ABSTRACT
Companion animals and humans are known to share extraintestinal pathogenic Escherichia coli (ExPEC), but the extent of E. coli sequence types (STs) that cause extraintestinal diseases in dogs is not well understood. Here, we generated whole-genome sequences of 377 ExPEC collected by the University of Melbourne Veterinary Hospital from dogs over an 11-year period from 2007 to 2017. Isolates were predominantly from urogenital tract infections (219, 58.1%), but isolates from gastrointestinal specimens (51, 13.5%), general infections (72, 19.1%), and soft tissue infections (34, 9%) were also represented. A diverse collection of 53 STs were identified, with 18 of these including at least five sequences. The five most prevalent STs were ST372 (69, 18.3%), ST73 (31, 8.2%), ST127 (22, 5.8%), ST80 (19, 5.0%), and ST58 (14, 3.7%). Apart from ST372, all of these are prominent human ExPEC STs. Other common ExPEC STs identified included ST12, ST131, ST95, ST141, ST963, ST1193, ST88, and ST38. Virulence gene profiles, antimicrobial resistance carriage, and trends in plasmid carriage for specific STs were generally reflective of those seen in humans. Many of the prominent STs were observed repetitively over an 11-year time span, indicating their persistence in the dogs in the community, which is most likely driven by household sharing of E. coli between humans and their pets. The case of ST372 as a dominant canine lineage observed sporadically in humans is flagged for further investigation.
IMPORTANCE Pathogenic E. coli that causes extraintestinal infections (ExPEC) in humans and canines represents a significant burden in hospital and veterinary settings. Despite the obvious interrelationship between dogs and humans favoring both zoonotic and anthropozoonotic infections, whole-genome sequencing projects examining large numbers of canine-origin ExPEC are lacking. In support of anthropozoonosis, we found that most STs from canine infections are dominant human ExPEC STs (e.g., ST73, ST127, ST131) with similar genomic traits, such as plasmid carriage and virulence gene burden. In contrast, we identified ST372 as the dominant canine ST and a sporadic cause of infection in humans, supporting zoonotic transfer. Furthermore, we highlight that, as is the case in humans, STs in canine disease are consistent over time, implicating the gastrointestinal tract as the major community reservoir, which is likely augmented by exposure to human E. coli via shared diet and proximity.
KEYWORDS: Escherichia coli, ExPEC, ST372, antimicrobial resistance, canine, dogs, genomic epidemiology, infections, one health, virulence, whole-genome sequencing
INTRODUCTION
Australia has one of the highest rates of ownership of dogs as companion animals in the world, with about 40% of households owning at least one dog (1). Most dog owners consider their dogs to be part of their family and often report high levels of physical contact with them in addition to sharing food from the household. Human-dog relationships are rooted in deep shared evolution and provide significant psychological benefits from improved self-confidence and companionship (2, 3). There is a general perception that pets can improve their owners’ health, sense of psychological well-being, and longevity (4). These benefits underpin calls to enable access of companion animals to health care facilities (5). However, there is the wide variety of pathogens that may transfer between humans and dogs, posing health risks to both (6). The benefits of dog ownership must therefore be weighed with the possible zoonotic disease implications that may be associated with these relationships (7–9).
Mammalian, avian, and reptilian species are colonized by commensal lineages of Escherichia coli that perform important functions in the gut. However, some E. coli lineages are known to cause severe intestinal and extraintestinal disease. Extraintestinal pathogenic E. coli (ExPEC) is the most common cause of Gram-negative infections in humans, causing a wide range of afflictions, including lower urinary tract infections, pyelonephritis, bacteremia, sepsis, skin infections, and ventilator-associated respiratory infections (10–13). Similarly, ExPEC is a leading cause of urinary tract infection in dogs and cats (14–16) and causes a range of extraintestinal diseases in companion animals in general (17, 18). Many studies of ExPEC in companion animals have focused on isolates with resistance to clinically important antimicrobials. For example, a recent study in New Zealand showed that humans living in a household shared the same drug-resistant E. coli with their pet dogs (19). Although these studies are clearly important, narrowing the scope of research to only antimicrobial-resistant isolates could obscure a deeper understanding of the epidemiology of E. coli sequence types associated with clinical disease in companion animals.
Despite its vast commensal and pathogenic range, deciphering the zoonotic and zooanthroponotic potential of E. coli remains a challenge (20, 21). Addressing this issue requires a deep understanding of genomic epidemiology of the dominant ExPEC sequence types (STs) as well as emerging ExPEC STs in both humans and animals (7, 22–26). There are more than 11,000 E. coli sequence types, but the top 20 ExPEC sequence types are responsible for more than 85% of ExPEC infections in humans (13). The remaining 15% of infections are caused by strains that display remarkable diversity, a pool that presumably harbors both clones which might emerge as novel pandemic lineages and others that might be less successful. However, the ability to predict which clone is which, and where the true reservoirs lie, currently remains outside our understanding.
There is an already-noted overlap in the STs that cause ExPEC infections in humans and dogs, with both species sharing ST73, ST131, and ST12 among the dominant types (8, 13). Among ExPEC infections in dogs, phylogroup B2 E. coli is highly prevalent, with ST372, ST73, ST127, ST12, and ST131 (8), as well as drug-resistant E. coli in commensal phylogroup A, with ST410 and ST683 the most common (18).
The role of plasmids in the evolution of ExPEC STs, their diversification into sublineages, and dissemination in nonhuman niches is an emerging theme in the genomic epidemiology of ExPEC. Despite the variety of plasmids that are found in E. coli, F plasmids dominate among a proportion of major and emerging ExPEC STs. For example, carriage of F plasmids is very common in ST131, ST95, ST58, and ST127, with separate plasmid lineages found to be characteristic of ST sublineages (7, 22, 23, 25). F plasmids can be categorized genotypically by their accessory gene content, and plasmid lineages within those genotypes can be approximated by their F replicon sequence types (RSTs). In terms of the categorical distinction, two major F plasmid genotypes, namely, ColV plasmids and ColIa/pUTI89-like plasmids, are commonly found in ExPEC (27, 28). Both types carry genetically distinct, but functionally similar, accessory gene loci that are primarily involved in iron acquisition. Iron acquisition genes function as both intestinal fitness factors and extraintestinal virulence factors, underscoring their obvious utility to E. coli (29, 30). In contrast to pUTI89-like plasmids, which rarely carry antimicrobial resistance genes (ARGs), ColV plasmids often carry ARG loci in association with smaller mobile genetic elements (MGEs), such as insertion sequences and transposons (28). Currently, little is known of their distribution within ExPEC in dogs.
Here, we have undertaken the largest whole-genome sequencing analysis of E. coli from dogs. The collection comprises 377 isolates, collected over 11 years from a restricted geographical area. Most isolates were from cases of extraintestinal diseases, such as urinary tract, respiratory, and skin infections. A small number of isolates from gastrointestinal tract specimens are also represented in the collection. We have determined their phylogroups, multilocus sequence types, e-serotypes, and fimH types. Furthermore, we have defined their plasmid repertoire, noting carriage of important F plasmids, and we carried out a thorough analysis of their virulence-associated gene (VAG) and antimicrobial resistance gene carriage.
RESULTS
Study collection.
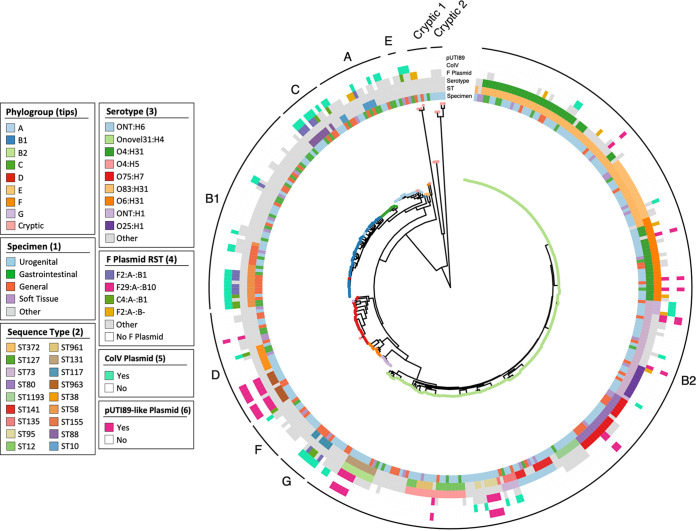
The study collection consisted of 377 E. coli genome sequences originating from dogs presenting at veterinary hospitals in Melbourne, Australia. E. coli was isolated over an 11-year period from 2007 to 2017 (Fig. 1a). Most isolates were of extraintestinal origin, and specimens were classified as urogenital tract (219, 58.1%), general (72, 19.1%), soft tissue (34, 9%), and other (one isolate had conflicting source information) (Fig. 1a). Fifty-one gastrointestinal tract isolates (13.5%), primarily from bile or feces, were also included.
FIG 1.
Characteristics of the genome collection. (a) Counts of isolates by year of isolation, stratified by specimen type. (b) Counts of phylogroups, stratified by ST. (c) Counts of specimen type, stratified by ST. (d) Counts of STs identified for each year of isolation.
B2 was the dominant phylogroup (225, 59.7%), followed by B1 (51, 13.5%), D (30, 8.0%), and A (21, 5.6%) (Fig. 1b). A total of 53 distinct STs were identified, and 18 of these had five or more representatives. STs with less than 5 representatives and isolates for which an ST could not be identified were grouped as “other.” The five most prevalent STs were ST372 (69, 18.3%), ST73 (31, 8.2%), ST127 (22, 5.8%), ST80 (19, 5.0%), and ST58 (14, 3.7%). Apart from ST58 (B1), these STs all belonged to phylogroup B2. Other well-recognized ExPEC STs identified included ST12, ST131, ST141, ST963, ST1193, ST95, ST88, and ST38. The prominent commensal ST10 and the avian-associated ST117 were also identified.
Among the 18 major STs, 17 were present in urogenital tract specimens, while 12 were present in gastrointestinal tract specimens. While extraintestinal isolates were presumptively the etiological agent responsible for presentation, it is possible that a proportion of gastrointestinal tract isolates were actually commensals, not intestinal pathogens. The facts that (i) ExPEC typically originates in the lower gastrointestinal tract, (ii) the ST distribution in gastrointestinal tract samples comprised most of the dominant urinary STs, and (iii) there was a lack of classical intestinal virulence factors among gastrointestinal tract isolates suggest that most gastrointestinal tract samples in the collection were intestinal commensals with the potential to cause extraintestinal disease.
Temporal persistence of several major STs, including ST372 (observed every year), ST127 (9 of 11 years), ST58 and ST73 (both 8 of 11 years), was detected (Fig. 1d). Only ST10 was seen in fewer than three sampling years. Despite the variable sample size each year, these data generally indicate that certain lineages of canine pathogenic E. coli are consistently present in the population over an extended period of time.
Phylogeny.
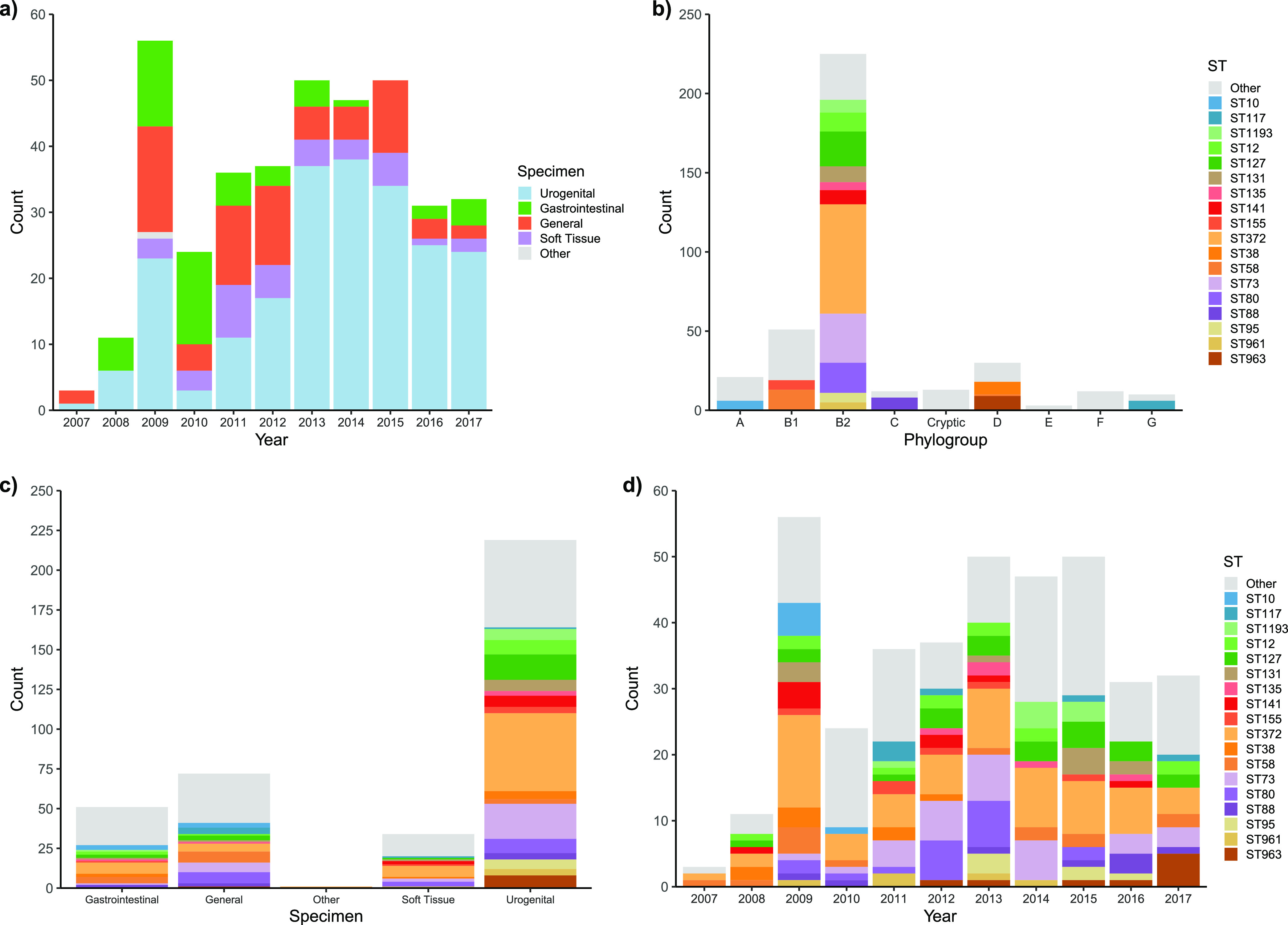
A maximum-likelihood core gene phylogeny was clearly structured by phylogroup and ST, as expected (Fig. 2). It did, however, reveal that the in silico phylogroup, as determined by EZClermont, was occasionally inaccurate, as illustrated by the presence of several sequences designated phylogroup A in the B1 clade, as well as two miscalls in the D clade. Overlaid metadata did not reveal any clustering of specimen by phylogeny, reflecting the previously described presence of STs across specimen types. Specific serotypes generally corresponded to STs, but O4:H5 was found in both ST12 and ST961.
FIG 2.
Core gene phylogeny, as shown by a maximum-likelihood phylogeny inferred by IQTree on the core gene alignment produced by Roary. Clades are labeled on the outermost ring by consensus phylogroup (determined by EZCLermont), shown on tree tips. Metadata for specimen, ST, serotype, F plasmid RST, ColV plasmid and pUTI89 plasmid presence are represented in bands around the phylogeny.
F plasmids.
Important F plasmid archetypes ColV (56/377, 14.9%) and pUTI89-like (29/377, 7.7%) were identified in a proportion of isolates. ColV+ sequences carried a variety of F RSTs including A-:B1:C4, F2:A-:B1, and F2:A-:B-, while all pUTI89+ sequences carried the F29:A-:B10 replicon (Fig. 2). These two plasmid types had different phylogenetic distributions. ColV plasmids were found in eight major STs belonging to all phylogroups (Fig. 3a and b), whereas pUTI89-like plasmids were present in seven STs restricted to phylogroups B2 and D (one pUTI89+ sequence was typed as cryptic but belonged to phylogroup D according to the phylogenetic tree, indicating that it was not a true member of the cryptic clades). ST372 and ST73 were the only STs that contained both ColV+ and pUTI89+ sequences, but most members of these STs carried neither plasmid. Consistent with principles of plasmid exclusion, no sequence was found to contain both plasmid types.
FIG 3.
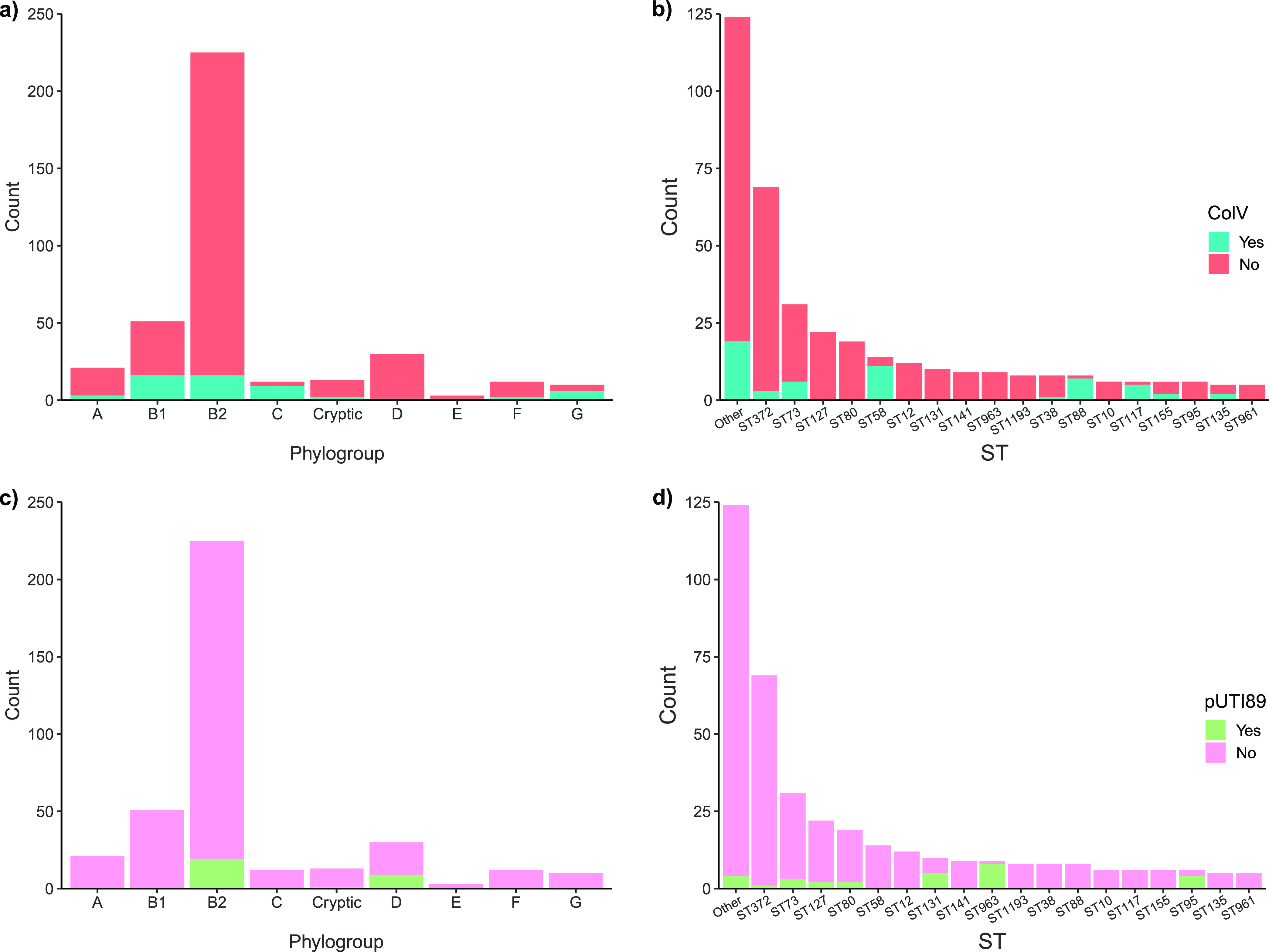
F plasmid carriage. Inference of ColV plasmid carriage based on phylogroup (a) and ST (b) and of pUTI89-like plasmid carriage based on phylogroup (c) and ST (d).
Antimicrobial resistance.
Antimicrobial resistance (AMR) to seven antimicrobial compounds comprising six drug classes commonly used in veterinary medicine was tested for by disk diffusion for 365/377 isolates (see Fig. S1 in the supplemental material). Antimicrobials tested included ampicillin, amoxicillin plus clavulanate, cephalexin, enrofloxacin, tetracycline, sulfamethoxazole, and trimethoprim. On average, isolates were only resistant to 1.26 compounds, with a median of zero. Seventy-seven isolates (20.4%) were resistant to three or more antimicrobial classes and were therefore considered multidrug resistant.
The class 1 integrase gene intI1, a common genetic proxy for multidrug resistance, was found in 51 sequences (13.5% at 90% sequence identity over 95% of the length of intI1), 40 of which were multidrug resistant (MDR). Truncated copies of intI1 were also detected, the most common of which was a 746-bp fragment in ST1193 (7/8, 87.5%) and ST131 (3/10, 30%). A further 10 isolates carried truncated copies of intI1 ranging in size from 114 to 746 bp, underscoring the ongoing evolution of the class 1 integron structure. All 20 sequences carrying truncated copies of intI1 were classified as MDR, and 2 of them (MVC207 and MVC227) also carried full copies of intI1 on other contigs. The total inferred carriage of class 1 integrons was therefore 70/377 (18.6%).
Genotypic AMR in the collection was generally moderate and reflective of the phenotypic data, with a mean 5.12 ARGs per sequence and a median of 4. Phylogroup B2 sequences displayed a low prevalence of ARGs (mean, 3.89), second only to cryptic phylogroup (mean, 3.15) (Fig. 4a; see also Fig. S1 in the supplemental material). Predominant phylogroups B1 (mean, 6.35) and D (mean, 7.8) showed moderate carriage, while phylogroup F, to which only 12 sequences belonged, showed the highest prevalence (mean, 9). Common ARGs included blaTEM-181 (98, 26%), sul2 (59, 15.6%), strA (aph-3-lb; 54, 14.3%), strB (aph-6-ld; 51, 13.5%), tetA (47, 12.5%), and sul1 (44, 11.7%).
FIG 4.
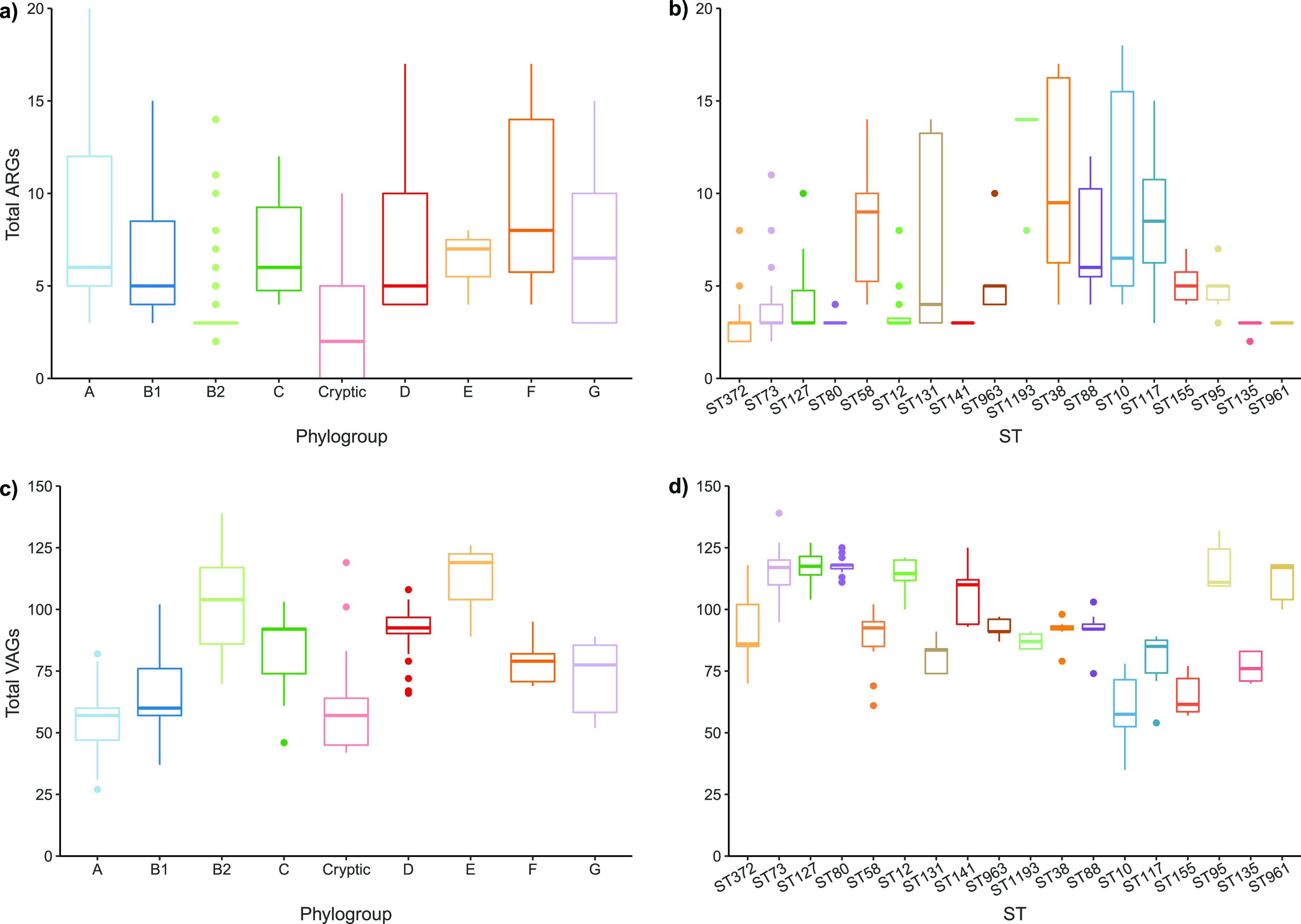
Distribution of antimicrobial resistance genes (ARGs) and virulence-associated genes (VAGs). Boxplots show average total ARGs by phylogroup (a), average total ARGs by ST (b), average total VAGs by phylogroup (c), and average total VAGs by ST (d).
The five most resistant STs in terms of the number of ARGs they contained were B2-ST1193 (mean, 13.2), D-ST38 (mean, 10.5), A-ST10 (mean, 9.67), G-ST117 (mean, 8.67), and B1-ST58 (mean, 8.29) (Fig. 4b). ST1193 was conspicuous as the only ST within phylogroup B2 to have consistently high rates of ARG carriage. All five STs with high ARG carriage showed evidence of integron carriage, including presence of characteristic components intI1, ARG cassettes (dfrA and aadA variants), and qacEΔ1. Within ST58 and ST117, intI1 carriage often co-occurred with ColV plasmid carriage.
Fluoroquinolone resistance mediated by point mutations was predicted for 66 sequences (17.5%), only 33 of which were phenotypically resistant to enrofloxacin. All ST131 (10) and ST1193 (8) sequences were predicted to be fluoroquinolone resistant. Other notable STs predicted to be resistant included ST38 (5/8), ST58 (2/14), ST73 (2/31), ST127 (2/22), and ST10 (2/6).
Virulence.
In contrast to AMR genotypes, VAG profiles were extensive—consistent with the pathogenic status of the isolates under investigation. The dominant phylogroup B2 had the second highest average VAG count, with 102 VAGs per strain (Fig. 4c). Phylogroup E had the highest average VAGs (mean, 111 per strain), but only contained three sequences (MVC307, MVC681, and MVC73). Phylogroups D and C also had extensive VAG arrays, with averages of 90.9 and 83.2 per strain, respectively. The sequence types with the most virulence genes (mean VAGs are in parentheses) within phylogroup B2 were ST80 (118), ST127 (118), ST95 (117), ST73 (116), ST12 (114), ST961 (111), and ST141 (107) (Fig. 4d). Sequences belonging to ST1193 (87.1) and ST372 (89.1) carried fewer VAGs than their B2 counterparts, a notable observation given the extensive ARG carriage of ST1193 and the dominance of ST372 in the collection. STs with high VAG carriage in other phylogroups included ST963 and ST38 (phylogroup D; means of 92.7 and 91.5, respectively) and ST88 (phylogroup C; 91.9). Generally, STs with higher ARG carriage displayed more moderate VAG carriage.
VAGs in the collection overwhelmingly encoded functions associated with ExPEC. Genes associated with intestinal pathotypes were very rare, with only two sequences containing a toxin gene of any kind (MVC147-ST10 for estIa and MVC785-ST2700 for toxB), and Shiga toxin genes were not detected in any sequence (see Table S1 in the supplemental material).
As B2 sequences carried high average VAGs, numerous specific genes were predictably clustered within this phylogroup (see Fig. S2 in the supplemental material). The hemolysin operon hlyABCD was mostly found in B2 sequences (total hylA of 144, 38.2%). The heme uptake operon chuASTUVWXY was present in all B2 sequences except for a single sequence missing chuA (total of 227, 60.2%). The K1 capsule genes (kpsCDEFMSU) were typically found as an operon in B2, G, F, D, and cryptic clades, whereas phylogroups B1, A, and C lacked these genes (total kpsM of 185, 49%). Most ST372 sequences lacked kps genes, a rarity among B2 sequences. P fimbriae encoded by genes of the pap operon were primarily found in B2 sequences with variability in the presence/absence patterns of individual gene carriage (total papC of 150, 39.8%). F1C fimbriae were only found in B2 sequences (ST372 and ST73), except for a single B1-ST155 sequence (total focA of 99, 26.3%). Genes of the sfa operon encoding S fimbriae were variably present, mostly within B2 sequences, though major subunit sfaA was mostly absent (13, 3.5%; total sfaB of 179, 47.5%).
Genes involved in iron acquisition that are typically found on ColV plasmids, such as iroN (220, 58.4%), iucD (78, 20.7%), and iutA (77, 20.4%), were also identified in sequences that did not carry a ColV plasmid, indicating chromosomal locations or carriage on other episomal elements. In B2, iroN carriage did not usually correspond to ColV plasmid carriage (B2: 12 ColV+ versus 167 ColV−), whereas in non-B2 sequences, iroN was almost always observed in conjunction with ColV (non-B2: 39 ColV+ versus 2 ColV−). Similarly, cjrABC-senB, a component of pUTI89-like plasmids and putative iron uptake system, was identified in sequences with and without pUTI89-like plasmids (29 pUTI89+, 25 pUTI89−; total of 54 cjrABC-senB, 14.3%), although these genes were restricted to phylogroups B2 and D regardless of plasmid carriage. Overall, these results point to an apparent interplay between specific iron acquisition systems, mobile genetic elements, and phylogenetic background within pathogenic E. coli. Further underscoring the importance of iron acquisition in pathogenic E. coli was the extensive carriage of the yersiniabactin high-pathogenicity island (HPI), indicated by marker genes fyuA and irp2 (both 287, 76.1%). HPI was present in almost all B2 sequences (222/225, 98.7%) and identified in every phylogroup except for E.
DISCUSSION
Canine and human ExPEC share common lineages.
Here, we generated the largest collection of canine-origin E. coli whole-genome sequences assembled to date. Phylogroup B2 dominated the collection. Phylogroup B2 was similarly overrepresented (79.6%) in a study of 618 E. coli isolates from dogs attending four veterinary clinics in France (18) and is by far the major phylogroup among human ExPEC (13, 31). A diversity of STs were identified across the specimen types, indicating that STs are not syndrome specific. The most common STs almost exclusively (barring the enigmatic B1-ST58) belonged to phylogroup B2, with ST372, ST73, and ST127 being the most prevalent types.
The most common type, ST372, was similarly dominant among E. coli from canine infections in Australia and fecal commensals from healthy dogs in Spain (8, 18, 32, 33). ST372 is also identified among human ExPEC isolates, although, unlike ST73 and ST127, it is not ranked in the top 20 most prevalent human ExPEC STs (34, 35). It was interesting that the virulence gene carriage of ST372 was lower than that of many of the other STs in the collection. This might be explained by database bias toward genes associated with virulence for humans and a lack of knowledge of dog-specific virulence genes. Alternatively, the dominance of the ST in the absence of an extensive array of virulence genes may be due to its possession of metabolic capacities facilitating success in the canine gut, with its infectivity being predominantly host-mediated. The latter possibility, in conjunction with its apparent dominance in both healthy and diseased dogs and lower prevalence in humans, supports the contention that ST372 is a dog-adapted lineage of E. coli (18). Future work involving in-depth genomic comparisons between dog and human ST372 isolates will provide further information in this regard.
ST73 is often overshadowed by ST131, despite consistent reports of its dominance as a human ExPEC sequence type causing UTI and bacteremia in Australia (36, 37), France (38), the United Kingdom (39, 40), and elsewhere (13). The dominance of ST73 in our study of E. coli from dogs, as well as in the large study of isolates from dogs in France, indicates that dogs may be a major reservoir of ST73 (18). A similar observation prevails in E. coli isolated from cats (41). It is as yet unknown whether the ST73 in dogs represents distinct dog-adapted sublineages or acquisition of human lineages, as has been postulated for ST131 and ST1193 (42).
ST127 is another common human ExPEC lineage, often associated with sepsis (43). We recently demonstrated that there is global-scale genomic linkage between ST127 from companion animals (including from this collection) and human origin ST127, reflecting the aforementioned scenario with ST131 and ST1193 (7, 42).
Apart from ST372, most of the common STs in this collection are well-described human ExPEC, and their presence in community-onset canine infections over multiple years suggests that dogs and humans are both colonized by a broad spectrum of human ExPEC lineages. This is easily explained by their close association with humans as companion animals, with cocarriage being driven by shared living spaces, physical proximity, and consumption of overlapping diets, which can include raw retail meats and human food scraps. Consistent with this view, these E. coli STs predominate in the feces of healthy humans (44). Further supporting the sharing of ExPEC with humans is the virulence content of major STs in the collection reflected that of their human counterparts, with a high prevalence of Yersinia HPI carriage and an abundance of other iron acquisition genes that function in both gut colonization and pathogenicity (29).
Overall, our results indicate that canine ExPEC mostly comprise commensals and pathogens that are commonly associated with humans. ST372 represents an exception in this regard; it is a lineage that may be mostly adapted to canines, with a lower prevalence in humans. What these results imply about relative rates and directions of transfer of ExPEC between humans and dogs is still uncertain and requires further investigation.
Major F plasmid types circulate in canine ExPEC.
The major human ExPEC STs, particularly ST95 (22), ST131 (23, 26), and ST73 (45), comprise sublineages that are often discernible by serotype and fimH allele variation. Lineage subdivision is also often accompanied by carriage of different F plasmid replicon sequence types belonging to ColV (various replicon types) and pUTI89-like (ColIa+/F29:A-:B10) genotypes (22, 25, 26). In the canine collection, 56 isolates (14.9%) carried a ColV plasmid and these sequences were identified across all phylogroups. ExPEC ColV carriage in our canine collection was similar to the estimated human ExPEC carriage rate of 16% (25). ColV plasmids were particularly dominant in phylogroups C (ST88) and G (ST117), but a significant proportion of phylogroup B1 (ST58) and a small number of B2 (numerous STs) isolates also carried a ColV plasmid. ST88 is a major ColV plasmid-carrying ST causing extraintestinal disease and has also been identified in store-bought produce (36, 46–48). ST58 is a multihost pathogen with a major sublineage rich in ColV plasmids and is frequently identified in poultry and pigs (25). ST117 is a noted avian pathogenic E. coli (APEC) lineage rich in ColV plasmids and is dominant in both commensal and pathogenic E. coli populations from poultry in Australia and abroad (49, 50). As has been demonstrated for Campylobacter species, the frequent consumption of raw chicken by dogs may present a risk for acquisition of poultry-associated ExPEC, such as ST117 (51). The association of ColV-carrying ST58, ST88, ST131, and ST95 isolates with bacteremia or sepsis in Australia is also notable (36, 52). Our results are therefore reflective of previous reports of ColV carriage within prominent and emerging STs, demonstrate their pathogenicity in dogs, and support interspecies transfer between numerous hosts. It will be important to monitor the frequency of isolation of STs that can carry ColV plasmids, given the important role they play in E. coli that cause extraintestinal disease in humans and domestic animals (53).
In contrast to ColV plasmid carriage, only about 7.7% (29/377) of the collection carried a pUTI89-like plasmid. These plasmids are common in human ExPEC infections and typically carry cjrABC-senB virulence genes, which are purported to contribute to iron acquisition and ExPEC virulence in murine models of UTI (27, 54). pUTI89-like plasmids were confined to phylogroups B2 and D and were most common in ST963 (8/9, 89%), ST95 (3/6, 66.7%), and ST131 (5/8, 62.5%) sequences. Their presence in these STs is indicative of sublineage partitioning, as has been recently described for ST131 and ST95 (22, 23).
Despite the relevance of ColV and pUTI89-like plasmids to several important ExPEC STs, the two dominant STs in the collection, ST372 and ST73, mostly lacked F plasmids of these types, reiterating the unavoidable importance of the core genomic background in ExPEC evolution. Interestingly, ST73 was one of the most VAG-rich STs, with an average 116 VAGs, whereas ST372 carried substantially fewer, at an average of 89.1. ST73 isolates in this collection and others were shown to carry an abundance of adhesins and genes involved in iron acquisition, suggesting a redundancy for genes of ColV or pUTI89-like plasmids (45). Despite the lower total number of VAGs, ST372 in this collection also carried adhesins and iron acquisition genes. Overall, this indicates that our understanding of the relative contribution of plasmids and chromosomally encoded gene functions to ExPEC intestinal fitness and extraintestinal pathogenicity is still in its infancy.
Antimicrobial resistance carriage is low but not trivial.
Notably, carriage of clinically important antibiotic resistance genes was not a common occurrence in the collection, but persistent drug resistant lineages were seen and were associated with class 1 integron carriage, often in the presence of ColV plasmids. Class 1 integrons with complete or truncated copies of intI1 were identified in 70/377 (18.6%) E. coli isolates, 27 (38.6%) of which carried a ColV plasmid. Carriage of intI1 with and without ColV was notable in several STs, including ST58 (ColV+), ST117 (ColV+), ST10 (ColV+/−), and ST38 (ColV−). The presence of intI1+ ARG loci on ColV plasmids has been well described, and our results indicate that this trend extends to canine ExPEC (28, 52, 55, 56). Extended-spectrum beta-lactamase (ESBL)-producing E. coli was infrequently detected; however, ESBL-producing E. coli in ST131, ST1193, and AmpC β-lactamase-producing E. coli in ST155, ST315, ST617, ST457, ST767, and ST372 have been detected in companion animals around the world (32, 57, 58). Fluoroquinolone resistance mutations were detected in 17.5% of sequences, also indicating exposure to human sources of E. coli, with successful human ExPEC lineages ST131 and ST1193 presenting as the predominant carriers of these mutations (57, 59).
Conclusion.
In summary, dogs are primarily infected with ExPEC characteristic of human infections, as characterized by the distribution of STs, phylogroups, plasmids, AMR, and virulence genes. One notable exception is ST372, which may be a “dog-adapted” ST that has spilled back into humans. The overall explanation for the shared genotypes is shared gut carriage of these E. coli between humans and their pets due to close proximity and shared diets.
MATERIALS AND METHODS
Isolates used in this study.
The 377 E. coli isolates analyzed were part of a collection isolated from dogs presenting with various extraintestinal diseases by the Clinical Microbiology Laboratory of the Melbourne Veterinary School, University of Melbourne, Australia, between 2007 and 2017. The isolates were transported as slope cultures on LB agar. Isolate names carry the prefix MVC (for Melbourne Veterinary Collection) followed by a 1- to 3-digit number specifying individual isolates from the collection. Full isolate metadata and public accession numbers are available in Table S1 in the supplemental material.
Genomic DNA isolation, whole-genome sequencing, and assembly.
E. coli isolates from the Melbourne Veterinary Collection were freshly cultured onto LB agar plates, and a single colony was used to inoculate 5 mL of sterile LB medium. Following overnight culture, total cellular DNA was extracted using the ISOLATE II Genomic DNA (Bioline) kit following the manufacturer’s standard protocol for bacterial cells and was stored at 4°C. Library preparation was done by the AIMI Core Sequencing Facility, University of Technology Sydney, following the adapted Nextera Flex library preparation kit process Hackflex (60). Briefly, genomic DNA was quantitatively assessed using the Quant-iT PicoGreen dsDNA assay kit (Invitrogen, USA). Each sample was normalized to a concentration of 1 ng/μL. A 10-ng sample of DNA was used for library preparation. After tagmentation, DNA was amplified using the facility’s custom-designed i7 and i5 barcodes, with 12 cycles of PCR. Due to the number of samples, the quality control for the samples was done by sequencing a pool of samples using the MiSeq V2 Nano kit for 300 cycles. Briefly, after library amplification, a 3-μL sample of each library was added to a library pool. The pool was then cleaned up using SPRIselect beads (Beckman Coulter, USA) following the Hackflex protocol. The pool was sequenced using the MiSeq V2 nano kit (Illumina, USA). Based on the sequencing data generated, the read count for each sample was used to identify the failed libraries (i.e., libraries with less than 100 reads) and normalized to ensure equal representation in the final pool. The final pool was sequenced on one lane of an Illumina Novaseq S4 flow cell, 2 × 150 bp, at Novogene (Singapore). The quality of reads generated was confirmed with fastp (0.20.1).
Genome assembly and gene screening.
Clermont phylogrouping was performed with EZCLermont (https://github.com/nickp60/EzClermont). A modular analysis pipeline known as pipelord2, implemented with the Snakemake workflow management system, was used to perform primary bioinformatic analysis (61). This pipeline is freely available to download from https://github.com/maxlcummins/pipelord2_0. Default settings were used unless otherwise stated. First, Kraken2 was applied to the sequence reads to confirm all genomes were E. coli. Draft genomes were then assembled with Shovill 1.0.4 (https://github.com/tseemann/shovill), with default settings and assembly stats run to confirm the quality of the assemblies (https://github.com/sanger-pathogens/assembly-stats). Assemblies with >800 contigs or total lengths of <4.5Mbp or >6.5Mbp were excluded. MLST 2.19.0 (https://github.com/tseemann/mlst) was used to determine E. coli sequence types. ABRicate 1.0.1 (https://github.com/tseemann/abricate) was used to screen draft genomes for genes from several publicly available and custom in-house databases. Public databases used were CARD, VFDB, PlasmidFinder, SerotypeFinder, and ISFinder (62–66). The custom database included the set of genes used to infer ColV plasmid carriage (see below) and additional virulence genes. This is available at https://github.com/maxlcummins/custom_DBs. ABRicate was also used to align assemblies to a variety of reference plasmids, including pUTI89 from the E. coli strain UTI89, sourced from GenBank (gb | NC_007941). The pMLST tool available at https://bitbucket.org/genomicepidemiology/cge-tools-docker/src/master/ was used to perform pMLST typing (67). AMR-associated single-nucleotide polymorphisms were identified with PointFinder (68). Finally, gene screening results were summarized using abricateR (https://github.com/maxlcummins/abricateR), with a gene being considered present at 95% length and 90% nucleotide identity.
Criteria for inference of plasmid presence.
The presence of a ColV-type plasmid was inferred using criteria previously described by Liu et al. (69). The presence of a pUTI89-like plasmid was inferred if a given assembly mapped to ≥90% of the pUTI89 sequence at ≥90% identity or if the isolate was determined by pMLST to carry the F29:A-:B10 RST combination, which is characteristic of pUTI89-like plasmids.
Pan-genome and phylogenetic analysis.
The assembled genomes were annotated using prokka 1.14.6 (70). The core and pan-genome were then determined with Roary 3.13.0, with default settings and paralog splitting on (71). The resulting core gene alignment of 1,770,948 bp was then used as the basis for subsequent analyses. IQTree 2.0.3 was used to infer a maximum-likelihood phylogenetic tree using the GTR+F+R substitution model and 1,000 bootstrap replicates (72). The tree was midpoint rooted for visualization.
Data analysis and visualization.
A custom R script was written in RStudio 1.4.1106 with R 4.0.5 to analyze and visualize the data generated by pipelord, including MLSTs, ARGs, VAGs, and MGEs. This script was also used to infer the presence of plasmids, based on BLAST data generated by pipelord with plasmidmapR (https://github.com/maxlcummins/plasmidmapR), and to visualize the phylogenetic tree in conjunction with metadata and gene data. The sequences of plasmids pCERC4 and pUTI89 were visualized with SnapGene Viewer (version 5.0.7; GSL Biotech LLC). Microsoft PowerPoint was used to compile elements of Fig. 2 and Fig. S1 to S5 in the supplemental material.
Data availability.
All genomes used in this study were deposited in GenBank and the Sequence Read Archive under the BioProject PRJNA678027. Individual accession numbers can be found with comprehensive metadata and genomic data in Table S1. The data analysis and visualization script are freely available at https://github.com/CJREID/MVC and can be used to reproduce all secondary analyses. R package versions used therein are available within the README.md document in the code repository.
Supplementary Material
ACKNOWLEDGMENTS
We thank Kay Anantanawat for assistance with whole-genome sequencing. This research was supported by the Australian Government Research Training Program and via funding from The Australian Centre for Genomic Epidemiological Microbiology (AusGEM), a collaborative partnership between NSW DPI and The University of Technology Sydney. Computing infrastructure was provided by the UTS Interactive High Performance Computing facility.
P.E. contributed formal analysis, investigation, data curation, and writing of the original draft; M.L.C. contributed investigation, data curation, project administration, and methodology; G.F.B. contributed investigation, data curation, and project administration; M.S.M. contributed investigation, data curation, and project administration; C.J.R. contributed conceptualization, methodology, software, validation, formal analysis, writing review and editing, visualization, and supervision; S.P.D. contributed conceptualization, resources, writing review and editing, supervision, project administration, and funding acquisition.
Footnotes
Supplemental material is available online only.
Contributor Information
Cameron J. Reid, Email: Cameron.Reid@uts.edu.au.
Steven P. Djordjevic, Email: Steven.Djordjevic@uts.edu.au.
Cheryl P. Andam, University at Albany, State University of New York
Jorge Blanco, Universidade de Santiago de Compostela.
Tim Downing, Dublin City University.
REFERENCES
- 1.Animal Medicines Australia. 2019. Pets in Australia: a national survey of pets and people. Animal Medicines Australia, Barton, ACT, Australia. https://animalmedicinesaustralia.org.au/report/pets-in-australia-a-national-survey-of-pets-and-people/. [Google Scholar]
- 2.Amiot C, Bastian B, Martens P. 2016. People and companion animals: it takes two to tango. Bioscience 66:552–560. doi: 10.1093/biosci/biw051. [DOI] [Google Scholar]
- 3.Jackson T, Chur-Hansen A, Duncanson E, Jesudason S. 2021. A qualitative content analysis of an online forum for people with kidney disease: exploring the role of companion and non-companion animals. J Ren Care doi: 10.1111/jorc.12406. [DOI] [PubMed] [Google Scholar]
- 4.Herzog H. 2011. The impact of pets on human health and psychological well-being: fact, fiction, or hypothesis? Curr Dir Psychol Sci 20:236–239. doi: 10.1177/0963721411415220. [DOI] [Google Scholar]
- 5.Acquadro Maran D, Capitanelli I, Cortese CG, Ilesanmi OS, Gianino MM, Chirico F. 2022. Animal-assisted intervention and health care workers' psychological health: a systematic review of the literature. Animals (Basel) 12:383. doi: 10.3390/ani12030383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sims E, Epp T. May 2021. Defining important canine zoonotic pathogens within the Prairie Provinces of Canada. Can Vet J 62:477–483. [PMC free article] [PubMed] [Google Scholar]
- 7.Elankumaran P, Browning GF, Marenda MS, Reid CJ, Djordjevic SP. 2022. Close genetic linkage between human and companion animal extraintestinal pathogenic Escherichia coli ST127. Curr Res Microb Sci 3:100106. doi: 10.1016/j.crmicr.2022.100106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kidsley AK, O'Dea M, Saputra S, Jordan D, Johnson JR, Gordon DM, Turni C, Djordjevic SP, Abraham S, Trott DJ. 2020. Genomic analysis of phylogenetic group B2 extraintestinal pathogenic E. coli causing infections in dogs in Australia. Vet Microbiol 248:108783. doi: 10.1016/j.vetmic.2020.108783. [DOI] [PubMed] [Google Scholar]
- 9.Vilibic-Cavlek T, Stevanovic V, Brlek-Gorski D, Ferencak I, Ferenc T, Ujevic-Bosnjak M, Tabain I, Janev-Holcer N, Perkovic I, Anticevic M, Bekavac B, Kaic B, Mrzljak A, Ganjto M, Zmak L, Mauric Maljkovic M, Jelicic P, Bucic L, Barbic L. 2021. Emerging trends in the epidemiology of COVID-19: the Croatian 'One Health' perspective. Viruses 13:2354. doi: 10.3390/v13122354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johnson JR, Russo TA. 2018. Molecular epidemiology of extraintestinal pathogenic Escherichia coli. EcoSal Plus 8. doi: 10.1128/ecosalplus.ESP-0004-2017. [DOI] [PubMed] [Google Scholar]
- 11.La Combe B, Clermont O, Messika J, Eveillard M, Kouatchet A, Lasocki S, Corvec S, Lakhal K, Billard-Pomares T, Fernandes R, Armand-Lefevre L, Bourdon S, Reignier J, Fihman V, de Prost N, Bador J, Goret J, Wallet F, Denamur E, Ricard J-D, COLOCOLI Group . 2019. Pneumonia-specific Escherichia coli with distinct phylogenetic and virulence profiles, France, 2012–2014. Emerg Infect Dis 25:710–718. doi: 10.3201/eid2504.180944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Poolman JT, Wacker M. 2016. Extraintestinal pathogenic Escherichia coli, a common human pathogen: challenges for vaccine development and progress in the field. J Infect Dis 213:6–13. doi: 10.1093/infdis/jiv429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Manges AR, Geum HM, Guo A, Edens TJ, Fibke CD, Pitout JDD. 2019. Global extraintestinal pathogenic Escherichia coli (ExPEC) lineages. Clin Microbiol Rev 32. doi: 10.1128/CMR.00135-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Darwich L, Seminati C, Burballa A, Nieto A, Durán I, Tarradas N, Molina-López RA. 2021. Antimicrobial susceptibility of bacterial isolates from urinary tract infections in companion animals in Spain. Vet Rec 188:e60. doi: 10.1002/vetr.60. [DOI] [PubMed] [Google Scholar]
- 15.Johnson J, Johnston B, Clabots C, Kuskowski M, Roberts E, DebRoy C. 2008. Virulence genotypes and phylogenetic background of Escherichia coli serogroup O6 isolates from humans, dogs, and cats. J Clin Microbiol 46:417–422. doi: 10.1128/JCM.00674-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johnson JR, Clabots C, Kuskowski MA. 2008. Multiple-host sharing, long-term persistence, and virulence of Escherichia coli clones from human and animal household members. J Clin Microbiol 46:4078–4082. doi: 10.1128/JCM.00980-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thompson MF, Litster AL, Platell JL, Trott DJ. 2011. Canine bacterial urinary tract infections: new developments in old pathogens. Vet J 190:22–27. doi: 10.1016/j.tvjl.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 18.Valat C, Drapeau A, Beurlet S, Bachy V, Boulouis H-J, Pin R, Cazeau G, Madec J-Y, Haenni M. 2020. Pathogenic Escherichia coli in dogs reveals the predominance of ST372 and the human-associated ST73 extra-intestinal lineages. Front Microbiol 11:580. doi: 10.3389/fmicb.2020.00580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Toombs-Ruane LJ, Benschop J, French NP, Biggs PJ, Midwinter AC, Marshall JC, Chan M, Drinković D, Fayaz A, Baker MG, Douwes J, Roberts MG, Burgess SA. 020. Carriage of extended-spectrum-beta-lactamase- and AmpC beta-lactamase-producing Escherichia coli strains from humans and pets in the same households. Appl Environ Microbiol 86. doi: 10.1128/AEM.01613-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Day MJ, Hopkins KL, Wareham DW, Toleman MA, Elviss N, Randall L, Teale C, Cleary P, Wiuff C, Doumith M, Ellington MJ, Woodford N, Livermore DM. 2019. Extended-spectrum β-lactamase-producing Escherichia coli in human-derived and food chain-derived samples from England, Wales, and Scotland: an epidemiological surveillance and typing study. Lancet Infect Dis 19:1325–1335. doi: 10.1016/S1473-3099(19)30273-7. [DOI] [PubMed] [Google Scholar]
- 21.Manges AR. 2019. Escherichia coli causing bloodstream and other extraintestinal infections: tracking the next pandemic. Lancet Infect Dis 19:1269–1270. doi: 10.1016/S1473-3099(19)30538-9. [DOI] [PubMed] [Google Scholar]
- 22.Cummins ML, Reid CJ, Djordjevic SP. 2022. F plasmid lineages in Escherichia coli ST95: implications for host range, antibiotic resistance, and zoonoses. mSystems 7:e0121221. doi: 10.1128/msystems.01212-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li D, Wyrsch ER, Elankumaran P, Dolejska M, Marenda MS, Browning GF, Bushell RN, McKinnon J, Chowdhury PR, Hitchick N, Miller N, Donner E, Drigo B, Baker D, Charles IG, Kudinha T, Jarocki VM, Djordjevic SP. 2021. Genomic comparisons of Escherichia coli ST131 from Australia. Microb Genom 7. doi: 10.1099/mgen.0.000721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nesporova K, Wyrsch ER, Valcek A, Bitar I, Chaw K, Harris P, Hrabak J, Literak I, Djordjevic SP, Dolejska M. 2020. Escherichia coli sequence type 457 is an emerging extended-spectrum-β-lactam-resistant lineage with reservoirs in wildlife and food-producing animals. Antimicrob Agents Chemother 65. doi: 10.1128/AAC.01118-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reid CJ, Cummins ML, Börjesson S, Brouwer MSM, Hasman H, Hammerum AM, Roer L, Hess S, Berendonk T, Nešporová K, Haenni M, Madec J-Y, Bethe A, Michael GB, Schink A-K, Schwarz S, Dolejska M, Djordjevic SP. 2022. A role for ColV plasmids in the evolution of pathogenic Escherichia coli ST58. Nat Commun 13:683. doi: 10.1038/s41467-022-28342-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reid CJ, McKinnon J, Djordjevic SP. 2019. Clonal ST131-H22 Escherichia coli strains from a healthy pig and a human urinary tract infection carry highly similar resistance and virulence plasmids. Microb Genom 5. doi: 10.1099/mgen.0.000295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cusumano CK, Hung CS, Chen SL, Hultgren SJ. 2010. Virulence plasmid harbored by uropathogenic Escherichia coli functions in acute stages of pathogenesis. Infect Immun 78:1457–1467. doi: 10.1128/IAI.01260-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moran RA, Hall RM. 2018. Evolution of regions containing antibiotic resistance genes in FII-2-FIB-1 ColV-Colla virulence plasmids. Microb Drug Resist 24:411–421. doi: 10.1089/mdr.2017.0177. [DOI] [PubMed] [Google Scholar]
- 29.Galardini M, Clermont O, Baron A, Busby B, Dion S, Schubert S, Beltrao P, Denamur E. 2020. Major role of iron uptake systems in the intrinsic extra-intestinal virulence of the genus Escherichia revealed by a genome-wide association study. PLoS Genet 16:e1009065. doi: 10.1371/journal.pgen.1009065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Searle LJ, Méric G, Porcelli I, Sheppard SK, Lucchini S. 2015. Variation in siderophore biosynthetic gene distribution and production across environmental and faecal populations of Escherichia coli. PLoS One 10:e0117906. doi: 10.1371/journal.pone.0117906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Denamur E, Clermont O, Bonacorsi S, Gordon D. 2021. The population genetics of pathogenic Escherichia coli. Nat Rev Microbiol 19:37–54. doi: 10.1038/s41579-020-0416-x. [DOI] [PubMed] [Google Scholar]
- 32.Flament-Simon S-C, de Toro M, García V, Blanco JE, Blanco M, Alonso MP, Goicoa A, Díaz-González J, Nicolas-Chanoine M-H, Blanco J. 2020. Molecular characteristics of extraintestinal pathogenic E. coli (ExPEC), uropathogenic E. coli (UPEC), and multidrug resistant E. coli isolated from healthy dogs in Spain. Whole genome sequencing of canine ST372 isolates and comparison with human isolates causing extraintestinal infections. Microorganisms 8:1712. doi: 10.3390/microorganisms8111712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.LeCuyer TE, Byrne BA, Daniels JB, Diaz-Campos DV, Hammac GK, Miller CB, Besser TE, Davis MA. 2018. Population structure and antimicrobial resistance of canine uropathogenic Escherichia coli. J Clin Microbiol 56:e00788-18. doi: 10.1128/JCM.00788-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Adler A, Gniadkowski M, Baraniak A, Izdebski R, Fiett J, Hryniewicz W, Malhota-Kumar S, Goossens H, Lammens C, Lerman Y, Kazma M, Kotlovsky T, Carmeli Y, MOSAR WP5 and WP2 Study Groups . 2012. Transmission dynamics of ESBL-producing Escherichia coli clones in rehabilitation wards at a tertiary care centre. Clin Microbiol Infect 18:E497–505. doi: 10.1111/j.1469-0691.2012.03999.x. [DOI] [PubMed] [Google Scholar]
- 35.Izdebski R, Baraniak A, Fiett J, Adler A, Kazma M, Salomon J, Lawrence C, Rossini A, Salvia A, Vidal Samso J, Fierro J, Paul M, Lerman Y, Malhotra-Kumar S, Lammens C, Goossens H, Hryniewicz W, Brun-Buisson C, Carmeli Y, Gniadkowski M, MOSAR WP2 and WP5 Study Groups . 2013. Clonal structure, extended-spectrum β-lactamases, and acquired AmpC-type cephalosporinases of Escherichia coli populations colonizing patients in rehabilitation centers in four countries. Antimicrob Agents Chemother 57:309–316. doi: 10.1128/AAC.01656-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hastak P, Cummins ML, Gottlieb T, et al. 2020. Genomic profiling of Escherichia coli isolates from bacteraemia patients: a 3-year cohort study of isolates collected at a Sydney teaching hospital. Microb Genom 6. doi: 10.1099/mgen.0.000371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li D, Reid CJ, Kudinha T, Jarocki VM, Djordjevic SP. 2020. Genomic analysis of trimethoprim-resistant extraintestinal pathogenic Escherichia coli and recurrent urinary tract infections. Microb Genom 6. doi: 10.1099/mgen.0.000475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Royer G, Darty MM, Clermont O, Condamine B, Laouenan C, Decousser J-W, Vallenet D, Lefort A, de Lastours V, Denamur E, COLIBAFI and SEPTICOLI groups . 2021. Phylogroup stability contrasts with high within sequence type complex dynamics of Escherichia coli bloodstream infection isolates over a 12-year period. Genome Med 13:77. doi: 10.1186/s13073-021-00892-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alhashash F, Wang X, Paszkiewicz K, Diggle M, Zong Z, McNally A. 2016. Increase in bacteraemia cases in the East Midlands region of the UK due to MDR Escherichia coli ST73: high levels of genomic and plasmid diversity in causative isolates. J Antimicrob Chemother 71:339–343. doi: 10.1093/jac/dkv365. [DOI] [PubMed] [Google Scholar]
- 40.Kallonen T, Brodrick HJ, Harris SR, Corander J, Brown NM, Martin V, Peacock SJ, Parkhill J. 2017. Systematic longitudinal survey of invasive Escherichia coli in England demonstrates a stable population structure only transiently disturbed by the emergence of ST131. Genome Res 27:1437–1449. doi: 10.1101/gr.216606.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kidsley AK, O'Dea M, Ebrahimie E, Mohammadi-Dehcheshmeh M, Saputra S, Jordan D, Johnson JR, Gordon D, Turni C, Djordjevic SP, Abraham S, Trott DJ. 2020. Genomic analysis of fluoroquinolone-susceptible phylogenetic group B2 extraintestinal pathogenic Escherichia coli causing infections in cats. Vet Microbiol 245:108685. doi: 10.1016/j.vetmic.2020.108685. [DOI] [PubMed] [Google Scholar]
- 42.Kidsley AK, White RT, Beatson SA, Saputra S, Schembri MA, Gordon D, Johnson JR, O'Dea M, Mollinger JL, Abraham S, Trott DJ. 2020. Companion animals are spillover hosts of the multidrug-resistant human extraintestinal Escherichia coli pandemic clones ST131 and ST1193. Front Microbiol 11:1968. doi: 10.3389/fmicb.2020.01968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lipworth S, Vihta K-D, Chau K, Barker L, George S, Kavanagh J, Davies T, Vaughan A, Andersson M, Jeffery K, Oakley S, Morgan M, Hopkins S, Peto TEA, Crook DW, Walker AS, Stoesser N. 2021. Ten-year longitudinal molecular epidemiology study of Escherichia coli and Klebsiella species bloodstream infections in Oxfordshire, UK. Genome Med 13:144. doi: 10.1186/s13073-021-00947-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Matsui Y, Hu Y, Rubin J, de Assis RS, Suh J, Riley LW. 2020. Multilocus sequence typing of Escherichia coli isolates from urinary tract infection patients and from fecal samples of healthy subjects in a college community. Microbiologyopen 9:1225–1233. doi: 10.1002/mbo3.1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bogema DR, McKinnon J, Liu M, Hitchick N, Miller N, Venturini C, Iredell J, Darling AE, Chowdhury PR, Djordjevic SP. 2020. Whole-genome analysis of extraintestinal Escherichia coli sequence type 73 from a single hospital over a 2 year period identified different circulating clonal groups. Microb Genom 6. doi: 10.1099/mgen.0.000255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Flament-Simon SC, García V, Duprilot M, Mayer N, Alonso MP, Garcia-Menino I, Blanco JE, Blanco M, Nicolas-Chanoine M-H, Blanco J. 2020. High prevalence of ST131 subclades C2-H30Rx and C1-M27 among extended-spectrum β-lactamase-producing Escherichia coli causing human extraintestinal infections in patients from two hospitals of Spain and France during 2015. Front Cell Infect Microbiol 10:125. doi: 10.3389/fcimb.2020.00125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Flament-Simon S-C, Nicolas-Chanoine M-H, García V, Duprilot M, Mayer N, Alonso MP, García-Meniño I, Blanco JE, Blanco M, Blanco J. 2020. Clonal structure, virulence factor-encoding genes and antibiotic resistance of Escherichia coli, causing urinary tract infections and other extraintestinal infections in humans in Spain and France during 2016. Antibiotics (Basel) 9:161. doi: 10.3390/antibiotics9040161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Reid CJ, Blau K, Jechalke S, Smalla K, Djordjevic SP. 2019. Whole genome sequencing of Escherichia coli from store-bought produce. Front Microbiol 10:3050. doi: 10.3389/fmicb.2019.03050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cummins ML, Reid CJ, Roy Chowdhury P, et al. 2019. Whole genome sequence analysis of Australian avian pathogenic Escherichia coli that carry the class 1 integrase gene. Microb Genom 5. doi: 10.1099/mgen.0.000250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mageiros L, Méric G, Bayliss SC, Pensar J, Pascoe B, Mourkas E, Calland JK, Yahara K, Murray S, Wilkinson TS, Williams LK, Hitchings MD, Porter J, Kemmett K, Feil EJ, Jolley KA, Williams NJ, Corander J, Sheppard SK. 2021. Genome evolution and the emergence of pathogenicity in avian Escherichia coli. Nat Commun 12:765. doi: 10.1038/s41467-021-20988-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Martinez-Anton L, Marenda M, Firestone SM, Bushell RN, Child G, Hamilton AI, Long SN, Le Chevoir MAR. 2018. Investigation of the role of Campylobacter infection in suspected acute polyradiculoneuritis in dogs. J Vet Intern Med 32:352–360. doi: 10.1111/jvim.15030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McKinnon J, Roy Chowdhury P, Djordjevic SP. 2018. Genomic analysis of multidrug-resistant Escherichia coli ST58 causing urosepsis. Int J Antimicrob Agents 52:430–435. doi: 10.1016/j.ijantimicag.2018.06.017. [DOI] [PubMed] [Google Scholar]
- 53.Johnson TJ. 2021. Role of plasmids in the ecology and evolution of “high-risk” extraintestinal pathogenic Escherichia coli clones. EcoSal Plus 9. doi: 10.1128/ecosalplus.ESP-0013-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stephens CM, Adams-Sapper S, Sekhon M, Johnson JR, Riley LW. 2017. Genomic analysis of factors associated with low prevalence of antibiotic resistance in extraintestinal pathogenic Escherichia coli sequence type 95 strains. mSphere 2. doi: 10.1128/mSphere.00390-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dawes FE, Kuzevski A, Bettelheim KA, Hornitzky MA, Djordjevic SP, Walker MJ. 2010. Distribution of class 1 integrons with IS26-mediated deletions in their 3'-conserved segments in Escherichia coli of human and animal origin. PLoS One 5:e12754. doi: 10.1371/journal.pone.0012754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.McKinnon J, Roy Chowdhury P, Djordjevic SP. 2020. Molecular analysis of an IncF ColV-like plasmid lineage that carries a complex resistance locus with a trackable genetic signature. Microb Drug Resist 26:787–793. doi: 10.1089/mdr.2019.0277. [DOI] [PubMed] [Google Scholar]
- 57.Dazio V, Nigg A, Schmidt JS, Brilhante M, Mauri N, Kuster SP, Brawand SG, Schüpbach-Regula G, Willi B, Endimiani A, Perreten V, Schuller S. 2021. Acquisition and carriage of multidrug-resistant organisms in dogs and cats presented to small animal practices and clinics in Switzerland. J Vet Intern Med 35:970–979. doi: 10.1111/jvim.16038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Liu FL, Kuan NL, Yeh KS. 2021. Presence of the extended-spectrum-β-lactamase and plasmid-mediated AmpC-encoding genes in Escherichia coli from companion animals—a study from a university-based veterinary hospital in Taipei, Taiwan. Antibiotics (Basel) 10:1536. doi: 10.3390/antibiotics10121536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Peirano G, Matsumara Y, Nobrega D, DeVinney R, Pitout J. 2021. Population-based epidemiology of Escherichia coli ST1193 causing blood stream infections in a centralized Canadian region. Eur J Clin Microbiol Infect Dis doi: 10.1007/s10096-021-04373-5. [DOI] [PubMed] [Google Scholar]
- 60.Gaio D, To J, Liu M, Monahan L, Anantanawat K, Darling AE. 2019. Hackflex: low cost Illumina sequencing library construction for high sample counts. bioRxiv:779215. doi: 10.1101/779215. [DOI]
- 61.Koster J, Rahmann S. 2012. Snakemake–a scalable bioinformatics workflow engine. Bioinformatics 28:2520–2522. doi: 10.1093/bioinformatics/bts480. [DOI] [PubMed] [Google Scholar]
- 62.Carattoli A, Zankari E, García-Fernández A, Voldby Larsen M, Lund O, Villa L, Møller Aarestrup F, Hasman H. 2014. In silico detection and typing of plasmids using PlasmidFinder and plasmid multilocus sequence typing. Antimicrob Agents Chemother 58:3895–3903. doi: 10.1128/AAC.02412-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chen SL, Hung C-S, Xu J, Reigstad CS, Magrini V, Sabo A, Blasiar D, Bieri T, Meyer RR, Ozersky P, Armstrong JR, Fulton RS, Latreille JP, Spieth J, Hooton TM, Mardis ER, Hultgren SJ, Gordon JI. 2006. Identification of genes subject to positive selection in uropathogenic strains of Escherichia coli: a comparative genomics approach. Proc Natl Acad Sci USA 103:5977–5982. doi: 10.1073/pnas.0600938103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ingle DJ, Valcanis M, Kuzevski A, Tauschek M, Inouye M, Stinear T, Levine MM, Robins-Browne RM, Holt KE. 2016. In silico serotyping of E. coli from short read data identifies limited novel O-loci but extensive diversity of O:H serotype combinations within and between pathogenic lineages. Microb Genom 2:e000064. doi: 10.1099/mgen.0.000064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jia B, Raphenya AR, Alcock B, Waglechner N, Guo P, Tsang KK, Lago BA, Dave BM, Pereira S, Sharma AN, Doshi S, Courtot M, Lo R, Williams LE, Frye JG, Elsayegh T, Sardar D, Westman EL, Pawlowski AC, Johnson TA, Brinkman FSL, Wright GD, McArthur AG. 2017. CARD 2017: expansion and model-centric curation of the comprehensive antibiotic resistance database. Nucleic Acids Res 45:D566–D573. doi: 10.1093/nar/gkw1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Siguier P, Perochon J, Lestrade L, Mahillon J, Chandler M. 2006. ISfinder: the reference centre for bacterial insertion sequences. Nucleic Acids Res 34:D32–D36. doi: 10.1093/nar/gkj014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Carattoli A, Hasman H. 2020. PlasmidFinder and in silico pMLST: identification and typing of plasmid replicons in whole-genome sequencing (WGS). Methods Mol Biol 2075:285–294. doi: 10.1007/978-1-4939-9877-7_20. [DOI] [PubMed] [Google Scholar]
- 68.Zankari E, Allesøe R, Joensen KG, Cavaco LM, Lund O, Aarestrup FM. 2017. PointFinder: a novel web tool for WGS-based detection of antimicrobial resistance associated with chromosomal point mutations in bacterial pathogens. J Antimicrob Chemother 72:2764–2768. doi: 10.1093/jac/dkx217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Liu CM, Stegger M, Aziz M, Johnson TJ, Waits K, Nordstrom L, Gauld L, Weaver B, Rolland D, Statham S, Horwinski J, Sariya S, Davis GS, Sokurenko E, Keim P, Johnson JR, Price LB. 2018. Escherichia coli ST131- H 22 as a foodborne uropathogen. mBio 9. doi: 10.1128/mBio.00470-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Seemann T. 2014. Prokka: rapid prokaryotic genome annotation. Bioinformatics 30:2068–2069. doi: 10.1093/bioinformatics/btu153. [DOI] [PubMed] [Google Scholar]
- 71.Page AJ, Cummins CA, Hunt M, Wong VK, Reuter S, Holden MTG, Fookes M, Falush D, Keane JA, Parkhill J. 2015. Roary: rapid large-scale prokaryote pan genome analysis. Bioinformatics 31:3691–3693. doi: 10.1093/bioinformatics/btv421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nguyen LT, Schmidt HA, von Haeseler A, Minh BQ. 2015. IQ-TREE: a fast and effective stochastic algorithm for estimating maximum-likelihood phylogenies. Mol Biol Evol 32:268–274. doi: 10.1093/molbev/msu300. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material. Download spectrum.01291-22-s0001.pdf, PDF file, 5.6 MB (5.7MB, pdf)
Supplemental material. Download spectrum.01291-22-s0002.csv, CSV file, 0.6 MB (673.4KB, csv)
Data Availability Statement
All genomes used in this study were deposited in GenBank and the Sequence Read Archive under the BioProject PRJNA678027. Individual accession numbers can be found with comprehensive metadata and genomic data in Table S1. The data analysis and visualization script are freely available at https://github.com/CJREID/MVC and can be used to reproduce all secondary analyses. R package versions used therein are available within the README.md document in the code repository.