Abstract
Objective
To examine the effect of the pandemic on, and factors associated with, change in home care (HC) recipients’ capacity for instrumental activities of daily living.
Design
Retrospective cohort study.
Setting and participants
HC recipients in Ontario, Canada, between September 1, 2018, and August 31, 2020, who were not totally dependent on others and not severely cognitively impaired at baseline.
Methods
Data were collected with the interRAI Home Care assessment. Outcomes of interest were declines in instrumental activities of daily living. Factors hypothesized to be associated with declining function were entered as independent variables into multivariable generalized estimating equations, and results were expressed as odds ratios (ORs) with 95% confidence intervals (CIs). Those significant at P < .01 were retained in the final models.
Results
There were 6786 and 5019 HC recipients in the comparison and pandemic samples, respectively. Between baseline and follow-up for the 2 groups, 34.1% and 42.1% of HC recipients declined in shopping, whereas 25.2% and 30.5% declined in transportation capacity in the comparison and pandemic sample, respectively. For shopping, those with cognitive impairment (OR 0.83, 95% CI 0.76-0.89) and receiving formal care (OR 0.72, 95% CI 0.62-0.85) were less likely to decline, whereas those who were older (OR 1.91, 95% CI 1.69-2.16) and had unstable health (OR 1.31, 95% CI 1.16-1.48) were more likely. For transportation, those receiving informal (OR 0.71, 95% CI 0.61-0.81) or formal care (OR 0.56, 95% CI 0.47-0.67) were less likely to decline, whereas those who were older (OR 1.81, 95% CI 1.58-2.07) and had unstable health (OR 1.35, 95% CI 1.119-1.54) were more likely.
Conclusions and implications
The pandemic was associated with a decline in HC recipients’ capacity for shopping and transportation. HC recipients who are older and have unstable health may benefit from preventive strategies.
Keywords: Home care, pandemic, instrumental activities of daily living, COVID-19, interRAI
The COVID-19 pandemic resulted in widespread physical distancing and stay-at-home orders. Because of the increased risk of serious complications of COVID-19 for vulnerable older adults,1 restrictions were especially strict for Canadian home care (HC) recipients—those receiving formal personal support or professional services (eg, nursing, physical therapy, occupational therapy) for 60 days or more within their home.2 HC recipients tend to be older and live with complex health conditions.3
In Canada, there were reports of functional decline in older adults receiving community services during the pandemic because of interruptions to service provision,4 and many sources posit that physical distancing has led to decreased physical activity, further increasing the risk for functional decline.5, 6, 7 However, this has not been substantiated with empirical evidence for the HC population. Therefore, our study examines the effect of the pandemic on, and factors associated with, the change in instrumental activities of daily living (IADL) of HC recipients in Ontario, Canada.
Methods
Data for this retrospective study were obtained from the interRAI Home Care (HC) assessment. In Ontario, Canada, the interRAI HC is a valid and reliable8, 9, 10 assessment used by care coordinators (often nurses) as part of routine clinical practice to gather person-level data on HC recipients who are expected to require HC services for at least 2 months.8 It is completed on admission and every 6-12 months thereafter, or earlier if there is a significant health change. Assessments are typically completed in person; however, in April 2020, HC providers in Ontario temporarily completed many assessments virtually to minimize close contact with recipients.11
The comparison sample included all HC recipients with an interRAI HC assessment completed in the community between September 1, 2018, and February 28, 2019, and a follow-up completed in any setting (ie, community or hospital) between March 1, 2019, and August 31, 2019 (n = 26,492). The pandemic sample was constructed in the same way, but between September 1, 2019, and August 31, 2020 (n = 19,126). We chose to have the baseline assessment for the pandemic sample prior to March 2020 to be able to describe change that resulted between baseline and follow-up because of the onset of the pandemic. We restricted the first assessment to the community, as the characteristics of people receiving an assessment in hospital are different from those living at home (eg, to determine long-term care placement). We excluded all assessments completed in the Ontario Health West region because they chose to discontinue interRAI HC assessments during the first wave of the pandemic.
We excluded HC recipients whose IADL capacity at baseline was impaired such that further decline was unlikely (ie, maximal or total dependence) and those with severe cognitive impairment (ie, first assessment Cognitive Performance Scale score of ≥4) as IADL would likely be managed by informal or formal caregivers.
Outcomes of interest were capacity of HC recipients to complete IADL: meal preparation, ordinary housework, managing finances, managing medications, phone use, stairs, shopping, and transportation. Each item is scored 0 (independent) to 6 (total dependence). Capacity, defined as the presumed ability to carry out the activity as independently as possible, is judged by the assessor based on their observations and discussions with the individual. The interRAI HC is gathered by trained assessors who are most often nurses.12 For the IADL capacity items, they are instructed to question the person about his or her performance of normal activities around the home or in the community in the last 3 days.12 The assessors are also instructed to talk to family members if they are available. Finally, the assessors are instructed to use their own observations in the home environment as they gather information.12 Capacity is based on the assessor's data-informed speculation about what the person might be able to do for themselves based on demonstrated skills or physical attributes. In contrast, performance is the person's actual level of involvement in the activity and the type and amount of support actually received. Assessors are instructed to distinguish between nonperformance that is due to impairment of capacity (caused by health problems) and that due to other factors (not related to the person's health). We chose capacity rather than performance because we could not distinguish between declines in performance associated with fewer opportunities to perform the IADL (ie, stores being closed, people limiting outings to reduce the chance of contracting COVID) vs real changes in performance associated with physical function. In the context of the pandemic, performance would be limited for everyone because of public health measures (eg, closed stores) whereas capacity (eg, could they go out shopping if they had the opportunity) might not and would depend on their presumed ability to do so. Performance of an activity can also be confounded by shared task assignments (eg, partners sharing parts of IADL tasks) and societal norms as to who should perform the tasks (eg, meal preparation and housework). IADL capacity has been shown to be related to cognition, hours of informal and formal care, levels of exercise, being housebound, functional improvement, and long-term care admission.13, 14, 15 First, we examined the proportion of HC recipients whose IADL capacity declined between their 2 assessments in both samples. For IADL where there was a statistically significant difference, assessed via chi-square tests, between the proportion of HC recipients declining in the pandemic vs the comparison sample, we examined factors associated with decline. The outcomes examined were dichotomous—decline (yes/no) at the follow-up as compared to the baseline assessment.
The following independent variables were hypothesized to have a relationship with IADL capacity:
-
1.
Frailty: The interRAI HC Frailty Scale is a 29-item scale, scored from zero or no frailty markers to a maximum of 29.16 Within the newer version of the interRAI HC there are no variables for 2 of the original scale items: renal failure and loss of appetite. Thus, we constructed the scale to have 27 items and found it to be highly correlated with the 29-item scale (r = 0.989). The 27-item scale has not been validated in other studies to date.
-
2.
Health instability: The Changes in End-Stage Disease, Signs and Symptoms (CHESS) Scale measures the degree of health instability, scored from 0 (no instability) to 5 (severe instability).17
-
3.
Hearing and vision: The Deaf Blind Severity Index measures the degree of hearing and vision impairment, scored from 0 (no impairment in either sense) to 6 (severe impairment in both senses).18
-
4.
Functional abilities: The Activity of Daily Living Hierarchy Scale measures functional abilities in basic activities of daily living (eg, walking, dressing, grooming, toilet use, bed mobility), scored from 0 (no impairment) to 6 (severe impairment).13
-
5.
Cognition: The Cognitive Performance Scale measures cognitive abilities, scored from 0 (no impairment) to 6 (severe impairment).19
-
6.
Depression: The Depression Rating Scale measures depressive symptoms, scored from 0 to 14, where a score of 3 or higher suggests possible depression.20
Age, sex, selected health conditions that affect cognition, physical, and mental health (ie, dementia, congestive heart failure, Parkinson's disease, and bipolar disorder), whether the person lives alone, and their reported amount of time spent with other people through informal (eg, family and friends) and formal (eg, health care providers) care were also included.
We used frequency statistics and chi-square tests to compare the clinical characteristics of the 2 samples. All independent variables were entered into bivariate generalized estimating equation models. Final multivariate models were constructed by adding all variables to the model and retaining those significant at P < .01. Analyses were completed in SAS, version 9.4 (SAS Institute). This study received clearance from the research ethics board at the University of Waterloo and Dalhousie University.
Results
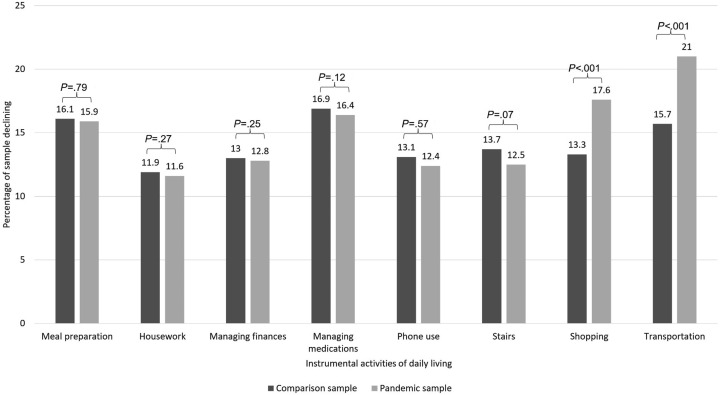
There were 6786 and 5019 HC recipients in the comparison and pandemic samples, respectively. Of these HC recipients, 887 (13.1%) were in both the comparison and the pandemic samples. Figure 1 shows the percentage of people declining in each IADL. The largest difference was observed in shopping and transportation; thus, we selected these outcomes to examine factors associated with decline. Table 1 describes the characteristics of the samples and presents the results of the bivariate and multivariate models for the 2 outcomes. A slightly higher percentage of HC recipients in the pandemic sample had unstable health, were cognitively impaired, and did not have depressive symptoms.
Fig. 1.
Percentage of home care clients experiencing decline in instrumental activities of daily living.
Table 1.
Sample Description and Univariate and Multivariate Model Results
| Characteristics | Sample Description |
Univariate and Multivariate Models |
||||
|---|---|---|---|---|---|---|
| Comparison Sample, n (%) (n = 6786) |
Pandemic Sample, n (%) (n = 5019) |
Shopping Decline |
Transportation Decline |
|||
| Univariate OR (95% CI) | Multivariate OR (95% CI) | Univariate OR (95% CI) | Multivariate OR (95% CI) | |||
| Pandemic (Ref.: no pandemic) | — | — | 1.44 (1.32-1.54) | 1.43 (1.33-1.55) | 1.31 (1.23-1.39) | 1.31 (1.21-1.42) |
| Age | ||||||
| 18-64 y | 1078 (15.9) | 829 (16.5) | Ref. | Ref. | Ref. | Ref. |
| 65-74 y | 1343 (19.8) | 956 (19.1) | 1.31 (1.15-1.49) | 1.30 (1.14-1.48) | 1.32 (1.18-1.48) | 1.34 (1.15-1.55) |
| 75-84 y | 2221 (32.7) | 1643 (32.7) | 1.54 (1.36-1.73) | 1.52 (1.34-1.72) | 1.57 (1.41-1.73) | 1.50 (1.31-1.72) |
| ≥85 y | 2144 (31.6) | 1590 (31.7) | 1.91 (1.70-2.15) | 1.91 (1.69-2.16) | 1.90 (1.71-2.10) | 1.81 (1.58-2.07) |
| Sex (Ref.: female) | 4239 (62.5) | 3170 (63.2) | 0.92 (0.85-1.00) | — | 0.97 (0.91-1.03) | — |
| InterRAI Home Care Frailty Scale | ||||||
| 0-6 (no to mild frailty) | 1741 (25.7) | 1228 (24.5) | Ref. | — | Ref. | — |
| 7-9 | 2119 (31.2) | 1604 (32.0) | 1.00 (0.91-1.11) | — | 1.05 (0.96-1.16) | — |
| 10-12 | 1732 (25.5) | 1323 (26.4) | 1.00 (0.90-1.11) | — | 0.99 (0.90-1.08) | — |
| 13-14 | 667 (9.8) | 518 (10.3) | 0.96 (0.83-1.10) | — | 0.91 (0.81-1.01) | — |
| 15-16 | 351 (5.2) | 239 (4.8) | 0.96 (0.80-1.15) | — | 0.95 (0.83-1.08) | — |
| 17-27 (severe frailty) | 176 (2.6) | 107 (2.1) | 0.80 (0.62-1.04) | — | 0.84 (0.72-0.99) | — |
| CHESS Scale | ||||||
| 0 (no instability) | 1375 (20.3)∗ | 909 (18.1)∗ | Ref. | Ref. | Ref. | Ref. |
| 1-2 (mild instability) | 3962 (58.4)∗ | 2963 (59.0)∗ | 1.03 (0.93-1.13) | 1.01 (0.92-1.12) | 1.11 (1.02-1.21) | 1.09 (0.97-1.20) |
| 3+ (moderate to severe instability) | 1449 (21.4)∗ | 1147 (22.9)∗ | 1.34 (1.19-1.51) | 1.31 (1.16-1.48) | 1.33 (1.21-1.46) | 1.40 (1.24-1.60) |
| Deaf Blind Severity Index | ||||||
| 0 (none) | 2563 (37.8) | 1836 (36.6) | Ref. | — | Ref. | — |
| 1-2 (mild) | 2723 (40.1) | 2057 (41.0) | 1.11 (1.01-1.20) | — | 1.13 (1.05-1.21) | — |
| 3+ (moderate to severe) | 1499 (22.1) | 1126 (22.4) | 1.19 (1.08-1.32) | — | 1.16 (1.07-1.25) | — |
| Activity of Daily Living Hierarchy Scale | ||||||
| 0 (no impairment) | 1896 (27.9) | 1317 (26.2) | Ref. | — | Ref. | — |
| 1-2 (mild impairment) | 1563 (23.0) | 1216 (24.2) | 0.88 (0.81-0.86) | — | 1.02 (0.93-1.12) | — |
| 3-4 (moderate impairment) | 2778 (40.9) | 2059 (41.0) | 0.96 (0.86-1.07) | — | 1.28 (1.14-1.43) | — |
| 5-6 (severe impairment) | 549 (8.1) | 427 (8.5) | 0.85 (0.69-1.03) | — | 1.29 (1.05-1.59) | — |
| Cognitive Performance Scale | ||||||
| 0-1 (no to mild impairment) | 2633 (38.8)∗ | 1823 (36.3)∗ | Ref. | Ref. | Ref. | — |
| 2-3 (mild to moderate impairment) | 4153 (61.2)∗ | 3196 (63.7)∗ | 0.92 (0.85-1.00) | 0.83 (0.76-0.89) | 0.93 (0.87-0.99) | — |
| Depression Rating Scale | ||||||
| 0 (none) | 3525 (52.0)∗ | 2683 (53.5)∗ | Ref. | — | Ref. | — |
| 1-2 (mild) | 1878 (27.7)∗ | 1439 (28.7)∗ | 0.98 (0.90-1.08) | — | 0.97 (0.91-1.05) | — |
| ≥3 (moderate) | 1383 (20.4)∗ | 897 (17.9)∗ | 0.95 (0.86-1.05) | — | 0.97 (0.90-1.06) | — |
| Dementia | 1423 (21.0) | 1034 (20.6) | 1.19 (1.09-1.31) | — | 1.23 (1.15-1.32) | — |
| Congestive Heart Failure | 868 (12.8) | 623 (12.4) | 0.98 (0.88-1.10) | — | 0.96 (0.87-1.05) | — |
| Parkinson's disease | 306 (4.5) | 204 (4.1) | 1.22 (1.02-1.47) | — | 1.23 (1.07-1.40) | — |
| Bipolar disorder | 153 (2.3) | 128 (2.6) | 0.72 (0.56-0.94) | — | 0.73 (0.59-0.92) | — |
| Lives alone | 3609 (53.2) | 2677 (53.3) | 0.90 (0.83-0.97) | — | 1.00 (0.94-1.06) | — |
| Informal care | ||||||
| 0-10 h | 5743 (84.6) | 4304 (85.8) | Ref. | — | Ref. | Ref. |
| 10-20 h | 781 (11.5) | 569 (11.3) | 0.98 (0.87-1.11) | — | 0.88 (0.81-0.95) | 0.71 (0.61-0.81) |
| ≥20 h | 262 (3.9) | 146 (2.9) | 1.16 (0.95-1.43) | — | 0.98 (0.87-1.10) | 0.93 (0.73-1.18) |
| Formal hours | ||||||
| 0-100 min | 3404 (50.2) | 2543 (50.7) | Ref. | Ref. | Ref. | Ref. |
| 100-500 min | 2850 (42.0) | 2131 (42.5) | 0.74 (0.68-0.80) | 0.77 (0.71-0.83) | 0.73 (0.68-0.77) | 0.63 (0.57-0.68) |
| ≥500 min | 532 (7.8) | 345 (6.9) | 0.63 (0.54-0.74) | 0.72 (0.62-0.85) | 0.69 (0.62-0.77) | 0.57 (0.47-0.68) |
OR, odds ratio.
Variables not retained in the model are indicated by dashes.
χ2P < .01.
The pandemic period was associated with higher odds of both shopping and transportation decline. In the final multivariate model, HC recipients who were older and had health instability had higher odds of declining in shopping capacity whereas those with cognitive impairment and receiving formal care had lower odds. Likewise, being older and having health instability was associated with higher odds of declining transportation capacity whereas receiving informal and formal care was associated with lower odds.
Discussion
Our study found that the pandemic was associated with a decline in the capacity of HC recipients for shopping and transportation after adjusting for a large range of functional, cognitive, and medical covariates. Individuals with cognitive impairment and receiving informal and formal care were less likely to decline, whereas those who were older and had unstable health and functional impairment were more likely.
A critical dimension of this research is that we show that capacity for shopping and transportation IADL declined whereas HC recipients faced the same access constraints as the entire population. Capacity refers to the presumed ability of the HC recipient to complete the activity, whereas performance describes what the person actually did. During the pandemic, most people limited their movement to within the community. As such, most faced decreases in their performance of shopping and transportation. However, our study reveals decreased capacity for these activities, indicating that the perceived ability of the HC recipient to complete the tasks decreased. These results could indicate perceived loss of function and cognition to independently complete these activities by the HC recipient, family members, and caregivers. HC recipients’ perceived loss of function could be due to not having as much opportunity to engage in these activities because of physical distancing measures, thus making them feel uncertain that they could complete it independently. In contrast, HC recipients would have continued to have the opportunity to engage in the other IADL (eg, managing finances and medications, housework), which is why we may not see differences in the proportion declining in those activities. Alternatively, perceived loss of function could be related to an increased sedentary lifestyle, or HC recipients contracting COVID and seeming more functionally impaired.
Functional loss typically follows a distinct progression, whereby people lose their ability to perform IADL followed by basic activities of daily living (eg, dressing, personal hygiene, walking).21 In the first wave of the pandemic, we observed negative changes in shopping and transportation capacity. Our results are from early in the pandemic, and if functional decline continues through subsequent waves, we may see decline in other IADL and basic ADL. Functional decline is important to prevent as it is associated with increased institutionalization and risk of mortality.22 Strategies that improve movement and physical activity, such as physical and occupational therapy programs,23 , 24 are necessary to prevent further functional decline. Our work suggests HC recipients being older and having unstable health may be the biggest benefactors of these strategies. We found that HC recipients with mild to moderate cognitive impairment were less likely to decline in their capacity for shopping than those without. The observed relationship may be because HC recipients with mild to moderate cognitive impairment may not have been completing these IADL independently at baseline. Although we attempted to account for this issue by limiting our sample to those without moderate to severe cognitive impairment, it could be that even those with mild to moderate cognitive impairment had less opportunity for decline. This issue should be examined further in future work.
A strength of our study is we had a comparison sample from the year prior to the pandemic, allowing for comparison of functional decline that normally occurs for people receiving HC with that of pandemic-associated functional decline. We did, however, observe small differences in our 2 samples, which has been found in other work by our group.25 We cannot be certain if these small differences were observed because of prioritization of complex HC recipients or real change in health status of the population. Furthermore, the different modes of assessment between the 2 groups could have biased our results, with some assessments being completed virtually during the pandemic, limiting the amount of visual and sensory information available to the assessor. Specifically, assessments not completed in person could have relied more heavily on HC recipients' or their caregivers’ perceptions of their capacity, which could differ from the perceptions of a trained assessor. Finally, given some HC recipients were in both the pandemic and comparison samples, the observed differences may be because of sample aging. However, only 13.1% of the sample overlapped between the 2 groups, so this effect may be small.
Conclusions and Implications
In conclusion, the pandemic was associated with a decline in capacity of HC recipients for shopping and transportation. HC recipients who are older and had unstable health were more likely to decline and could benefit from preventive strategies specifically designed for this group.
Acknowledgments
This research was supported through funding from the Ontario Ministry of Health and the New Frontiers Research Fund. We also gratefully acknowledge the technical support of Ontario Health related to preparation of the study data. All views expressed are those of the coauthors.
Footnotes
This study was funded by the Ontario Ministry of Health.
The authors declare no conflicts of interest.
References
- 1.Levin A.T., Hanage W.P., Owusu-Boaitey N., Cochran K.B., Walsh S.P., Meyerowitz-Katz G. Assessing the age specificity of infection fatality rates for COVID-19: systematic review, meta-analysis, and public policy implications. Eur J Epidemiol. 2020;35:1123–1138. doi: 10.1007/s10654-020-00698-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ontario Home and Community Care. https://www.ontario.ca/page/homecare-seniors
- 3.Armstrong J.J., Zhu M., Hirdes J.P., Stolee P. Rehabilitation therapies for older clients of the Ontario home care system: regional variation and client-level predictors of service provision. Disabil Rehabil. 2015;37:625–631. doi: 10.3109/09638288.2014.935494. [DOI] [PubMed] [Google Scholar]
- 4.Van Ineveld C., Chien-Chieh Huang S., Varshney N., French Merkley V. The impact of COVID-19 pandemic restrictions on geriatric day hospitals and geriatric ambulatory care in canada: adapting for future waves and beyond. Can Geraitr Soc J CME. 2020;10 [Google Scholar]
- 5.Sepúlveda-Loyola W., Rodríguez-Sánchez I., Pérez-Rodríguez P., et al. Impact of social isolation due to COVID-19 on health in older people: mental and physical effects and recommendations. J Nutr Health Aging. 2020;24:938–947. doi: 10.1007/s12603-020-1500-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Padala K.P., Parkes C.M., Padala P.R. Neuropsychological and functional impact of COVID-19 on mild cognitive impairment. Am J Alzheimers Dis Other Demen. 2020;35 doi: 10.1177/1533317520960875. 153331752096087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aroos R., Wong B.L.L., Merchant R.A. Delayed health consequences of COVID-19 lockdown in an older adult. Age Ageing. 2021;50:673–675. doi: 10.1093/ageing/afab052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hirdes J.P., Ljunggren G., Morris J.N., et al. Reliability of the interRAI suite of assessment instruments: a 12-country study of an integrated health information system. BMC Health Serv Res. 2008;8:277. doi: 10.1186/1472-6963-8-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Landi F., Tua E., Onder G., et al. Minimum data set for home care: a valid instrument to assess frail older people living in the community. Med Care. 2000;38:1184–1190. doi: 10.1097/00005650-200012000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Morris J.N., Carpenter I., Berg K., Jones R.N. Outcome measures for use with home care clients. Can J Aging. 2000;19:87–105. [Google Scholar]
- 11.Canadian Institute for Health Information COVID-19’s Impact on Home Care. 2021. https://www.cihi.ca/en/covid-19-resources/impact-of-covid-19-on-canadas-health-care-systems/home-care-services
- 12.Morris J., Fries B., Bernebei R., et al. InterRAI Home Care (HC) Assessment Form and User’s Manual. 9.1.3. interRAI. 2009 [Google Scholar]
- 13.Morris J.N., Berg K., Fries B.E., Steel K., Howard E.P. Scaling functional status within the interRAI suite of assessment instruments. BMC Geriatr. 2013;13:128. doi: 10.1186/1471-2318-13-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morris J.N., Berg K., Howard E.P., Jonsson P.V., Craig M. Functional recovery within a formal home care program. J Am Med Dir Assoc. 2019;20:1001–1006. doi: 10.1016/j.jamda.2018.12.014. [DOI] [PubMed] [Google Scholar]
- 15.Jamieson H.A., Abey-Nesbit R., Pickering J.W. Effect of capacity to undertake instrumental activities of daily living on entry to aged residential care in older people with heart failure. Front Med (Lausanne) 2020;7:386. doi: 10.3389/fmed.2020.00386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morris J.N., Howard E.P., Steel K.R. Development of the interRAI home care frailty scale. BMC Geriatr. 2016;16:188. doi: 10.1186/s12877-016-0364-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hirdes J.P., Frijters D.H., Teare G.F. The MDS-CHESS scale: a new measure to predict mortality in institutionalized older people. J Am Geriatr Soc. 2003;51:96–100. doi: 10.1034/j.1601-5215.2002.51017.x. [DOI] [PubMed] [Google Scholar]
- 18.Dalby D.M., Hirdes J.P., Stolee P., et al. Development and psychometric properties of a standardized assessment for adults who are deaf-blind. J Vis Impairment Blindness. 2009;103:7–16. [Google Scholar]
- 19.Morris J.N., Fries B.E., Mehr D.R., et al. MDS Cognitive Performance Scale. J Gerontol. 1994;49:M174–M182. doi: 10.1093/geronj/49.4.m174. [DOI] [PubMed] [Google Scholar]
- 20.Burrows A.B., Morris J.N., Simon S.E., Hirdes J.P., Phillips C. Development of a Minimum Data Set-based depression rating scale for use in nursing homes. Age Ageing. 2000;29:165–172. doi: 10.1093/ageing/29.2.165. [DOI] [PubMed] [Google Scholar]
- 21.Katz S., Ford A.B., Moskowitz R.W., Jackson B.A., Jaffe M.W. Studies of illness in the aged: the Index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 22.Martin Lesende I., Mendibil Crespo L.I., Garaizar Bilbao I., et al. Functional decline, mortality and institutionalization after 18 months in multimorbid older persons living in the community: the FUNCIPLUR longitudinal study. Eur Geriatr Med. 2019;10:523–528. doi: 10.1007/s41999-019-00193-1. [DOI] [PubMed] [Google Scholar]
- 23.Middleton A., Simpson K.N., Bettger J.P., Bowden M.G. COVID-19 pandemic and beyond: considerations and costs of telehealth exercise programs for older adults with functional impairments living at home—lessons learned from a pilot case study. Phys Ther. 2020;100:1278–1288. doi: 10.1093/ptj/pzaa089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Machado C.L.F., Pinto R.S., Brusco C.M., Cadore E.L., Radaelli R. COVID-19 pandemic is an urgent time for older people to practice resistance exercise at home. Exp Gerontol. 2020;141:111101. doi: 10.1016/j.exger.2020.111101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sinn C.L.J., Sutlan H., Turcotte L.A., McArthur C., Hirdes J.P. Patterns of home care assessment and service provision before and during the COVID-19 pandemic in Ontario Canada. PLoS One. 2022;17:e0266160. doi: 10.1371/journal.pone.0266160. [DOI] [PMC free article] [PubMed] [Google Scholar]