23G–25G 1.5-in |
mean 1.6 (10–15 mL) | 8 |
Note: *% Lidocaine not reported.
Abbreviations: AE, adverse events; F-U, follow-up; GAIS, Global Aesthetic Improvement Scale with Grade 1, very much improved, Grade 2, much improved, Grade 3, improved, Grade 4, no change, Grade 5, worse; L, Lidocaine; LEp, lidocaine + epinephrine; PA, photographic assessment; wks, weeks; SC, subcutaneous.
A case study on women younger than 50 years who received 1 to 3 sessions showed a long-lasting visible improvement of the skin quality and texture, abdominal laxity and contour, more than 12 months post PLLA administration, and a high level of patient satisfaction.101 In another study, PLLA treatment resulted in a GAIS improvement in more than 90% of the patients treated in this area (n=6).94 PLLA demonstrated a good safety profile with no serious adverse events reported.94,101
PLLA is resuspended in 8 to 10 mL of sterile water 2h to 72h before administration with lidocaine (Table 3).94,98,101 The product was injected subcutaneously at the level of the mid-to-deep dermis, radially around the umbilicus using a threading,98 retrograde manner101 or fanning technique94,98 with a needle or a cannula.27
PLLA and Limbs
Medial Upper Arms
The arms are also affected by aging. The epidermis, dermis, and subcutaneous fat are particularly thin in the medial upper arm and a hanging skin can appear (beating bat wings).105 Different techniques exist to correct skin laxity or localized fat such as cryolipolysis,106,107 radiofrequency or laser treatments.108,109 Injectable biostimulatory fillers are of potential value to treat this area for their ability to stimulate dermal remodeling while increasing skin tightening such as CaHA10,12,103,104,110 and PLLA.26,27,111,112
PLLA demonstrated its efficacy for the treatment of the medial upper arms (Table 4). PLLA treatment is associated with an improvement of the skin 4 weeks after the first application with a reduction in sagging of the skin and cellulite appearance of the arm (5mL/arm, 6mL/vial).111 Mazzuco et al showed a considerable improvement of the GAIS from 89.9% to 100%, depending on the evaluator, and a high level of patient satisfaction in a study on 9 subjects, two months after treatment for arm skin laxity including 2 subjects with cellulite, in a group of 45 women treated in different body areas (0.5 vial/arm; 10mL/vial).94 PLLA has a good safety profile with self-limited pain during injection and transient mild ecchymosis.94,111 No early nodules or late granulomas were reported.94
Table 4.
Published Efficacy/Safety Data and Protocols on PLLA in Limbs
| Reference (Nb of Patients) | Design/Objectives | Efficacy | Safety | Reconstitution/Vial | Session/Patient | Injection Technique/Device | Nb Vial | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Volume/Time | Total Volume | Nb | Intervals (wks) | Per Session | Total | |||||
| MEDIAL UPPER ARM | ||||||||||
| Mazzuco et al 202094 (n=9/45) | Case study Laxity, cellulite F-U: 2 months |
GAIS: improvement of 88.9–100%; All patients satisfied/very satisfied | Well-tolerated pain during/after application, mild ecchymosis | 10 mL for 48–72h + L2% | 12 mL | 1–3 | 6–8 | Fanning injection Needle 26G ½ or cannula 22G |
0.5 | 1–3 |
| Coimbra & Gutstein da Fonseca A 2012;111 Coimbra & Stefanello 2020112 (n=22) | Clinical practice111/method description110 Laxity, cellulite |
PA: Skin improvement 4 weeks after the 1st session and better after the 2nd; Effect maintained >22 months | Pain during application, local erythema, transient hematoma | 8 mL for 24–36h + L2% then 12 mL aqueous solution | 20 mL | 2–4 | 4 | Linear retrograde injection into the deep dermis or SC layer | 0.5 | 1–2 |
| THIGHS | ||||||||||
| Mazzuco et al 202094 (n=17/45) | Case study Laxity, cellulite FU: 2 months |
GAIS: improvement >81.3% | Pain during application and mild ecchymosis | 10 mL for 48–72h + L2% | 12 mL | 1–3 | 6–8 | Fanning injection Needle 26G ½ or cannula 22G |
0.5 | 1–3 |
| Mazzuco 202093 (n=5/24) | Case study PLLA + SubcisionTM Cellulite-associated skin flaccidity F-U: 2-year |
GAIS score improvement: 1 (n=3) and 2 (n=2); 92% of patients satisfied 60 days post-treatment | Pain during procedure, transient bruising and ecchymosis | 10 mL for 48–96h + L2% | 12 mL | 1–3** | 6–8 | Injection in the superficial SC layer Needle 26G ½ |
1–2 | <6 |
| Shridharani et al 202198 (n=4/20) | Clinical experience Cellulite, skin laxity |
PA: improvement in 100% of patients | Bruising, oedema, tenderness and numbness, nodule (n=1) resolved spontaneously | 8 mL for 2h + L2% | 10–15 mL | 2–13 | 4–12 | Linear threading or cross-hatching injection in deep dermal/subdermal planes Needle 23G–25G 1.5-in |
1–9 (median 4) | 12 |
| Swearingen et al 202197 (n=31) | Randomized, DB, Placebo controlled study Cellulite F-U: 6 months |
Standardized photographs (VISIA): Significant GAIS improvement 3- and 6-months post-treatment | No serious AE reported; only injection site reactions (bruising, erythema) resolving in 2 weeks |
10 mL for 48–96h + L2% | 12 mL | 3 | 4 | Needle 26G ½ | 0.5–1 | 2–3 |
| KNEES | ||||||||||
| Machado Costa & Mesquita 2019118 (n=3) | Case series Skin laxity |
PA: Increase of skin thickness/sagging skin | Safe | 8 mL for 24h + L* | 10 mL | 3 | 4 | Retrograde SC injection Needle 26G |
1 | 3 |
| Kollipara et al 2020119 (n=20) | Randomized, split body, placebo controlled study Skin laxity F-U: 6 months |
Standard 2D- and Vectra 3-D photographs: PGAIS improvement vs placebo at day 28 (p<0.05), sustained at days 84/168 | Well-tolerated without any significant AE; no significant difference vs placebo at 6 months | 14 mL, incubation time NR + L1% | 16 mL | 3 | 4 | Retrograde fanning injection Needle 25G 1.5-in |
1 | 3 |
| Shridharani et al 202198 (n=3/20) | Clinical experience Skin laxity |
PA: improvement in 66.7% of patients | Bruising, oedema, tenderness and numbness, nodule (n=1) resolved spontaneously | 8 mL for 2h + L2% | 10 mL | 1–2 | 7 | Linear threading or cross-hatching injection in deep dermal/subdermal planes Needle 23–25G 1.5-in |
4–6 (median 6) | 9 |
Note: NR, not reported; *% of L not reported; **Combined with SubcisionTM.
Abbreviations: AE, adverse event; F-U, follow-up; GAIS, Global Aesthetic Improvement Scale with Grade 1, very much improved, Grade 2, much improved, Grade 3, improved, Grade 4, no change, Grade 5, worse; NR, not reported; PA, photographic assessment; PGAIS, Physician Global Aesthetic Improvement Scale; SC, subcutaneous.
PLLA is injected subcutaneously in the medial branchial area of the arm. A method of PLLA injection for the arms has been described in detail.112 The volume injected has increased in parallel with experience in using the product from 5 mL in 2012111 to 8 mL and more in 2020 per arm per session (Table 4).26,94,112 The injection technique commonly used is the linear threading technique.26,111,112 Subcutaneous injection can be performed with a 25G, 2.5-inch cannula,26 a 26G½ needle or 22G cannula.94 An average of 2 to 3 sessions is recommended, 4 to 8-weeks apart.
Thighs
Thighs, with their immediate proximity to the gluteal and abdomen areas, are important in the appearance of both the posterior and anterior regions. Ideal legs have been characterized as wider thighs with greater horizontal projection.113 With aging and weight loss, changes in fat distribution and loss of collagen also affect the thighs resulting in skin flaccidity and cellulite/striae appearance.
Surgery is being used to lift thighs.83,114 The use of collagen stimulators is increasing. One study included subjects treated with CaHA for thighs among other areas.103 Few studies have been published on PLLA, but its properties make it an interesting option for treating the thighs (Table 4).27,93,94,97,98
A case-study on 17 out of 45 patients with skin laxity and cellulite appearance of the thighs treated with PLLA was associated with a GAIS improvement higher than 81.3% with all patients satisfied (1 vial/session; 10mL/vial). The benefit appeared 6–8 weeks post-treatment and for up to 2 years.94 A prospective study of 4 out 20 patients treated with PLLA in clinical practice showed an improvement of 100% after a median number of 3 sessions/patient (4 vials/session; 7–15mL/vial).98 A very recent randomized double-blind, placebo-controlled clinical trial in 31 patients who received 3 treatments every 4 weeks reported a significant improvement of cellulite appearance at 3 and 6 months post-treatment (0.5–1 vial/thigh; 10mL/vial).97 A study based on the author’s experience was dedicated to the use of SubcisionTM in combination with PLLA (0.5–1 vial/thigh; 10mL/vial) in the treatment of cellulite associated with flaccidity in the thighs and buttocks, SubcisionTM being recommended for the first session in case of cellulite. The study follow-up was 2 years. This combination of treatment provided beneficial and safe results, as indicated previously.93 In all studies, no nodule formation or granulomas was observed and pain was well tolerated by all the patients.93,94,97,98
PLLA is reconstituted in 8 mL,69 or 10 mL94,97 of sterile water plus lidocaine (Table 4). Incubation time varies from 2h,98 at least 12h69 to 48–96h before administration.94,97 The product should be injected in the subcutaneous layer in the anterior and medial regions, avoiding vasculature and muscle,27,112 with a 23-to 26 ½ needle or a 22 G cannula using a fanning technique. One to nine vials are used per session for a total of 1 to 3 sessions, 4 to 12 weeks apart.69,94,97,98
Knees
Skin laxity of the knee is increased with aging resulting in the formation of skin folds with sagging skin around the upper knees and has become of real concern for subjects seeking body improvement. Treating this area is a relatively new approach and few studies were conducted. Few minimally invasive options have been published like lipofilling,115 microfocused ultrasound,116 and more recently, collagen-stimulators such as CaHA10,117 and PLLA.98,118,119
PLLA to correct skin laxity of the knees was assessed in three recent studies using different techniques and reported to lead to an improvement of skin laxity and a significant increase of skin thickness associated with a favorable safety profile (Table 4).98,118,119 They concerned few cases treated for this condition98,118 although, interestingly a very recent randomized, double-blind, split-body placebo-controlled study was performed on 20 patients with mild-to-severe skin laxity, treated at the anterior upper knees.119 The results showed a statistically significant improvement versus placebo on the primary endpoint, the PGAIS (Physician Global Aesthetic Improvement Scale) from 28 days to 168 days after 3 treatment sessions (1 vial/session; 16mL/vial). The safety profile was favorable with only minor adverse events reported.119
All the studies used a relatively high volume of PLLA reconstitution ranging from 10 mL,98 13 mL118 to 16 mL,119 2–24h before administration (Table 4).98,118 The product was injected subcutaneously in the anterior upper knee with a 25–26G needle using a threading linear technique,118 or fanning technique.119 One to 4 vials were injected per session, for a total of 1–3 sessions, 4–7 weeks apart.98,118,119
PLLA and Hands
Hands, one of the most visible parts of the body, are affected by aging due to photodamage and environmental factors combined with the natural phenomenon of aging. The skin of the hands becomes thinner due to a loss of collagen and a decrease of skin density, leading to the formation of wrinkles. Subcutaneous fat loss, bone resorption and muscle atrophy are associated with thin and transparent skin and deep wrinkles, and prominent veins, tendons, and bones.120 Different aesthetic approaches exist to improve hand appearance. When seeking tissue cells renewal, the use of techniques or products such as topical agents, chemical peels, intense pulsed light, and lasers are indicated. Non-ablative lasers, radiofrequency and sclerotherapy can be proposed to increase hands remodeling.121,122 When addressing loss of volume in hands, several products such as autologous fat or HAs are often used. Collagen stimulators also occupy an important place; many studies evidenced the efficacity of PCL-based filler,123–125 CaHA that has FDA-approval for hand augmentation,121,126–130 and PLLA.22,26,69,131–136
PLLA induced a high level of patient satisfaction (Table 5).67,131,133 Efficacy was associated with an increased number of sessions and a higher reconstitution volume to treat the hands.68 Patients need a long follow-up to properly assess treatment efficacy as the production of PLLA-induced collagen needs time due to the biological process involved.133 It is really important not to overcorrect the hands.68 The efficacy of PLLA has been observed for up to 2 years post-treatment.121,132
Table 5.
Published Efficacy/Safety Data and Protocols on PLLA in Hands
| Reference (Nb of Patients) | Design/Objectives | Efficacy | Safety | Reconstitution/Vial | Treatment Sessions | Injection Technique/Device | Nb Vial | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Volume/Time | Total Volume | Nb | Intervals (wks) | Per Session | Total | |||||
| Redaelli 2006133 (N=27) | Clinical practice Volume loss F-U: 6–15 months |
DGS: 4 to 9 | Nodule formation (n=1) | 5 mL (session 1) or 6–8 mL for 12 h + C3% | 5.5– 9 mL |
3–6 | 4 (session 1–3)/12 | Linear threading SC injection Needle 25–27G |
1 | 3–6 |
| Sadick et al 2008131 (N=26) | Clinical practice Volume loss |
High level of patients’ satisfaction | Bruising, swelling, pain, itching; no nodule formation | 5–6 mL o/night + L1% | 8– 10 mL |
1–3 | 4–8 | Linear threading injection into the immediate subdermal plane Needle 25G 1.5-in |
1 | 3 |
| Fabi and Goldman 2012;132 Palm et al 201069 (N=8) | Clinical practice Volume loss |
Patients’ satisfaction: 63% of patients with good to excellent results | Nodule formation (n=1) | 5 mL o/night + L1% | 12 mL | 2–3 | 4 | Fanning injection in the SC tissue plane Needle 27G 1.5-in |
1 | 2–3 |
| Vleggaar 200667 (NR) | Clinical practice Skin laxity F-U: 4–6 weeks post-treatment |
95.1% of patient satisfied | No serious AE; ecchymosis, transient soreness | 4 mL, 30 min to o/night + L2% | 5 mL | NR | 4–6 | Tunneling injection in the deep dermal subcutaneous plane Device NR |
NR | NR |
Abbreviations: AE, adverse events; C, carbocain; DGS, Definitive Graduated Score (from 1–10 with 10 associated with the best results); L, lidocaine; NR, not reported; SC, subcutaneous.
No important side effects were reported. The use of PLLA was associated with only minor and short-term injection site reactions.131,133 Nodules formation occurred in studies using a 5 to 7 mL PLLA reconstitution volume,133,134 while none have been reported for higher reconstitution volume (8–10 mL).131 This risk has, however, drawn attention and has contributed to slow down the use of PLLA in this area with low reconstitution volume.
PLLA must be injected in the very thin subcutaneous layer of the hand dorsum, avoiding the muscles, tendons and veins.133,134 PLLA volume reconstitution varied between studies. One study proposed to use a high PLLA concentration during the first 3 sessions (dilution in 5 mL using 2 mL/hand/session) followed by PLLA at lower concentration for the subsequent sessions (dilution in 6–8 mL with 1.5 to 2 mL/hand/session).133 Usually, the PLLA reconstitution volume is the same throughout the treatment and increases from 4 mL,67 6 mL,68,134 8–10 mL,68,131,135 12 mL69,132 to 14 mL.22 Reconstituted PLLA was hydrated at least 2h131,134 to 12 h before injection,133 for a maximum of 72h.135 For most studies, the product is injected using a threading technique131,133–135 with a 25G,22,131,135 26G,68,134 27G68,69,132 or a cannula.22 One vial is used per session to treat both hands22,68,69,132 for a total number of sessions ranging from 1 to 3, 4 to 8 weeks apart.22,69,131–134 Practical treatment modalities have been published recently.136
Discussion
Collagen stimulators commonly used in face are now extended to multiple areas for the global rejuvenation of various body parts. In the body, some studies or case-series concern PCL,51,88,123–125,137 and CaHA,56–58,103,110,117,127 and their use in clinical practice is increasing. PMMA is also used in body treatment.17,89 This review focused on PLLA as the first and one of the most investigated collagen stimulator, particularly in body areas.
In most of the studies and in clinical practice, PLLA has shown high efficacy and patient satisfaction, but to reach the optimal effect, it is mandatory in aesthetic treatment for the physician to define the realistic target and expected outcome with the patient. It has been mentioned that patient can respond differently to PLLA treatment.24 The reason behind was evoked to be related to the variable response of the patient to collagen stimulation, a biological process that implicated a cascade of events, and to several factors as age, immune status, past treatment and past pathological medical history. The number of non-responders to PLLA is very low and globally, satisfaction is high.
In facial rejuvenation, PLLA has been used for years worldwide and in numerous clinical studies in multiple areas and indications, for volume augmentation, contouring, wrinkle correction, and HIV lipoatrophy.67,138 American and European recommendations were published in 2014 covering many aspects from reconstitution conditions to injection modalities, marking a turning point in clinical development.6,8 Since then several studies have been conducted and very recently, two clinical studies further evidenced the safety and efficacy of PLLA in different conditions of reconstitution and with different injection techniques.30,139
Body rejuvenation is challenging since the objectives and the procedures are specific of the treated area. Collagen-stimulators such as PLLA have shown their efficiency to improve volume, skin laxity, and cellulite appearance. In off facial applications, as shown in the present review, PLLA use has been progressively applied to many areas in clinical practice. Off-face applications started logically on the neck and chest as visible prolongations of the face, and on hands, first published in 2006,67 since these areas are most frequently affected by photoaging, and progressively on the buttocks22 and arms111 in 2012, the abdomen101 in 2017, the knees118 in 2019 and the thighs94 in 2020. All the published studies reviewed demonstrated the effectiveness of PLLA. They are mostly conducted on the neck and chest (10 studies) and the buttocks (9 studies). For the other parts, there were several published studies (abdomen, 3 studies; arms, 2 studies; thighs, 5 studies; knees, 3 studies, hands, 4 studies) which were mainly case reports or retrospective studies. The most recent ones were performed following higher standard protocols including a higher number of subjects94,96,97,119 and for some of them a placebo-controlled group.97,119 The targeted clinical signs favorably improved by the treatment were volume augmentation, body contouring, body reshaping, skin laxity, cellulite/dimples associated with sagging, as well as skin quality, localized atrophy after liposuction or lipoatrophy, striae distensae and scar improvement (Tables 1–5).
PLLA has a good safety profile, supported by many years of clinical practice worldwide, and a study among others, conducted on a large cohort of 4112 HIV patients in the treatment of facial lipoatrophy.140 The reported adverse reactions were generally minor and comparable to those observed with other injectables and resolved rapidly. However, nodules formation was reported early in its use; this adverse event occurred with a low reconstitution volume of 3 to 4 mL. Increasing the reconstitution volume was shown to improve safety134,141,142 and this was taken in account in the European and American recommendations on PLLA use.7,8 This went along with improved patient selection and injection modalities. To summarize, some practical means to avoid or limit nodule formation concern: a) the production preparation: reconstitution in sterile water for injection and good homogenization of the reconstituted product before administration; b) the volume of reconstitution: the reconstitution in higher volume was proposed and published in the American7 and the European8 PLLA experts’ recommendations; an improved safety and a decreased incidence of nodule formation were reached when PLLA was reconstituted in higher volume (7–9 mL with lidocaine versus 4–5 mL);142 and c) Hydration time: a hydration time up to 48–72 hours was related to suspension quality and safety, but very recently, immediate injection together with high volume of reconstitution showed to be safe and leading to low adverse events and nodule formation rates.30,139 These modifications consisting in immediate injection in high volume were finally approved by the FDA in 2021. The other practical means of key importance are: a) good selection of patients according to treatment aims; b) administration of the treatment by experienced and trained physicians; c) appropriate injection modalities (injection technique, depth of injection, volume injected according to the treated area and slow speed injection); d) to avoid overcorrection; and e) to proceed post-treatment massages.
In body treatment, data confirmed that PLLA is well tolerated, with each area possessing its own specificity. For example, possible complications at the gluteal level have been well described,73 highlighting the need for the physician to have very good knowledge of the anatomy of the treated area and good clinical experience. They also show the need to respect pre- and post-care procedures as well as optimal PLLA preparation and injection modalities.73
Combination treatment, one of several new trends in aesthetics, was shown to be beneficial in body treatment, particularly in the case of cellulite. It was also shown to improve skin quality and, more globally, various body conditions following PLLA treatment.51,54,143 The use of PLLA in cellulite and associated-striae distensae, in the buttocks and thighs, the areas most affected by these phenomena, has become frequent and is generally administered with SubcisionTM in the first session as a recommended practice.93 For optimal results, combination with other procedures such as radiofrequency, lasers and shock waves is recommended, bringing additional benefit particularly by increasing skin quality.54,102
Taken together, there is a range of evidence in support of PLLA efficacy and safety in body applications. However, there are several limitations. The use of PLLA is still today based more on the clinical experience of physicians than on large clinical studies. Indeed, body treatment was started individually by few pioneer physicians and is now commonly used in daily practice by an increasing number of physicians. Several case studies including few patients92,101,118 were published starting to render visible the opportunity to use PLLA in body areas. They were followed by some larger retrospective studies including sometimes the treatment of several facial and non-facial areas into the same study and often again including few subjects per area97,119 and variable designs especially regarding the reconstitution volume, the injected volume and the number of vials per treatment. Variable follow-up times, often short, do not allow determining the duration of action and the optimal conditions of the product use. Nowadays, the studies performed satisfy higher standards and include more patients.96 Very recent randomized placebo-controlled studies have emerged.97,119 The level of evidence can be drawn from the designs of the studies (Tables 1–4). As discussed above, several studies are case studies of level III/IV, retrospective studies of level II/III and few recent placebo-controlled randomized studies can be regarded as level I/II. In view of further supporting PLLA use in body, larger clinical studies should be initiated based on standardized study protocols, in larger population and targeting well-defined areas with fixed procedures including the volume of reconstitution and the injection technique. Efficacy and safety should be confirmed in these optimal conditions as well as duration of action of the treatment. Altogether, this will clarify the procedures of PLLA use and confirm the benefit of the treatment for the patient.
Interestingly, the development of body applications has stimulated clinical research, the set-up of methods for assessing quantitative effects and particularly assessment scales for the main signs as skin laxity,32,33,40,44,48 cellulite severity,37–39,41,42 cellulite dimple,34 wrinkles,35,36,49 volume,45,46 and striae distensae.43 The increasing interest in the body treatment approach is remarkably apparent due to the number of scales published in the recent past years from 2019 to 202132–34,37,38,40,43–45 for buttocks/thighs, abdomen and knees in addition to the well-established ones logically concerning the neck and chest, hands and cellulite from 2008 to 2016 (Figure 1).35,36,39,42,45,46,48,49,144 Recommendations6,8,27,100 and reviews26,73 provide information on practices. Research on implementation on the body has also accentuated the use of product dilution according to area treated and of higher volume injected for large and depressed areas. This is a current topic of interest that goes beyond body applications. Everything considered, there is still a need for established procedures and recommendations of use in the light of upcoming standardized clinical trials outcomes. New clinical studies are awaited to further support the use of PLLA in body rejuvenation and to determine its duration of action.
Conclusion
Both patients’ expectations and physicians’ challenges for body rejuvenation are increasing. PLLA, first developed to restore loss of volume and reshape the face, is now widely used for the body, mostly in clinical practice. It effectively increases volume, corrects laxity and improves contours, the quality of the skin and cellulite appearance in different body areas. PLLA has a good safety profile when used in the appropriate conditions. Although limited, the available data support the use of PLLA and point to the need for further investigations to establish the most optimal and safest treatment modalities for body applications.
Acknowledgments
A medical writing assistance was provided by Potentiel d’action, France.
Disclosure
The author is a consultant for Sinclair Pharma (London, UK) and reports no other conflicts of interest in this work.
References
- 1.American Society Plastic Surgeons. 2020 national plastic surgery statistics; 2020. Available from: https://www.plasticsurgery.org/news/plastic-surgery-statistics. Accessed May 23, 2022.
- 2.Wat H, Wu DC, Goldman MP. Noninvasive body contouring: a male perspective. Dermatol Clin. 2018;36(1):49–55. doi: 10.1016/j.det.2017.09.007 [DOI] [PubMed] [Google Scholar]
- 3.Wang JV, Akintilo L, Geronemus RG. Growth of cosmetic procedures in millennials: a 4.5-year clinical review. J Cosmet Dermatol. 2020;19(12):3210–3212. doi: 10.1111/jocd.13768 [DOI] [PubMed] [Google Scholar]
- 4.Christen MO, Vercesi F. Polycaprolactone: how a well-known and futuristic polymer has become an innovative collagen-stimulator in esthetics. Clin Cosmet Investig Dermatol. 2020;13:31–48. doi: 10.2147/CCID.S229054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim JA, Van Abel D. Neocollagenesis in human tissue injected with a polycaprolactone-based dermal filler. J Cosmet Laser Ther. 2015;17(2):99–101. doi: 10.3109/14764172.2014.968586 [DOI] [PubMed] [Google Scholar]
- 6.Vleggaar D, Fitzgerald R, Lorenc ZP, et al. Consensus recommendations on the use of injectable poly-L-lactic acid for facial and nonfacial volumization. JDD. 2014;13(4 Suppl):s44–51. [PubMed] [Google Scholar]
- 7.Vleggaar D, Fitzgerald R, Lorenc ZP. The need for consensus recommendations on the use of injectable poly-L-lactic acid for facial and nonfacial volumization. JDD. 2014;13(4 Suppl):s28. [PubMed] [Google Scholar]
- 8.Redaelli A, Rzany B, Eve L, et al. European expert recommendations on the use of injectable poly-L-lactic acid for facial rejuvenation. JDD. 2014;13(9):1057–1066. [PubMed] [Google Scholar]
- 9.Goldberg D, Guana A, Volk A, Daro-Kaftan E. Single-arm study for the characterization of human tissue response to injectable poly-L-lactic acid. Dermatol Surg. 2013;39(6):915–922. doi: 10.1111/dsu.12164 [DOI] [PubMed] [Google Scholar]
- 10.de Almeida AT, Figueredo V, da Cunha ALG, et al. Consensus recommendations for the use of hyperdiluted calcium hydroxyapatite (radiesse) as a face and body biostimulatory agent. Plast Reconstr Surg Glob Open. 2019;7(3):e2160. doi: 10.1097/GOX.0000000000002160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loghem JV, Yutskovskaya YA, Werschler WP. Calcium hydroxylapatite: over a decade of clinical experience. J Clin Aesthetic Dermatol. 2015;8(1):38–49. [PMC free article] [PubMed] [Google Scholar]
- 12.Goldie K, Peeters W, Alghoul M, et al. Global consensus guidelines for the injection of diluted and hyperdiluted calcium hydroxylapatite for skin tightening. Dermatol Surg. 2018;44(Suppl 1):S32–S41. doi: 10.1097/DSS.0000000000001685 [DOI] [PubMed] [Google Scholar]
- 13.Ahn CS, Rao BK. The life cycles and biological end pathways of dermal fillers. J Cosmet Dermatol. 2014;13(3):212–223. doi: 10.1111/jocd.12100 [DOI] [PubMed] [Google Scholar]
- 14.Narins RS, Baumann L, Brandt FS, et al. A randomized study of the efficacy and safety of injectable poly-L-lactic acid versus human-based collagen implant in the treatment of nasolabial fold wrinkles. J Am Acad Dermatol. 2010;62(3):448–462. doi: 10.1016/j.jaad.2009.07.040 [DOI] [PubMed] [Google Scholar]
- 15.Moers-Carpi M, Christen MO, Delmar H, Brun P, Bodokh I, Kestemont P. European multicenter prospective study evaluating long-term safety and efficacy of the polycaprolactone-based dermal filler in nasolabial fold correction. Dermatol Surg. 2021;47(7):960–965. doi: 10.1097/DSS.0000000000002978 [DOI] [PubMed] [Google Scholar]
- 16.Lin SL, Christen MO. Polycaprolactone-based dermal filler complications: a retrospective study of 1111 treatments. J Cosmet Dermatol. 2020;19(8):1907–1914. doi: 10.1111/jocd.13518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Serra MS. Polymethyl Methacrylate for the Body. In: Costa AD, editor. Minimally Invasive Aesthetic Procedures: A Guide for Dermatologists and Plastic Surgeons. Springer International Publishing; 2020:589–592. doi: 10.1007/978-3-319-78265-2_82 [DOI] [Google Scholar]
- 18.De Albuquerque GC. Fillers and collagen stimulator for body rejuvenation and cellulitis. In: Issa MCA, Tamura B, editors. Botulinum Toxins, Fillers and Related Substances. Clinical Approaches and Procedures in Cosmetic Dermatology. Springer International Publishing; 2017:1–7. doi: 10.1007/978-3-319-20253-2_27-1 [DOI] [Google Scholar]
- 19.Fitzgerald R, Bass LM, Goldberg DJ, Graivier MH, Lorenc ZP. Physiochemical characteristics of Poly-L-Lactic Acid (PLLA). Aesthet Surg J. 2018;38(suppl_1):S13–S17. doi: 10.1093/asj/sjy012 [DOI] [PubMed] [Google Scholar]
- 20.Herrmann JL, Hoffmann RK, Ward CE, Schulman JM, Grekin RC. Biochemistry, physiology, and tissue interactions of contemporary biodegradable injectable dermal fillers. Dermatol Surg. 2018;44(Suppl 1):S19–S31. doi: 10.1097/DSS.0000000000001582 [DOI] [PubMed] [Google Scholar]
- 21.Lacombe V. Sculptra: a stimulatory filler. Facial Plast Surg. 2009;25(2):95–99. doi: 10.1055/s-0029-1220648 [DOI] [PubMed] [Google Scholar]
- 22.Lorenc ZP. Techniques for the optimization of facial and nonfacial volumization with injectable poly-l-lactic acid. Aesthetic Plast Surg. 2012;36(5):1222–1229. doi: 10.1007/s00266-012-9920-3 [DOI] [PubMed] [Google Scholar]
- 23.Vleggaar D, Fitzgerald R, Lorenc ZP. Composition and mechanism of action of poly-L-lactic acid in soft tissue augmentation. JDD. 2014;13(4 Suppl):s29–31. [PubMed] [Google Scholar]
- 24.Bauer U, Graivier MH. Optimizing injectable poly-L-lactic acid administration for soft tissue augmentation: the rationale for three treatment sessions. Can J Plast Surg. 2011;19(3):e22–27. doi: 10.1177/229255031101900311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sickles CK, Nassereddin A, Gross GP. Poly-L-lactic acid. In: StatPearls. StatPearls Publishing; 2021. [PubMed] [Google Scholar]
- 26.Jabbar A, Arruda S, Sadick N. Off face usage of poly-L-lactic acid for body rejuvenation. JDD. 2017;16(5):489–494. [PubMed] [Google Scholar]
- 27.Haddad A, Menezes A, Guarnieri C, et al. Recommendations on the use of injectable poly-L-lactic acid for skin laxity in off-face areas. JDD. 2019;18(9):929–935. [PubMed] [Google Scholar]
- 28.Lin MJ, Dubin DP, Goldberg DJ, Khorasani H. Practices in the usage and reconstitution of poly-L-lactic acid. JDD. 2019;18(9):880–886. [PubMed] [Google Scholar]
- 29.Li CN, Wang CC, Huang CC, Wang HH, Hsu NJ, A novel, optimized method to accelerate the preparation of injectable poly-L-lactic acid by sonication. JDD. 2018;17(8):894–898. [PubMed] [Google Scholar]
- 30.Bravo BSF, de Carvalho RM. Safety in immediate reconstitution of poly-l-lactic acid for facial biostimulation treatment. J Cosmet Dermatol. 2020. doi: 10.1111/jocd.13597 [DOI] [PubMed] [Google Scholar]
- 31.Narins RS. Minimizing adverse events associated with poly-L-lactic acid injection. Dermatol Surg. 2008;34(Suppl 1):S100–104. doi: 10.1111/j.1524-4725.2008.34250.x [DOI] [PubMed] [Google Scholar]
- 32.Guida S, Spadafora M, Longhitano S, Pellacani G, Farnetani F. A validated photonumeric scale for the evaluation of neck skin laxity. Dermatol Surg. 2021;47(5):e188–e190. doi: 10.1097/DSS.0000000000002865 [DOI] [PubMed] [Google Scholar]
- 33.Kaminer MS, Casabona G, Peeters W, et al. Validated assessment scales for skin laxity on the posterior thighs, buttocks, anterior thighs, and knees in female patients. Dermatol Surg. 2019;45(Suppl 1):S12–S21. doi: 10.1097/DSS.0000000000001994 [DOI] [PubMed] [Google Scholar]
- 34.Hexsel D, Fabi SG, Sattler G, et al. Validated assessment scales for cellulite dimples on the buttocks and thighs in female patients. Dermatol Surg. 2019;45(Suppl 1):S2–S11. doi: 10.1097/DSS.0000000000001993 [DOI] [PubMed] [Google Scholar]
- 35.Landau M, Geister TL, Leibou L, et al. Validated assessment scales for décolleté wrinkling and pigmentation. Dermatol Surg. 2016;42(7):842–852. doi: 10.1097/DSS.0000000000000786 [DOI] [PubMed] [Google Scholar]
- 36.Fabi S, Bolton J, Goldman MP, Guiha I. The Fabi-Bolton chest wrinkle scale: a pilot validation study. J Cosmet Dermatol. 2012;11(3):229–234. doi: 10.1111/j.1473-2165.2012.00628.x [DOI] [PubMed] [Google Scholar]
- 37.Longhitano S, Galadari H, Cascini S, et al. A validated photonumeric cellulite severity scale for the area above the knees: the knee cellulite severity score. JEADV. 2020;34(9):2152–2155. doi: 10.1111/jdv.16269 [DOI] [PubMed] [Google Scholar]
- 38.Cohen JL, Sadick NS, Kirby MT, et al. Development and validation clinician and patient reported photonumeric scales to assess buttocks cellulite severity. Dermatol Surg. 2020;46(12):1628–1635. doi: 10.1097/DSS.0000000000002756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hexsel DM, Dal’Forno T, Hexsel CL. A validated photonumeric cellulite severity scale. JEADV. 2009;23(5):523–528. doi: 10.1111/j.1468-3083.2009.03101.x [DOI] [PubMed] [Google Scholar]
- 40.Tateo A, Siquier-Dameto G, Artzi O, et al. Development and validation of IBSA photographic scale for the assessment of neck laxity. Clin Cosmet Investig Dermatol. 2021;14:349–354. doi: 10.2147/CCID.S302860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Young VL, DiBernardo BE. Comparison of cellulite severity scales and imaging methods. Aesthet Surg J. 2021;41(6):NP521–NP537. doi: 10.1093/asj/sjaa226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.DiBernardo BE, Sasaki GH, Katz BE, Hunstad JP, Petti C, Burns AJ. A multicenter study for cellulite treatment using a 1440-nm Nd: YAG wavelength laser with side-firing fiber. Aesthet Surg J. 2016;36(3):335–343. doi: 10.1093/asj/sjv203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.de Freitas VMP, Miot HA, Miot LDB, et al. Development of a clinical scale to assess the severity of striae distensae. Skin Res Technol. 2021;27(4):627–631. doi: 10.1111/srt.12995 [DOI] [PubMed] [Google Scholar]
- 44.Cassuto D, Pellacani G, Tateo A, et al. Development and validation of IBSA photographic scale for the assessment of inner upper arm laxity. Clin Cosmet Investig Dermatol. 2021;14:1465–1471. doi: 10.2147/CCID.S317857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee JH, Choi YS, Park ES, et al. A novel photonumeric hand grading scale for hand rejuvenation. Arch Plast Surg. 2019;46(4):359–364. doi: 10.5999/aps.2019.00521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Carruthers A, Carruthers J, Hardas B, et al. A validated hand grading scale. Dermatol Surg. 2008;34(Suppl 2):S179–183. doi: 10.1111/j.1524-4725.2008.34368.x [DOI] [PubMed] [Google Scholar]
- 47.Jones D, Donofrio L, Hardas B, et al. Development and validation of a photonumeric scale for evaluation of volume deficit of the hand. Dermatol Surg. 2016;42(Suppl 1):S195–S202. doi: 10.1097/DSS.0000000000000850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sattler G, Carruthers A, Carruthers J, et al. Validated assessment scale for neck volume. Dermatol Surg. 2012;38(2 Spec No.):343–350. doi: 10.1111/j.1524-4725.2011.02253.x [DOI] [PubMed] [Google Scholar]
- 49.Jones D, Carruthers A, Hardas B, et al. Development and validation of a photonumeric scale for evaluation of transverse neck lines. Dermatol Surg. 2016;42(Suppl 1):S235–S242. doi: 10.1097/DSS.0000000000000851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vanaman M, Fabi SG. Décolletage: regional approaches with injectable fillers. Plast Reconstr Surg. 2015;136(5Suppl):276S–281S. doi: 10.1097/PRS.0000000000001832 [DOI] [PubMed] [Google Scholar]
- 51.de Melo F, Carrijo A, Hong K, et al. Minimally invasive aesthetic treatment of the face and neck using combinations of a PCL-based collagen stimulator, PLLA/PLGA suspension sutures, and cross-linked hyaluronic acid. Clin Cosmet Investig Dermatol. 2020;13:333–344. doi: 10.2147/CCID.S248280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Peterson JD, Goldman MP. Rejuvenation of the aging chest: a review and our experience. Dermatol Surg. 2011;37(5):555–571. doi: 10.1111/j.1524-4725.2011.01972.x [DOI] [PubMed] [Google Scholar]
- 53.Peterson JD, Kilmer SL. Three-dimensional rejuvenation of the décolletage. Dermatol Surg. 2016;42(Suppl 2):S101–S107. doi: 10.1097/DSS.0000000000000758 [DOI] [PubMed] [Google Scholar]
- 54.Vanaman M, Fabi SG, Cox SE. Neck rejuvenation using a combination approach: our experience and a review of the literature. Dermatol Surg. 2016;42(Suppl 2):S94–S100. doi: 10.1097/DSS.0000000000000699 [DOI] [PubMed] [Google Scholar]
- 55.Chao YY, Chiu HH, Howell DJ. A novel injection technique for horizontal neck lines correction using calcium hydroxylapatite. Dermatol Surg. 2011;37(10):1542–1545. doi: 10.1111/j.1524-4725.2011.02086.x [DOI] [PubMed] [Google Scholar]
- 56.Yutskovskaya YA, Kogan EA. Improved neocollagenesis and skin mechanical properties after injection of diluted calcium hydroxylapatite in the neck and décolletage: a pilot study. JDD. 2017;16(1):68–74. [PubMed] [Google Scholar]
- 57.Fabi SG, Alhaddad M, Boen M, Goldman M. Prospective clinical trial evaluating the long-term safety and efficacy of calcium hydroxylapatite for chest rejuvenation. JDD. 2021;20(5):534–537. doi: 10.36849/JDD.5680 [DOI] [PubMed] [Google Scholar]
- 58.Guida S, Longhitano S, Spadafora M, et al. Hyperdiluted calcium hydroxylapatite for the treatment of skin laxity of the neck. Dermatol Ther. 2021;34(5):e15090. doi: 10.1111/dth.15090 [DOI] [PubMed] [Google Scholar]
- 59.Casabona G, Nogueira Teixeira D. Microfocused ultrasound in combination with diluted calcium hydroxylapatite for improving skin laxity and the appearance of lines in the neck and décolletage. J Cosmet Dermatol. 2018;17(1):66–72. doi: 10.1111/jocd.12475 [DOI] [PubMed] [Google Scholar]
- 60.Hart DR, Fabi SG, White WM, Fitzgerald R, Goldman MP. Current concepts in the use of PLLA: clinical synergy noted with combined use of microfocused ultrasound and poly-L-lactic acid on the face, neck, and décolletage. Plast Reconstr Surg. 2015;136(5 Suppl):180S–187S. doi: 10.1097/PRS.0000000000001833 [DOI] [PubMed] [Google Scholar]
- 61.Mazzuco R, Hexsel D. Poly-L-lactic acid for neck and chest rejuvenation. Dermatol Surg. 2009;35(8):1228–1237. doi: 10.1111/j.1524-4725.2009.01217.x [DOI] [PubMed] [Google Scholar]
- 62.Zac RI, Da Costa A. Poly-L-lactic acid for the neck. In: Costa AD, editor. Minimally Invasive Aesthetic Procedures. Springer International Publishing; 2020:529–532. doi: 10.1007/978-3-319-78265-2_73 [DOI] [Google Scholar]
- 63.Bolton J, Fabi S, Peterson JD, Goldman MP. Poly-L-lactic acid for chest rejuvenation: a retrospective study of 28 cases using a 5-point chest wrinkle scale. Cosmet Dermatol. 2011;24(6):278–284. [Google Scholar]
- 64.Wilkerson EC, Goldberg DJ. Poly-L-lactic acid for the improvement of photodamage and rhytids of the décolletage. J Cosmet Dermatol. 2018;17(4):606–610. doi: 10.1111/jocd.12447 [DOI] [PubMed] [Google Scholar]
- 65.Schulman MR, Lipper J, Skolnik RA. Correction of chest wall deformity after implant-based breast reconstruction using poly-L-lactic acid (Sculptra). Breast J. 2008;14(1):92–96. doi: 10.1111/j.1524-4741.2007.00529.x [DOI] [PubMed] [Google Scholar]
- 66.Fabi SG. Fillers for the décolletage area. Pract Dermatol. 2015;42:29–40. [Google Scholar]
- 67.Vleggaar D. Soft-tissue augmentation and the role of poly-L-lactic acid. Plast Reconstr Surg. 2006;118(3 Suppl):46S–54S. doi: 10.1097/01.prs.0000234846.00139.74 [DOI] [PubMed] [Google Scholar]
- 68.Redaelli A, Forte R. Cosmetic use of polylactic acid: report of 568 patients. J Cosmet Dermatol. 2009;8(4):239–248. doi: 10.1111/j.1473-2165.2009.00459.x [DOI] [PubMed] [Google Scholar]
- 69.Palm MD, Woodhall KE, Butterwick KJ, Goldman MP. Cosmetic use of poly-l-lactic acid: a retrospective study of 130 patients. Dermatol Surg. 2010;36(2):161–170. doi: 10.1111/j.1524-4725.2009.01419.x [DOI] [PubMed] [Google Scholar]
- 70.ISAPS. Plastic surgery statistics | Global plastic surgery statistics. ISAPS. Available from: https://www.isaps.org/medical-professionals/isaps-global-statistics/. Accessed December 27, 2021. [Google Scholar]
- 71.Singh D. Universal allure of the hourglass figure: an evolutionary theory of female physical attractiveness. Clin Plast Surg. 2006;33(3):359–370. doi: 10.1016/j.cps.2006.05.007 [DOI] [PubMed] [Google Scholar]
- 72.Gonzalez R. Etiology, definition, and classification of gluteal ptosis. Aesthetic Plast Surg. 2006;30(3):320–326. doi: 10.1007/s00266-005-0051-y [DOI] [PubMed] [Google Scholar]
- 73.Lin MJ, Dubin DP, Khorasani H. Poly-L-lactic acid for minimally invasive gluteal augmentation. Dermatol Surg. 2020;46(3):386–394. doi: 10.1097/DSS.0000000000001967 [DOI] [PubMed] [Google Scholar]
- 74.Amore R, Amuso D, Leonardi V, et al. Treatment of dimpling from cellulite. Plast Reconstr Surg Glob Open. 2018;6(5):e1771. doi: 10.1097/GOX.0000000000001771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Whipple LA, Fournier CT, Heiman AJ, et al. The anatomical basis of cellulite dimple formation: an ultrasound-based examination. Plast Reconstr Surg. 2021;148(3):375e–381e. doi: 10.1097/PRS.0000000000008218 [DOI] [PubMed] [Google Scholar]
- 76.Sadick N. Treatment for cellulite. Int J Womens Dermatol. 2019;5(1):68–72. doi: 10.1016/j.ijwd.2018.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rosique RG, Rosique MJF. Augmentation gluteoplasty: a Brazilian perspective. Plast Reconstr Surg. 2018;142(4):910–919. doi: 10.1097/PRS.0000000000004809 [DOI] [PubMed] [Google Scholar]
- 78.Wong WW, Motakef S, Lin Y, Gupta SC. Redefining the ideal buttocks: a population analysis. Plast Reconstr Surg. 2016;137(6):1739–1747. doi: 10.1097/PRS.0000000000002192 [DOI] [PubMed] [Google Scholar]
- 79.Nteli Chatzioglou G, Govsa F, Bicer A, Ozer MA, Pinar Y. Physical attractiveness: analysis of buttocks patterns for planning body contouring treatment. Surg Radiol Anat. 2019;41(1):133–140. doi: 10.1007/s00276-018-2083-4 [DOI] [PubMed] [Google Scholar]
- 80.Mendieta CG, Sood A. Classification system for gluteal evaluation: revisited. Clin Plast Surg. 2018;45(2):159–177. doi: 10.1016/j.cps.2017.12.013 [DOI] [PubMed] [Google Scholar]
- 81.Cuzalina A, Retana A. Creating the ideal buttock (lifting, implanting or fat grafting). In: Aguilera A, editor. The Art of Body Contouring. IntechOpen; 2019. doi: 10.5772/intechopen.84660 [DOI] [Google Scholar]
- 82.Toledo LS. Gluteal augmentation with fat grafting: the Brazilian buttock technique: 30 years’ experience. Clin Plast Surg. 2015;42(2):253–261. doi: 10.1016/j.cps.2014.12.004 [DOI] [PubMed] [Google Scholar]
- 83.Abboud M, Geeroms M, El Hajj H, Abboud N. Improving the female silhouette and gluteal projection: an anatomy-based, safe, and harmonious approach through liposuction, suspension loops, and moderate lipofilling. Aesthet Surg J. 2021;41(4):474–489. doi: 10.1093/asj/sjaa157 [DOI] [PubMed] [Google Scholar]
- 84.Oranges CM, Tremp M, Di Summa PG, et al. Gluteal augmentation techniques: a comprehensive literature review. Aesthet Surg J. 2017;37(5):560–569. doi: 10.1093/asj/sjw240 [DOI] [PubMed] [Google Scholar]
- 85.Mofid MM, Teitelbaum S, Suissa D, et al. Report on mortality from gluteal fat grafting: recommendations from the ASERF task force. Aesthet Surg J. 2017;37(7):796–806. doi: 10.1093/asj/sjx004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Friedmann DP, Vick GL, Mishra V. Cellulite: a review with a focus on subcision. Clin Cosmet Investig Dermatol. 2017;10:17–23. doi: 10.2147/CCID.S95830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hexsel DM, Mazzuco R. Subcision: a treatment for cellulite. Int J Dermatol. 2000;39(7):539–544. doi: 10.1046/j.1365-4362.2000.00020.x [DOI] [PubMed] [Google Scholar]
- 88.Santaella-Sosa E. Gluteal projection and augmentation using polycaprolactone-based filler: a promising new indication. J Aesthetic Nurs. 2020;9(6):229–232. doi: 10.12968/joan.2020.9.6.229 [DOI] [Google Scholar]
- 89.Chacur R, Menezes HS, Chacur NMBDS, et al. Gluteal augmentation with polymethyl methacrylate: a 10-year cohort study. Plast Reconstr Surg Glob Open. 2019;7(5):e2193. doi: 10.1097/GOX.0000000000002193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Logas C, Kosche C, Perez M, Martinez-Diaz GJ. Biostimulatory injectables for the treatment of cellulite and gluteal enhancement. Plast Surg Mod Tech. 2018;5(4). doi: 10.29011/2577-1701.100042 [DOI] [Google Scholar]
- 91.Davis DS, Boen M, Fabi SG. Cellulite: patient selection and combination treatments for optimal results-a review and our experience. Dermatol Surg. 2019;45(9):1171–1184. doi: 10.1097/DSS.0000000000001776 [DOI] [PubMed] [Google Scholar]
- 92.Mazzuco R, Sadick NS. The use of poly-L-lactic acid in the gluteal area. Dermatol Surg. 2016;42(3):441–443. doi: 10.1097/DSS.0000000000000632 [DOI] [PubMed] [Google Scholar]
- 93.Mazzuco R. SubcisionTM plus poly-l-lactic acid for the treatment of cellulite associated to flaccidity in the buttocks and thighs. J Cosmet Dermatol. 2020;19(5):1165–1171. doi: 10.1111/jocd.13364 [DOI] [PubMed] [Google Scholar]
- 94.Mazzuco R, Dal’Forno T, Hexsel D. Poly-L-lactic acid for nonfacial skin laxity. Dermatol Surg. 2020;46(Suppl 1):S86–S88. doi: 10.1097/DSS.0000000000002390 [DOI] [PubMed] [Google Scholar]
- 95.Cunha MG, da Daza F, Rezende FC, Machado Filho CDA. Poly-L-lactic acid injections in sagging body skin. Surg Cosmet Dermatol. 2016;8(4). doi: 10.5935/scd1984-8773.20168404 [DOI] [Google Scholar]
- 96.Durairaj KK, Devgan L, Lee A, et al. Poly-L-lactic acid for gluteal augmentation found to be safe and effective in retrospective clinical review of 60 patients. Dermatol Surg. 2020;46(Suppl 1):S46–S53. doi: 10.1097/DSS.0000000000002598 [DOI] [PubMed] [Google Scholar]
- 97.Swearingen A, Medrano K, Ferzli G, Sadick N, Arruda S. Randomized, double-blind, placebo-controlled study of poly-L-lactic acid for treatment of cellulite in the lower extremities. JDD. 2021;20(5):529–533. doi: 10.36849/JDD.5380 [DOI] [PubMed] [Google Scholar]
- 98.Shridharani SM, Tisch GM, Ebersole TG, Moak TN, Edwartz C. Clinical experience of poly-L-lactic acid injections for body contouring treatment. J Cosmet Dermatol. 2021;20:1655–1662. doi: 10.1111/jocd.14141 [DOI] [PubMed] [Google Scholar]
- 99.Sandoval MHL. Poly-L-lactic acid for the gluteal area. In: Costa AD, editor. Minimally Invasive Aesthetic Procedures: A Guide for Dermatologists and Plastic Surgeons. Springer International Publishing; 2020:543–547. doi: 10.1007/978-3-319-78265-2_76 [DOI] [Google Scholar]
- 100.Harper J, Avelar L, Haddad A, et al. Expert recommendations on the use of injectable poly-L-lactic acid for contour deficiencies of the buttocks. JDD. 2022;21(1):21–26. doi: 10.36849/JDD.2022.6180 [DOI] [PubMed] [Google Scholar]
- 101.Sadick NS, Arruda S. The use of poly-L-lactic acid in the abdominal area. Dermatol Surg. 2017;43(2):313–315. doi: 10.1097/DSS.0000000000000881 [DOI] [PubMed] [Google Scholar]
- 102.Jerdan K, Fabi S. A noninvasive approach to off-face skin laxity and tightening: a review of the literature. Semin Cutan Med Surg. 2015;34(3):118–128. doi: 10.12788/j.sder.2015.0173 [DOI] [PubMed] [Google Scholar]
- 103.Cogorno Wasylkowski V. Body vectoring technique with Radiesse(®) for tightening of the abdomen, thighs, and brachial zone. Clin Cosmet Investig Dermatol. 2015;8:267–273. doi: 10.2147/CCID.S75631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Lapatina NG, Pavlenko T. Diluted calcium hydroxylapatite for skin tightening of the upper arms and abdomen. JDD. 2017;16(9):900–906. [PubMed] [Google Scholar]
- 105.Teimourian B, Malekzadeh S. Rejuvenation of the upper arm. Plast Reconstr Surg. 1998;102(2):545–553. doi: 10.1097/00006534-199808000-00041 [DOI] [PubMed] [Google Scholar]
- 106.Lee SJ, Jang HW, Kim H, Suh DH, Ryu HJ. Non-invasive cryolipolysis to reduce subcutaneous fat in the arms. J Cosmet Laser Ther. 2016;18(3):126–129. doi: 10.3109/14764172.2015.1114644 [DOI] [PubMed] [Google Scholar]
- 107.Wanitphakdeedecha R, Sathaworawong A, Manuskiatti W. The efficacy of cryolipolysis treatment on arms and inner thighs. Lasers Med Sci. 2015;30(8):2165–2169. doi: 10.1007/s10103-015-1781-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.McKnight B, Tobin R, Kabir Y, Moy R. Improving upper arm skin laxity using a tripollar radiofrequency device. JDD. 2015;14(12):1463–1466. [PubMed] [Google Scholar]
- 109.Miotto G, Ortiz-Pomales Y. Arm contouring: review and current concepts. Aesthet Surg J. 2018;38(8):850–860. doi: 10.1093/asj/sjx218 [DOI] [PubMed] [Google Scholar]
- 110.Amselem M. Radiesse(®): a novel rejuvenation treatment for the upper arms. Clin Cosmet Investig Dermatol. 2016;9:9–14. doi: 10.2147/CCID.S93137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Coimbra D, Gutstein da Fonseca Amorim A. Poly-L-lactic acid in the rejuvenation of the medial and anterior arms. Surg Cosmet Dermatol. 2012;4(2):182–185. [Google Scholar]
- 112.Coimbra DD, Stefanello B. Poly-L-lactic acid for arms. In: Costa AD, editor. Minimally Invasive Aesthetic Procedures. Springer International Publishing; 2020:533–537. doi: 10.1007/978-3-319-78265-2_74 [DOI] [Google Scholar]
- 113.Vartanian E, Gould DJ, Hammoudeh ZS, Azadgoli B, Stevens WG, Macias LH. The ideal thigh: a crowdsourcing-based assessment of ideal thigh aesthetic and implications for gluteal fat grafting. Aesthet Surg J. 2018;38(8):861–869. doi: 10.1093/asj/sjx191 [DOI] [PubMed] [Google Scholar]
- 114.Michaels J. Vertical medial thigh contouring. Clin Plast Surg. 2019;46(1):91–103. doi: 10.1016/j.cps.2018.08.014 [DOI] [PubMed] [Google Scholar]
- 115.Okumus A. Combination of lipofilling with liposuction in the correction of pseudo genu varus deformity. Aesthet Surg J. 2020;40(3):NP94–NP100. doi: 10.1093/asj/sjz305 [DOI] [PubMed] [Google Scholar]
- 116.Gold MH, Sensing W, Biron J. Use of micro-focused ultrasound with visualization to lift and tighten lax knee skin (1.). J Cosmet Laser Ther. 2014;16(5):225–229. doi: 10.3109/14764172.2014.949273 [DOI] [PubMed] [Google Scholar]
- 117.Guida S, Longhitano S, Shaniko K, et al. Hyperdiluted calcium hydroxylapatite for skin laxity and cellulite of the skin above the knee: a pilot study. Dermatol Ther. 2020;33(6):e14076. doi: 10.1111/dth.14076 [DOI] [PubMed] [Google Scholar]
- 118.Machado Costa GR, Mesquita AC. Poly-L-lactic acid for the knee area skin laxity treatment; 2019. Available from: https://www.wcd2019milan-dl.org/abstract-book/documents/late-breaking-abstracts/03-aesthetic-cosmetic-dermatology/poly-l-lactic-acid-for-428.pdf. Accessed May 23, 2022.
- 119.Kollipara R, Hoss E, Boen M, Alhaddad M, Fabi SG, Randomized A. Split-body, placebo-controlled trial to evaluate the efficacy and safety of poly-L-lactic acid for the treatment of upper knee skin laxity. Dermatol Surg. 2020;46(12):1623–1627. doi: 10.1097/DSS.0000000000002685 [DOI] [PubMed] [Google Scholar]
- 120.Park JA, Lee SH, Hwang SJ, Koh KS, Song WC. Anatomic, histologic, and ultrasound analyses of the dorsum of the hand for volumetric rejuvenation. JPRAS. 2021;74(7):1615–1620. doi: 10.1016/j.bjps.2020.11.017 [DOI] [PubMed] [Google Scholar]
- 121.Butterwick K, Sadick N. Hand rejuvenation using a combination approach. Dermatol Surg. 2016;42(Suppl 2):S108–118. doi: 10.1097/DSS.0000000000000687 [DOI] [PubMed] [Google Scholar]
- 122.Shamban AT. Combination hand rejuvenation procedures. Aesthet Surg J. 2009;29(5):409–413. doi: 10.1016/j.asj.2009.08.003 [DOI] [PubMed] [Google Scholar]
- 123.Figueiredo VM. A five-patient prospective pilot study of a polycaprolactone based dermal filler for hand rejuvenation. J Cosmet Dermatol. 2013;12(1):73–77. doi: 10.1111/jocd.12020 [DOI] [PubMed] [Google Scholar]
- 124.Lowe NJ, Ghanem AM. Volume restoration of hands with polycaprolactone by cannula delivery; a prospective single center consecutive case series evaluation. J Cosmet Laser. 2020;22(2):55–59. doi: 10.1080/14764172.2019.1711127 [DOI] [PubMed] [Google Scholar]
- 125.de Melo F, Nicolau P, Piovano L, et al. Recommendations for volume augmentation and rejuvenation of the face and hands with the new generation polycaprolactone-based collagen stimulator (Ellansé®). Clin Cosmet Investig Dermatol. 2017;10:431–440. doi: 10.2147/CCID.S145195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kühne U, Imhof M. Treatment of the ageing hand with dermal fillers. J Cutan Aesthetic Surg. 2012;5(3):163–169. doi: 10.4103/0974-2077.101369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Goldman MP, Moradi A, Gold MH, et al. Calcium hydroxylapatite dermal filler for treatment of dorsal hand volume loss: results from a 12-month, multicenter, randomized, blinded trial. Dermatol Surg. 2018;44(1):75–83. doi: 10.1097/DSS.0000000000001203 [DOI] [PubMed] [Google Scholar]
- 128.Graivier MH, Lorenc ZP, Bass LM, Fitzgerald R, Goldberg DJ. Calcium hydroxyapatite (CaHA) indication for hand rejuvenation. Aesthet Surg J. 2018;38(suppl_1):S24–S28. doi: 10.1093/asj/sjy013 [DOI] [PubMed] [Google Scholar]
- 129.Haq S, Storck R, Baspeyras M, et al. Multinational, multipatient study of calcium hydroxylapatite for treatment of the aging hand: European cosmetic physician group on hand augmentation. Dermatol Surg. 2010;36(1):782–789. doi: 10.1111/j.1524-4725.2010.01548.x [DOI] [Google Scholar]
- 130.Edelson KL. Hand recontouring with calcium hydroxylapatite (Radiesse). J Cosmet Dermatol. 2009;8(1):44–51. doi: 10.1111/j.1473-2165.2009.00423.x [DOI] [PubMed] [Google Scholar]
- 131.Sadick NS, Anderson D, Werschler WP. Addressing volume loss in hand rejuvenation: a report of clinical experience. J Cosmet Laser Ther. 2008;10(4):237–241. doi: 10.1080/14764170802524429 [DOI] [PubMed] [Google Scholar]
- 132.Fabi SG, Goldman MP. Hand rejuvenation: a review and our experience. Dermatol Surg. 2012;38(7 Pt 2):1112–1127. doi: 10.1111/j.1524-4725.2011.02291.x [DOI] [PubMed] [Google Scholar]
- 133.Redaelli A. Cosmetic use of polylactic acid for hand rejuvenation: report on 27 patients. J Cosmet Dermatol. 2006;5(3):233–238. doi: 10.1111/j.1473-2165.2006.00259.x [DOI] [PubMed] [Google Scholar]
- 134.Sadick NS. Poly-L-lactic acid: a perspective from my practice. J Cosmet Dermatol. 2008;7(1):55–60. doi: 10.1111/j.1473-2165.2008.00362.x [DOI] [PubMed] [Google Scholar]
- 135.Atamoros FMP, Lozano AA. Poly-L-lactic acid for hands. In: Costa AD, editor. Minimally Invasive Aesthetic Procedures: A Guide for Dermatologists and Plastic Surgeons. Springer International Publishing; 2020:539–542. doi: 10.1007/978-3-319-78265-2_75 [DOI] [Google Scholar]
- 136.Da Costa A Minimally invasive aesthetic procedures: a guide for dermatologists and plastic surgeons. Springer International Publishing; 2020. Available from: https://books.google.fr/books?id=7aDSDwAAQBAJ. Accessed May 23, 2022. [Google Scholar]
- 137.Quezada Gaón N, Wortsman X, Apt P. Polycaprolactone for extrafacial areas. In: Costa AD, editor. Minimally Invasive Aesthetic Procedures: A Guide for Dermatologists and Plastic Surgeons. Springer International Publishing; 2020:565–573. doi: 10.1007/978-3-319-78265-2_79 [DOI] [Google Scholar]
- 138.Vleggaar D, Fitzgerald R, Lorenc ZP. The history behind the use of injectable poly-L-lactic acid for facial and nonfacial volumization: the positive impact of evolving methodology. JDD. 2014;13(4 Suppl):s32–34. [PubMed] [Google Scholar]
- 139.Palm M, Mayoral F, Rajani A, et al. Chart review presenting safety of injectable PLLA used with alternative reconstitution volume for facial treatments. JDD. 2021;20(1):118–122. doi: 10.36849/JDD.5631 [DOI] [PubMed] [Google Scholar]
- 140.Duracinsky M, Leclercq P, Herrmann S, Christen MO, et al. Safety of poly-L-lactic acid (New-Fill®) in the treatment of facial lipoatrophy: a large observational study among HIV-positive patients. BMC Infect Dis. 2014;14:474. doi: 10.1186/1471-2334-14-474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Lorenc ZP, Greene T, Gottschalk RW. Injectable poly-L-lactic acid: understanding its use in the current era. JDD. 2016;15(6):759–762. [PubMed] [Google Scholar]
- 142.Rossner F, Rossner M, Hartmann V, Erdmann R, Wiest LG, Rzany B. Decrease of reported adverse events to injectable polylactic acid after recommending an increased dilution: 8-year results from the Injectable Filler Safety study. J Cosmet Dermatol. 2009;8(1):14–18. doi: 10.1111/j.1473-2165.2009.00417.x [DOI] [PubMed] [Google Scholar]
- 143.Fabi SG, Burgess C, Carruthers A, et al. Consensus recommendations for combined aesthetic interventions using botulinum toxin, fillers, and microfocused ultrasound in the neck, décolletage, hands, and other areas of the body. Dermatol Surg. 2016;42(10):1199–1208. doi: 10.1097/DSS.0000000000000869 [DOI] [PubMed] [Google Scholar]
- 144.Cohen JL, Carruthers A, Jones DH, et al. A randomized, blinded study to validate the Merz hand grading scale for use in live assessments. Dermatol Surg. 2015;41(Suppl 1):S384–S388. doi: 10.1097/DSS.0000000000000553 [DOI] [PubMed] [Google Scholar]
- 145.Hexsel D, Valente-Bezerra I, Dal’Forno T, et al. Buttocks’ skin laxity severity scale. Dermatol Surg. 2022. doi: 10.1097/DSS.0000000000003434 [DOI] [PubMed] [Google Scholar]
- 146.Green JB, Pavicic T, Pooth R, et al. Validated 5 – point photonumeric scales for the assessment of hand atrophy. J Cosmet Dermatol. 2022;21:933–939. doi: 10.1111/jocd.14776 [DOI] [PubMed] [Google Scholar]