Abstract
This paper adopts a method of narrative critical review based on a non-systematic search of the literature to provide insights into the trends of developmental coordination disorder (DCD) treatment and to point out some future alternative approaches to prevent secondary health implications in children with DCD. The cause of DCD is unknown, but evidence suggests that these children have atypical brain structure and function. Interventions to help children cope with their activity limitations are effective in improving motor competence and motor skill related fitness in the short term. Although activity-orientated interventions can improve motor outcomes in children with DCD, high quality intervention trials and evaluation of long-term effects are urgently needed. Importantly, motor coordination problems associated with DCD extend to exercise-related activities leading to reduced participation in play and sports, which causes secondary problems in muscular fitness and body composition. Hence, treatment goals should not be limited to the improvement of motor skills (in ADL), but should also focus on health-related quality of life. We therefore propose when noticing motor problems in a child, already before enrolling but also during intervention, to explore ways to adapt everyday physical activities to optimally match the child's skill level. Hence, such activities will not only train the skills and improve physical fitness but will lead to positive engagement, thereby preventing the child from opting out of active play and sports. This provides the child with chances for exercise-dependent learning and will also positively impact social-emotional well-being.
Keywords: DCD, Physical fitness, Assessment, Intervention, Review, Neurodevelopment disorders
Take home messages.
-
•
To learn a skill, children with and without motor coordination limitations, need to move and like it!
-
•
Physical activity and fitness examination should be part of the standard assessment and treatment protocol in children with DCD.
-
•
Physical activity prescription pads should be on every pediatrician's desk and should be used to prescribe activities that keep children engaged and active in daily life.
-
•
Early incorporation of physical activity into their lifestyle is even more important in children with poor motor skills.
-
•
Preparing children with neuromuscular limitations for a lifetime of health requires a solid basis of motor skills and physical fitness.
-
•
High levels of endurance are not required in the majority of games and sports for young children but power and agility are.
-
•
Staying as close as possible to the task the child wants to learn will maximize the transfer to everyday situations (task-oriented training).
-
•
Adapting tasks to the child's skill level will lead to positive engagement.
-
•
Positive meaningful feedback will give the child a feeling of success (more than telling them what went wrong).
-
•
Deficiency in motor control, coupled with a lack of engagement in physical activity, makes children with neurodevelopmental disorders prone to non-communicable diseases later in life.
-
•
Understanding the underlying basis of the co-occurring motor difficulties in neurodevelopmental disorders is critically important for the development of effective interventions.
Developmental coordination disorder (DCD) (also known as Specific Developmental Disorder of Motor Function (SDDMF); ICD-10 code F82) is a neurodevelopmental condition characterized by a marked impairment in the development of motor skills or motor coordination that develops early-on and interferes with an individual's activities of daily living [1]. DCD is a common and chronic disorder resulting in considerable consequences in daily life. Prevalence estimates of 5–6% are most frequently quoted in the literature [2,3] but ranges in reports between 1.4% and 19%, making it one of the more common childhood disorders [4]. At least 2% of all individuals with normal intelligence experience severe consequences of motor coordination difficulties in everyday living including academic performance, and a further 3% have a degree of functional impairment in activities of daily living (ADL) [5]. The diagnosis of DCD requires meeting four diagnostic criteria, including (A) impaired ability to acquire and execute motor skills at an age-appropriate level (B) significant interference with activities of daily living, academic performance, leisure and play (C) onset early in the developmental period and (D) the movement difficulties are not better explained by intellectual disability, visual impairment or other neurological conditions affecting movement [1,6].
To better understand the neural and performance factors that may underlie DCD, and their implications for theory and practice, several systematic reviews of the recent research have been conducted [1,7,8]. Although there is consensus that DCD defines a heterogeneous group of children exhibiting marked impairment in motor skills, no consensus about symptoms and etiology has been established [9]. Recent reviews of the functional magnetic resonance imaging literature indicate that although several brain areas are unquestionably linked to DCD (frontal lobe, parietal lobe, basal ganglia, and cerebellum) no neural signature for DCD has yet been established [10,11]. For instance, children with DCD have less activation of the left brain, especially areas responsible for action observation and motor imagery (mirror neurons system) and areas for sensory integration [11]. Based on whole-brain resting-state examination, children with DCD also demonstrate altered functional connectivity between the sensorimotor network and the posterior cingulate cortex, precuneus, and the posterior middle temporal gyrus, preventing efficient use of action-related knowledge and thereby potentially impairing motor learning [12]. The involvement of different brain areas already suggests the widespread implications and constraints on functioning in children with DCD.
Developmental Coordination Disorder (DCD) and constraints
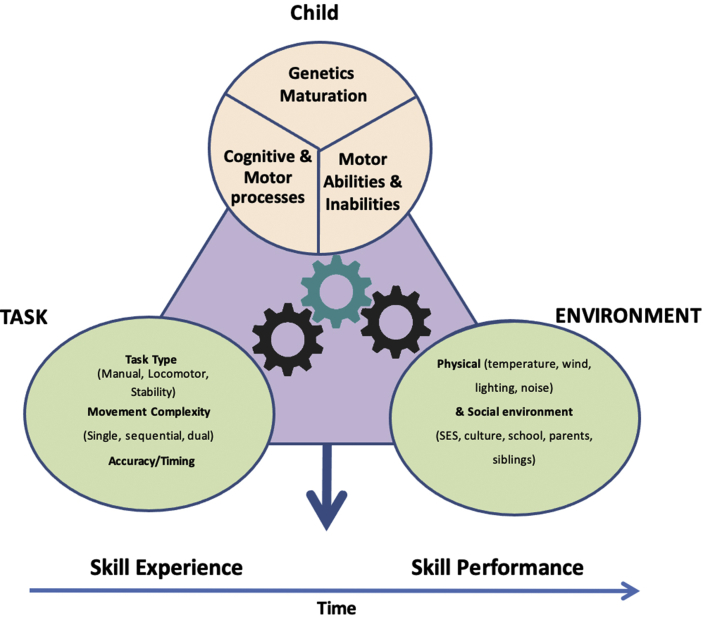
Most school children love to play and learn fundamental skills easily. Practicing catching, jumping and climbing leads to adaptations, resulting in improved performance in the particular motor skills and in maintaining good levels of physical fitness using these skills in active play. This way, children become increasingly competent in skills with increasing age and experience. As shown in Fig. 1 [13], the emerging competency will be the result of child (e.g. weight, age, genetic make-up and psychological characteristics), environmental (e.g. opportunities for physical education (PE) and sports) and task related constraints (the rules of the game, goals of the task and the equipment used).
Fig. 1.
Multi-component model of motor skill development and performance – adapted from Wilson et al., 2017 [13].
DCD is sometimes called a motor learning deficit, as these children have difficulties learning to perform all kinds of motor skills in daily life, whereas their typically developing peers seem to acquire them almost effortlessly. Having an adequate amount of practice is critical for producing meaningful gains in motor performance during development. Therefore, the clause in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) emphasizes that the criterion “learning and execution of coordinated motor skills is below expected level for age”, is only met in case the child has been “given opportunities for skill learning”. All factors impacting the performance of active play in children can be categorized as either personal (motor skills, fitness levels, self-efficacy) or environmental factors (opportunities, safety, physical education (PE) options).
Child factors specific for DCD
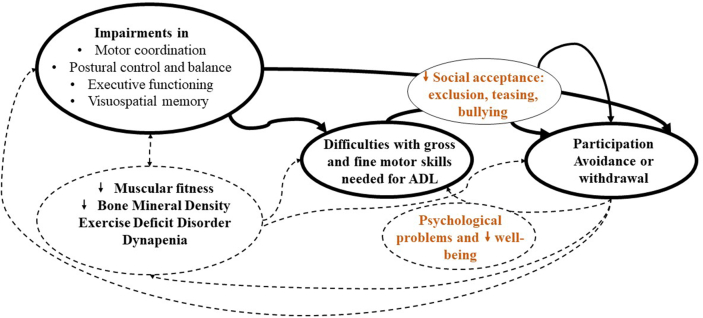
There is agreement that the core deficit in children with DCD lies in the motor competence, which in a global perspective contemplates all forms of tasks directed to objectives that involve coordination and control of the human body [14]. Although highly prevalent in school-aged children, DCD remains underdiagnosed. Unlike a condition such as cerebral palsy, the symptoms of DCD can be hardly visible and therefore overseen to impact functioning compared to other more overt pediatric movement-related conditions. Even in high-income countries, medical professionals have little knowledge of DCD [15]. Obtaining a diagnosis and therapy is quite a challenge for children with DCD and their families [16]. In case a child suspected of DCD gets diagnosed, getting intervention may be hard and many children end up on a waitlist for quite some time. This makes these children vulnerable at different levels of functioning. Because of their difficulties with coordination of fine and gross motor skills, they are usually unable to successfully participate in school, sports and leisure games, which often leads to exclusion, teasing, or even bullying [17]. Negative reactions from peers may lead to withdrawal from arts and craft activities, sports and games, which in turn again impacts their motor competence and social acceptance, eventually causing a vicious circle of avoiding participation in motor activities [18] (Fig. 2). As a consequence, the primary motor disorder in these children has far-reaching consequences at a psychological level, as all these factors may contribute to the development of internalizing symptoms as anxiety and depression [18].
Fig. 2.
Vicious circle of DCD - The solid black lines depict the primary problems and their consequences; the dotted lines represent the secondary problems. Apart from the motor difficulties (black text), children with DCD may also experience social-emotional and psychological consequences (orange text). The impairments in motor coordination, postural control and balance, executive functioning and visuospatial memory result in difficulties with gross and fine motor skills needed for participation. Due to their clumsiness, children with DCD will be less accepted by peers, which may lead to exclusion, teasing and even bullying, potentially causing participation avoidance or withdrawal. Once children move less, they will have less opportunities for learning skills and their motor impairments, ADL difficulties and feelings of exclusion will become more pronounced. Additionally, they may develop secondary problems due to lack of movement, such as decreased muscular fitness, bone mineral density and could even develop exercise deficit disorder and/or dynapenia. Along these additional motor problems, their psychological well-being can be affected, amplifying the negative effects on movement.
Children with high levels of motor competence tend to have a higher engagement in physical activities and better physical fitness, both cardiovascular and muscular [19]. Due to their participation avoidance, children (who may be clinically diagnosed) with DCD show diminished physical activity levels and fitness compared to their well-coordinated peers, and are therefore at a higher risk of developing a range of poor health outcomes such as metabolic, cardiovascular and musculoskeletal diseases [20,21]. They may also be at risk of low bone mineral density (BMD) because they have difficulties with the acquisition and execution of many basic movement skills such as running, jumping and hopping. These skills are well recognized as ideal for improving and developing BMD from early childhood into adulthood through interactions between muscle and bone [20]. Some scientists are currently defending the concept of “Exercise Deficit Disorder” (EDD), which is used to describe a condition characterized by reduced levels of regular physical activity (<60 min of daily moderate-to-vigorous physical activity, MVPA) that are recommended because of their association with positive health outcomes [22]. This highlights the need for the awareness of EDD in order to prevent it during childhood [23], a phenomenon that may also be applicable to many children with neurodevelopmental disorders.
Furthermore, DCD is often accompanied by other medical conditions such as Attention Deficit Hyperactivity Disorder (ADHD, co-occurrence: ≥ 50%), Specific Language Impairment (co-occurrence: ≤ 70%), Autism Spectrum Disorder (ASD, co-occurrence: ≤ 70%) and other cognitive impairments such as visuospatial short-term and working memory deficits [1]. Strong evidence indicates that DCD is associated with emotional, social and learning disorders [24]. However, it is often difficult to determine whether behavioral problems are coexisting disorders or long-term consequences of negative social experiences due to poor motor competence [1].
Importantly, different neurodevelopmental disorders may exhibit shared symptoms and substantial epidemiological comorbidity. Although, not included in the diagnostic criteria for ASD or ADHD, motor deficits are common characteristics in these children. Difficulty in performing age-appropriate motor skills affects up to 83% of the children with ASD [25,26] and 50% of the children with ADHD [27]. Given their motor restrictions, children with neurodevelopmental difficulties have reduced levels of sports participation and typically have decreased fitness, which often prevents them from participating with their peers, thereby indirectly reducing opportunities to develop age-appropriate communication, social, and behavioral skills [28] and places them at risk for secondary health problems (i.e. low cardiorespiratory fitness and overweight) [29].
Environmental factors
Not only are the emerging activities of daily living dependent on the child's characteristics (intrinsic), they are also highly dependent upon the environment. Environmental constraints are features related to the physical environment like the weather or to the sociocultural factors, such as family, school context and cultural expectations (religion, gender, local sport tradition) [30]. Facilitating physical environmental constraints include the parks, backyards, empty spaces and alleyways that provide the backdrop for active play and early sport experiences of many children. Various researchers report that socioeconomic influences play a significant role in obtaining movement proficiency and physical fitness. An environment poor in resources (play areas, membership fees for sports clubs, safety) or that lacks stimulating factors (parents, siblings, PE classes, only focus on academic outcomes) is considered to hamper motor development [31]. Children in disadvantaged circumstances have fewer chances of participating in organized physical activity and sports, which impedes the development of fundamental movement skills and physical fitness. Research also showed that fundamental motor skills proficiency generally increases with increasing socioeconomic conditions [32,33]. Furthermore, each context places specific demands on the motor competencies and physical activities of infants and children. The quality of living conditions, the family size or number of siblings and overall socioeconomic circumstances are potentially important factors to take under consideration [34]. Thus, environmental factors are crucial for developing motor competence and physical fitness in children, especially those with DCD.
Task constraints
Task constraints consist of modifiable features related to the task or activity itself like the tools used, temporal and spatial limits for success. For example, in ball skills, numerous constraints, such as ball size, bouncing properties, speed, trajectory, distance, and height of interception point, can make the catching task simple or complex. When starting with ball skills a soft, medium sized ball can be more efficient for dodgeball or aiming at a lowered basketball hoop will build up more self-confidence. Consequently, optimal matching between a child's skill level and the challenge posed by an activity will lead to positive engagement. This may be one of the factors why children with DCD opt out of active play and sport. If we can keep their skill level matched with the level of task requirements in PE, sports and active games, they will have positive experiences and opportunities to keep learning and improving their skills. Rehabilitation research has shown that task context can be a great and important factor in improving motor performance in individuals with movement disorders [35]. If we can help children to move more competently, they will be more engaged in physical activity and more likely remain physically active into adulthood [36,37].
Assessment and treatment in children with DCD
While the motor difficulties of children with DCD may appear to be less debilitating than those experienced by children with severe physical disabilities, it is the high prevalence of DCD, and its impact on children's social-emotional well-being and future health status, that makes DCD a significant condition in need of appropriate intervention.
Overall, DCD has long been an under-researched neurodevelopmental disorder, especially in non-Western countries and in low- and middle-income countries, but recent research in these areas has grown substantially [33,38,39]. Furthermore, the publication of a set of international clinical practice recommendations for professionals working with individuals with DCD [1] has highlighted the importance of multidisciplinary research. Blank and colleagues (2019) made efforts to improve the identification, diagnosis and delivery of evidence-based interventions for children with DCD by composing a clinical practice guideline. However, more extensive implementation of the diagnostic guidelines into clinical practice is still needed [1]. Moreover, implementation will be different per country, given the diversity of opportunities and priorities [40,41]. Two accompanying reviews for these recommendations concerned the exploration of mechanisms underpinning the motor coordination difficulties [8] and evaluation of the efficacy of intervention for individuals with DCD [7].
Assessment
Current knowledge
To enable effective identification and management of children with DCD, the appropriate assessment and intervention should be undertaken. Consequently, movement coaches (or therapists) need to identify those tasks that require improvement and use these tasks in their intervention planning. As in many areas of developmental disabilities, there is no gold standard for assessing DCD, so not surprisingly, a significant number of studies have explored the concurrent validity of different tests of motor proficiency and impaired coordination for identifying children with this condition and to plan treatment [42]. Moreover, most tests are only validated and normed for Western countries (mainly USA and UK) and not specifically developed for other cultures [7,[43], [44], [45]]. As mentioned before, a child's movement skills are determined by how well the child utilizes his/her personal attributes and information about the environment and task demands to create the desired movement outcomes. However, this is not the way the most frequently used tests are currently developed.
To objectify the age-inappropriate motor competency in children with DCD (criterion A), the Movement Assessment Battery for Children, 2nd edition (MABC-2) and Bruininks–Oseretsky Test for Motor Proficiency, 2nd edition (BOT-2) are often applied in research and clinical practice [1,46,47]. Both tests are psychometrically sound to determine the level of motor performance [48]. For the MABC-2, norms were established by the developers in the United Kingdom and cross-culturally validated with own norms in the Netherlands and Flanders (Belgium), China and Brazil [[49], [50], [51]]. The developers of the BOT-2 also established norms in the United States and a cross-cultural validation was done in Turkey, Brazil and Germany [[52], [53], [54]]. Some test items in both tests come close to everyday tasks, but they give less information about the adaptability to changing task demands and the critical skill level the child can master [48]. Adaptation of existing behaviors to a changing or new performance context involves the process of skill transfer [[55], [56], [57]], which is known to be difficult for children with DCD. Recently, a new psychometrically sound motor scale was developed, the PERFormance and FITness (PERF-FIT) test battery [[58], [59], [60]]. The PERF-FIT provides an integrated way to evaluate increasing levels of fundamental motor skills and muscular-fitness that has cross-cultural applicability. This instrument was specifically developed for low-resourced areas, lacking the means to purchase expensive test equipment.
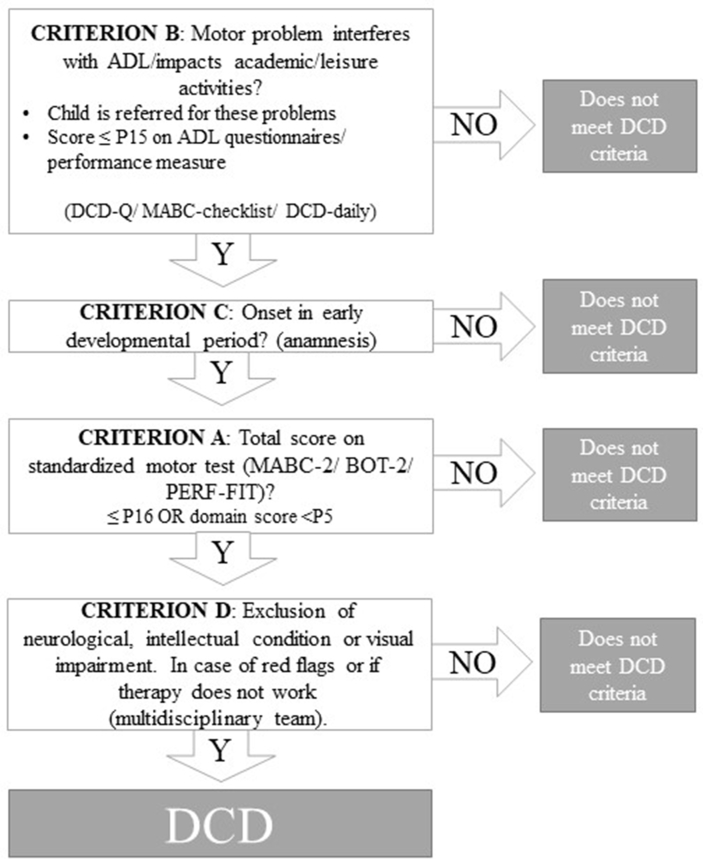
The diagnostic process for children with suspect of DCD is depicted in Fig. 3. To establish whether the motor skill difficulties presented by the child also impact its daily functioning (criterion B), several measurement tools can be applied: the MABC-checklist, the DCD questionnaire (DCD-Q) and the DCD-Daily. The MABC-checklist and DCD-Q are both parental questionnaires gauging the difficulties with daily activities. The MABC-checklist has poor sensitivity (41%) and fairly good specificity (88%) [61], whereas overall sensitivity and specificity of the DCD-Q are good (85% and 71%, respectively) [62], indicating such questionnaires are mainly useful in children referred for diagnostic assessment and not for general screening purposes. The DCD-Q has been the most widely researched and used in many countries around the world [[62], [63], [64], [65], [66], [67]].
Fig. 3.
Flowchart for the diagnosis of DCD using DSM-5 criteria – adapted from Smits-Engelsman et al., 2015 [47].
The DCD-Daily consists of a questionnaire, which covers domains of ADL that are relevant for children (“self-care and self-maintenance,” “productivity and school” and “leisure and play”) and a standardized performance measure that comprises 18 short tasks covering the domains of selfcare (feeding, dressing), school (writing, crafts, coloring, cutting) and play (hopping). Both sensitivity and specificity of the DCD-daily are good (both 80%) [68]. The instrument is currently under study for use in other cultures.
Early signs of motor difficulties (Criterion C) are usually mapped during anamnesis and if any signs of other medical conditions such as neurological disorders or intellectual disabilities come up during the history taking or observation (Criterion D) a multi-disciplinary approach is required.
Standardized tests are needed to enable diagnosis (confirm criterion A) and identification of impaired motor domains, but may not be very helpful for treatment planning. In contrast to standardized tests, task performance analysis, which comprises an activity-oriented assessment, will reveal the specific difficulties a child encounters in his/her everyday context. These assessment approaches focus on the analysis of performance (of skills that keep children engaged and active in daily life) and incorporate loading and unloading aspects of skills (tasks) and contextual factors that can influence behavior. Information gained during task performance analysis can be used to shape the treatment.
Future implications
To meet the criteria for DCD, the DSM-5 states that children should have had the opportunity for learning and using the skills they are showing problems with. As motor development occurs in a specific social context, the environment in which a child is reared is important. However, if motor skill execution in tests is normed for a certain population, it is by definition based on the performance level of age- and gender matched peers in that specific cultural environment. This would mean that every motor skill norm-referenced test should have culturally adapted norms. An important other implication is that, these commonly used assessment batteries provide only a limited view of the overall movement competence of children. Moreover, the question remains whether the “average” South African, Chinese, Australian, American or European child exits. Many societies have large diversity within their citizens. Hence, assessment of motor tasks should not be isolated from their functional context because spontaneous exploration of possibilities for actions is necessary to accomplish a goal-directed activity [69].
Assessing motor skills outside a functional context, can lead to either an over- or under-estimated DCD prevalence, reflecting only the number of children who performed poorly on standardized motor assessment tools rather than the actual number of children who experience difficulties in daily living and have limited ability to participate in physical activity in their society due to their motor coordination deficiencies. To obtain a more holistic picture of the movement competencies of children, future clinical studies should examine both every day motor tasks used in that society (using cutlery, getting dressed, catching a ball during a game played during recess), and fitness related skills (running, stair walking, carrying a box with tools, jumping rope, forms of active transportation) because active children become active adults.
Motor skill related fitness is a modifiable risk factor for physical inactivity and overweight, meaning that monitoring fitness and muscle strength is of considerable importance for prevention, but it requires validated tests or specialized equipment to follow up on the child's performance level. Consequently, physical fitness is rarely measured in populations with a lower socioeconomic background due to time, budget, and logistic limitations. An alternative to objective testing is to use self-rated measures obtained from questionnaires. However, little is known on the precision of the self-rated physical fitness levels in children and existing evidence is hampered by cultural bias towards Western communities. Fortunately, some reliable field-based tests for both aerobic and anaerobic capacity, and functional strength and agility are available that could also be used during the assessment of children with DCD [70]. However, studies on what these fitness tests are measuring in children with DCD are needed because the development of motor competence and physical fitness are linked directly via neuromuscular function [14], and the two components are hard to separate [31,71].
Recently, more apps measuring jump distance or height, balance sway, running and bike trajectories, or fine motor skills became available, which can assist in having more regular updates on the child's level of performance. It is even better if these objective measurements are built-in in games with stimulating goal setting linked to some kind of reward system.
Children with DCD experience significant activity limitations that are associated with impairments in the development of fundamental movement skills and postural control or balance. The control of posture limitations in children with DCD has been widely described and summarized in the literature [72]. However, the frameworks used to subdivide postural control have been diverse, e.g. static versus dynamic balance or anticipatory versus reactive control. In order to improve consistency in the approach to assessment and treatment, Dewar and colleagues (2017) proposed an overarching construct of postural control and its elements to be used in cerebral palsy [73,74]. This construct defines stability limits and verticality, anticipatory postural adjustments, reactive postural responses, sensory orientation and stability in gait [74]. Such an approach could be valuable to apply in children with DCD as well.
Due to participation avoiding behavior, health-related quality of life (HRQoL) is an important aspect of overall assessment, including screening of mental health, emotional and behavioral problems [75,76]. Improvement of HRQoL should be included as one of the treatment outcomes assessed in addition to the core aspects of a developmental disorder [77]. Eventually with coaching or treatment we want to lessen the impact of the disorder on well-being and daily functioning. An effective intervention induces improvements of the core symptoms of a disorder but also diminishes its impact on daily activity and future life. Furthermore, these children need to experience success in movement-related practical life skills, highlighting the need for the identification of protective factors when developing intervention programs. Positive self-perception, positive parenting, positive feedback from teachers and coaches, positive peer relationships and social acceptance, good social communication skills, and absence of bullying will make them more resilient.
In summary, the activity-oriented assessment approach will focus on the measurement of performance of skills that keep children engaged and active in daily life and that incorporates loading and unloading aspects of skills/tasks and looks at contextual factors that can influence behavior. DCD does not only manifest itself on motor coordination difficulties, it has a widespread impact on different domains of functioning such as the cognitive, language, and social-emotional domains, which creates a challenge for good assessment [78]. Therefore, if indicated, a multidisciplinary approach is needed to disentangle primary and secondary underlying factors in children with DCD to understand the practical implications [75,79].
Interventions
Current knowledge
The ultimate goal of intervention in children with DCD is to lessen the impact of the disorder on well-being and daily functioning. Therefore, clinicians should prescribe interventions that are most likely to produce the greatest improvement in motor outcomes. Significant effort from many perspectives and disciplines has been made to develop interventions that remediate motor impairments and alleviate the associated problems in DCD. A wide variety of interventions is used to support children with DCD. For the purpose of this paper, we will focus on neurorehabilitation or motor-based studies, i.e. occupational and physical therapy, and physical education-based interventions. Such interventions can be grouped based on the International Classification of Functioning, Disability and Health for children and youth (ICF-CY) [80] level they are tackling (Table 1).
Table 1.
Intervention approaches for children with DCD.
|
| Goal: improvement of body functions and prevention of significant deviation or loss body function or structure, considering developmental risks. |
|
| Goal: Improvement of the execution of a task or action. Removing the activity limitations that an individual may have in executing activities, considering the task and context specificity. The training situation is similar to the common encountered constraints and environment where the activity has to be performed after the intervention. |
|
| Goal: Improvement in the child's involvement in a real-life situation. Removing restrictions that individual may experience in involvement in life situations, considering the environmental factors of the physical, social and attitudinal environment in which the child lives. To ensure transfer of the new activity abilities to the real-life situation, active involvement of the child, parents and/or teachers is needed. |
The simplest summary of the literature is that there is evidence to support the idea that what is trained will improve; pointing to an advantage for activity- or task-oriented training (like Cognitive-Orientation to Occupational Performance (CO-OP), Neuromotor Task Training (NTT)) because by definition these approaches stay as close as possible to the activities that need improvement [1,44,45,81]. Impairment oriented approaches focus on reducing impairments. However, these improvement do not necessarily transfer into improvements of daily activities and participation, and are therefore not recommended in isolation [1,82]. A task-oriented approach allows us to help children with DCD overcome activity limitations and participation restrictions by practicing real-life activities with the intention of acquiring a skill, instead of focusing on the underlying deficits. Although there is evidence that interventions aimed at improving motor capacity are beneficial for children with DCD on the short run, long-term studies are lacking [45,81,83]. Moreover, no hard evidence is currently available verifying that one task-oriented approach should be preferred over another in children with DCD. Based on the best available research evidence, Preston and colleagues (2017), concluded that the most effective motor-based interventions had some features in common: a task-oriented approach was a key feature and even when interventions were group-based, they were tailored to the individual needs and particular interests of the children [44]. Consequently, therapists and coaches should identify those tasks that need improvement, and use these tasks in the training program and as a part of the objective evaluation of the efficacy of the training program [84]. For each child there should be a balance between the skill capacity and the skill level of the tasks. However, in children with negative experience, the balance between skill level and challenge of the task is even more critical. Although many intervention studies took place in schools, evaluation of adapted PE for children with motor impairments is still lacking in literature [85]. Bonney [[86], [87], [88]], Neto [89] and Jelsma [90] have shown in three different countries that children with DCD may improve their motor performance (like dynamic balance) by playing active video games (AVG) during school hours. Ferguson and coworkers (2015) have shown that a school-based health promotion plan that focuses on increasing opportunities for physical activity may be effective in improving motor performance in children with DCD and can increase fitness levels in general [31].
In individuals with DCD the acquisition of basic fine and gross motor skills is the primary focus. Although DCD is defined as a deficit in skill acquisition, few studies have addressed the process of motor learning. There is no doubt that children with DCD show poor motor skills, which may indicate less effective learning. However, the literature is not ubiquitous that a motor learning deficit causes the low motor performance. Children with DCD benefit from practicing motor skills, still their performance lags that of their peers. Hence, it is not clear if their motor learning is impaired and if so, which aspect of learning (which learning phase and which aspects of the learning process: performance, consolidation, retention, near or far transfer) is affected. What we do know is that training in DCD does lead to gains in motor performance, which seems to suggest they are able to learn new skills [91]. Consolidation, retention, and transfer of motor learning have been studied less often in DCD [86,88,92], and need to be investigated in future research. Moreover, studies comparing intervention effects and motor learning differences in children with comorbidity or co-occurring neurodevelopmental disorders are virtually lacking.
How to apply effective treatment in children with DCD
Given the large number of ways to help children with DCD and their families, we will discuss one example of a task-oriented approach (NTT) and one example of an adjunct intervention (Virtual Reality (VR)), since we have studied those.
Activity-oriented approach
One of the recommended activity-oriented approaches is NTT [1,44], specifically developed for children with DCD to facilitate participation [7]. Activity in this context is defined as the execution of a task or action by an individual (ICF-CY) [80]. NTT is based on motor control and motor learning principles but also takes motor teaching and motivation principles into account. Treatment of children with DCD must be based on an understanding of the functional nature of the limitations. Interventions may then be tailored to the unique combination of symptoms and problems exhibited by the child. Within the NTT therapy framework, the child's needs, i.e. the specific activity problems the child has, are analyzed and then the factors within the environment-task-child that contribute to these problems are determined. This is called the constraint or task analysis. Each activity or task has a specific goal that involves physical movement (e.g., rope skipping, free-throw shooting in basketball, walking on stepping stones, tying shoelaces, writing neatly, etc.) and is normally learned and refined with practice. Insight into the task constraints of an activity is required for the therapist to load the different task demands. In the task performance analysis, attention is given to the specific components of the task, identifying the task demands and difficulties that are present in the individual child's performance of that task. This is done for example by varying the demands of the task (i.e. task (un)loading) or the environment and observing its effect on the child's movement performance and outcome. To make a task more difficult or easier, three principles can be applied: changing task requirements, decreasing or increasing workload and subdividing or linking activities. Changing task requirements refers to adapting factors by which the coordination demands get easier or harder, i.e. spatial (distance, direction, precision) and temporal features (timing, tempo, decision time, duration). Increasing workload means that the task is adapted so it increases or decreases strength, fitness and speed. By increasing the workload, the task-oriented approach integrates with aspects of an impairment-oriented approach (strengthening or improving anaerobic capacity) however within the specific task context. If the task is combined with other tasks, then linking has been applied. Linking refers to the coupling of at least two skills that can be performed separately. Linking can be parallel (dual task) or serial (dribble the ball then shoot).
Virtual reality and physical activity
Although playing outside with other children will have many benefits besides being physically active, this may not always be possible due to circumstances, such as: safety, air pollution, lack of parks, sport facilities and playgrounds, and lack of supervision. Given this fact, new technologies may help to keep the children motivated for the practice of physical activity [[93], [94], [95], [96]] and also play with other children over the internet. AVG could offer movement experience comparable to playing outside [95,96]. The games are very entertaining leading to longer times on task. If children truly like to engage with AVG, this may open doors to social (multiplayer games) activities using these new technologies. This way AVG can potentially provide rich exercise environments that entice participants to work longer, harder, and more often because it is fun and may help in solving some of the motor control problems. Tasks practiced within virtual environments may enhance motor skill learning through the integration of multiple sensory processes such as proprioceptive, visual, auditory, and vestibular information with the engagement of cognitive processes. Feedback given by AVG is not experienced as negative, maybe because it is not given to the child but to its Avatar or in another universe. Representation on the screen of each body response may help improve speed and anticipation in agility and balance tasks. Children watch the Avatar carefully and get immediate, safe feedback, something that is not always the case during life intervention or training. We tend to explain to the child what (s)he did wrong (“You didn't make your arms swing when you jumped”) and put less emphasis what went well (“You reached for the sky with your hands in this great jump”). Giving meaningful positive feedback is one of the most important abilities that a therapist of movement coach should possess.
The results regarding the effectiveness of the application of AVG in intervention are promising [7]. The evidence of the effectiveness of AVG in children in terms of motor learning (retention, transfer, generalization to real-world situations) is still in its early stages. One reason to expect that training in virtual reality (VR) supports motor learning is that the performer must resolve differences between sensory signals, thereby requiring active error correction [97]. Sensory feedback linked to the actual task performance may generate more accurate repetition than indirect verbal or visual reinforcement given by a therapist. Motor learning is not only experience-dependent and feedback-related but also largely dependent on the type and intensity of practice as well as on the environmental context in which practice occurs [98]. Despite the caveats related to the validity of movements made in different VR environments, some studies in typically developing children and children with DCD suggest that movements acquired through practice in AVG may transfer to meaningful real-world function. The AVG systems combine gaming and physical activity, via digital platforms (e.g., consoles, wearables, smartphone apps, VR glasses) and are plausible alternative strategies to encourage physical activity participation [93]. Thus, even if the motor patterns learned in a soccer or tennis game would not transfer to better hitting or kicking a ball in the real world, children still perceive these activities as fun [90] and like to keep doing them which also limits their sedentary time and may improve their anaerobic fitness [87] and dynamic balance [90].
Comorbidity in DCD and motor problems in children with other developmental disorders
As mentioned above, physical activity promotes the development of motor skill competence in children with neurodevelopmental disorders. One understudied aspect to be considered is health-related physical fitness when children are primarily referred for behavioral or emotional problems. Also, in these children, even without meeting all the criteria for DCD, motor impairment can be a barrier to sports participation; the child cannot keep up with their peers, in turn reducing motivation to continue, which may additionally affect these children with comorbidity socially and emotionally. This emphasizes the need for interventions to promote optimal motor skills as well as overall fitness for these groups.
Importantly, teaching a group of children with mixed levels of – motor and social-skills requires specific expertise among trainers and physical educators. Appropriately differentiating for various motor skill levels within the normal spread of motor development is a core competency for PE teachers and professional sports coaches. However, they may not be trained sufficiently at the lower motor skills levels seen in children with DCD and in the specific didactics needed for children with motor disabilities. This is especially the case if combined with emotional, behavioral and social challenges. If the level of motor skill is really low, individual or small group intervention may be needed at the start. Later the movement coach (e.g. pediatric physical therapist, special physical educator) will facilitate the transition from training adapted for children with motor difficulties to more mainstream sports participation, by preparing them for competition elements and social interaction [99]. Community sport centers may be the place where children can maintain appropriate levels of physical activity and physical fitness. This is essential in developing healthy lifestyles and providing a setting for families of children with and without motor disorders to engage in recreation together and to develop friendships among families [99].
Future implications
Clearly, effective training approaches exist and can be applied in clinical practice [1,7,44]. Unfortunately, before children who are suspected of having DCD are actually being treated, they often have to wait quite some time before being diagnosed due to the general unawareness of the disorder in pediatric caregivers or the waitlists in centers for diagnosing developmental disorders. Also, once they find their way to treatment, not all therapists are fully familiar with activity- or task-oriented approaches, which then may lead to limited or absent progress in motor performance and therapy goal achievement. The longer the child has to wait before adequate treatment can be commenced, the higher the chance of opting out of gross and fine motor activities and avoiding participation with a vicious circle of primary and the development of secondary physical, social and emotional malfunctioning as a result (Fig. 2). In this section, we will therefore discuss the need for critical assessment of treatment efficacy, when children with (suspected) DCD find their way to a therapist. Finally, we will share our view on secondary prevention as it seems that, despite our good intentions, we are often being too late and are doing too little for children with DCD.
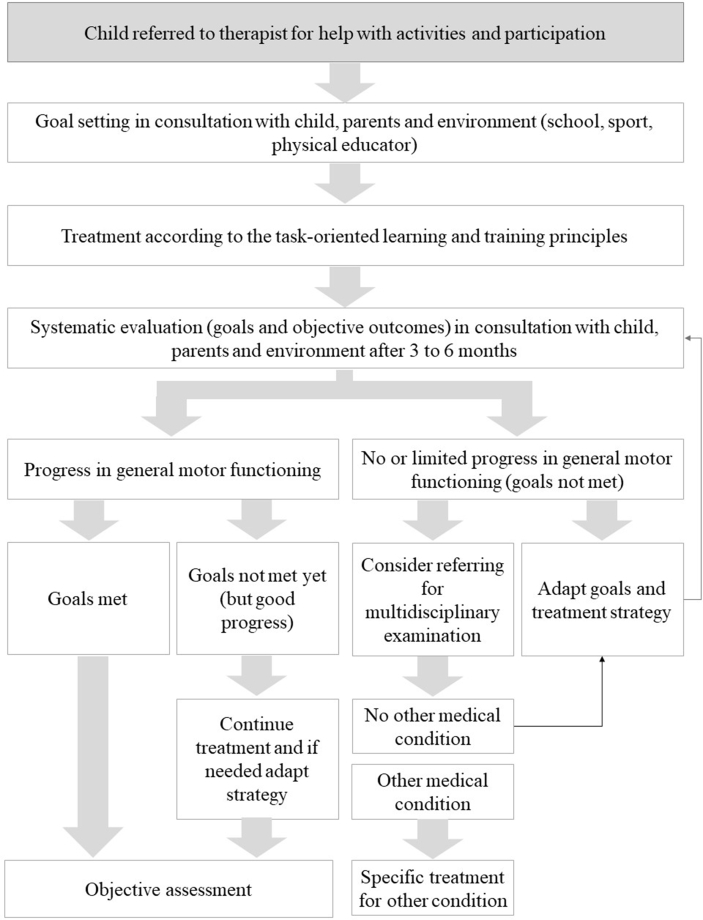
Setting treatment goals and tracking treatment success
When a child and his/her parents have applied for treatment, treatment goals will set in consultation with the child, parents and environment. Next, the training takes places according to an activity- or task-oriented approach (Fig. 4). Once the training has started, the progress should be assessed together with child, parents and environment and the effectiveness of the treatment should be tracked carefully and objectively measured. New media (apps, smart watches, activity trackers) can be used as additional measures of skills and activities and also as motivators. If the child shows progression in motor functioning and the goals are met, actions should be put in place to watch and monitor the transfer of the newly gained skills to everyday life. When the child shows progression in motor functioning, and the goals are not yet met, continuation of treatment is in order and evaluated again after the second treatment series. However, if progress in motor functionin is limited or absent, either the goals and/or the treatment strategy should to be adapted or referral for a multidisciplinary examination considered. When multidisciplinary examination does not reveal any other condition that can explain the poor motor performance (e.g. neurological or other comorbid disorder), the goals and intervention strategy require adaptation. If another underlying condition is present, those specific treatment protocols should be followed.
Fig. 4.
Treatment process with potential steps to be taken by the treating therapist.
Prevention is key to avoid doing “too little” and being “too late”
Early childhood is a critical time for the development of fundamental movement skills, which are considered the building blocks of more complex movements and a key factor in promoting lifelong active lifestyles and health [100]. Hence, merely focusing intervention on improvement of fundamental movements, like included in the standardized motor performance tests, means we will do too little to help children with DCD on the long term. Thus, the integration of both health- and skill-related components of physical fitness into physical activity promotion is specifically important in this group of children and should not be overlooked [101].
Motor delays and difficulties in children with DCD are typically observed early in life but children are usually diagnosed between 5 and 7 years. The international guideline recommended not labeling children under the age of 5 because the lack of stability of DCD diagnosis at early ages [1]. But shouldn't we be stimulating motor development earlier and focus on young children? Not diagnosing, but helping parents and teachers who feel disheartened by the unrelenting encouragement required by the children with and at risk for DCD. If motor performance is lower, children need more and not less physical activity experience. By focusing on their strengths (e.g., activities they can do) instead of their weaker points (e.g., their motor problems), children will manage to preserve a more positive self-image [77]. Goals should be realistic, and divided into smaller steps but still aiming for the child to reach his/her full potential. Supporting the child in day-to-day tasks takes up a lot of time (mostly of the mother) and a support systems (father, grandparent, siblings, clubs, PE teacher, coaches) will help to find time and ways to keep the child moving and enjoying the games or active transportation it has mastered [102].
Children with DCD spend less time participating in recreational physical activities and may experience lower physical fitness than children without DCD [103]. Low levels of muscular fitness, i.e. muscular strength, muscular power and muscular endurance, in children are associated with poor motor competence, functional limitations and adverse health outcomes [104,105]. Children who do not develop the prerequisite motor skills early in life may not develop the motor skill repertoire and perceived confidence to meet recommendations for daily levels of MVPA [106,107]. Thus, it is clear that motor competence plays an important role in growth, development, and opens up opportunities that lead to a physically active lifestyle, in which prevention and non-structured intervention (activity prescription) are key. Importantly, outdoor play and sport-like games in young children are characterized by short periods of intensive physical activity, interspersed with short periods of reduced or less intensive activity. Both motor skills and anaerobic capacity are of importance in these short burst activities. High levels of endurance are not required in the majority of games and sports for young children but power and agility are [108]. By giving these children the right environment and tasks to experience the fun of moving, they have opportunities to practice and learn motor skills. Experiencing movement as a fun activity, will then encourage them to move more frequently and maybe even more intensively. Feeling more competent will motivate children with motor coordination problems to participate in a variety of physical activities without the stress of embarrassment and instead with feelings of perceived motor competence. Furthermore, participating in active play is an option for making friends. Raz-Silbiger and colleagues (2015) indeed showed that children with DCD who participated more in vigorous physical activities had higher parent-rated HRQoL in the social domain than children who participated less in vigorous activities [109]. So, we may conclude that treatment of DCD may not just be a matter of practicing motor skills but also of creating an environment in which children can engage in activities and learn to detect and correct their motor performance [77]. Furthermore, it allows children to adopt an active life style, which is known to correspond with positive health outcomes and with smaller increases in weight and adiposity during childhood and adolescence.
Given the importance of a stimulating environment, natural play spaces should also provide for more diverse forms of play for children of varying ages and competencies. Parents need to see the importance of active play (not as a waste of academic time) and it should not be a safety hazard. Public parks, playgrounds, community centers, walking trails/hiking areas, all can provide a variety of opportunities to practice movement skills. Safe environments (physically and psychologically) where the children can be active and keep practicing, need to be part of the overall approach. Important factors may be to create a support system, which encourages children to stay active over time. Research has shown that, to be effective, physical activity interventions need to be embedded in pediatric health care by practitioners, stakeholders, and policy makers [110,111]. Movement coaches and pediatricians can be advocates, but they are usually not experts in politics. However, we do have an obesity- and inactivity pandemic [111], which will not reside by itself. Hence, we need community engagement that strives for inclusive, accessible, and walkable/bikeable communities. Children intrinsically want to move if we give them the right environment and support. For children with neurodevelopmental disabilities, inclusive active play and transportation is even more important. For them (and all other children with health risks) we need to create a public realm with as many safe movement affordances as possible. Thus, communities and government need to ensure safety within these public environments and they have an important role to play in advertising the importance of physical activity in children and youth. True safety begins with designing our streets to prioritize safe and accessible active transportation, thereby allowing physical activity as part of daily life. These are huge challenges for communities to engage in implementing ideas on active living and mobility [112].
Prospective
Children with motor problems (at risk for DCD) and their family need support, also in the early stages, even before the child is diagnosed. Given that children with poor motor skills need more practice time and that motor skill proficiency is an important predictor of future physical activity, maximal affordances for safe and fun movement experiences should be made available taking into account the child, task and environmental constraints. Once enrolled in intervention, the main focus should be on improving meaningful activities and to facilitate participation. Prevention of activity-avoiding behavior of children with DCD and improvement of health-related quality of life is an important aspect of assessment and intervention.
Footnotes
Peer review under responsibility of Chang Gung University.
References
- 1.Blank R., Barnett A.L., Cairney J., Green D., Kirby A., Polatajko H., et al. International clinical practice recommendations on the definition, diagnosis, assessment, intervention, and psychosocial aspects of developmental coordination disorder. Dev Med Child Neurol. 2019;61:242–285. doi: 10.1111/dmcn.14132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Psychiatric Association . 5th ed. American Psychiatric Association; Arlington, VA: 2013. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- 3.Blank R., Smits-Engelsman B.C., Polatajko H., Wilson P.H. European Academy for Childhood Disability (EACD): recommendations on the definition, diagnosis and intervention of developmental coordination disorder (long version) Dev Med Child Neurol. 2012;54:54–93. doi: 10.1111/j.1469-8749.2011.04171.x. [DOI] [PubMed] [Google Scholar]
- 4.Amador-Ruiz S., Gutierrez D., Martínez-Vizcaíno V., Gulías-González R., Pardo-Guijarro M.J., Sánchez-López M. Motor competence levels and prevalence of developmental coordination disorder in Spanish children: the MOVI-KIDS study. J Sch Health. 2018;88:538–546. doi: 10.1111/josh.12639. [DOI] [PubMed] [Google Scholar]
- 5.Lingam R., Hunt L., Golding J., Jongmans M., Emond A. Prevalence of developmental coordination disorder using the DSM-IV at 7 years of age: a UK population-based study. Pediatrics. 2009;123:e693–e700. doi: 10.1542/peds.2008-1770. [DOI] [PubMed] [Google Scholar]
- 6.Association A.P. 5th ed. ed. American Psychiatric Association; Arlington, VA: 2013. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- 7.Smits-Engelsman B., Vinçon S., Blank R., Quadrado V.H., Polatajko H., Wilson P.H. Evaluating the evidence for motor-based interventions in developmental coordination disorder: a systematic review and meta-analysis. Res Dev Disabil. 2018;74:72–102. doi: 10.1016/j.ridd.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 8.Wilson P.H., Smits-Engelsman B., Caeyenberghs K., Steenbergen B., Sugden D., Clark J., et al. Cognitive and neuroimaging findings in developmental coordination disorder: new insights from a systematic review of recent research. Dev Med Child Neurol. 2017;59:1117–1129. doi: 10.1111/dmcn.13530. [DOI] [PubMed] [Google Scholar]
- 9.Vaivre-Douret L., Lalanne C., Golse B. Developmental coordination disorder, an umbrella term for motor impairments in children: nature and Co-morbid disorders. Front Psychol. 2016;7:502. doi: 10.3389/fpsyg.2016.00502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Biotteau M., Chaix Y., Blais M., Tallet J., Péran P., Albaret J.M. Neural signature of DCD: a critical review of mri neuroimaging studies. Front Neurol. 2016;7:227. doi: 10.3389/fneur.2016.00227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Irie K., Matsumoto A., Zhao S., Kato T., Liang N. Neural basis and motor imagery intervention methodology based on neuroimaging studies in children with developmental coordination disorders: a review. Front Hum Neurosci. 2021;15:620599. doi: 10.3389/fnhum.2021.620599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rinat S., Izadi-Najafabadi S., Zwicker J.G. Children with developmental coordination disorder show altered functional connectivity compared to peers. Neuroimage Clin. 2020;27:102309. doi: 10.1016/j.nicl.2020.102309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilson P.H., Smits-Engelsman B., Caeyenberghs K., Steenbergen B. Toward a hybrid model of developmental coordination disorder. Current Developmental Disorders Reports. 2017;4:64–71. [Google Scholar]
- 14.Cattuzzo M.T., Dos Santos Henrique R., Ré A.H., de Oliveira I.S., Melo B.M., de Sousa Moura M., et al. Motor competence and health related physical fitness in youth: a systematic review. J Sci Med Sport. 2016;19:123–129. doi: 10.1016/j.jsams.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 15.Wilson B.N., Neil K., Kamps P.H., Babcock S. Awareness and knowledge of developmental co-ordination disorder among physicians, teachers and parents. Child Care Health Dev. 2013;39:296–300. doi: 10.1111/j.1365-2214.2012.01403.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Licari M.K., Alvares G.A., Bernie C., Elliott C., Evans K.L., McIntyre S., et al. The unmet clinical needs of children with developmental coordination disorder. Pediatr Res. 2021;90:826–831. doi: 10.1038/s41390-021-01373-1. [DOI] [PubMed] [Google Scholar]
- 17.Zwicker J.G., Suto M., Harris S.R., Vlasakova N., Missiuna C. Developmental coordination disorder is more than a motor problem: children describe the impact of daily struggles on their quality of life. Br J Occup Ther. 2017;81:65–73. [Google Scholar]
- 18.Schoemaker M.M., Smits-Engelsman B.C.M. Is treating motor problems in DCD just a matter of practice and more practice? Current Developmental Disorders Reports. 2015;2:150–156. doi: 10.1007/s40474-015-0045-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barnett L.M., Lai S.K., Veldman S.L.C., Hardy L.L., Cliff D.P., Morgan P.J., et al. Correlates of gross motor competence in children and adolescents: a systematic review and meta-analysis. Sports Med. 2016;46:1663–1688. doi: 10.1007/s40279-016-0495-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hands B., Chivers P., McIntyre F., Bervenotti F.C., Blee T., Beeson B., et al. Peripheral quantitative computed tomography (pQCT) reveals low bone mineral density in adolescents with motor difficulties. Osteoporos Int. 2015;26:1809–1818. doi: 10.1007/s00198-015-3071-8. [DOI] [PubMed] [Google Scholar]
- 21.Faught B.E., Hay J.A., Cairney J., Flouris A. Increased risk for coronary vascular disease in children with developmental coordination disorder. J Adolesc Health. 2005;37:376–380. doi: 10.1016/j.jadohealth.2004.09.021. [DOI] [PubMed] [Google Scholar]
- 22.Stracciolini A., Myer G.D., Faigenbaum A.D. Exercise-deficit disorder in children: are we ready to make this diagnosis? Physiother Sport. 2013;41:94–101. doi: 10.3810/psm.2013.02.2003. [DOI] [PubMed] [Google Scholar]
- 23.Faigenbaum A.D., Myer G.D. Exercise deficit disorder in youth: play now or pay later. Curr Sports Med Rep. 2012;11:196–200. doi: 10.1249/JSR.0b013e31825da961. [DOI] [PubMed] [Google Scholar]
- 24.Lingam R., Golding J., Jongmans M.J., Hunt L.P., Ellis M., Emond A. The association between developmental coordination disorder and other developmental traits. Pediatrics. 2010;126:e1109–e1118. doi: 10.1542/peds.2009-2789. [DOI] [PubMed] [Google Scholar]
- 25.Green D., Charman T., Pickles A., Chandler S., Loucas T., Simonoff E., et al. Impairment in movement skills of children with autistic spectrum disorders. Dev Med Child Neurol. 2009;51:311–316. doi: 10.1111/j.1469-8749.2008.03242.x. [DOI] [PubMed] [Google Scholar]
- 26.Hilton C.L., Zhang Y., Whilte M.R., Klohr C.L., Constantino J. Motor impairment in sibling pairs concordant and discordant for autism spectrum disorders. Autism. 2012;16:430–441. doi: 10.1177/1362361311423018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaiser M.L., Schoemaker M.M., Albaret J.M., Geuze R.H. What is the evidence of impaired motor skills and motor control among children with attention deficit hyperactivity disorder (ADHD)? Systematic review of the literature. Res Dev Disabil. 2015;36c:338–357. doi: 10.1016/j.ridd.2014.09.023. [DOI] [PubMed] [Google Scholar]
- 28.Leonard H.C., Hill E.L. Review: the impact of motor development on typical and atypical social cognition and language: a systematic review. Child Adolesc Ment Health. 2014;19:163–170. doi: 10.1111/camh.12055. [DOI] [PubMed] [Google Scholar]
- 29.Fragala-Pinkham M.A., Haley S.M., Goodgold S. Evaluation of a community-based group fitness program for children with disabilities. Pediatr Phys Ther. 2006;18:159–167. doi: 10.1097/01.pep.0000223093.28098.12. [DOI] [PubMed] [Google Scholar]
- 30.Bonney E., Ferguson G., Smits-Engelsman B. Relationship between body mass index, cardiorespiratory and musculoskeletal fitness among South African adolescent girls. Int J Environ Res Publ Health. 2018;15:1087. doi: 10.3390/ijerph15061087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ferguson G.D., Naidoo N., Smits-Engelsman B.C. Health promotion in a low-income primary school: children with and without DCD benefit, but differently. Phys Occup Ther Pediatr. 2015;35:147–162. doi: 10.3109/01942638.2015.1009230. [DOI] [PubMed] [Google Scholar]
- 32.Armstrong M.E., Lambert E.V., Lambert M.I. Physical fitness of South African primary school children, 6 to 13 years of age: discovery vitality health of the nation study. Percept Mot Skills. 2011;113:999–1016. doi: 10.2466/06.10.13.PMS.113.6.999-1016. [DOI] [PubMed] [Google Scholar]
- 33.Pienaar A.E., Visagie M., Leonard A. Proficiency at object control skills BY nine- to ten-year-old children IN South Africa: the NW-child study. Percept Mot Skills. 2015;121:309–332. doi: 10.2466/10.PMS.121c15x8. [DOI] [PubMed] [Google Scholar]
- 34.Hua J., Jin H., Gu G., Liu M., Zhang L., Wu Z. The influence of Chinese one-child family status on developmental coordination disorder status. Res Dev Disabil. 2014;35:3089–3095. doi: 10.1016/j.ridd.2014.07.044. [DOI] [PubMed] [Google Scholar]
- 35.Ricken A.X., Bennett S.J., Savelsbergh G.J. Coordination of reaching in children with spastic hemiparetic cerebral palsy under different task demands. Mot Contr. 2005;9:357–371. doi: 10.1123/mcj.9.4.357. [DOI] [PubMed] [Google Scholar]
- 36.Logan S.W., Webster E.K., Getchell N., Pfeiffer K.A., Robinson L.E. Relationship between fundamental motor skill competence and physical activity during childhood and adolescence: a systematic review. Kinesiol Rev. 2015;4:416. [Google Scholar]
- 37.Stodden D.F., Langendorfer S.J., Goodway J.D., Roberton M.A., Rudisill M.E., Garcia C., et al. A developmental perspective on the role of motor skill competence in physical activity: an emergent relationship. Quest. 2008;60:290–306. [Google Scholar]
- 38.Maphatane M. Understanding support systems for Black street children and their families: an ecological perspective. Social Work Practice. 1994;2:22–30. [Google Scholar]
- 39.Martin E.H., Rudisill M.E., Hastie P.A. Motivational climate and fundamental motor skill performance in a naturalistic physical education setting. Phys Educ Sport Pedagog. 2009;14:227–240. [Google Scholar]
- 40.Barnett A.L., Hill E.L., Kirby A., Sugden D.A. Adaptation and extension of the European recommendations (EACD) on developmental coordination disorder (DCD) for the UK context. Phys Occup Ther Pediatr. 2015;35:103–115. doi: 10.3109/01942638.2014.957430. [DOI] [PubMed] [Google Scholar]
- 41.Hua J., Du W., Dai X., Wu M., Cai X., Shen M., et al. International clinical practice recommendations on the definition, diagnosis, assessment, intervention, and psychosocial aspects of developmental coordination disorder – Chinese (Mandarin) translation. Dev Med Child Neurol. 2019;61:e1. doi: 10.1111/dmcn.14693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Venetsanou F., Kambas A., Ellinoudis T., Fatouros I., Giannakidou D., Kourtessis T. Can the movement assessment battery for children-test be the "gold standard" for the motor assessment of children with Developmental Coordination Disorder? Res Dev Disabil. 2011;32:1–10. doi: 10.1016/j.ridd.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 43.Miyahara M., Lagisz M., Nakagawa S., Henderson S. Intervention for children with developmental coordination disorder: how robust is our recent evidence? Child Care Health Dev. 2020;46:397–406. doi: 10.1111/cch.12763. [DOI] [PubMed] [Google Scholar]
- 44.Preston N., Magallón S., Hill L.J., Andrews E., Ahern S.M., Mon-Williams M. A systematic review of high quality randomized controlled trials investigating motor skill programmes for children with developmental coordination disorder. Clin Rehabil. 2017;31:857–870. doi: 10.1177/0269215516661014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yu J.J., Burnett A.F., Sit C.H. Motor skill interventions in children with developmental coordination disorder: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2018;99:2076–2099. doi: 10.1016/j.apmr.2017.12.009. [DOI] [PubMed] [Google Scholar]
- 46.Geuze R.H., Schoemaker M.M., Smits-Engelsman B.C. Clinical and research criteria for developmental coordination disorder-should they Be one and the same? Curr Dev Disord Rep. 2015;2:127–130. doi: 10.1007/s40474-015-0043-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Smits-Engelsman B., Schoemaker M., Delabastita T., Hoskens J., Geuze R. Diagnostic criteria for DCD: past and future. Hum Mov Sci. 2015;42:293–306. doi: 10.1016/j.humov.2015.03.010. [DOI] [PubMed] [Google Scholar]
- 48.Cools W., Martelaer K.D., Samaey C., Andries C. Movement skill assessment of typically developing preschool children: a review of seven movement skill assessment tools. J Sports Sci Med. 2009;8:154–168. [PMC free article] [PubMed] [Google Scholar]
- 49.Ke L., Du W., Wang Y., Duan W., Hua J., Barnett A.L. The movement ABC-2 test in China: comparison with UK norms for 3-10 year olds. Res Dev Disabil. 2020;105:103742. doi: 10.1016/j.ridd.2020.103742. [DOI] [PubMed] [Google Scholar]
- 50.Niemeijer A.S., van Waelvelde H., Smits-Engelsman B.C. Crossing the north sea seems to make DCD disappear: cross-validation of movement assessment battery for children-2 norms. Hum Mov Sci. 2015;39:177–188. doi: 10.1016/j.humov.2014.11.004. [DOI] [PubMed] [Google Scholar]
- 51.Valentini N.C., Ramalho M.H., Oliveira M.A. Movement assessment battery for children-2: translation, reliability, and validity for Brazilian children. Res Dev Disabil. 2014;35:733–740. doi: 10.1016/j.ridd.2013.10.028. [DOI] [PubMed] [Google Scholar]
- 52.KÖSE B., ŞAHİN S., KARABULUT E., KAYIHAN H. Turkish Version of Bruininks-Oseretsky Test of Motor Proficiency 2 Brief Form: Its Validity and Reliability in Children with Specific Learning Disability. Bezmialem Science. 2021;9:198–204. [Google Scholar]
- 53.Okuda P.M.M., Pangelinan M., Capellini S.A., Cogo-Moreira H. Motor skills assessments: support for a general motor factor for the movement assessment battery for children-2 and the bruininks-oseretsky test of motor proficiency-2. Trends Psychiatry Psychother. 2019;41:51–59. doi: 10.1590/2237-6089-2018-0014. [DOI] [PubMed] [Google Scholar]
- 54.Vinçon S., Green D., Blank R., Jenetzky E. Ecological validity of the German bruininks-oseretsky test of motor proficiency - 2nd edition. Hum Mov Sci. 2017;53:45–54. doi: 10.1016/j.humov.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 55.Blackwell J.R., Newell K.M. The informational role of knowledge of results in motor learning. Acta Psychol. 1996;92:119–129. doi: 10.1016/0001-6918(95)00013-5. [DOI] [PubMed] [Google Scholar]
- 56.Kelso J.A., Zanone P.G. Coordination dynamics of learning and transfer across different effector systems. J Exp Psychol Hum Percept Perform. 2002;28:776–797. [PubMed] [Google Scholar]
- 57.Zanone P.G., Kelso J.A. Coordination dynamics of learning and transfer: collective and component levels. J Exp Psychol Hum Percept Perform. 1997;23:1454–1480. doi: 10.1037//0096-1523.23.5.1454. [DOI] [PubMed] [Google Scholar]
- 58.Smits-Engelsman B., Cavalcante Neto J.L., Draghi T.T.G., Rohr L.A., Jelsma D. Construct validity of the PERF-FIT, a test of motor skill-related fitness for children in low resource areas. Res Dev Disabil. 2020;102:103663. doi: 10.1016/j.ridd.2020.103663. [DOI] [PubMed] [Google Scholar]
- 59.Smits-Engelsman B.C.M., Bonney E., Neto J.L.C., Jelsma D.L. Feasibility and content validity of the PERF-FIT test battery to assess movement skills, agility and power among children in low-resource settings. BMC Publ Health. 2020;20:1139. doi: 10.1186/s12889-020-09236-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Smits-Engelsman B.C.M., Smit E., Doe-Asinyo R.X., Lawerteh S.E., Aertssen W., Ferguson G., et al. Inter-rater reliability and test-retest reliability of the Performance and Fitness (PERF-FIT) test battery for children: a test for motor skill related fitness. BMC Pediatr. 2021;21:119. doi: 10.1186/s12887-021-02589-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Schoemaker M.M., Niemeijer A.S., Flapper B.C., Smits-Engelsman B.C. Validity and reliability of the movement assessment battery for children-2 checklist for children with and without motor impairments. Dev Med Child Neurol. 2012;54:368–375. doi: 10.1111/j.1469-8749.2012.04226.x. [DOI] [PubMed] [Google Scholar]
- 62.Wilson B.N., Crawford S.G., Green D., Roberts G., Aylott A., Kaplan B.J. Psychometric properties of the revised developmental coordination disorder questionnaire. Phys Occup Ther Pediatr. 2009;29:182–202. doi: 10.1080/01942630902784761. [DOI] [PubMed] [Google Scholar]
- 63.Caravale B., Baldi S., Gasparini C., Wilson B.N. Cross-cultural adaptation, reliability and predictive validity of the Italian version of Developmental Coordination Disorder Questionnaire (DCDQ) Eur J Paediatr Neurol. 2014;18:267–272. doi: 10.1016/j.ejpn.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 64.Civetta L.R., Hillier S.L. The developmental coordination disorder questionnaire and movement assessment battery for children as a diagnostic method in Australian children. Pediatr Phys Ther. 2008;20:39–46. doi: 10.1097/PEP.0b013e31815ccaeb. [DOI] [PubMed] [Google Scholar]
- 65.Kennedy-Behr A., Wilson B.N., Rodger S., Mickan S. Cross-cultural adaptation of the developmental coordination disorder questionnaire 2007 for German-speaking countries: dcdq-g. Neuropediatrics. 2013;44:245–251. doi: 10.1055/s-0033-1347936. [DOI] [PubMed] [Google Scholar]
- 66.Schoemaker M.M., Flapper B., Verheij N.P., Wilson B.N., Reinders-Messelink H.A., de Kloet A. Evaluation of the developmental coordination disorder questionnaire as a screening instrument. Dev Med Child Neurol. 2006;48:668–673. doi: 10.1017/S001216220600140X. [DOI] [PubMed] [Google Scholar]
- 67.Tseng M.H., Fu C.P., Wilson B.N., Hu F.C. Psychometric properties of a Chinese version of the developmental coordination disorder questionnaire in community-based children. Res Dev Disabil. 2010;31:33–45. doi: 10.1016/j.ridd.2009.07.018. [DOI] [PubMed] [Google Scholar]
- 68.van der Linde B.W., van Netten J.J., Otten B.E., Postema K., Geuze R.H., Schoemaker M.M. Development and psychometric properties of the DCDDaily: a new test for clinical assessment of capacity in activities of daily living in children with developmental coordination disorder. Clin Rehabil. 2013;27:834–844. doi: 10.1177/0269215513481227. [DOI] [PubMed] [Google Scholar]
- 69.Howie E.K., Pate R.R. Physical activity and educational achievement. Routledge; 2017. Physical activity and educational achievement: dose–response relationships. [Google Scholar]
- 70.Aertssen W., Jelsma D., Smits-Engelsman B. Field-based tests of strength and anaerobic capacity used in children with developmental coordination disorder: a systematic review. Phys Ther. 2020;100:1825–1851. doi: 10.1093/ptj/pzaa118. [DOI] [PubMed] [Google Scholar]
- 71.Smits-Engelsman B., Bonney E., Ferguson G. Effects of graded exergames on fitness performance in elementary school children with developmental coordination disorder. Front Sports Act Living. 2021;3:653851. doi: 10.3389/fspor.2021.653851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Verbecque E., Johnson C., Rameckers E., Thijs A., van der Veer I., Meyns P., et al. Balance control in individuals with developmental coordination disorder: a systematic review and meta-analysis. Gait Posture. 2021;83:268–279. doi: 10.1016/j.gaitpost.2020.10.009. [DOI] [PubMed] [Google Scholar]
- 73.Dewar R., Claus A.P., Tucker K., Johnston L.M. Perspectives on postural control dysfunction to inform future research: a delphi study for children with cerebral palsy. Arch Phys Med Rehabil. 2017;98:463–479. doi: 10.1016/j.apmr.2016.07.021. [DOI] [PubMed] [Google Scholar]
- 74.Horak F.B., Wrisley D.M., Frank J. The balance evaluation systems test (BESTest) to differentiate balance deficits. Phys Ther. 2009;89:484–498. doi: 10.2522/ptj.20080071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Crane L., Sumner E., Hill E.L. Emotional and behavioural problems in children with Developmental Coordination Disorder: exploring parent and teacher reports. Res Dev Disabil. 2017;70:67–74. doi: 10.1016/j.ridd.2017.08.001. [DOI] [PubMed] [Google Scholar]
- 76.van den Heuvel M., Jansen D.E., Reijneveld S.A., Flapper B.C., Smits-Engelsman B.C. Identification of emotional and behavioral problems by teachers in children with developmental coordination disorder in the school community. Res Dev Disabil. 2016;51–52:40–48. doi: 10.1016/j.ridd.2016.01.008. [DOI] [PubMed] [Google Scholar]
- 77.Schoemaker M.M., Houwen S. Health-related quality of life in children with developmental disorders. Current Developmental Disorders Reports. 2021;8:69–76. [Google Scholar]
- 78.Tamplain P., Sherrod G.M., Fuchs C., Miller H.L. Preliminary improvements in dynamic postural control after A group-based intervention program for children with developmental coordination disorder: a brief report. Dev Neurorehabil. 2021;24:63–67. doi: 10.1080/17518423.2020.1819463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Barnett L.M., Hnatiuk J.A., D'Souza N., Salmon J., Hesketh K.D. What factors help young children develop positive perceptions of their motor skills? Int J Environ Res Publ Health. 2021;18:759. doi: 10.3390/ijerph18020759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Who . World Health Organization; Geneva: 2007. International classification of functioning, disability and health for children and youth (ICF-CY) [Google Scholar]
- 81.Smits-Engelsman B.C., Blank R., van der Kaay A.C., Mosterd-van der Meijs R., Vlugt-van den Brand E., Polatajko H.J., et al. Efficacy of interventions to improve motor performance in children with developmental coordination disorder: a combined systematic review and meta-analysis. Dev Med Child Neurol. 2013;55:229–237. doi: 10.1111/dmcn.12008. [DOI] [PubMed] [Google Scholar]
- 82.Novak I., Honan I. Effectiveness of paediatric occupational therapy for children with disabilities: a systematic review. Aust Occup Ther J. 2019;66:258–273. doi: 10.1111/1440-1630.12573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hillier S. Intervention for children with developmental coordination disorder: a systematic review. Internet J Allied Health Sci Pract. 2007;5:1–11. [Google Scholar]
- 84.Kümmel J., Kramer A., Giboin L.S., Gruber M. Specificity of balance training in healthy individuals: a systematic review and meta-analysis. Sports Med. 2016;46:1261–1271. doi: 10.1007/s40279-016-0515-z. [DOI] [PubMed] [Google Scholar]
- 85.Jarani J., Grøntved A., Muca F., Spahi A., Qefalia D., Ushtelenca K., et al. Effects of two physical education programmes on health- and skill-related physical fitness of Albanian children. J Sports Sci. 2016;34:35–46. doi: 10.1080/02640414.2015.1031161. [DOI] [PubMed] [Google Scholar]
- 86.Bonney E., Jelsma D., Ferguson G., Smits-Engelsman B. Variable training does not lead to better motor learning compared to repetitive training in children with and without DCD when exposed to active video games. Res Dev Disabil. 2017;62:124–136. doi: 10.1016/j.ridd.2017.01.013. [DOI] [PubMed] [Google Scholar]
- 87.Bonney E., Rameckers E., Ferguson G., Smits-Engelsman B. "Not just another Wii training": a graded Wii protocol to increase physical fitness in adolescent girls with probable developmental coordination disorder-a pilot study. BMC Pediatr. 2018;18:78. doi: 10.1186/s12887-018-1029-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Smits-Engelsman B., Bonney E., Ferguson G. Motor skill learning in children with and without developmental coordination disorder. Hum Mov Sci. 2020;74:102687. doi: 10.1016/j.humov.2020.102687. [DOI] [PubMed] [Google Scholar]
- 89.Cavalcante Neto J.L., Steenbergen B., Wilson P., Zamunér A.R., Tudella E. Is Wii-based motor training better than task-specific matched training for children with developmental coordination disorder? A randomized controlled trial. Disabil Rehabil. 2020;42:2611–2620. doi: 10.1080/09638288.2019.1572794. [DOI] [PubMed] [Google Scholar]
- 90.Jelsma L.D., Smits-Engelsman B.C., Krijnen W.P., Geuze R.H. Changes in dynamic balance control over time in children with and without Developmental Coordination Disorder. Hum Mov Sci. 2016;49:148–159. doi: 10.1016/j.humov.2016.07.003. [DOI] [PubMed] [Google Scholar]
- 91.Missiuna C., Rivard L., Bartlett D. Exploring assessment tools and the target of intervention for children with Developmental Coordination Disorder. Phys Occup Ther Pediatr. 2006;26:71–89. [PubMed] [Google Scholar]
- 92.Adi-Japha E., Brestel G. Motor skill learning with impaired transfer by children with developmental coordination disorder. Res Dev Disabil. 2020;103:103671. doi: 10.1016/j.ridd.2020.103671. [DOI] [PubMed] [Google Scholar]
- 93.Sween J., Wallington S.F., Sheppard V., Taylor T., Llanos A.A., Adams-Campbell L.L. The role of exergaming in improving physical activity: a review. J Phys Activ Health. 2014;11:864–870. doi: 10.1123/jpah.2011-0425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ferguson G.D., Jelsma D., Jelsma J., Smits-Engelsman B.C. The efficacy of two task-orientated interventions for children with developmental coordination disorder: neuromotor task training and nintendo wii fit training. Res Dev Disabil. 2013;34:2449–2461. doi: 10.1016/j.ridd.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 95.MacArthur B., Coe D., Sweet A., Raynor H. Active videogaming compared to unstructured, outdoor play in young children: percent time in moderate- to vigorous-intensity physical activity and estimated energy expenditure. Game Health J. 2014;3:388–394. doi: 10.1089/g4h.2014.0017. [DOI] [PubMed] [Google Scholar]
- 96.Bonney E., Ferguson G., Smits-Engelsman B. The efficacy of two activity-based interventions in adolescents with Developmental Coordination Disorder. Res Dev Disabil. 2017;71:223–236. doi: 10.1016/j.ridd.2017.10.013. [DOI] [PubMed] [Google Scholar]
- 97.Sober S.J., Sabes P.N. Multisensory integration during motor planning. J Neurosci. 2003;23:6982–6992. doi: 10.1523/JNEUROSCI.23-18-06982.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kleim J.A., Jones T.A. Principles of experience-dependent neural plasticity: implications for rehabilitation after brain damage. J Speech Lang Hear Res. 2008;51:S225–S239. doi: 10.1044/1092-4388(2008/018). [DOI] [PubMed] [Google Scholar]
- 99.Adams I.L.J., Broekkamp W., Wilson P.H., Imms C., Overvelde A., Steenbergen B. Role of pediatric physical therapists in promoting sports participation in developmental coordination disorder. Pediatr Phys Ther. 2018;30:106–111. doi: 10.1097/PEP.0000000000000485. [DOI] [PubMed] [Google Scholar]
- 100.Lopes L., Santos R., Coelho E.S.M., Draper C., Mota J., Jidovtseff B., et al. A narrative review of motor competence in children and adolescents: what we know and what we need to find out. Int J Environ Res Publ Health. 2020;18:18. doi: 10.3390/ijerph18010018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Faigenbaum A.D., Farrell A., Fabiano M., Radler T., Naclerio F., Ratamess N.A., et al. Effects of integrative neuromuscular training on fitness performance in children. Pediatr Exerc Sci. 2011;23:573–584. doi: 10.1123/pes.23.4.573. [DOI] [PubMed] [Google Scholar]
- 102.Novak C., Lingam R., Coad J., Emond A. 'Providing more scaffolding': parenting a child with developmental co-ordination disorder, a hidden disability. Child Care Health Dev. 2012;38:829–835. doi: 10.1111/j.1365-2214.2011.01302.x. [DOI] [PubMed] [Google Scholar]
- 103.Cairney J., Hay J.A., Faught B.E., Wade T.J., Corna L., Flouris A. Developmental coordination disorder, generalized self-efficacy toward physical activity, and participation in organized and free play activities. J Pediatr. 2005;147:515–520. doi: 10.1016/j.jpeds.2005.05.013. [DOI] [PubMed] [Google Scholar]
- 104.García-Hermoso A., Ramírez-Campillo R., Izquierdo M. Is muscular fitness associated with future health benefits in children and adolescents? A systematic review and meta-analysis of longitudinal studies. Sports Med. 2019;49:1079–1094. doi: 10.1007/s40279-019-01098-6. [DOI] [PubMed] [Google Scholar]
- 105.Smith J.J., Eather N., Weaver R.G., Riley N., Beets M.W., Lubans D.R. Behavioral correlates of muscular fitness in children and adolescents: a systematic review. Sports Med. 2019;49:887–904. doi: 10.1007/s40279-019-01089-7. [DOI] [PubMed] [Google Scholar]
- 106.Faigenbaum A.D., MacDonald J.P., Stracciolini A., Rebullido T.R. Making a strong case for prioritizing muscular fitness in youth physical activity guidelines. Curr Sports Med Rep. 2020;19:530–536. doi: 10.1249/JSR.0000000000000784. [DOI] [PubMed] [Google Scholar]
- 107.Faigenbaum A.D., Best T.M., MacDonald J., Myer G.D., Stracciolini A. Top 10 research questions related to exercise deficit disorder (EDD) in youth. Res Q Exerc Sport. 2014;85:297–307. doi: 10.1080/02701367.2014.931179. [DOI] [PubMed] [Google Scholar]
- 108.Rivilis I., Hay J., Cairney J., Klentrou P., Liu J., Faught B.E. Physical activity and fitness in children with developmental coordination disorder: a systematic review. Res Dev Disabil. 2011;32:894–910. doi: 10.1016/j.ridd.2011.01.017. [DOI] [PubMed] [Google Scholar]
- 109.Raz-Silbiger S., Lifshitz N., Katz N., Steinhart S., Cermak S.A., Weintraub N. Relationship between motor skills, participation in leisure activities and quality of life of children with Developmental Coordination Disorder: temporal aspects. Res Dev Disabil. 2015;38:171–180. doi: 10.1016/j.ridd.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 110.Andersen L.B., Mota J., Di Pietro L. Update on the global pandemic of physical inactivity. Lancet. 2016;388:1255–1256. doi: 10.1016/S0140-6736(16)30960-6. [DOI] [PubMed] [Google Scholar]
- 111.Kohl H.W., 3rd, Craig C.L., Lambert E.V., Inoue S., Alkandari J.R., Leetongin G., et al. The pandemic of physical inactivity: global action for public health. Lancet. 2012;380:294–305. doi: 10.1016/S0140-6736(12)60898-8. [DOI] [PubMed] [Google Scholar]
- 112.Hallal P.C., Andersen L.B., Bull F.C., Guthold R., Haskell W., Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380:247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]