Abstract
Background: Diabetic nephropathy (DN) and diabetic retinopathy (DR) are microvascular complications of diabetes that share a similar pathogenesis and clinical relevance. The study aimed to visually analyze the research status and development trend of the relationship between DN and DR by means of bibliometrics and knowledge mapping.
Methods: Publications were collected from the Science Citation Index-Expanded of the Web of Science Core Collection between 2000 and 2021. CiteSpace, Alluvial Generator, and Microsoft Excel were used to analyze and present the data.
Results: A total of 3,348 publications were retrieved and 3,285 were included in the analysis after deduplication. The publications demonstrated an annually increasing trend. The results of the collaborative network analysis showed that the United States, Steno Diabetes Center, and Tien Y. Wong were the most influential country, institution and author, in this field of research, respectively. The analysis of references and keywords showed that the pathogenesis of DN and DR and their relationship with cardiovascular disease are research hotspots. The clinical relevance and drug therapy for DN and DR will become frontiers of future research in this field.
Conclusion: This study is the first to visualize the correlation between DN and DR using a bibliometric approach. This study provides a reference of research trends for scholars.
Keywords: diabetic nephropathy, diabetic retinopathy, diabetes, bibliometrics, citespace
Introduction
Diabetes is a worldwide public health problem that affects millions of people of all ages, sexes, and racial and ethnic groups (Rangel et al., 2019). The International Diabetes Federation (IDF) report estimated that in 2021, 536.6 million people worldwide had diabetes. These figures are expected to increase to 783.2 million by 2045 (Sun et al., 2022). Diabetic nephropathy (DN) and diabetic retinopathy (DR) are two major microvascular complications of diabetes that increase all-cause and cardiovascular disease (CVD)-related mortality (Sabanayagam et al., 2019).
DN is the leading cause of end-stage renal disease, accounting for approximately 50% of cases in developed countries (Tuttle et al., 2014). DN is a clinical syndrome characterized by persistent albuminuria, elevated arterial blood pressure, a relentless decline in the glomerular filtration rate, and a high risk of cardiovascular morbidity and mortality (Jawa et al., 2004). Moreover, the prevalence rate of DN in patients with type 2 diabetes is reported to be 41.3% (Tong et al., 2020).
DR is the most common and serious ocular complication of diabetes (Cheung et al., 2010). It is the leading cause of blindness and visual impairment in adults (Congdon et al., 2003). More than one-third of people with diabetes have signs of DR, and one-third of those with DR have vision-threatening DR (Yau et al., 2012). DN and DR share a similar pathogenesis and common risk factors (Tsilibary, 2003; Wong et al., 2014). Srivastav et al. revealed that in DR, deranged serum urea and creatinine levels can augment the damage to the retinal neural tissue (Srivastav et al., 2015). Additionally, Zhuang et al. demonstrated that stage of estimated glomerular filtration rate (eGFR) and urine albumin-to-creatinine ratio (UACR) were associated with the stage of DR and diabetic macular edema development (Zhuang et al., 2019). Finally, vascular abnormalities in DR are predictors of impaired renal function and microalbuminuria is an accurate biomarker of DR progression (Pan et al., 2021).
Currently, renal microvessel examination is mainly performed by histological examination, namely renal biopsy, which is an invasive operation. The retinal microvasculature is the only part of the human circulatory system that can be directly visualized non-invasively in vivo, readily photographed, and subjected to digital image analysis (Patton et al., 2006). Thus, the retinal vessels offer a unique and easily accessible window to study the health and disease of the human microcirculation. Moreover, the kidney and retina have similar anatomical and physiological characteristics (Cheung et al., 2012). Therefore, the study of the correlation between DN and DR will provide the possibility of non-invasive operation for the detection of DN.
Bibliometrics is seen as a valuable quantitative and qualitative method for evaluating scientific production, and its influence is growing (Ellegaard and Wallin, 2015; Liu et al., 2021). Bibliometrics applies mathematical and statistical methods to the analysis of scholarly publications to understand research hotspots and research fronts in specific fields of study. Many current applications of bibliometrics in medical science and healthcare can be used to discover new information about academic trends, pharmacotherapy, disease, and broader health sciences trends (Thompson and Walker, 2015). The results of bibliometric analysis help to identify gaps in research hotspots and can be used for future studies with more forward connections (Kumar et al., 2021; Kumar and Goel, 2021). Bibliometrics has been applied to the respective fields of DN and DR (Zou and Sun, 2019; Li X. J. et al., 2021), and previous studies have demonstrated a link between these two diseases (Yun et al., 2016; Hsieh and Hsieh, 2021). However, no systematic visual analysis of topics in this field has been performed using bibliometric methods. Therefore, this study aimed to visually analyze the research status and development trends of the relationship between DN and DR by means of bibliometrics and knowledge mapping.
Materials and Methods
To analyze research trends, references and keywords analysis of the association between DN and DR, CiteSpace, Alluvial Generator, and Microsoft Excel are used (Figure 1).
FIGURE 1.
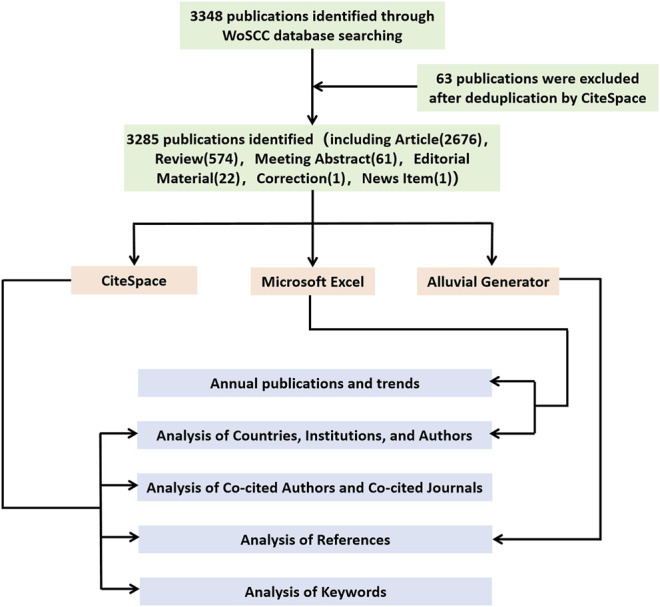
Flow diagram of the publications screening process and bibliometric analysis methods.
Data Source and Search Strategy
Science Citation Index Expanded (SCI-E) from the Web of Science Core Collection (WoSCC) was used as the data source. The search expressions were constructed as follows: TS = (Diabetic Retinopathy) AND TS = (Diabetic Nephropathies or Diabetic Nephropathy or Diabetic Kidney Disease or Diabetic Glomerulosclerosis or Intracapillary Glomerulosclerosis or Nodular Glomerulosclerosis or Kimmelstiel-Wilson Syndrome or Kimmelstiel Wilson Syndrome or Kimmelstiel-Wilson Disease or Kimmelstiel Wilson Disease). The publication period in this study was set between 2000 and 2021. All searches were completed on the same day on February 24, 2022. No restrictions on the type or language of the publications was set. A total of 3,348 publications were retrieved, and after deduplication with CiteSpace, 3,285 publications were included in the analysis (Figure 1). These 3,285 publications were exported to CiteSpace and Alluvial Generator for further analysis.
Bibliometric Analysis and Software Assistance
In this study, CiteSpace v.5.8. R3 (64-bit) software was used to draw a knowledge map of the research status and trends of the association between DN and DR. CiteSpace is an information visualization software developed by Professor Chen Chaomei using Java language. CiteSpace supports visual exploration with knowledge discovery in bibliographic databases. It provides a wide range of users with a visual mapping tool to explore areas of expertise and the emergence of research topics within knowledge areas, and to identify emerging trends and transient patterns in the scientific literature (Chen and Chen, 2005; Synnestvedt et al., 2005).
The visual graphs produced by CiteSpace consist of nodes and lines. The size of the node represents the frequency. Moreover, the connection between nodes represents the strength of cooperation; the thicker the connection, the stronger the cooperation. In addition, nodes with betweenness centrality >0.1 are usually marked with purple circles. The larger the centrality value, the more cooperative the node is with other nodes. Log-Likelihood Ratio (LLR) algorithm was chosen to cluster co-cited references and keywords. Each cluster is composed of multiple closely related words. The smaller the number of cluster labels, the more references or keywords are included in that cluster. The silhouette (S) value refers to the average contour value of the cluster. It is generally considered that, with an S > 0.5, the cluster is reasonable, while with an S > 0.7, the cluster is convincing (Chen et al., 2012).
For this study, the specific parameters of CiteSpace were set as follows: 1) Time Slicing: From January 2000 to December 2021; Years Per Slice: 1; 2) Term Source: Title, Abstract, Author, Keywords, and Keyword Plus; 3) Node Types: Author, Institution, Country, Keyword, Reference, Cited Author, and Cited Journal; 4) Selection Criteria: Top N = 50.
Alluvial Generator was used to draw an alluvial flow map showing the change process of co-cited documents in the past 5 years (2017-2021). The modules of publications cited in these five consecutive years are colored, indicating that the document has received a high degree of attention in this time frame.
Microsoft Excel was used to construct tables, make rose charts, and demonstrate the annual national trends in publications.
Results
There were 6 document types in 3,285 publications from 2000 to 2021. Among them, articles were the most (2,676), followed by reviews (574), meeting abstracts (61), editorial materials (22), collection 1) and news item 1) (Figure 1).
Annual Publications and Trends
From 2000 to 2021, the SCI-E of the WoSCC database included a total of 3,285 publications on DN and DR. As shown in Figure 2, the number of publications related to DN and DR from 2000 to 2021 showed a fluctuating upward trend. The number of publications in 2001, 2002, 2006, 2009, 2013, 2017, and 2021 declined, while the number of publications in the rest of the years rose. The most publications in 1 year occurred in 2020 and reached 249 articles. The polynomial curve fitting between year and number of annual publications was drawn to better understand the trends in publications on DN and DR. As presented in Figure 2, the correlation coefficient R-square of the equation reached 0.9423.
FIGURE 2.
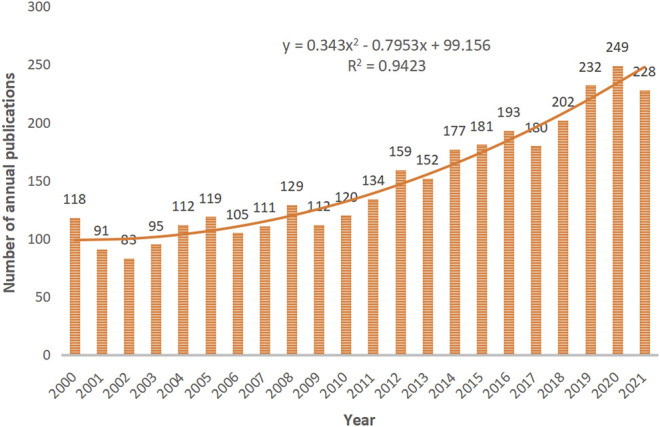
The number of annual publications on DN and DR research between 2000 and 2021. The horizontal coordinates represent the year of publication. The vertical coordinates represent the number of publications.
Analysis of Countries, Institutions, and Authors
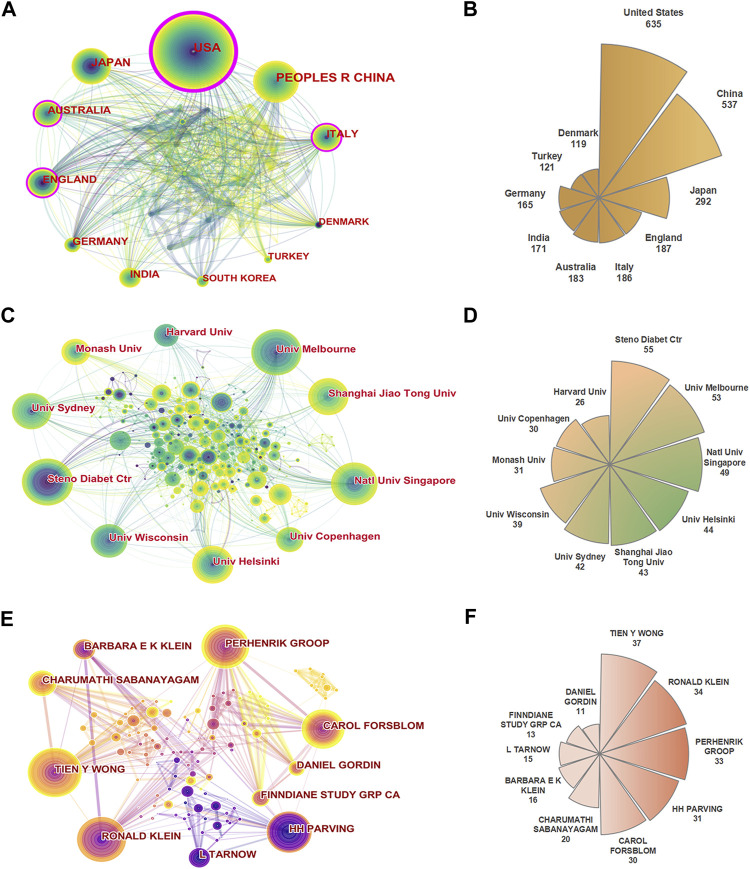
To understand the contribution of each country to the research field of DN and DR, the global collaboration network analysis is shown in Figure 3A. The United States (635) had the most publications, followed by China (537), Japan (292), England (187), and Italy (186) (Figure 3B). Regarding the centrality of countries, the United States (0.32) ranked first, followed by Italy (0.17), Australia (0.14), England (0.13), and Saudi Arabia (0.08) (Table 1). The United States is not only a major research center on DN and DR, but also has close cooperation with many countries such as China, Australia, and Japan in this field of research.
FIGURE 3.
(A) The collaboration network of countries. (B) Rose chart of the top 10 productive countries. (C) The collaboration network of institutions. (D) Rose chart of the top 10 productive institutions. (E) The collaboration network of authors. (F) Rose chart of the top 10 productive authors.
TABLE 1.
Top 10 publication counts and centralities of countries, institutions, and authors.
| Items | Rank | Count | Name | Rank | Centrality | Name |
|---|---|---|---|---|---|---|
| Country | 1 | 635 | United States | 1 | 0.32 | United States |
| 2 | 537 | China | 2 | 0.17 | Italy | |
| 3 | 292 | Japan | 3 | 0.14 | Australia | |
| 4 | 187 | England | 4 | 0.13 | England | |
| 5 | 186 | Italy | 5 | 0.08 | Saudi Arabia | |
| 6 | 183 | Australia | 6 | 0.08 | Malaysia | |
| 7 | 171 | India | 7 | 0.07 | Germany | |
| 8 | 165 | Germany | 8 | 0.06 | India | |
| 9 | 121 | Turkey | 9 | 0.06 | France | |
| 10 | 119 | Denmark | 10 | 0.05 | China | |
| Institution | 1 | 55 | Steno Diabet Ctr | 1 | 0.09 | Steno Diabet Ctr |
| 2 | 53 | Univ Melbourne | 2 | 0.09 | Harvard Univ | |
| 3 | 49 | Natl Univ Singapore | 3 | 0.09 | Univ Tokyo | |
| 4 | 44 | Univ Helsinki | 4 | 0.08 | Univ Melbourne | |
| 5 | 43 | Shanghai Jiao Tong Univ | 5 | 0.08 | Natl Univ Singapore | |
| 6 | 42 | Univ Sydney | 6 | 0.06 | Univ Toronto | |
| 7 | 39 | Univ Wisconsin | 7 | 0.05 | Univ Helsinki | |
| 8 | 31 | Monash Univ | 8 | 0.05 | Shanghai Jiao Tong Univ | |
| 9 | 30 | Univ Copenhagen | 9 | 0.05 | Tianjin Med Univ | |
| 10 | 26 | Harvard Univ | 10 | 0.04 | Univ Sydney | |
| Author | 1 | 37 | Tien Y. Wong | 1 | 0.01 | Tien Y. Wong |
| 2 | 34 | Ronald Klein | 2 | 0.01 | Ronald Klein | |
| 3 | 33 | Per-henrik Groop | 3 | 0.01 | Per-henrik Groop | |
| 4 | 31 | Hans-Henrik Parving | 4 | 0.01 | Hans-Henrik Parving | |
| 5 | 30 | Carol Forsblom | 5 | 0 | Carol Forsblom | |
| 6 | 20 | Charumathi Sabanayagam | 6 | 0 | Charumathi Sabanayagam | |
| 7 | 16 | Barbara E. K. Klein | 7 | 0 | Barbara E. K. Klein | |
| 8 | 15 | Lise Tarnow | 8 | 0 | Lise Tarnow | |
| 9 | 13 | FinnDiane Study Group | 9 | 0 | FinnDiane Study Group | |
| 10 | 11 | Daniel Gordin | 10 | 0 | Daniel Gordin |
Through the analysis of research institutions, scholars can understand the global distribution of institutions conducting research on the correlation between DN and DR, and then provide a basis for seeking cooperating institutions during research (Figure 3C). The top 10 institutions according to the number of publications came from 5 countries, namely Denmark (Steno Diabetes Center, University of Copenhagen), Australia (University of Melbourne, University of Sydney, Monash University), Singapore (National University of Singapore), Finland (University of Helsinki), China (Shanghai Jiao Tong University), and the United States (University of Wisconsin, Harvard University). The institution with the most publications was Steno Diabetes Center (55), followed by University of Melbourne (53), National University of Singapore (49), University of Helsinki (44) and Shanghai Jiao Tong University (43). In terms of centrality, the top 5 institutions were Steno Diabetes Center (0.09), Harvard University (0.09), University of Tokyo (0.09), University of Melbourne (0.08) and National University of Singapore (0.08) (Figure 3D; Table 1).
Figure 3E shows the collaboration network of authors, which provides a basis for finding research partners and identifying industry giants. The author with the most publications was Tien Y. Wong (37), followed by Ronald Klein (34), Per-henrik Groop (33), Hans-Henrik Parving (31), and Carol Forsblom (30) (Figure 3F). The top 4 authors according to centrality were Tien Y. Wong (0.04), Ronald Klein (0.04), Per-henrik Groop (0.04), and Hans-Henrik Parving (0.04) (Table 1).
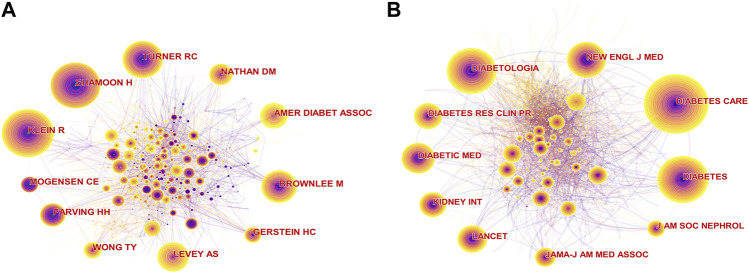
Analysis of Co-Cited Authors and Co-Cited Journals
Co-cited authors in this field of research are presented in Figure 4A. The top 5 co-cited authors by citation frequency were Ronald Klein (486), Harry Shamoon (471), Robert C. Turner (388), Michael Brownlee (347), and Andrew S. Levey (308). The top 5 co-cited authors for centrality were Lloyd Paul Aiello (0.08), followed by Michael Brownlee (0.07), Hans-Henrik Parving (0.07), Paola Fioretto (0.07), and Antonio Ceriello (0.06) (Table 2).
FIGURE 4.
(A) The collaboration network of co-cited authors. (B) The collaboration network of co-cited journals.
TABLE 2.
Top 10 publication counts and centralities of co-cited authors and co-cited journals.
| Items | Rank | Count | Name | Rank | Centrality | Name |
|---|---|---|---|---|---|---|
| Co-cited author | 1 | 486 | Ronald Klein | 1 | 0.08 | Lloyd Paul Aiello |
| 2 | 471 | Harry Shamoon | 2 | 0.07 | Michael Brownlee | |
| 3 | 388 | Robert C. Turner | 3 | 0.07 | Hans-Henrik Parving | |
| 4 | 347 | Michael Brownlee | 4 | 0.07 | Paola Fioretto | |
| 5 | 308 | Andrew S. Levey | 5 | 0.06 | Antonio Ceriello | |
| 6 | 274 | American Diabetes Association | 6 | 0.05 | Robert C. Turner | |
| 7 | 264 | Hans-Henrik Parving | 7 | 0.05 | Andrzej S. Krolewski | |
| 8 | 240 | David M. Nathan | 8 | 0.05 | Hans-Peter Hammes | |
| 9 | 192 | Carl Erik Mogensen | 9 | 0.05 | Nish Chaturvedi | |
| 10 | 188 | Hertzel C. Gerstein | 10 | 0.05 | Trevor J. Orchard | |
| Co-cited journal | 1 | 2,517 | Diabetes Care | 1 | 0.05 | J. Cardiovasc. Pharm. |
| 2 | 2,102 | Diabetologia | 2 | 0.04 | Eur. J. Pharmacol. | |
| 3 | 2018 | Diabetes | 3 | 0.04 | Curr. Eye Res. | |
| 4 | 1698 | New Engl. J. Med. | 4 | 0.04 | Mol. Cell Biochem. | |
| 5 | 1393 | Diabetic Med. | 5 | 0.04 | Cancer Res. | |
| 6 | 1321 | Lancet | 6 | 0.03 | J. Intern. Med. | |
| 7 | 1260 | Diabetes Res. Clin. Pr. | 7 | 0.03 | Free Radical Bio. Med. | |
| 8 | 1246 | Kidney Int. | 8 | 0.03 | Endocrinology | |
| 9 | 1043 | JAMA | 9 | 0.03 | Febs. Lett. | |
| 10 | 932 | J. Am. Soc. Nephrol. | 10 | 0.03 | Brit. J. Pharmacol. |
In the analysis of co-cited journals (Figure 4B), identifying the core journals in the field is beneficial. The highest frequency among co-cited journals was Diabetes Care (2,517), followed by Diabetologia (2,102), Diabetes (2018), New Engl. J Med. (1698), and Diabetic Med. (1393). The top 5 co-cited journals for centrality were J. Cardiovasc. Pharm. (0.05), Eur. J. Pharmacol. (0.04), Curr. Eye Res. (0.04), Mol. Cell Biochem. (0.04), and Cancer Res. (0.04) (Table 2).
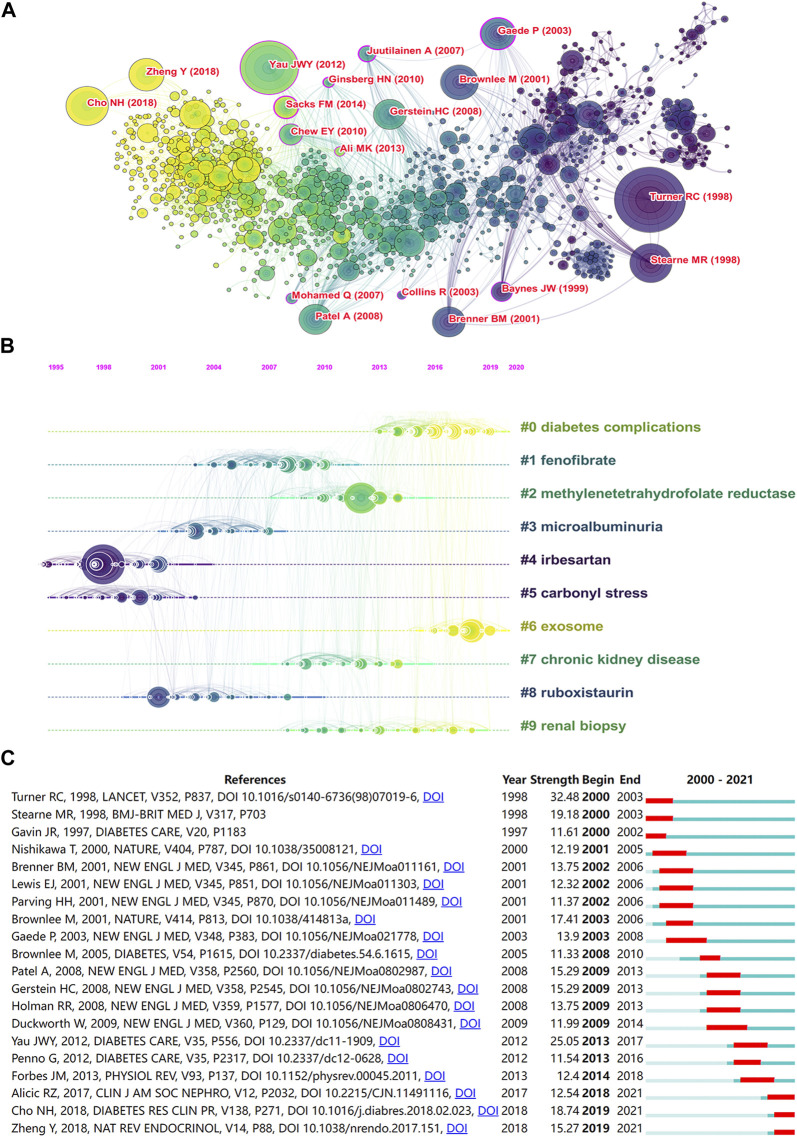
Analysis of References
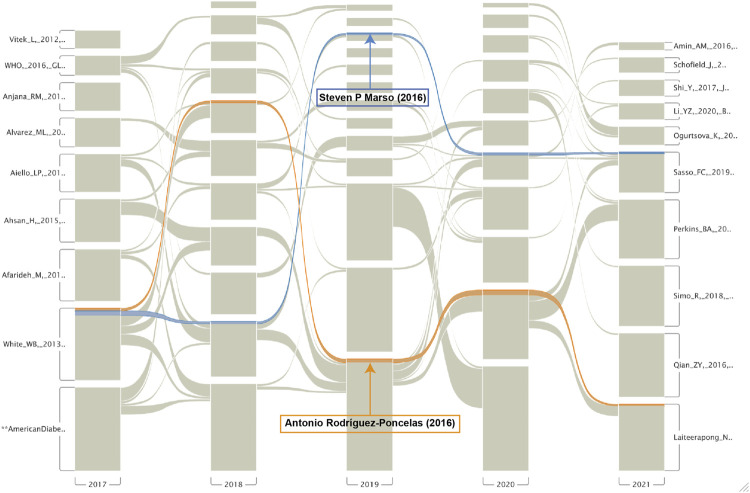
As shown in Figure 5A and Table 3, “Turner RC (1998), Yau et al. (2012), Stearne MR (1998), and Cho NH (2018)” were frequently cited references. Top 10 clusters of co-cited references were found. The S values of the top 10 clusters were all above 0.7, indicating that these clusters were convincing (Table 4). The top five cluster labels were “diabetes complications,” “fenofibrate,” “methylenetetrahydrofolate reductase,” “microalbuminuria,” and “irbesartan.” The largest cluster of “diabetes complications” indicated that studies related to diabetes complications may be the current research hotspot. The timeline view of co-cited references (Figure 5B) shows that irbesartan and carbonyl stress were early research areas for DN and DR. Additionally, diabetes complications and exosome were shown to be the current research hotspots in DN and DR. The top 20 references with the strongest citation bursts are shown in Figure 5C. The highest burst strength was from Turner RC (1998). Furthermore, Radica Z. Alicic (2017), NH Cho (2018), and Yan Zheng (2018) received more attention in recent years. The alluvial flow map shown in Figure 6 represents the most cited references from 2017 to 2021, with Marso et al. (2016) and Rodríguez-Poncelas (2016) cited for five consecutive years.
FIGURE 5.
(A) The network of co-cited references. (B) The timeline view network of co-cited references. (C) The top 20 references with the strongest citation bursts.
TABLE 3.
Top 10 co-cited references.
| Rank | Frequency | Title | Author | Year | Journal |
|---|---|---|---|---|---|
| 1 | 64 | Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) | Robert C. Turner | 1998 | Lancet |
| 2 | 52 | Global Prevalence and Major Risk Factors of Diabetic Retinopathy | Joanne W.Y. Yau | 2012 | Diabetes Care |
| 3 | 38 | Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38 | M. R. Stearne | 1998 | BMJ |
| 4 | 38 | IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045 | N.H. Cho | 2018 | Diabetes Res. Clin. Pr. |
| 5 | 34 | Biochemistry and molecular cell biology of diabetic complications | Michael Brownlee | 2001 | Nature |
| 6 | 31 | Multifactorial Intervention and Cardiovascular Disease in patients with Type 2 Diabetes | Peter Gaede | 2003 | New Engl. J. Med. |
| 7 | 31 | Global aetiology and epidemiology of type 2 diabetes mellitus and its complications | Yan Zheng | 2018 | Nat. Rev. Endocrinol. |
| 8 | 30 | Intensive Blood Glucose Control and Vascular Outcomes in Patients with Type 2 Diabetes | Anushka Patel | 2008 | New Engl. J. Med. |
| 9 | 30 | Effects of Intensive Glucose Lowering in Type 2 Diabetes | H.C. Gerstein | 2008 | New Engl. J. Med. |
| 10 | 29 | Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy | Barry M. Brenner | 2001 | New Engl. J. Med. |
TABLE 4.
Top 10 largest clusters of co-cited references.
| Cluster ID | Size | Silhouette | Mean year | Top terms (LLR) |
|---|---|---|---|---|
| #0 | 185 | 0.809 | 2015 | diabetes complications |
| #1 | 153 | 0.857 | 2007 | fenofibrate |
| #2 | 118 | 0.872 | 2011 | methylenetetrahydrofolate reductase |
| #3 | 109 | 0.89 | 2004 | microalbuminuria |
| #4 | 96 | 0.92 | 1998 | irbesartan |
| #5 | 93 | 0.954 | 1999 | carbonyl stress |
| #6 | 83 | 0.937 | 2017 | exosome |
| #7 | 81 | 0.917 | 2010 | chronic kidney disease |
| #8 | 73 | 0.928 | 2003 | ruboxistaurin |
| #9 | 62 | 0.95 | 2014 | renal biopsy |
FIGURE 6.
The alluvial flow map of co-cited references from 2017 to 2021.
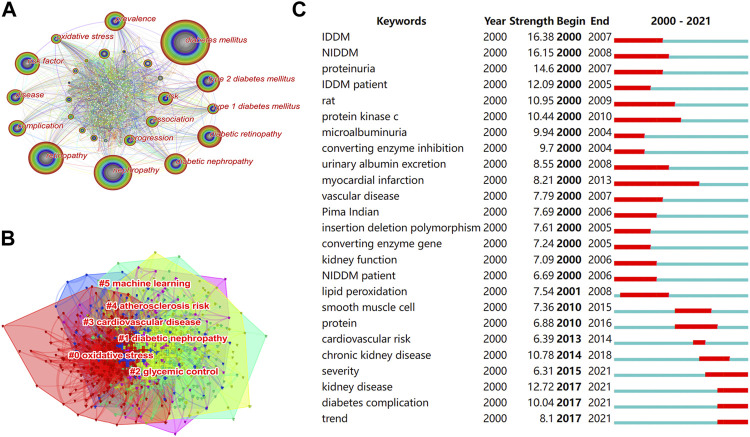
Analysis of Keywords
Research topics with high-frequency keyword performance were considered research hotspots in the field. “Diabetes mellitus,” “nephropathy,” “retinopathy,” “risk factor,” “diabetic retinopathy,” “type 2 diabetes mellitus,” “diabetic nephropathy,” “prevalence,” “disease,” and “complication” were high-frequency keywords (Figure 7A). The top 10 keywords for centrality were “glycation end product,” “diagnosis,” “neuropathy,” “insulin,” “follow up,” “diabetic nephropathy,” “oxidative stress,” insulin resistance,” “glomerular filtration rate,” and “coronary heart disease” (Table 5). Figure 7B shows the cluster analysis of keywords. The S values of the top six largest clusters were all >0.5, indicating that the clustering network was reasonable. The top six largest cluster labels were “oxidative stress,” “diabetic nephropathy,” “glycemic control,” “cardiovascular disease,” “atherosclerosis risk,” and “machine learning” (Table 6). Burst keywords can judge the change of research trends and intuitively show the research hotspots in recent years. Top 25 keywords with the strongest citation bursts are shown in Figure 7C. The term with the highest burst strength was “IDDM”. Moreover, “severity,” “kidney disease,” “diabetes complication,” and “trend” were the most recent keywords that appeared in the last 6 years.
FIGURE 7.
(A) The co-occurrence network of keywords. (B) The clusters of keywords. (C) The top 25 keywords with the strongest citation bursts.
TABLE 5.
Top 10 keywords by frequency and centrality.
| Rank | Count | Keyword | Centrality | Keyword |
|---|---|---|---|---|
| 1 | 1005 | diabetes mellitus | 0.05 | glycation end product |
| 2 | 785 | nephropathy | 0.05 | diagnosis |
| 3 | 727 | retinopathy | 0.05 | neuropathy |
| 4 | 552 | risk factor | 0.05 | insulin |
| 5 | 549 | diabetic retinopathy | 0.05 | follow up |
| 6 | 526 | type 2 diabetes mellitus | 0.04 | diabetic nephropathy |
| 7 | 507 | diabetic nephropathy | 0.04 | oxidative stress |
| 8 | 493 | prevalence | 0.04 | insulin resistance |
| 9 | 413 | disease | 0.04 | glomerular filtration rate |
| 10 | 410 | complication | 0.04 | coronary heart disease |
TABLE 6.
Top 6 largest clusters of keywords.
| Cluster ID | Silhouette | Mean year | Top terms (LLR) |
|---|---|---|---|
| 0 | 0.674 | 2007 | oxidative stress |
| 1 | 0.718 | 2005 | diabetic nephropathy |
| 2 | 0.59 | 2010 | glycemic control |
| 3 | 0.672 | 2009 | cardiovascular disease |
| 4 | 0.748 | 2008 | atherosclerosis risk |
| 5 | 0.98 | 2020 | machine learning |
Discussion
General Information
Publications regarding the association between DN and DR showed an overall upward trend between 2000 and 2021. The United States was the country with the highest number of publications in the field. Two of the top ten institutions in terms of publications were from the United States, namely the University of Wisconsin and Harvard University. The centrality of the United States was the highest, representing the close cooperation between the United States and other countries. The most frequently cited document (citations = 2,798) of the United States was published by Ferdinando Giacco and Michael Brownlee. It mainly described the progress made in understanding oxidative stress and its role in the development of diabetic complications (Giacco and Brownlee, 2010).
The institution with the most publications and greatest centrality ranking was Steno Diabetes Center from Denmark, with 55 publications covering the epidemiology, progression, risk factors, biomarkers, genetics, and other aspects of microvascular complications of diabetes (Rossing et al., 2002; Rossing et al., 2004; Rossing, 2005; Alkhalaf et al., 2010; Alkayyali and Lyssenko, 2014). The most cited of these was a cross-sectional study published by Hans-Henrik Parving evaluating 32,208 patients with type 2 diabetes from 33 countries without known proteinuria. The results of this study showed that retinopathy was an independent risk factor for microalbuminuria. The study also showed a high global prevalence of microalbuminuria and decreased renal function detected in patients with type 2 diabetes without known renal disease, both of which are associated with increased renal and cardiovascular risk (Parving et al., 2006). Additionally, the University of Melbourne from Australia was working on clinical research on the relationship between DN and DR. The institution found that changes in the retinal vascular caliber can predict the risk of DN (Wong et al., 2004; Klein et al., 2007). Thus, assessing the risk of DN by noninvasive testing of retinal microvessels in diabetic patients may be possible. Gilbert et al. found that angiotensin converting enzyme inhibition and angiotensin receptor blockade could reduce the development and progression of diabetic nephropathy, cardiovascular disease, and possibly retinopathy (Gilbert et al., 2003).
The results showed that Tien Y. Wong (University of Melbourne, National University of Singapore) had the most publications. His main focus was on the correlation of retinal blood vessels with chronic kidney disease, demonstrating that retinal microangiopathy is associated with the development of DN in diabetic patients (Klein et al., 2007; Broe et al., 2014; Yip et al., 2015; Nusinovici et al., 2021). Moreover, Diabetes Care was the most co-cited journal. One of the most cited publications in Diabetes Care addressed the role of oxidative stress in the development of diabetic complications (Giacco and Brownlee, 2010). The latest research of this journal has focused on sodium-glucose cotransporter 2 (SGLT2) inhibitors and DN. SGLT2 inhibitors are nephroprotective and play a role in the primary prevention of DN (Mosenzon et al., 2021; Nagasu et al., 2021). Matthews et al. found that SGLT2 inhibition may be a useful therapeutic approach to prevent the development of DR and lessen its severity if administered early in the disease process (Matthews et al., 2022).
Hotspots and Frontiers
Cluster analysis of co-cited reference and keyword showed that the pathogenesis of DN and DR and their relationship with CVD were research hotspots. The largest cluster for co-cited reference was labeled as “diabetes complications.” The most relevant citer in the cluster was Winston Crasto. He has discussed the microvascular complications of diabetes, including DN, DR, and diabetic neuropathy, and provides best practice clinical care recommendations to guide health care professionals to better manage people with these conditions (Crasto et al., 2021). Additionally, cluster #2 was labeled as “methylenetetrahydrofolate reductase (MTHFR)”. The results of a study on the association of MTHFR polymorphisms with DR and DN in Japanese patients with type 2 diabetes suggest an important role of the MTHFR genotype in susceptibility to retinopathy under hyperglycemia, but not to nephropathy (Maeda et al., 2008). However, a meta-analysis of the MTHFR gene 677C/T polymorphism with DN and DR demonstrated that this genotype might confer a moderately augmented risk for DN and DR (Niu and Qi, 2012). The largest cluster of a keyword (#0) was that of “oxidative stress.” Oxidative stress, a cytopathic outcome of excessive generation of reactive oxygen species (ROS) and the repression of antioxidant defense system for ROS elimination, is involved in the pathogenesis of DN and DR (Jha et al., 2016; Kang and Yang, 2020). Cluster #2 was “glycemic control,” which is a significant risk factor for the development of diabetic complications (Nordwall et al., 2009). Hyperglycemia is an important indicator of risk for both DN with albuminuria or DR and less specific forms of CKD (Bash et al., 2008). Therefore, strict glycemic control can prevent diabetic microvascular complications, including DN and DR (Vasudevan et al., 2006). Cluster #3 was “cardiovascular disease”. A cross-sectional study showed that patients with type 1 diabetes and CKD without proliferative DR had a reduced prevalence of CVD (Gordin et al., 2018). Among people with diabetes, those with DN and DR had a higher risk of death from CVD (Sabanayagam et al., 2019). Continuing, cluster #4 was “atherosclerosis risk.” Atherosclerosis is the leading cause of heart disease and stroke (Lusis, 2000). Risk factors for atherosclerosis include hypertension, smoking, and diabetes mellitus (Libby et al., 2019). In patients with type 1 diabetes, atherosclerosis is associated with DR, and patients with DN have a greater coronary plaque burden than those with normoalbuminuria (Kim et al., 2007; Lovshin et al., 2018). Next, cluster #5 was “machine learning.” It has been found that artificial intelligence (AI)-based machine learning can predict microvascular complications in diabetic patients (Sambyal et al., 2021; Rashid et al., 2022).
A growing number of studies have demonstrated a correlation between DN and DR. Moriya et al. found that patients with type 2 diabetes with DR and concomitant microalbuminuria showed typical diabetic glomerulosclerosis and progressive renal dysfunction (Moriya et al., 2016). Previous studies have shown that in patients with type 2 diabetes, regardless of DR, microalbuminuria can cause early retinal microvascular changes (Cankurtaran et al., 2020; Ucgul et al., 2021). Thus, we may be able to identify early DN by detecting retinal microcirculation. Ansquer et al. has shown that fenofibrate offers an opportunity to prevent DN and DR (Ansquer et al., 2009). Furthermore, irbesartan is an angiotensin II receptor blocker that has become an important drug for the treatment of hypertension, heart failure, and prevention of DN (Michel et al., 2013). It has a protective effect on the kidneys in patients with type 2 diabetes and microalbuminuria (Parving et al., 2001). One study showed that angiotensin II receptor blockers play a potential role in the prevention and treatment of DR (Behl and Kotwani, 2017).
The top 10 co-cited references were related to the epidemiology of diabetes complications, drug interventions, molecular mechanisms, and CVD risk. The most frequently co-cited reference was a randomized controlled trial published by Robert C. Turner. The study suggested that intensive blood-glucose control by either sulphonylureas or insulin could substantially decrease the risk of microvascular complications in patients with type 2 diabetes (UK Prospective Diabetes Study Group, 1998a). The first milestone papers in this field of research were published in 1998. One reported that intensive blood-glucose control by either sulphonylureas or insulin substantially decreased the risk of microvascular complications (UK Prospective Diabetes Study Group, 1998a). This study is also the most frequently cited and has the most co-citations and highest burst strength. The other study reported that tight blood pressure control in diabetic patients delayed the progression of DR and renal failure (UK Prospective Diabetes Study Group, 1998b). Furthermore, the alluvial flow map showed two references that had been cited for five consecutive years from 2017 to 2021. Marso et al. found that liraglutide reduced the rate of first occurrence of death from cardiovascular causes, nonfatal myocardial infarction, or nonfatal stroke in patients with type 2 diabetes mellitus (Marso et al., 2016). Liraglutide appears to be effective in reducing proteinuria and improving renal function (Liu et al., 2019). In addition, liraglutide also has a certain protective effect on diabetic retinal injury (Wu et al., 2019). The team of Rodríguez-Poncelas showed that CKD, high UACR and low eGFR, appear to be associated with DR in patients with type 2 diabetes mellitus in Catalonia (Spain) (Rodriguez-Poncelas et al., 2016).
According to the analysis of burst keywords, research hotspots included the physiopathology, genetics, and biomarkers of DN and DR. We speculate that the study of the correlation between the severity of DN and DR will become a new trend. DN and DR have a similar pathogenesis, including oxidative stress (Jha et al., 2016; Kang and Yang, 2020), massive accumulation of glycation end products (Zong et al., 2011; Nishad et al., 2021), polyol pathway activation (Lewko et al., 2011), protein kinase C (Kamiya et al., 2003), and genetic factors (Alkayyali and Lyssenko, 2014). DN and DR share common clinical risk factors, including age, smoking, hypertension, obesity, and hyperlipidemia (Wong et al., 2014). Moreover, a study on the relationship between DN and DR in the Chinese population found that 48.8% of patients with type 2 diabetes mellitus diagnosed with DN by renal biopsy were accompanied by DR (Cao et al., 2019). Additionally, DR can be used to predict the risk and prognosis of DN (Zhang et al., 2018; Li Y. et al., 2021). It has also been found that DN is an independent risk factor for the development and progression of DR (Butt et al., 2020). Finally, the severity of DR is a risk factor for progression to CKD in patients with type 2 diabetes (Hsing et al., 2020).
Limitations
This study is the first to visualize the correlation between DN and DR using a bibliometric approach; however, it still has some limitations. First, only the WOS core database was included in this study, and other databases, such as PubMed, Google Scholar, and Scope were not included. The primary data source for CiteSpace software is WOS (Synnestvedt et al., 2005). To meet the format requirements of the software, the WOS database is the primary choice. Other databases are not common in the practice of this software. Currently the software cannot automatically remove duplicates from different databases and analyze them simultaneously. Second, this study combined synonyms in the analysis, and the result bias due to subjectivity cannot be ruled out.
Conclusion
This study systematically assessed the relationship between DN and DR based on a bibliometric analysis. The number of publications is annually increasing, and although a slight decline was observed in 2021, it is enough to show that this research field has continuously stimulated the interest of many scholars. Publications from different countries, institutions, authors, and journals were evaluated, showing their contributions to the field, which may also be used to guide future research. Through the analysis of references and keywords, we have predicted the future research hotspots and trends of DN and DR. For example, the pathogenesis of DN and DR and their relationship with CVD are current research hotspots. Moreover, the clinical relevance and drug therapy of DN and DR will be the frontiers of future research in this field. This study analyzes the status and trends of the relationship between DN and DR, which may promote the development of this research field. The study can provide scholars interested in this field with a reference of research trends and reduce their time to search for research hotspots and frontiers.
Acknowledgments
Thanks to associate professor Weiwen Shao and Bo Zhang from Library of Chinese Academy of Sciences for their professional suggestions on the study. The authors would like to thank Editage (www.editage.com) for English language editing.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author Contributions
WL, ZD, and XC designed the study. YL and FL collected the data. WL, HL, and QW analyzed the data. WL, ZD, and XC wrote and revised the manuscript. All authors contributed to the article and approved the published version of the manuscript.
Funding
This study was supported by the Natural Science Foundation of China (No.32141005) and Science and Technology Project of Beijing, China (D17110700280000 and D171100002817002).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- Alkayyali S., Lyssenko V. (2014). Genetics of Diabetes Complications. Mamm. Genome. 25 (9-10), 384–400. 10.1007/s00335-014-9543-x [DOI] [PubMed] [Google Scholar]
- Alkhalaf A., Zürbig P., Bakker S. J., Bilo H. J., Cerna M., Fischer C., et al. (2010). Multicentric Validation of Proteomic Biomarkers in Urine Specific for Diabetic Nephropathy. PLoS One 5 (10), e13421. 10.1371/journal.pone.0013421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ansquer J. C., Foucher C., Aubonnet P., Le Malicot K. (2009). Fibrates and Microvascular Complications in Diabetes-Iinsight from the FIELD Study. Curr. Pharm. Des. 15 (5), 537–552. 10.2174/138161209787315701 [DOI] [PubMed] [Google Scholar]
- Bash L. D., Selvin E., Steffes M., Coresh J., Astor B. C. (2008). Poor Glycemic Control in Diabetes and the Risk of Incident Chronic Kidney Disease Even in the Absence of Albuminuria and Retinopathy: Atherosclerosis Risk in Communities (ARIC) Study. Arch. Intern Med. 168 (22), 2440–2447. 10.1001/archinte.168.22.2440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behl T., Kotwani A. (2017). Potential of Angiotensin II Receptor Blockers in the Treatment of Diabetic Retinopathy. Life Sci. 176, 1–9. 10.1016/j.lfs.2017.03.020 [DOI] [PubMed] [Google Scholar]
- Broe R., Rasmussen M. L., Frydkjaer-Olsen U., Olsen B. S., Mortensen H. B., Hodgson L., et al. (2014). Retinal Vessel Calibers Predict Long-Term Microvascular Complications in Type 1 Diabetes: the Danish Cohort of Pediatric Diabetes 1987 (DCPD1987). Diabetes 63 (11), 3906–3914. 10.2337/db14-0227 [DOI] [PubMed] [Google Scholar]
- Butt A., Mustafa N., Fawwad A., Askari S., Haque M. S., Tahir B., et al. (2020). Relationship between Diabetic Retinopathy and Diabetic Nephropathy; A Longitudinal Follow-Up Study from a Tertiary Care Unit of Karachi, Pakistan. Diabetes Metab. Syndr. 14 (6), 1659–1663. 10.1016/j.dsx.2020.08.026 [DOI] [PubMed] [Google Scholar]
- Cankurtaran V., Inanc M., Tekin K., Turgut F. (2020). Retinal Microcirculation in Predicting Diabetic Nephropathy in Type 2 Diabetic Patients without Retinopathy. Ophthalmologica 243 (4), 271–279. 10.1159/000504943 [DOI] [PubMed] [Google Scholar]
- Cao X., Gong X., Ma X. (2019). Diabetic Nephropathy versus Diabetic Retinopathy in a Chinese Population: A Retrospective Study. Med. Sci. Monit. 25, 6446–6453. 10.12659/MSM.915917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C., Chen Y. (2005). Searching for Clinical Evidence in CiteSpace. AMIA Annu. Symp. Proc. 2005, 121. [PMC free article] [PubMed] [Google Scholar]
- Chen C., Hu Z., Liu S., Tseng H. (2012). Emerging Trends in Regenerative Medicine: a Scientometric Analysis in CiteSpace. Expert Opin. Biol. Ther. 12 (5), 593–608. 10.1517/14712598.2012.674507 [DOI] [PubMed] [Google Scholar]
- Cheung C. Y., Ikram M. K., Sabanayagam C., Wong T. Y. (2012). Retinal Microvasculature as a Model to Study the Manifestations of Hypertension. Hypertension 60 (5), 1094–1103. 10.1161/HYPERTENSIONAHA.111.189142 [DOI] [PubMed] [Google Scholar]
- Cheung N., Mitchell P., Wong T. Y. (2010). Diabetic Retinopathy. Lancet 376 (9735), 124–136. 10.1016/S0140-6736(09)62124-3 [DOI] [PubMed] [Google Scholar]
- Congdon N. G., Friedman D. S., Lietman T. (2003). Important Causes of Visual Impairment in the World Today. JAMA 290 (15), 2057–2060. 10.1001/jama.290.15.2057 [DOI] [PubMed] [Google Scholar]
- Crasto W., Patel V., Davies M. J., Khunti K. (2021). Prevention of Microvascular Complications of Diabetes. Endocrinol. Metab. Clin. North Am. 50 (3), 431–455. 10.1016/j.ecl.2021.05.005 [DOI] [PubMed] [Google Scholar]
- Ellegaard O., Wallin J. A. (2015). The Bibliometric Analysis of Scholarly Production: How Great Is the Impact? Scientometrics 105 (3), 1809–1831. 10.1007/s11192-015-1645-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giacco F., Brownlee M. (2010). Oxidative Stress and Diabetic Complications. Circ. Res. 107 (9), 1058–1070. 10.1161/CIRCRESAHA.110.223545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert R. E., Krum H., Wilkinson-Berka J., Kelly D. J. (2003). The Renin-Angiotensin System and the Long-Term Complications of Diabetes: Pathophysiological and Therapeutic Considerations. Diabet. Med. 20 (8), 607–621. 10.1046/j.1464-5491.2003.00979.x [DOI] [PubMed] [Google Scholar]
- Gordin D., Harjutsalo V., Tinsley L., Fickweiler W., Sun J. K., Forsblom C., et al. (2018). Differential Association of Microvascular Attributions with Cardiovascular Disease in Patients with Long Duration of Type 1 Diabetes. Diabetes Care 41 (4), 815–822. 10.2337/dc17-2250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh Y. T., Hsieh M. C. (2021). Time-sequential Correlations between Diabetic Kidney Disease and Diabetic Retinopathy in Type 2 Diabetes - an 8-year Prospective Cohort Study. Acta Ophthalmol. 99 (1), e1. 10.1111/aos.14487 [DOI] [PubMed] [Google Scholar]
- Hsing S. C., Lee C. C., Lin C., Chen J. T., Chen Y. H., Fang W. H. (2020). The Severity of Diabetic Retinopathy Is an Independent Factor for the Progression of Diabetic Nephropathy. J. Clin. Med. 10 (1), 3. 10.3390/jcm10010003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jawa A., Kcomt J., Fonseca V. A. (2004). Diabetic Nephropathy and Retinopathy. Med. Clin. North Am. 88 (4), 1001. 10.1016/j.mcna.2004.04.012 [DOI] [PubMed] [Google Scholar]
- Jha J. C., Banal C., Chow B. S., Cooper M. E., Jandeleit-Dahm K. (2016). Diabetes and Kidney Disease: Role of Oxidative Stress. Antioxid. Redox Signal 25 (12), 657–684. 10.1089/ars.2016.6664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamiya H., Nakamura J., Hamada Y., Nakashima E., Naruse K., Kato K., et al. (2003). Polyol Pathway and Protein Kinase C Activity of Rat Schwannoma Cells. Diabetes Metab. Res. Rev. 19 (2), 131–139. 10.1002/dmrr.354 [DOI] [PubMed] [Google Scholar]
- Kang Q., Yang C. (2020). Oxidative Stress and Diabetic Retinopathy: Molecular Mechanisms, Pathogenetic Role and Therapeutic Implications. Redox Biol. 37, 101799. 10.1016/j.redox.2020.101799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim W. Y., Astrup A. S., Stuber M., Tarnow L., Falk E., Botnar R. M., et al. (2007). Subclinical Coronary and Aortic Atherosclerosis Detected by Magnetic Resonance Imaging in Type 1 Diabetes with and without Diabetic Nephropathy. Circulation 115 (2), 228–235. 10.1161/CIRCULATIONAHA.106.633339 [DOI] [PubMed] [Google Scholar]
- Klein R., Klein B. E., Moss S. E., Wong T. Y. (2007). Retinal Vessel Caliber and Microvascular and Macrovascular Disease in Type 2 Diabetes: XXI: the Wisconsin Epidemiologic Study of Diabetic Retinopathy. Ophthalmology 114 (10), 1884–1892. 10.1016/j.ophtha.2007.02.023 [DOI] [PubMed] [Google Scholar]
- Kumar R., Goel P. (2021). Exploring the Domain of Interpretive Structural Modelling (ISM) for Sustainable Future Panorama: A Bibliometric and Content Analysis. Arch. Comput. Methods Eng.. 10.1007/s11831-021-09675-7 [DOI] [Google Scholar]
- Kumar R., Singh S., Sidhu A. S., Pruncu C. I. (2021). Bibliometric Analysis of Specific Energy Consumption (SEC) in Machining Operations: A Sustainable Response. Sustainability 13 (10), 5617. 10.3390/su13105617 [DOI] [Google Scholar]
- Lewko B., Latawiec E., Maryn A., Barczyńska A., Pikuła M., Zieliński M., et al. (2011). Osmolarity and Glucose Differentially Regulate Aldose Reductase Activity in Cultured Mouse Podocytes. Exp. Diabetes Res. 2011, 278963. 10.1155/2011/278963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X. J., Li C. Y., Bai D., Leng Y. (2021). Insights into Stem Cell Therapy for Diabetic Retinopathy: a Bibliometric and Visual Analysis. Neural Regen. Res. 16 (1), 172–178. 10.4103/1673-5374.286974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Su X., Ye Q., Guo X., Xu B., Guan T., et al. (2021). The Predictive Value of Diabetic Retinopathy on Subsequent Diabetic Nephropathy in Patients with Type 2 Diabetes: a Systematic Review and Meta-Analysis of Prospective Studies. Ren. Fail 43 (1), 231–240. 10.1080/0886022X.2020.1866010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Libby P., Buring J. E., Badimon L., Hansson G. K., Deanfield J., Bittencourt M. S., et al. (2019). Atherosclerosis. Nat. Rev. Dis. Prim. 5 (1), 56. 10.1038/s41572-019-0106-z [DOI] [PubMed] [Google Scholar]
- Liu T., Yang L., Mao H., Ma F., Wang Y., Zhan Y. (2021). Knowledge Domain and Emerging Trends in Podocyte Injury Research from 1994 to 2021: A Bibliometric and Visualized Analysis. Front. Pharmacol. 12, 772386. 10.3389/fphar.2021.772386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W., Yu J., Tian T., Miao J., Shang W. (2019). Meta-analysis of the Efficacy of Liraglutide in Patients with Type 2 Diabetes Accompanied by Incipient Nephropathy. Exp. Ther. Med. 18 (1), 342–351. 10.3892/etm.2019.7577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovshin J. A., Bjornstad P., Lovblom L. E., Bai J. W., Lytvyn Y., Boulet G., et al. (2018). Atherosclerosis and Microvascular Complications: Results from the Canadian Study of Longevity in Type 1 Diabetes. Diabetes Care 41 (12), 2570–2578. 10.2337/dc18-1236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lusis A. J. (2000). Atherosclerosis. Nature 407 (6801), 233–241. 10.1038/35025203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marso S. P., Daniels G. H., Brown-Frandsen K., Kristensen P., Mann J. F., Nauck M. A., et al. (2016). Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. N. Engl. J. Med. 375 (4), 311–322. 10.1056/NEJMoa1603827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews J., Herat L., Rooney J., Rakoczy E., Schlaich M., Matthews V. B. (2022). Determining the Role of SGLT2 Inhibition with Empagliflozin in the Development of Diabetic Retinopathy. Biosci. Rep. 42 (3), BSR20212209. 10.1042/BSR20212209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michel M. C., Foster C., Brunner H. R., Liu L. (2013). A Systematic Comparison of the Properties of Clinically Used Angiotensin II Type 1 Receptor Antagonists. Pharmacol. Rev. 65 (2), 809–848. 10.1124/pr.112.007278 [DOI] [PubMed] [Google Scholar]
- Moriya T., Matsubara M., Kishihara E., Yoshida Y., Ouchi M. (2016). Type 2 Diabetic Patients with Diabetic Retinopathy and Concomitant Microalbuminuria Showed Typical Diabetic Glomerulosclerosis and Progressive Renal Dysfunction. J. Diabetes Complicat. 30 (6), 1111–1116. 10.1016/j.jdiacomp.2016.04.007 [DOI] [PubMed] [Google Scholar]
- Mosenzon O., Wiviott S. D., Heerspink H. J. L., Dwyer J. P., Cahn A., Goodrich E. L., et al. (2021). The Effect of Dapagliflozin on Albuminuria in DECLARE-TIMI 58. Diabetes Care 44 (8), 1805–1815. 10.2337/dc21-0076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagasu H., Yano Y., Kanegae H., Heerspink H. J. L., Nangaku M., Hirakawa Y., et al. (2021). Kidney Outcomes Associated with SGLT2 Inhibitors versus Other Glucose-Lowering Drugs in Real-World Clinical Practice: The Japan Chronic Kidney Disease Database. Diabetes Care 44 (11), 2542–2551. 10.2337/dc21-1081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishad R., Tahaseen V., Kavvuri R., Motrapu M., Singh A. K., Peddi K., et al. (2021). Advanced-Glycation End-Products Induce Podocyte Injury and Contribute to Proteinuria. Front. Med. 8, 685447. 10.3389/fmed.2021.685447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordwall M., Arnqvist H. J., Bojestig M., Ludvigsson J. (2009). Good Glycemic Control Remains Crucial in Prevention of Late Diabetic Complications-Tthe Linköping Diabetes Complications Study. Pediatr. Diabetes. 10 (3), 168–176. 10.1111/j.1399-5448.2008.00472.x [DOI] [PubMed] [Google Scholar]
- Nusinovici S., Sabanayagam C., Lee K. E., Zhang L., Cheung C. Y., Tai E. S., et al. (2021). Retinal Microvascular Signs and Risk of Diabetic Kidney Disease in Asian and White Populations. Sci. Rep. 11 (1), 4898. 10.1038/s41598-021-84464-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan W. W., Gardner T. W., Harder J. L. (2021). Integrative Biology of Diabetic Retinal Disease: Lessons from Diabetic Kidney Disease. J. Clin. Med. 10 (6), 1254. 10.3390/jcm10061254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parving H. H., Lehnert H., Bröchner-Mortensen J., Gomis R., Andersen S., Arner P. (2001). The Effect of Irbesartan on the Development of Diabetic Nephropathy in Patients with Type 2 Diabetes. N. Engl. J. Med. 345 (12), 870–878. 10.1056/NEJMoa011489 [DOI] [PubMed] [Google Scholar]
- Parving H. H., Lewis J. B., Ravid M., Remuzzi G., Hunsicker L. G. (2006). Prevalence and Risk Factors for Microalbuminuria in a Referred Cohort of Type II Diabetic Patients: a Global Perspective. Kidney Int. 69 (11), 2057–2063. 10.1038/sj.ki.5000377 [DOI] [PubMed] [Google Scholar]
- Patton N., Aslam T. M., Macgillivray T., Deary I. J., Dhillon B., Eikelboom R. H., et al. (2006). Retinal Image Analysis: Concepts, Applications and Potential. Prog. Retin. Eye Res. 25 (1), 99–127. 10.1016/j.preteyeres.2005.07.001 [DOI] [PubMed] [Google Scholar]
- Rangel É. B., Rodrigues C. O., de Sá J. R. (2019). Micro- and Macrovascular Complications in Diabetes Mellitus: Preclinical and Clinical Studies. J. Diabetes Res. 2019, 2161085. 10.1155/2019/2161085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rashid M., Alkhodari M., Mukit A., Ahmed K. I. U., Mostafa R., Parveen S., et al. (2022). Machine Learning for Screening Microvascular Complications in Type 2 Diabetic Patients Using Demographic, Clinical, and Laboratory Profiles. J. Clin. Med. 11 (4), 903. 10.3390/jcm11040903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Poncelas A., Mundet-Tudurí X., Miravet-Jiménez S., Casellas A., Barrot-De la Puente J. F., Franch-Nadal J., et al. (2016). Chronic Kidney Disease and Diabetic Retinopathy in Patients with Type 2 Diabetes. PLoS One 11 (2), e0149448. 10.1371/journal.pone.0149448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossing K., Christensen P. K., Hovind P., Tarnow L., Rossing P., Parving H. H. (2004). Progression of Nephropathy in Type 2 Diabetic Patients. Kidney Int. 66 (4), 1596–1605. 10.1111/j.1523-1755.2004.00925.x [DOI] [PubMed] [Google Scholar]
- Rossing P., Hougaard P., Parving H. H. (2002). Risk Factors for Development of Incipient and Overt Diabetic Nephropathy in Type 1 Diabetic Patients: a 10-year Prospective Observational Study. Diabetes Care 25 (5), 859–864. 10.2337/diacare.25.5.859 [DOI] [PubMed] [Google Scholar]
- Rossing P. (2005). The Changing Epidemiology of Diabetic Microangiopathy in Type 1 Diabetes. Diabetologia 48 (8), 1439–1444. 10.1007/s00125-005-1836-x [DOI] [PubMed] [Google Scholar]
- Sabanayagam C., Chee M. L., Banu R., Cheng C. Y., Lim S. C., Tai E. S., et al. (2019). Association of Diabetic Retinopathy and Diabetic Kidney Disease with All-Cause and Cardiovascular Mortality in a Multiethnic Asian Population. JAMA Netw. Open 2 (3), e191540. 10.1001/jamanetworkopen.2019.1540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sambyal N., Saini P., Syal R. (2021). A Review of Statistical and Machine Learning Techniques for Microvascular Complications in Type 2 Diabetes. Curr. Diabetes Rev. 17 (2), 143–155. 10.2174/1573399816666200511003357 [DOI] [PubMed] [Google Scholar]
- Srivastav K., Saxena S., Mahdi A. A., Kruzliak P., Khanna V. K. (2015). Increased Serum Urea and Creatinine Levels Correlate with Decreased Retinal Nerve Fibre Layer Thickness in Diabetic Retinopathy. Biomarkers 20 (6-7), 470–473. 10.3109/1354750X.2015.1094142 [DOI] [PubMed] [Google Scholar]
- Sun H., Saeedi P., Karuranga S., Pinkepank M., Ogurtsova K., Duncan B. B., et al. (2022). IDF Diabetes Atlas: Global, Regional and Country-Level Diabetes Prevalence Estimates for 2021 and Projections for 2045. Diabetes Res. Clin. Pract. 183, 109119. 10.1016/j.diabres.2021.109119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Synnestvedt M. B., Chen C., Holmes J. H. (2005). CiteSpace II: Visualization and Knowledge Discovery in Bibliographic Databases. AMIA Annu. Symp. Proc. 2005, 724. [PMC free article] [PubMed] [Google Scholar]
- Thompson D. F., Walker C. K. (2015). A Descriptive and Historical Review of Bibliometrics with Applications to Medical Sciences. Pharmacotherapy 35 (6), 551–559. 10.1002/phar.1586 [DOI] [PubMed] [Google Scholar]
- Tong X., Yu Q., Ankawi G., Pang B., Yang B., Yang H. (2020). Insights into the Role of Renal Biopsy in Patients with T2DM: A Literature Review of Global Renal Biopsy Results. Diabetes Ther. 11 (9), 1983–1999. 10.1007/s13300-020-00888-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsilibary E. C. (2003). Microvascular Basement Membranes in Diabetes Mellitus. J. Pathol. 200 (4), 537–546. 10.1002/path.1439 [DOI] [PubMed] [Google Scholar]
- Tuttle K. R., Bakris G. L., Bilous R. W., Chiang J. L., de Boer I. H., Goldstein-Fuchs J., et al. (2014). Diabetic Kidney Disease: a Report from an ADA Consensus Conference. Diabetes Care 37 (10), 2864–2883. 10.2337/dc14-1296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ucgul Atilgan C., Atilgan K. G., Kosekahya P., Goker Y. S., Karatepe M. S., Caglayan M., et al. (2021). Retinal Microcirculation Alterations in Microalbuminuric Diabetic Patients with and without Retinopathy. Semin. Ophthalmol. 36 (5-6), 406–412. 10.1080/08820538.2021.1896745 [DOI] [PubMed] [Google Scholar]
- UK Prospective Diabetes Study (UKPDS) Group (1998a). Intensive Blood-Glucose Control with Sulphonylureas or Insulin Compared with Conventional Treatment and Risk of Complications in Patients with Type 2 Diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet 352 (9131), 837–853. [PubMed] [Google Scholar]
- UK Prospective Diabetes Study (UKPDS) Group (1998b). Tight Blood Pressure Control and Risk of Macrovascular and Microvascular Complications in Type 2 Diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ 317 (7160), 703–713. 10.1136/bmj.317.7160.703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasudevan A. R., Burns A., Fonseca V. A. (2006). The Effectiveness of Intensive Glycemic Control for the Prevention of Vascular Complications in Diabetes Mellitus. Treat. Endocrinol. 5 (5), 273–286. 10.2165/00024677-200605050-00002 [DOI] [PubMed] [Google Scholar]
- Wong C. W., Wong T. Y., Cheng C. Y., Sabanayagam C. (2014). Kidney and Eye Diseases: Common Risk Factors, Etiological Mechanisms, and Pathways. Kidney Int. 85 (6), 1290–1302. 10.1038/ki.2013.491 [DOI] [PubMed] [Google Scholar]
- Wong T. Y., Shankar A., Klein R., Klein B. E. (2004). Retinal Vessel Diameters and the Incidence of Gross Proteinuria and Renal Insufficiency in People with Type 1 Diabetes. Diabetes 53 (1), 179–184. 10.2337/diabetes.53.1.179 [DOI] [PubMed] [Google Scholar]
- Wu L., Gao L., Cao Y., Chen F., Sun T., Liu Y. (2019). Analysis of the Protective Mechanism of Liraglutide on Retinopathy Based on Diabetic Mouse Model. Saudi J. Biol. Sci. 26 (8), 2096–2101. 10.1016/j.sjbs.2019.09.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yau J. W., Rogers S. L., Kawasaki R., Lamoureux E. L., Kowalski J. W., Bek T., et al. (2012). Global Prevalence and Major Risk Factors of Diabetic Retinopathy. Diabetes Care 35 (3), 556–564. 10.2337/dc11-1909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yip W., Sabanayagam C., Teo B. W., Tay W. T., Ikram M. K., Tai E. S., et al. (2015). Retinal Microvascular Abnormalities and Risk of Renal Failure in Asian Populations. PLoS One 10 (2), e0118076. 10.1371/journal.pone.0118076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yun K. J., Kim H. J., Kim M. K., Kwon H. S., Baek K. H., Roh Y. J., et al. (2016). Risk Factors for the Development and Progression of Diabetic Kidney Disease in Patients with Type 2 Diabetes Mellitus and Advanced Diabetic Retinopathy. Diabetes Metab. J. 40 (6), 473–481. 10.4093/dmj.2016.40.6.473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Wang Y., Li L., Zhang R., Guo R., Li H., et al. (2018). Diabetic Retinopathy May Predict the Renal Outcomes of Patients with Diabetic Nephropathy. Ren. Fail 40 (1), 243–251. 10.1080/0886022X.2018.1456453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhuang X., Cao D., Yang D., Zeng Y., Yu H., Wang J., et al. (2019). Association of Diabetic Retinopathy and Diabetic Macular Oedema with Renal Function in Southern Chinese Patients with Type 2 Diabetes Mellitus: a Single-Centre Observational Study. BMJ Open 9 (9), e031194. 10.1136/bmjopen-2019-031194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zong H., Ward M., Stitt A. W. (2011). AGEs, RAGE, and Diabetic Retinopathy. Curr. Diab Rep. 11 (4), 244–252. 10.1007/s11892-011-0198-7 [DOI] [PubMed] [Google Scholar]
- Zou L. X., Sun L. (2019). Global Diabetic Kidney Disease Research from 2000 to 2017: A Bibliometric Analysis. Med. Baltim. 98 (6), e14394. 10.1097/MD.0000000000014394 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.