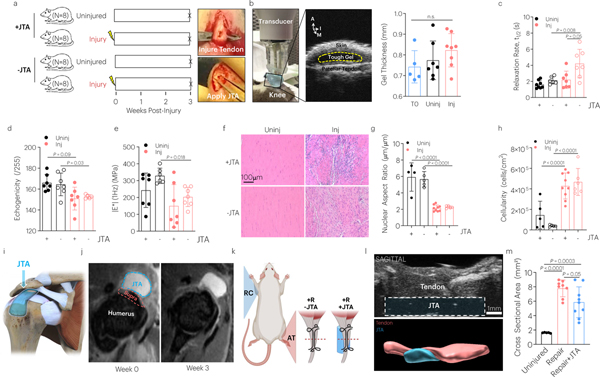
Fig. 4 |. The JTA is biocompatible to tendon and supports healing.
(a) The effect of patellar tendon injury and JTA implantation on tendon structural and mechanical properties was investigated. Following injury, the JTA was applied on the central midsubstance of the patellar tendon. (b) At 3-weeks post implantation, gel thickness was evaluated using high frequency ultrasound. Mean values are shown and error bars are ± s.d. (n=5–8 samples/group), as analyzed by a one-way ANOVA. A- Anterior; I- Inferior; M- Medial. (c-e) The effect of healing and JTA implantation on patellar tendon relaxation half-life, echogenicity, and |E*| was evaluated. Mean values are shown and error bars are +s.d. (n=6–8 samples/group), as analyzed by a two-way ANOVA with post hoc t-tests with Bonferroni corrections. (f-h) The effect of healing and JTA implantation on patellar tendon nuclear aspect ratio and cellularity was evaluated. Scale bar = 100 μm. Mean values are shown and error bars are ± s.d. (n=4–8 samples/group), as analyzed by a two-way ANOVA with post hoc t-tests with Bonferroni correction. (i,k) The JTA was designed to be placed over the supraspinatus tendon and pass under the acromion for testing in the rotator cuff. (j) T2-weighted MRI images were acquired from the rotator cuff to examine JTA placement and material compatibility over time. (k) The effect of the JTA on Achilles tendon healing in a repair model was evaluated. (l) Sagittal high frequency ultrasound imaging evaluated JTA (blue) placement over time adjacent to the Achilles tendon (red). (m) Axial high frequency ultrasound imaging examined the effect of tendon repair with and without the JTA on Achilles tendon cross sectional area. Mean values are shown and error bars are ± s.d. (n=8–9 tendons/group), as analyzed by a one-way ANOVA with post hoc t-tests with Bonferroni corrections.