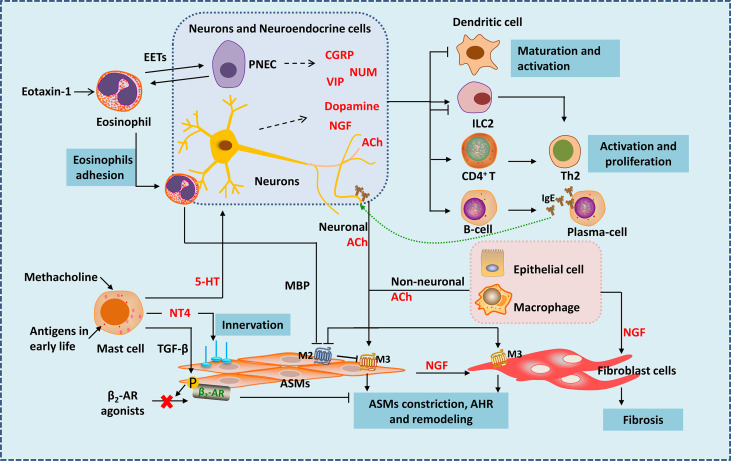
Figure 1.
Neuro-immune interactions in inflammation and airway remodeling of allergic asthma. Eosinophils migrate to airway during inflammation via eotaxin-1. They release EETs surrounding and activating PNECs. Under the action of VLA-4 and CD11b, eosinophils adhere to VCAM-1 and ICAM-1 on parasympathetic fibers. Eosinophils are then activated and release MBP, which is an antagonist of M2 muscarinic receptor, thus enhancing parasympathetic mediated bronchoconstriction. Besides, eosinophils increase airway innervation. Under the stimulation of methacholine, mast cells release 5-HT, interacting with 5-HT2 receptors in parasympathetic nerves, thus release ACh (neuronal ACh), enhancing bronchoconstriction. Mast cells also produce NT4 following allergen exposure during early-life, increasing ASMs innervation through NT4/TrkB signaling, causing long-term airway dysfunction. Mast cells also produce TGF-β to induce β2-AR phosphorylation in ASMs, thereby causing β2-AR agonists resistance. Neuropeptides generate form neurons and neuroendocrine cells such as NMU and VIP activate ILC2s. CGRP generated mainly from PNECs inhibits maturation of DCs, it may have bidirectional effects on ILC2s. Besides neuronal ACh, non-neuronal ACh released from epithelia cells and macrophages mainly acted in small airways. ACh activate muscarinic 3 acetylcholine receptor on ASMs and fibroblast cells, causing airway contraction and airway remodeling. NGF released from neurons, epithelial cells, ASMs and other immune cells acts on fibroblasts leading to fibrosis. NGF can also activate Th2 cells and promote the differentiation of B cells into plasma cells. EETS, Eosinophil extracellular traps; PNEC, pulmonary neuroendocrine cell; MBP, major basic protein; 5-HT, 5-hydroxytryptamine; ACh, acetylcholine; NT4, neurotrophin 4; ASMs, airway smooth muscle cells; NGF, nerve growth factor.