Abstract
Effective pain control enables procedural success and improved patient satisfaction in interventional radiology. Regional anesthesia techniques are now established for intraoperative and postoperative anesthesia during major surgery, and interventional radiologists (IRs) can readily apply these injections for intraprocedural nerve blocks that can reduce anesthetic requirements and ensure durable analgesia postprocedure. Moreover, IR is poised to advance this field with novel blocks unique to IR needs and by blocking deep plexi safely reachable with CT guidance (e.g., hepatic hilar plexus, aorticorenal plexus blocks). This report aims to provide a succinct IR-directed primer for image-guided nerve blocks usable in the interventional radiology suite.
Keywords: interventional radiology, cancer pain, pain management, analgesia, nerve block
As interventional radiology performs increasingly complex procedures in an increasingly fragile patient population, in many cases palliating cancer pain, and as procedural trends lean toward outpatient and office-based practice, there is a growing desire to expand intraprocedural analgesia beyond basic intravenous moderate sedation. This report aims to provide an IR-directed primer on nerve blocks that can be performed by the interventional radiologist (IR) to assist with intraprocedural pain control.
Although intravenous moderate sedation is safe and effective, more patients are seeking IR procedures to palliate painful conditions (such as intractable cancer pain or critical limb ischemia) and moderate sedation may not provide effective procedural sedation and pain control especially if the patient is already on high opioid doses prior to their procedure. Furthermore, the patient may not be a safe candidate for general anesthesia or general anesthesia availability may be limited. As IR performs increasingly complex procedures on increasingly complex patients, nerve blocks can help keep outpatient procedures in the outpatient setting and provide a stable patient on whom the operator can perform the intended intervention.
Nerve Blocks: Fundamentals
Understanding both the basics and nuances of nerve blockade is critical for interventionalists. As we often discuss colloquially with patients, the nerve blocks keep pain signals from reaching the brain, but they also interfere with other sensory, motor, and autonomic signaling. Nerve blocks then can interrupt all electrical signal along axons that conduct stimulation from structures in the periphery back and forth from the central nervous systems. 1 The conceptual simplicity of a block belies the complexity of the permutations possible, as the injectates, additives, volumes, and nerves to target create an array of ever expanding options.
The primary agents used in nerve blocks target sodium channels on the surface of the axons or soma of the cell body. 2 These are the local anesthetics such as lidocaine, bupivacaine, and ropivacaine which are commonly used amide class local anesthetics. For the rare patients with allergies to amide anesthetics, ester-based anesthetics such as 2-chloroprocaine or tetracaine are commonly available, although some providers would prefer to utilize alternative agents such as 1% diphenhydramine. 3 The local anesthetics agents all work through an intracellular blockade of the sodium transport which propagates an action potential in neurons. They all diffuse into the cell as a function of the local pH, the concentration of the drug used, and the size/composition of the membrane they are diffusing through. Thus, a given local anesthetic will block small diameter unmyelinated sensory nerves faster than larger, myelinated motor nerves of the brachial plexus.
The chemical characteristics and concentration of the agent as well as the milieu of the injection field also impact the diffusion of the local anesthetic to the target site. Although local anesthetics exist in solution as a charged quaternary salt and an uncharged tertiary base, the base is the molecule which diffuses across the plasma membrane into the cell, while the quaternary salt must reform intracellularly to block the sodium channel. 2 The acidicity or lack thereof of the tissue or the injectate as compared with the pK a of the drug will then effect the concentration of the base available to diffuse into an axon. This is the mechanism underlying sodium bicarbonate addition to agents such as lidocaine or bupivacaine. 4 It may also be the mechanism underlying less than optimal analgesia encounter when injecting local anesthetic into acidic environments such as the ischemic penumbra of a metabolically active tumor or an abscess. For large nerves such as those of the brachial plexus, this is a critical factor in the speed of onset and quality of the block, as even a fast-acting agent such as lidocaine can take 13 minutes to take effect, while a slower onset agent such as bupivacaine can take 16 to 17 minutes. 5 Usage of higher concentrations and buffered injectates would be expected to reduce these times.
There are many other additional adjuvants injected that provide different effects to augment a block. 6 The most common is epinephrine which provides both a marker of intravascular injection and a means to vasoconstrict perineural vasculature to prolong the duration of a block. Many other adjuvants including clonidine, dexmedetomidine, opioids, benzodiazepines, nonsteroidal anti-inflammatory drugs, and steroids have been used. Of these, in common clinical practice dexamethasone has been rapidly adopted at a dose of 1 to 4 mg to prolong the analgesic effect of a nerve block. Regardless of the adjuvants, however, the majority of the effect is mediated by the local anesthetic chosen and its kinetics.
When a block is performed, it is also critical to understand the goals of the injection both in terms of the target and the end effect desired. A nerve block with low concentrations of 0.5 to 1% lidocaine may be sufficient to provide analgesia for a skin incision. A higher concentration of 1 to 1.5% may be needed for a motor block of a large mixed sensorimotor nerve such as the sciatic. In some scenarios, a lower concentration with a higher volume may be sufficient; however, with the increased volume supplementing for the lower concentration but expecting a dense sensory block with low concentrations may be foolish. The higher volume exposes a greater length of the nerve to local anesthetic, which can significantly reduce the concentration required for a conductive block. 7 Targeted nerve blocks may be performed with as little as 0.1 to 0.15 mL per mm 2 of cross-sectional nerve area depending on the nerve. 8 9 10 However, many providers are now utilizing fascial plane blocks which allow for reduced targeting of individual nerves by injecting within a tissue plane which contains many of the target nerves. 1 11 These injections are generally higher volume blocks of 20 to 40 mL, providing a high probability of coverage of multiple regions with the higher volumes.
These higher volumes and larger surface areas of a region exposed in fascial plane blocks may provide novel mechanisms of analgesia as compared with conventional nerve blocks. 1 It may also create an increased risk for certain tenuous patients who are more prone to local anesthetic systemic toxicity, as the systemic concentrations of local anesthetic from fascial plane blocks may mimic that of intravenous local anesthetic infusions. These patients with known seizure disorders, 12 preexisting cardiac disease, old age, malnutrition with hypoalbuminemia, poor hepatic or renal function, and acidemia are more likely to be adversely sensitive to local anesthetics. 13 These are generally risk/benefit discussion points more so than absolute contraindications, but one may opt to at least be more conservative on the total amount of local anesthetic used to stay well below toxic doses.
Specific Nerve Blocks
Pectoralis Plane Block
Mastectomy and thoracotomy are often preceded by a bedside ultrasound-guided plane block called the pectoralis plane block. IR applications include ablation of chest wall and breast tumors, extra-anatomic venous shunt creation in the axilla and chest, Denver shunt placement, and pleural catheter installation.
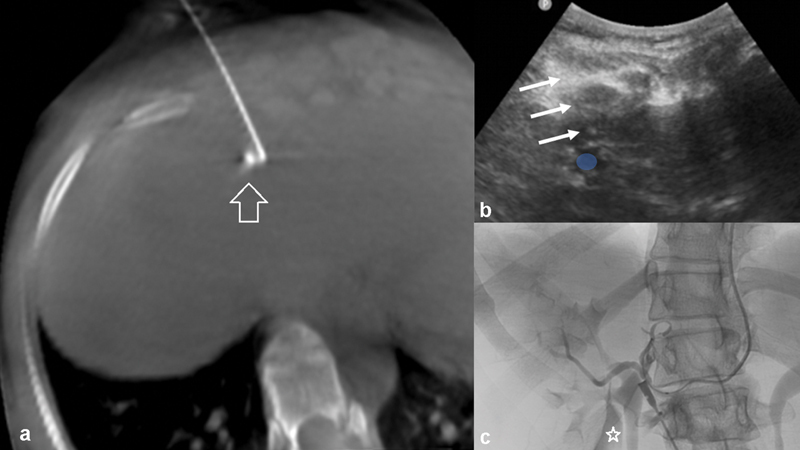
The target for injection is the interfascial plane between the pectoralis minor and major muscles (PECS 1 block) which can be upgraded with an additional injection one layer deeper into the interfascial plane between pectoralis minor and serratus anterior muscles at the level of rib 4 (PECS 2 block). These are shown in the CT image ( Fig. 1 ). The target total volume for each respective block is generally accepted to be 0.2 mL/kg of long-acting local anesthetic.
Fig. 1.
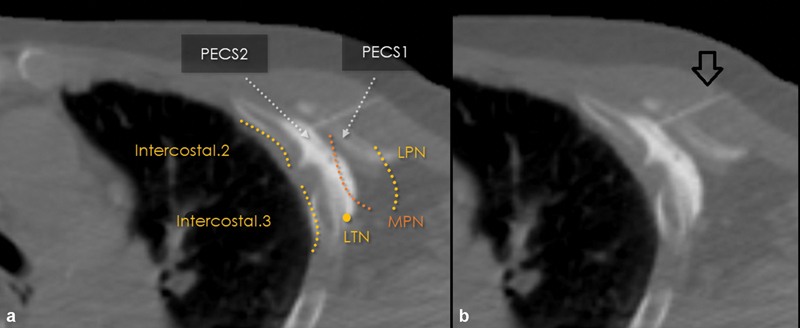
CT-guided PECS-2 nerve block. Images ( a , with annotations; b , without annotations) demonstrate needle placement (arrow, b ) and course of the relevant nerves in this axial CT image of the chest prior to ablation of chest wall tumor. LPN, lateral pectoral nerve; LTN, long thoracic nerve; MPN, medial pectoral nerve.
PECS 1 includes the medial pectoral nerve (MPN) and lateral pectoral nerve (LPN), both branches of the brachial plexus. As there is motor supply to the pectoralis muscles, the patient should be informed of the potential for muscle weakness until the block wears off.
PECS 2 includes the MPN and LPN and then dives to the deeper second interfascial compartment between pectoralis minor and serratus anterior to include the sensory branches that arise to the axilla and chest from the intercostal nerves.
Intercostal Nerve Block
The intercostal nerves supply sensory dermatomes of the corresponding thoracic vertebra and this nerve block is helpful for chest wall interventions and also hepatic interventions, as terminal fibers of the intercostal nerves supply nerves in the hepatic Glisson capsule. Intercostal nerve blocks can be a prelude to intercostal cryoneurolysis, for example, including a small volume of dexamethasone to provide longer block duration for any potential deafferentation pain.
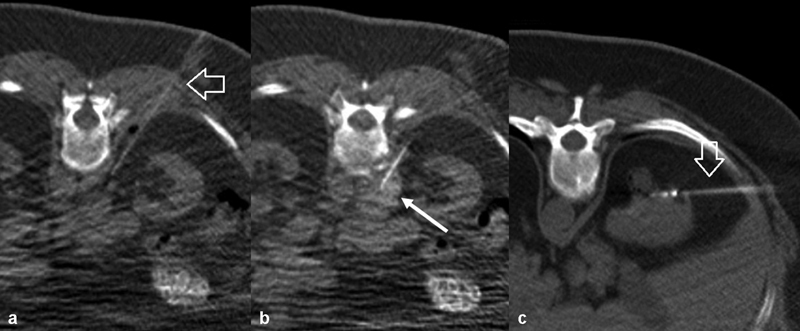
The target for injection is the subcostal space at each level intended to provide analgesia as seen in Figs. 2 and 3 . The point of injection can occur at any point along the rib; though posterior and lateral to the transverse process will allow approximately 5 mL of injectate to be deposited before it spreads medially toward the epidural space, further laterally larger volumes such as 10 mL can be injected allowing spread along the internal thoracic fascia and potentially numbing of adjacent intercostal levels as well. The injection can be repeated for multiple contiguous ribs (e.g., numbing each rib with overlap of the liver prior to a right hepatic embolization for liver metastases) and the allowable injection would correspond to weight-based limits for the chosen medications (usually lidocaine with epinephrine, bupivacaine, and possibly preservative-free dexamethasone).
Fig. 2.
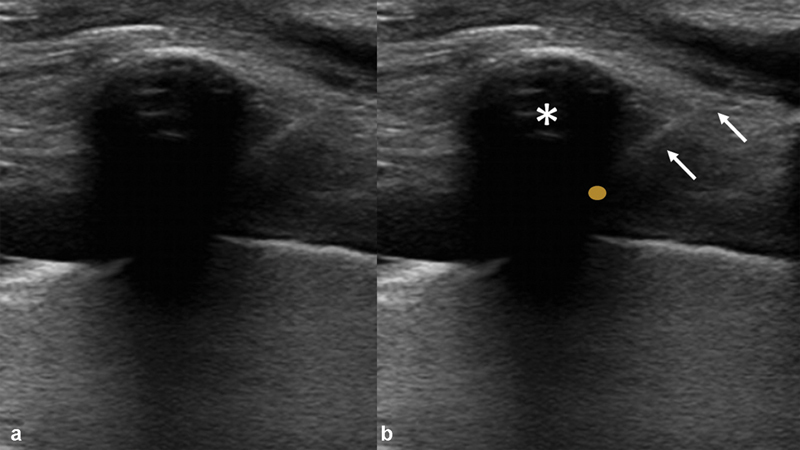
Ultrasound-guided intercostal nerve block images ( a , without annotations; b , with annotations) show axial in the sagittal plane with rib (*) and intercostal nerve (yellow dot) and 25-gauge needle (arrows) directed to the subcostal space for injection.
Fig. 3.
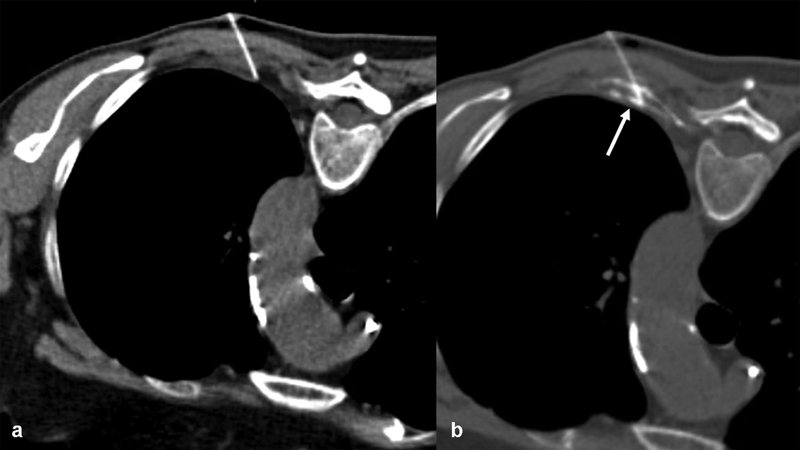
CT-guided intercostal nerve block images ( a , without annotations; b , with annotations) with 25-gauge needle, injectate containing contrast is seen spreading along the subcostal space favorably ( b , arrow).
In patients who have had prior radiotherapy for thoracic tumors, the injectate may not have the desired spread. In these cases, a paravertebral block can be considered (injecting a step more centrally) and depending on the planned procedure, adjacent level intercostal blocks can be added (as there is known collateral sensory innervation across adjacent rib levels especially for the anterior chest where neural arborization is most prevalent).
Paravertebral Plane Block
Paravertebral blocks are an established technique of regional anesthesia providing coverage for multiple spinal nerves as they emerge from the intervertebral foramen on one side of the spinal column, for example, used in the context of breast surgery. The expected outcome includes a somatic blockade in addition to a sympathetic blockade (for thoracic paravertebral blocks). The sympathetic nervous system can carry pain signals, so this is favorable; however, there may also be hemodynamic consequences (subdiaphragmatic engorgement of the capacitance vessels may lead to orthostatic hypotension or frank hypotension though, unlikely for a unilateral block). This block has also been described for hepatic interventions since it covers both the sympathetic and intercostal contributions to the liver (for procedures such as biliary drainage and tumor ablation). Of note, paravertebral blocks do not result in motor weakness of the arms or legs.
The injection target is the space lateral to the vertebral body as seen in Fig. 4 . The paravertebral space communicates with both the intercostal space and the epidural space. So, while a paravertebral block with large volume (20–25 mL) can cover multiple adjacent level intercostal nerves, it also can lead to unintended epidural injection and monitoring by CT is helpful. Alternatively, multiple paravertebral spaces can be accessed with 5 mL of injectate at each level. The maximum dose of local anesthetic is chosen based on patient factors (age, weight, general condition). Including epinephrine in the injectate benefits here by causing vasoconstriction and limiting systemic absorption (which increases risk of toxicity and also reduces the duration of the block since the block medication gets rapidly absorbed).
Fig. 4.
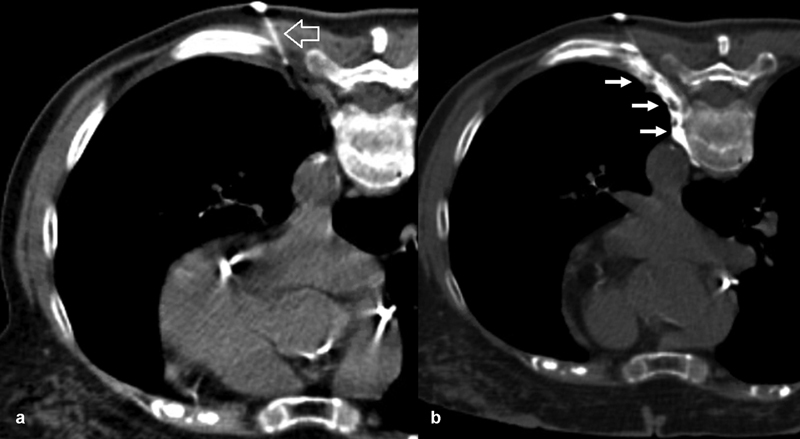
CT-guided paravertebral nerve block with 25-gauge needle ( a , arrow), injectate containing contrast is seen spreading along the paravertebral space favorably ( b , arrows).
Hepatic Hilar Plane Block
The distribution of cutaneous sensory innervation (dermatomes) remains very well delineated, while, unfortunately, such pain distribution for the liver (hepatotomes) remains understudied. As is already known, pain is carried along the autonomic nervous system which also modulates hepatic metabolic crosstalk with other organs. Sympathetic fibers from T7 to 12 travel in the paravertebral space (explaining why paravertebral blocks have shown promise in this domain) to reach the celiac ganglia (explaining why celiac plexus blocks have been explored in this domain). These fibers course through the hepatic hilum along the portal veins, in the fat containing periportal potential space. Also, parasympathetic nerves travel along vagus to reach the celiac plexus and join at the hepatic hilum alongside sympathetic counterparts. In addition, the intercostal nerves contribute terminal fibers to Glisson's capsule. The phrenic nerve is a mixed motor and sensory nerve and is believed to contribute variably.
Many core interventional procedures focus on the liver and could benefit from strategies to avoid general anesthesia or reduce need for sedation medications. Procedures that have been explored in this domain include paravertebral blocks, celiac plexus blocks, and more recently hepatic hilar blocks for procedures such as liver tumor microwave ablation, biliary drainage, and tumor embolization.
One of the main challenges with a block strategy for the liver has been patient positioning, which is why the hepatic hilar block has become the focus of recent publications. The technical skills required to place the block are very similar to those used by interventional radiologists to perform the hepatic procedure. In contrast, a paravertebral block requires initial prone positioning, while the paravertebral and celiac plexus blocks carry different risk profiles of pneumothorax, bleeding, and viscous perforation. The hepatic hilar plane block keeps the block and procedure in the same organ.
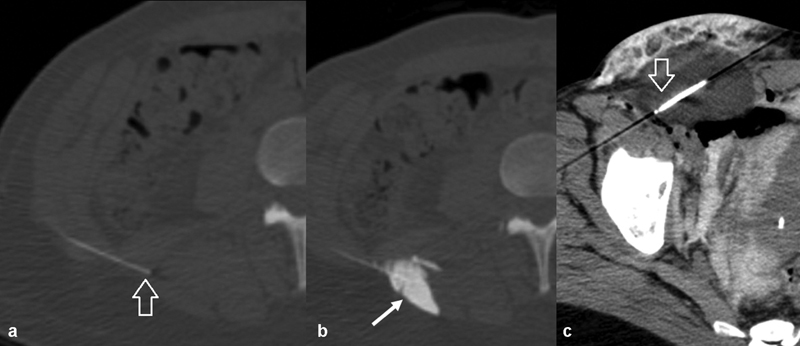
The target for injection is the peri-portal space, ideally at the hilum where the right and left hepatic innervations coalesce. Once the needle is confirmed to be extravascular, an injection of approximately 15 to 20 mL of injectate (e.g., including lidocaine with epinephrine and bupivacaine) allows hydrodissection along this plane and interaction with the plexus nerves. This can provide intraprocedural and postprocedural analgesia. In some cases where anatomy does not allow easy access of the hilum, or if a single-side procedure is planned, the operator may choose to adapt the procedure to inject the periportal space on one side, as seen in Fig. 5 .
Fig. 5.
Ultrasound-guided and cone-beam CT-confirmed hepatic hilar block performed prior to left hepatic arterial bland embolization. Ultrasound guidance was used to target the left periportal space ( b , blue circle denotes left portal vein, arrows denote needle trajectory) and a small test injection was checked on plain X-ray to not wash into a vascular structure (also confirmed on cone beam CT arrow, a ). At this point, the nerve block is delivered. ( c ) Postembolization angiogram, with residual nerve block agent noted lateral to the renal collecting system (star).
Aorticorenal Plexus Plane Block
The innervation of the kidney remains relatively understudied, but the relevance to interventional radiology mainly lies in the application to microwave ablation, which can be prohibitively painful and require general anesthesia. While this area remains understudied, much like the hepatic hilar block, the aorticorenal plexus that carries pain on the autonomic nervous pathways can be targeted with CT guidance.
The target for injection is the potential space immediately around the renal artery. A needle placed at a safe distance can be used to infiltrate approximately 20 mL of injectate. This will likely spread cranially to include the receiving periaortic nervous plexus. An example is shown in Fig. 6 .
Fig. 6.
CT-guided aorticorenal plexus block prior to microwave ablation of kidney tumor. ( a ) Needle (arrow) trajectory. ( b ) The early injectate is seen spreading along the aorta and posterior to the renal artery (arrow) at the time point shown in this image. ( c ) Microwave antenna placement (arrow).
Quadratus Lumborum Plane Block
An established technique to provide abdominal somatic (T4 through L1 dermatomes) and visceral analgesia before general surgery is the quadratus lumborum block. This truncal block has been applied to urologic, gynecologic, orthopaedic, and general surgical cases and can be applied to a variety of interventional radiology techniques, notably complex abdominal wall tumor ablations where the surfaces needing pain control are diverse and include skin, muscle, and peritoneum. A plane block to cover all these in a single step can improve consistency and efficiency of the procedure.
The quadratus lumborum (QL) block is actually performed in one of three target positions (QL1, QL2, and QL3). The block shown in the current report is a QL2 block because of ease of identification of the target on CT, accessibility while in the supine position using CT guidance, as well as decreasing risk of potential motor blockade seen with the QL3 block. QL2 is a plane block that covers the iliohypogastric, ilioinguinal, and subcostal nerves and with greater injectate volume, the lateral femoral cutaneous, obturator, and very rarely femoral nerves (which may provide temporary motor blockade for which the patient should be aware).
The target for injection is the triangular potential space (lumbar interfascial triangle) formed lateral to the erector spinae muscles between the latissimus dorsi muscle and quadratus lumborum muscle, as seen in Fig. 7 . Injectate here is within the middle thoracolumbar fascia layer and a volume of 20 to 30 mL will allow for adequate spread, with the concentration of anesthetic to be dosed according to patient age, weight, and clinical status to stay within safe limits.
Fig. 7.
CT-guided quadratus lumborum block (QL2) showing needle placed in the lumbar interfascial triangle ( a , arrow) and subsequent injection ( b , arrow) prior to large abdominal wall cryoablation ( c [arrow—cryoprobe]).
Superior Hypogastric Plexus Plane Block
Uterine fibroid embolization with intent for rapid discharge home is now routinely facilitated with superior hypogastric plexus blockade. The technique is a cornerstone of routine IR education and reference is made to the existing illustrative publications on this matter. 14 This block again relies on the concept that pain travels on sympathetic networks. Much like the celiac plexus wraps around the aorta at the level of the celiac artery, the superior hypogastric plexus wraps around the aorta at the level of the aortic bifurcation. A needle is targeted into the potential space immediately inferior to the aortic bifurcation and an injection volume of 20 mL (typical for plane blocks) is infused. For interventional radiologists who seek to enter the domain of nerve blocks, this block is likely the first that can be implemented into daily clinical practice.
Sciatic Nerve Block
Sciatic nerve block at the popliteal fossa is an established technique that has gained favor in the treatment of patients with critical limb ischemia. Anesthetic injected here both numbs and paralyzes the lower extremity below the knee, allowing for motionless digital subtracted angiography for the duration of the block while reducing the patient's need for sedation medications. This technique can also be applied before other interventions in the distribution, as shown below, prior to cryoneurolysis of the distal sciatic nerve for the treatment of post-amputation phantom pain and pain with prosthetic usage ( Fig. 8 ). Of note, in some, the contribution of the femoral nerve to sensation in the lower limb is disproportionately large in some (also for the stump in post-amputation pain) and therefore, a saphenous nerve block can be considered for additional analgesia (providing a nerve block at the lateral fibular head as an adjunct).
Fig. 8.
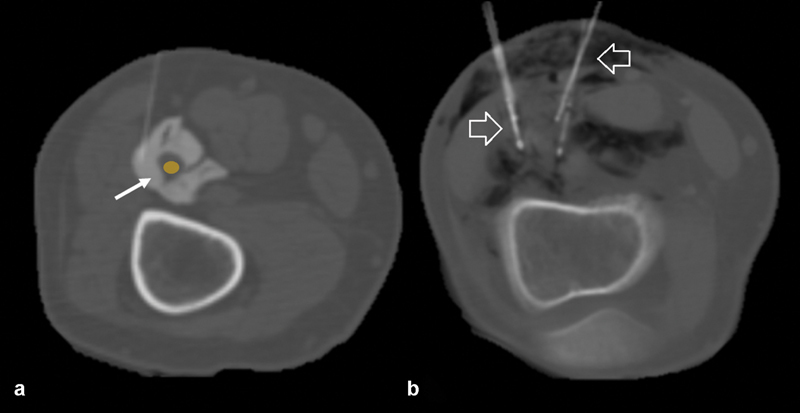
CT-guided distal sciatic nerve block at a level above the popliteal fossa with injectate ( a , arrow) surrounding the sciatic nerve ( a , yellow circle) prior to cryoneurolysis of the distal sciatic nerve at the level of the popliteal fossa ( b [arrows—cryoprobes]).
Conclusion
Interventional radiology patients can benefit from regional anesthesia techniques and the image-guided injections are within reach for the interventionalist at the same session. Furthermore, with CT guidance and cone beam CT vector guidance, deeper and novel targets are becoming accessible for patient care, allowing IR to contribute to the growth of regional anesthesia techniques.
Funding Statement
Funding No funding was received for any portion of this work.
Footnotes
Conflict of Interest None declared.
References
- 1.Chin K J, Lirk P, Hollmann M W, Schwarz S KW. Mechanisms of action of fascial plane blocks: a narrative review. Reg Anesth Pain Med. 2021;46(07):618–628. doi: 10.1136/rapm-2020-102305. [DOI] [PubMed] [Google Scholar]
- 2.Becker D E, Reed K L.Local anesthetics: review of pharmacological considerations Anesth Prog 2012590290–101., quiz 102–103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bina B, Hersh E V, Hilario M, Alvarez K, McLaughlin B. True allergy to amide local anesthetics: a review and case presentation. Anesth Prog. 2018;65(02):119–123. doi: 10.2344/anpr-65-03-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Best C A, Best A A, Best T J, Hamilton D A. Buffered lidocaine and bupivacaine mixture - the ideal local anesthetic solution? Plast Surg (Oakv) 2015;23(02):87–90. doi: 10.4172/plastic-surgery.1000913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Almasi R, Rezman B, Kriszta Z, Patczai B, Wiegand N, Bogar L. Onset times and duration of analgesic effect of various concentrations of local anesthetic solutions in standardized volume used for brachial plexus blocks. Heliyon. 2020;6(09):e04718. doi: 10.1016/j.heliyon.2020.e04718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kirksey M A, Haskins S C, Cheng J, Liu S S. Local anesthetic peripheral nerve block adjuvants for prolongation of analgesia: a systematic qualitative review. PLoS One. 2015;10(09):e0137312. doi: 10.1371/journal.pone.0137312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Raymond S A, Steffensen S C, Gugino L D, Strichartz G R. The role of length of nerve exposed to local anesthetics in impulse blocking action. Anesth Analg. 1989;68(05):563–570. [PubMed] [Google Scholar]
- 8.Eichenberger U, Stöckli S, Marhofer P. Minimal local anesthetic volume for peripheral nerve block: a new ultrasound-guided, nerve dimension-based method. Reg Anesth Pain Med. 2009;34(03):242–246. doi: 10.1097/AAP.0b013e31819a7225. [DOI] [PubMed] [Google Scholar]
- 9.Keplinger M, Marhofer P, Marhofer D. Effective local anaesthetic volumes for sciatic nerve blockade: a clinical evaluation of the ED99. Anaesthesia. 2015;70(05):585–590. doi: 10.1111/anae.13013. [DOI] [PubMed] [Google Scholar]
- 10.Latzke D, Marhofer P, Zeitlinger M. Minimal local anaesthetic volumes for sciatic nerve block: evaluation of ED 99 in volunteers. Br J Anaesth. 2010;104(02):239–244. doi: 10.1093/bja/aep368. [DOI] [PubMed] [Google Scholar]
- 11.Kim D H, Kim S J, Liu J, Beathe J, Memtsoudis S G. Fascial plane blocks: a narrative review of the literature. Reg Anesth Pain Med. 2021;46(07):600–617. doi: 10.1136/rapm-2020-101909. [DOI] [PubMed] [Google Scholar]
- 12.Kopp S L, Wynd K P, Horlocker T T, Hebl J R, Wilson J L. Regional blockade in patients with a history of a seizure disorder. Anesth Analg. 2009;109(01):272–278. doi: 10.1213/ane.0b013e3181a832da. [DOI] [PubMed] [Google Scholar]
- 13.Macfarlane A JR, Gitman M, Bornstein K J, El-Boghdadly K, Weinberg G. Updates in our understanding of local anaesthetic systemic toxicity: a narrative review. Anaesthesia. 2021;76 01:27–39. doi: 10.1111/anae.15282. [DOI] [PubMed] [Google Scholar]
- 14.Pereira K, Morel-Ovalle L M, Taghipour M. Superior hypogastric nerve block (SHNB) for pain control after uterine fibroid embolization (UFE): technique and troubleshooting. CVIR Endovasc. 2020;3(01):50. doi: 10.1186/s42155-020-00141-2. [DOI] [PMC free article] [PubMed] [Google Scholar]


