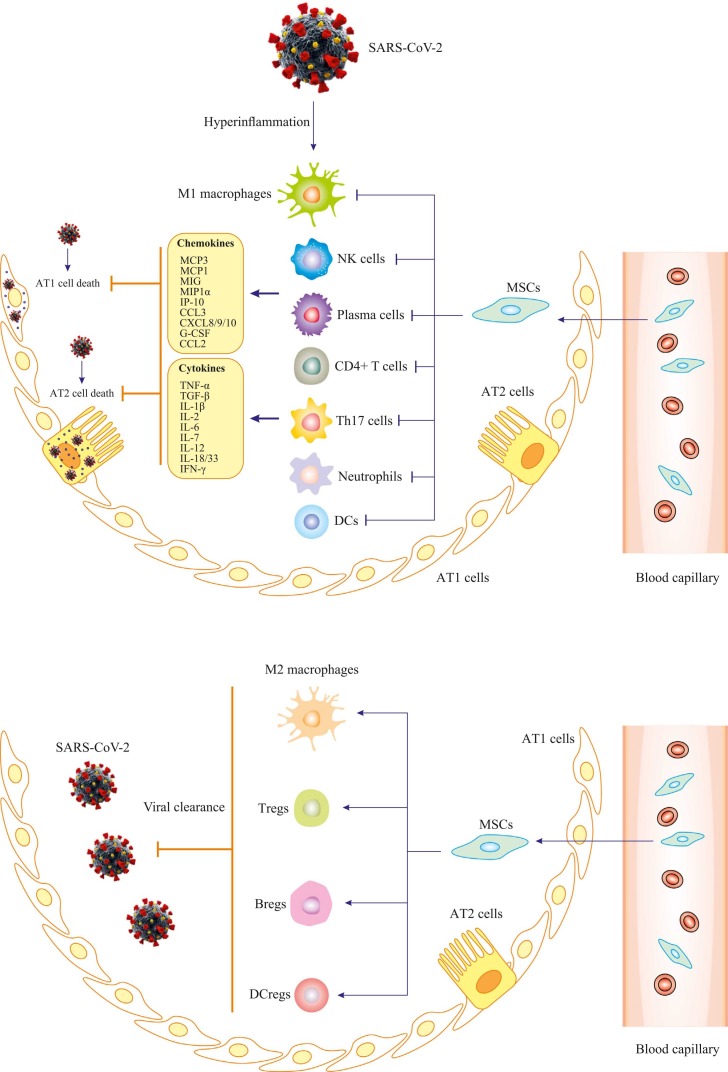
Fig. 2.
Proposed mechanisms for MSCs function in severe COVID-19 patients. Firstly, SARS-CoV-2 infects respiratory tract; infiltration of immune cells (monocytes/macrophages, neutrophils, natural killer cells, T cells and B cells) increases; then cytokine storm (such as TNF‐α, IL-2, IL-6, MCP1 and IP10) occurs. Hyaline membrane formation, cellular fibrous mucinous exudation and diffuse alveolar damage develop. After stem cells administration, the number of infiltrated immune cells significantly reduces, and damaged lung tissue is repaired. MSCs have properties of anti-inflammation, immunoregulation and tissue regeneration, although detailed mechanisms underlying these roles remain to be further elucidated. MCP3, monocyte-chemotactic protein 3; MCP1, monocyte-chemotactic protein 1; MIG, monokine induced by gamma; MIP1α, macrophage inflammatory protein 1α; IP-10, interferon gamma-induced protein 10; CCL3, C-C motif chemokine ligand 3; CXCL8/9/10, C-X-C motif chemokine ligand 8/9/10; G-CSF, granulocyte colony-stimulating factor; CCL2, C-C motif chemokine ligand 2; IL-1β, IL-1 beta protein; IFN-γ, interferon gamma; NK cells, natural killer cells; DCs, dendritic cells; Th17, T helper 17 cells; Tregs, T regulatory cells; Bregs, B regulatory cells.