Abstract
To report a case of MEWDS post-COVID-19 infection with multimodal imaging. A 17-year-old boy reported blurring of vision in both eyes 2 months and 10 days following the SARS-CoV-2 infection. Fundus examination revealed hypopigmented lesions nasal to the optic disc, inferior periphery, and near macula in both eyes. Multimodal imaging was consistent with MEWDS. A complete systemic workup was performed to exclude infectious etiology. Fundus lesions resolved with a course of oral corticosteroids and was confirmed on multimodal imaging.
Keywords: Choroidal inflammation, complications of COVID-19, MEWDS, posterior uveitis
Coronavirus disease 2019 (COVID-19) is a contagious disease caused by severe acute respiratory syndrome (SARS-CoV-2) virus. The first case was identified in Wuhan, China in December 2019. Since then, the disease has spread worldwide, leading to an ongoing pandemic.
Most people who contract COVID-19 experience mild to moderate symptoms. The infection can sometimes be associated with severe lymphopenia and eosinopenia, extensive pneumonia, acute respiratory distress syndrome, and multiorgan failure due to a dysfunctional immune response.[1] An increased prevalence of autoantibodies in infected patients and higher susceptibility of patients with autoimmune conditions to SARS-CoV-2 infection has been reported. It has been proposed that SARS-CoV-2 can activate an autoimmune response. Various ocular manifestations such as acute conjunctivitis, episcleritis, acute anterior uveitis, reactivation of serpiginous choroiditis, retinal vasculitis, central retinal artery occlusion (CRAO), central retinal vein occlusion (CRVO), optic neuritis, and papilledema have been reported.[2] We report a case of MEWDS following SARS-CoV-2. To our knowledge, this is the first report of a MEWDS manifesting after SARS-CoV-2 infection.
Case Report
A 17-year-old boy presented with the blurring of vision, photopsia, and floaters in both eyes. Two months ten days ago, he developed fever and tested positive for SARS-CoV-2 by reverse transcriptase-polymerase chain reaction (RT-PCR). He was treated for mild symptoms with oral azithromycin for 5 days; 2 weeks later, his RT-PCR tested negative. His visual symptoms developed after 2 months 10 days of COVID-19 infection.
He was diagnosed with right-eye multifocal choroiditis by a local ophthalmologist and treated with oral prednisolone for 2 weeks (60 mg/day for a week followed by 50 mg/day for a week) along with topical steroids, mydriatic, and cycloplegics.
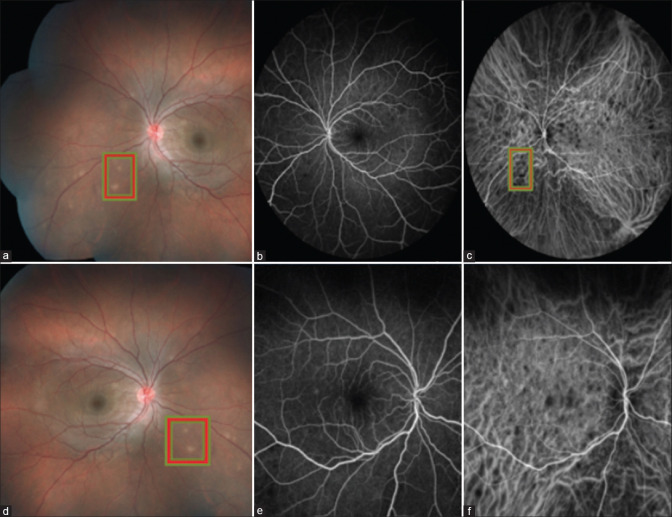
On examination, his best-corrected visual acuity (BCVA) was 6/9, N6 in both eyes. Anterior segment examination was unremarkable. Fundus examination revealed multiple hypopigmented active choroidal lesions nasal to disc, inferior periphery, and near the macula. There was no vitreous inflammation or vasculitis. Our clinical diagnosis was MEWDS. Ancillary testing was performed [Fig. 1] to characterize the described fundoscopic lesions such as color fundus photographs, fundus fluorescein angiography (FFA), indocyanine-green angiography (ICGA), fundus autofluorescence (FAF), and swept-source optical coherence tomography (SS-OCT). FFA demonstrated early hyperfluorescence with late staining, and ICGA showed hypocyanescence in both early and late frames. SS-OCT showed disruption of the ellipsoid zone and mild attenuation of the external limiting membrane. Choriocapillaris were normal.
Figure 1.
At presentation (a-c) of left eye (a) color fundus photograph (b) FFA showing a multiple hyperflouroscence with late staining (c) ICG showing hypocyanescence, and (d-f) showing similar lesions in the right eye
The clinical and imaging characteristics of the lesions were consistent with MEWDS.
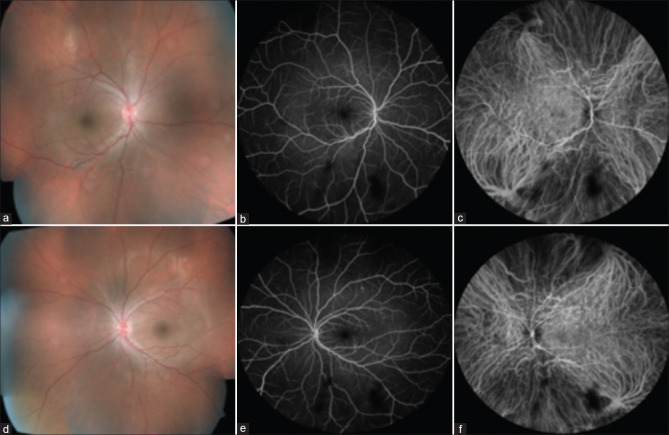
A complete systemic workup was conducted, including routine laboratory screening with complete blood cell counts, liver function tests, renal function tests, Mantoux and QuantiFERON-TB Gold test, and serum angiotensin-converting enzyme. All the tests were found to be within normal limits. The patient was continued on oral prednisolone 1 mg/kg of bodyweight (60 mg with slow tapering 5 mg per week) and was treated for a duration of 5 months. During the follow-up period, serial multimodal imaging was performed at baseline [Fig. 1], 2 months, 4 months, and 6 months [Fig. 2], demonstrating complete resolution of MEWDS. The patient developed deranged liver functions for which the hepatologist opinion was sought and suspected oral steroids as the cause of deranged liver function. Oral steroids were temporarily stopped for 2 weeks. At final follow-up, BCVA improved to 6/5; N6 with complete resolution of the lesions. The patient was systemically well. The liver function test came back to normal limits.
Figure 2.
At 6 months follow-up: Right eye (a) color fundus photograph (b) FFA and (c) ICG images showing complete resolution of lesions, similarly (d-f) showing complete resolution in the left eye
Discussion
MEWDS was first reported in 1984 by Jampol et al.[3] as an idiopathic intraocular inflammatory disorder characterized by the development of transient small gray-white lesions presumed to occur at the level of retinal photoreceptors or retinal pigment epithelium (RPE). Clinical manifestations have been described in the retina, choroid, and optic nerve, including transient white fundus lesions, macular granularity, and mild inflammation of the optic nerve.[3]
The lesions are best characterized as punctate areas of early hyperfluorescence on FFA with late staining. In contrast, ICGA in patients with MEWDS reveals numerous hypocyanescent lesions.
The exact pathogenesis of MEWDS is unknown, but it is thought to be caused by an underlying autoimmune mechanism. Suggested explanations include viral agents entering retinal photoreceptor cells at the edge of the optic nerve and ora serrata, triggering an autoimmune response.[4,5,6] Associations with environmental triggers and human leukocyte antigen (HLA)-B51 have also been reported. Cases have also been reported after vaccinations for human papillomavirus, hepatitis A, and hepatitis B.[7,8] There is a hypothesis that the pathophysiology of coronavirus infection comprises two phases: the first phase of viral infection and induction of immune response and the second phase of inducing autoimmunity.[9] Sen et al. performed a literature review and described various ocular manifestation of SARS-CoV-2 and their pathogenesis. They suggested that the ocular manifestation may be due to the direct effect of the virus, immune-mediated tissue damage, activation of the coagulation cascade, and prothrombotic state induced by the viral infection.[10] The viral ribonucleic acid (RNA) has been isolated from the ocular tissue, but the role of the eye as a route of infection is still not established. Ophthalmic manifestations may be the presenting feature of COVID-19 infection or they may develop several weeks after recovery. A similar case of reactivation of serpiginous choroiditis has been reported following SARS-CoV-2, which also suggested the role of autoimmunity.[2] Our patient responded to oral steroids, suggesting an autoimmune trigger.
To the best of our knowledge, this is the first report of a MEWDS following COVID-19 infection.
Conclusion
MEWDS can also be a presentation of post COVID-19 infection.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
Ms. Esther, content writer of Sankara Netralaya, Chennai for English and Grammar.
References
- 1.Cascella M, Rajnik M, Aleem A, Dulebohn SC, Di Napoli R. StatPearls. Treasure Island (FL): StatPearls Publishing; 2021. [Last accessed on 2021 Sep 02]. Features, evaluation, and treatment of coronavirus (COVID-19) Available from: https://www.ncbi.nlm.nih.gov/books/NBK554776/ [PubMed] [Google Scholar]
- 2.Providência J, Fonseca C, Henriques F, Proença R. Serpiginous choroiditis presenting after SARS-CoV-2 infection: A new immunological trigger? Eur J Ophthalmol. 2022;32:NP97–NP101. doi: 10.1177/1120672120977817. [DOI] [PubMed] [Google Scholar]
- 3.Jampol LM, Sieving PA, Pugh D, Fishman GA, Gilbert H. Multiple evanescent white dot syndrome, I: Clinical findings. Arch Ophthalmol. 1984;102:6714. doi: 10.1001/archopht.1984.01040030527008. [DOI] [PubMed] [Google Scholar]
- 4.Crawford CM, Igboeli O. A review of the inflammatory chorioretinopathies: The white dot syndromes. ISRN Inflamm 2013. 2013 doi: 10.1155/2013/783190. 783190. doi: 10.1155/2013/783190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abu-Yaghi NE, Hartono SP, Hodge DO, Pulido JS, Bakri SJ. White dot syndromes: A 20-year study of incidence, clinical features, and outcomes. Ocul Immunol Inflamm. 2011;19:426–30. doi: 10.3109/09273948.2011.624287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.dell'Omo R, Pavesio CE. Multiple evanescent white dot syndrome (MEWDS) Int Ophthalmol Clin. 2012;52:221–8. doi: 10.1097/IIO.0b013e31826647ed. [DOI] [PubMed] [Google Scholar]
- 7.Baglivo E, Safran AB, Borruat FX. Multiple evanescent white dot syndrome after hepatitis B vaccine. Am J Ophthalmol. 1996;122:431–2. doi: 10.1016/s0002-9394(14)72074-4. [DOI] [PubMed] [Google Scholar]
- 8.Romanowski B, de Borba PC, Naud PS, Roteli-Martins CM, De Carvalho NS, et al. GlaxoSmithKline Vaccine HPV-007 Study Group. Sustained efficacy and immunogenicity of the human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine: Analysis of a randomised placebo-controlled trial up to 6.4 years. Lancet. 2009;374:1975–85. doi: 10.1016/S0140-6736(09)61567-1. [DOI] [PubMed] [Google Scholar]
- 9.Hooper LC, Chin MS, Detrick B, Hooks JJ. Retinal degeneration in experimental coronavirus retinopathy (ECOR) is associated with increased TNF-alpha, soluble TNFR2 and altered TNF-alpha signaling. J Neuroimmunol. 2005;166:65–74. doi: 10.1016/j.jneuroim.2005.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sen M, Honavar SG, Sharma N, Sachdev MS. COVID-19 and eye: A review of ophthalmic manisfestations of COVID-19. Indian J Ophthalmol. 2021;69:488–509. doi: 10.4103/ijo.IJO_297_21. [DOI] [PMC free article] [PubMed] [Google Scholar]