Abstract
Objectives
Tai chi (TC) is a potential complementary treatment for type 2 diabetes mellitus (T2DM). This overview systematically summarizes and evaluates the existing evidence of TC in the treatment of T2DM.
Methods
Systematic reviews (SRs)/meta-analyses (MAs) on TC interventions for T2DM were comprehensively searched in seven databases. Methodological quality, risk of bias, reporting quality, and quality of evidence were assessed using the Assessment of Multiple Systematic Reviews 2 (AMSTAR-2), the Risk of Bias in Systematic (ROBIS) scale, the list of Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA), and the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system.
Results
Eight published SRs/MAs were included in our study. Based on the methodology and quality of evidence assessment, all SRs/MAs are considered to be of very low quality, and only 1 SR/MA has been assessed as low risk of bias, and none of the SR/MA has been fully reported on the checklist. A total of 65 outcome indicators extracted from the included SRs/MAs were evaluated, and only 1 item was assessed as high quality.
Conclusions
TC may be an effective and safe complementary treatment for T2DM. However, this conclusion must be treated with caution because the quality of the evidence provided by the included SRs/MAs is generally low.
1. Introduction
As a chronic metabolic disease, type 2 diabetes mellitus (T2DM) is characterized by elevated blood glucose levels, which induces disturbances in glucose, fat, and protein metabolism in the body [1]. The pathophysiological hallmark of T2DM is insulin resistance, accompanied by decreased insulin secretion due to pancreatic β cell dysfunction, and oxidative stress (OS) is also considered to be a major hallmark of the pathogenesis and progression of T2DM [2]. T2DM accounts for 90% of all diabetes cases, and the International Diabetes Federation (IDF) estimates that the number of people with type 2 diabetes worldwide is expected to reach 578 million by 2030 and 700 million by 2045 [3]. T2DM is generally associated with a higher risk of vascular complications, including macrovascular complications (e.g., cardiovascular complications) and microvascular complications (including neuropathy, nephropathy, and retinopathy) [4]. The current mainstream treatments for T2DM include oral hypoglycemic drugs and subcutaneous insulin injections. In addition, body movement constitutes a significant part of a diabetes management program and plays a specific role in preventing diabetes complications and managing blood sugar in patients with T2DM [5].
OS occurs when the accumulation of the by-products of oxygen metabolism eventually exceeds the antioxidant capacity [6]. Experimental and clinical studies have shown that OS is involved in the pathogenesis of cardiovascular disease, carcinogenesis, and other diseases. It is known to play a key role in the etiology and pathophysiology of diabetes [7]. Mitochondrial dysfunction and dysregulation of prooxidase appear to be major factors involved in chronic reactive oxygen species (ROS) generation, resulting in a chronic OS state [2]. Chronic hyperglycemia is considered to be a major contributor to the development of microvascular and macrovascular complications in type 2 diabetes and is known to cause DNA, lipid, and protein damage, the extent of which is related to the hyperglycemia-induced reactive oxygen species production and the degree of OS [8]. Physical exercise intervention induces an adaptive response characterized by a reduction in markers of OS damage and an increase in the body's antioxidant response [9].
Originated in ancient China, TC has a history of thousands of years. It was formed under the guidance of traditional Chinese medicine theories and Chinese folk martial arts, and it is a gem of the Chinese nation [10]. The pathogenesis of T2DM is closely related to the physical and mental state of the individual. TC is a movement that emphasizes the unity of energy, breath, and spirit and combines physical activity with breathing [11]. A meta-analysis showed that regular TC exercise increased superoxide dismutase and catalase levels while decreasing lipid peroxide levels [12]. Therefore, TC plays an active role in glycemic control and OS regulation in T2DM patients, and the ADA recommends TC as a mind-body therapy for T2DM patients to increase balance, muscle strength, and flexibility [13].
Systematic review (SR)/meta-analysis (MA) is an important tool for evidence-based clinical work, but its methods must strictly follow a series of guidelines to minimize the possibility of deviation in answering specific questions [14]. A growing number of SRs/MAs based on TC interventions for T2DM have shown that TC can reduce fasting glucose (FGB) and glycated hemoglobin (HbA1c) and improve the quality of life in patients with T2DM. However, the methodological and evidentiary quality of these SRs/MAs has not been assessed, and it remains controversial whether these findings could provide credible evidentiary support for clinical staff [15]. The SR/MA overview is a newly emerged approach that combines multiple SRs/MAs to assess their quality and various findings in an attempt to resolve inconsistencies between them [16]. The purpose of this overview is to objectively and comprehensively evaluate the scientific validity and applicability of SRs/MAs regarding the effects of TC exercise on T2DM.
2. Methods
2.1. Research Methods
The SR/MA overview is based on the guidelines specified in the Cochrane Handbook [17], and we followed the methods of Shi et al. [18], Liu et al. [19], and Shen et al. [20].
2.2. Eligibility Criteria
2.2.1. Literature Inclusion Criteria
(1) Type of Research. This overview includes SRs/MAs of randomized controlled trials (RCTs) of the effects of TC exercise on T2DM.
(2) Type of Participants. Subjects were patients diagnosed with T2DM by any international or national standard.
(3) Type of Intervention. The intervention for the control group was usual care or standard treatment (ST) or any type of other exercises, and the intervention for the experimental group was TC exercise or TC combined with the treatments received by the control group.
(4) Types of Outcomes. Outcomes assessed in this overview include fasting blood glucose (FBG), glycated hemoglobin (HbA1c), homeostasis model assessment of insulin resistance (HOMA-IR), fasting serum insulin (FINs), postprandial blood glucose (PBG), low-density lipoprotein (LDL), triglycerides (TG), high-density lipoprotein (HDL), total cholesterol (TCL), diastolic blood pressure (DBP), systolic blood pressure (SBP), body mass index (BMI), and quality of life.
2.2.2. Exclusion Criteria
The exclusion criteria were as follows: (1) animal studies and (2) network MAs, research protocols, narrative reviews, overviews, dissertation, and conference abstracts.
2.3. Data Sources and Search Strategy
The literatures were retrieved from PubMed, Cochrane Library, Embase, Chongqing VIP, Wanfang Database, CNKI, and SINOMED on January 1, 2022. We adopted a strategy that combines keyword search with free word search, and the keywords include “Type 2 Diabetes Mellitus”, “Tai Chi”, “Systematic Review”, and “Meta-Analysis”. The literature search strategy of the PubMed database is shown in Table 1, which was reasonably tuned for each database. We also reviewed the references of all retrieved literatures to avoid missing topic-related SRs/MAs.
Table 1.
Search strategy for the PubMed database.
| Query | Search term |
|---|---|
| #1 | “Tai Ji”[Mesh] |
| #2 | “Tai-ji” OR “Tai Chi” OR “Chi, Tai” OR “Tai Ji Quan” OR “Ji Quan, Tai” OR “Quan, Tai Ji” OR “Taiji" OR “Taijiquan” OR “T'ai Chi” OR “Tai Chi Chuan” OR “Tai ji” |
| #3 | #1 OR #2 |
| #4 | “Diabetes Mellitus, Type 2”[Mesh] |
| #5 | “Diabetes Mellitus, Noninsulin-Dependent” OR “Diabetes Mellitus, Ketosis-Resistant” OR “Diabetes Mellitus, Ketosis Resistant” OR “Ketosis-Resistant Diabetes Mellitus” OR “Diabetes Mellitus, Non Insulin Dependent” OR “Diabetes Mellitus, Non-Insulin-Dependent” OR “Non-Insulin-Dependent Diabetes Mellitus” OR “Diabetes Mellitus, Stable” OR “Stable Diabetes Mellitus” OR “Diabetes Mellitus, Type II” OR "NIDDM” OR “Diabetes Mellitus, Noninsulin Dependent” OR “Diabetes Mellitus, Maturity-Onset” OR “Diabetes Mellitus, Maturity Onset” OR “Maturity-Onset Diabetes Mellitus” OR “Maturity Onset Diabetes Mellitus” OR “MODY” OR “Diabetes Mellitus, Slow-Onset” OR “Diabetes Mellitus, Slow Onset” OR “Slow-Onset Diabetes Mellitus” OR “Type 2 Diabetes Mellitus” OR “Noninsulin-Dependent Diabetes Mellitus” OR “Noninsulin Dependent Diabetes Mellitus" OR “Maturity-Onset Diabetes” OR “Diabetes, Maturity-Onset” OR “Maturity Onset Diabetes" OR “Type 2 Diabetes” OR “Diabetes, Type 2” OR “Diabetes Mellitus, Adult-Onset" OR “Adult-Onset Diabetes Mellitus” OR “Diabetes Mellitus, Adult Onset” |
| #6 | #4 OR #5 |
| #7 | Meta-Analysis as Topic [Mesh] |
| #8 | “Systematic review” OR “meta-analysis” OR “meta analysis” OR “meta-analyses” OR “Review, Systematic” |
| #9 | #7 OR #8 |
| #10 | #3 AND #6 AND #9 |
2.4. Literature Screening and Data Extraction
The literature screening (HS-S and YF-Z) and information extraction (PL-L and CD-C) were performed independently by two researchers. We imported the retrieved documents into Endnote X9 document management software and removed the duplicates. The literatures that potentially met the inclusion and exclusion criteria were then obtained by reading the titles and abstracts of these literatures. Ultimately, we finalized the included SRs/MAs by reading the full text. All SRs/MAs were read by two independent researchers, and the following data were extracted from the SRs/MAs: first author, publication year, country, number of RCTs included, interventions for experimental and control groups, included RCT quality assessment tools, and main conclusion. The disagreement between the two researchers was resolved through discussion.
2.5. SR/MA Quality Assessment
Two researchers (HS-S and CD-C) independently assessed the methodological and evidentiary quality of the included SRs/MAs.
2.6. Assessment of Methodological Quality
2.6.1. Estimate of Methodological Quality
The methodological quality of the included SRs/MAs was assessed by the Assessment System for Evaluating Methodological Quality 2 (AMSTAR-2) [21]. Seven (2, 4, 7, 9, 11, 13, and 15) of the 16 items in the tool were critical areas.
2.6.2. Assessment of Risk of Bias
The Risk of Bias in Systematic Review (ROBIS) [22] scale was used in this overview to evaluate the risk of bias of the inclusion of SRs/MAs. The scale was used to assess the overall risk of bias in the inclusion of SRs/MAs in three stages.
2.6.3. Assessment of Reporting Quality
The quality of each SR/MA report of the included SRs/MAs was evaluated by the list of PRISMA [23] which consisted of 27 items focusing on the reporting methods and results that were incorporated into the SRs/MAs.
2.6.4. Assessment of Quality of Evidence
The quality of evidence for each SR/MA outcome was evaluated by the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) [24], according to which, five aspects will lead to the degradation of evidence quality, including limitations, inconsistencies, indirectness, imprecision, and publication bias.
3. Results
3.1. Results on Literature Search and Selection
Using our search strategy, a total of 83 articles were identified. After removing 33 duplicate articles, the researchers screened the remaining 50 articles by reading titles and abstracts. Subsequently, 16 articles were obtained. After reading the full text, 6 articles [25–30] were found irrelevant to SRs/MAs in RCTs, and 2 SRs/MAs [31, 32] were not about people with T2DM. Thus, 8 SRs/MAs [33–40] were finally included in this overview. The process of study selection is shown in Figure 1.
Figure 1.
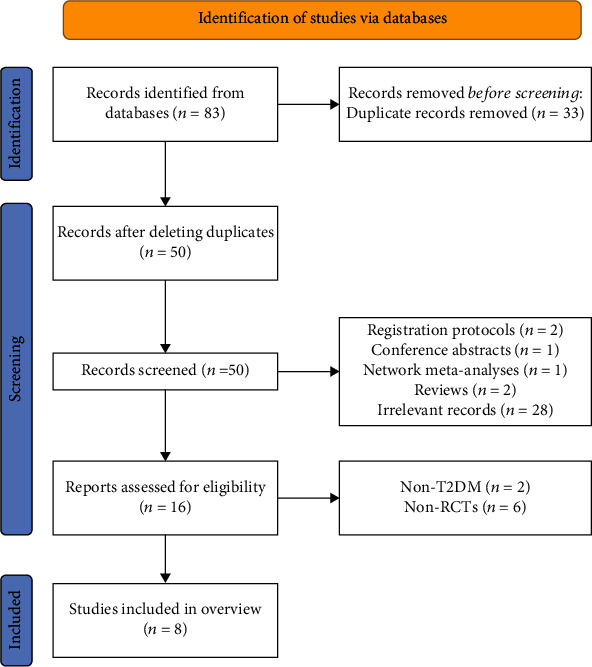
The flowchart of the screening process.
3.2. Description of Included SRs/MAs
The characteristics included in the overview are shown in Table 2. These SRs/MAs were all published between 2017 and 2021, 5 [33–37] of which were in English, and the remaining 3 [38–40] were in Chinese. One [34] of the SRs/MAs was published by Korean researchers, and the remaining 7 SRs/MAs [33, 35–40] were published by Chinese researchers. The number of RCTs was between 10 and 23, and the sample size was between 740 and 1,800. In terms of quality evaluation scales, 6 SRs/MAs [34–36, 38–40] used the Cochrane risk of bias standard, 1 SR/MA [37] used the Physiotherapy Evidence Database scale, and 1 SR/MA [33] used the Jadad scale.
Table 2.
Characteristics of the included SRs/MAs. Note: N: nonexercise; AE: aerobic exercise; ST: standard treatment.
| Author, year (country) | Trials (subjects) | Intervention group | Control group | Quality assessment | Main results |
|---|---|---|---|---|---|
| Mengyao Chao, 2018 (China) [33] | 14 (798) | TC | N, AE | Jadad | TC can effectively influence the management of blood glucose and HbA1c in patients with T2DM. Long-term adherence to TC has a better effect on reducing blood sugar and HbA1c levels in patients with T2DM |
| Myeong Soo Lee, 2015 (South Korea) [34] | 15 (754) | TC, TC+control group | N, ST, AE | Cochrane criteria | In conclusion, the evidence that TC may benefit people with T2DM compared with exercise therapy is not convincing. In addition, evidence from RCTs comparing TC with conventional antidiabetic drugs appears to be mixed |
| Shuai Guo, 2021 (China) [35] | 23 (1,800) | TC, TC+control group | ST, AE | Cochrane criteria | Compared with routine clinical treatment, TC has better effects on blood sugar control, lipid metabolism, and body composition and is superior to aerobic exercise in improving partial metabolic control. The optimal intervention time window for TC may vary for different metabolic markers |
| Ting-Wei Xia, 2019 (China) [36] | 17 (774) | TC, TC+control group | N, ST, AE | Cochrane criteria | TC appears to be effective in treating T2DM compared to control interventions. Different training times and methods will lead to differences in effects |
| Zonglei Zhou, 2019 (China) [37] | 23 (1,235) | TC | AE, ST | PEDro scale | TC was effective in controlling biomedical outcomes and improving the quality of life-related outcomes in patients with T2DM, but no effects on balance and fasting insulin were observed |
| Yao Ge, 2020 (China) [38] | 13 (856) | TC, TC+control group | N, ST | Cochrane criteria | TC exercise can control blood sugar level and regulate lipoprotein concentration in patients with T2DM, which can provide the basis for exercise therapy for later stage diabetes |
| Yongjin Liu, 2017 (China) [39] | 10 (740) | TC | N, AE | Cochrane criteria | TC exercise can regulate the level of glucose and lipid metabolism and improve the quality of life in patients with T2DM and can be used as an important part of exercise therapy for diabetes |
| Qing Tang, 2017 (China) [40] | 11 (764) | TC | CT | Cochrane criteria | TC helps improve blood sugar control, weight loss, blood lipid regulation, and quality of life in patients with T2DM |
3.3. Results on SR/MA Quality Assessment
3.3.1. Methodological Quality Assessment
Regarding the methodological quality of the included SRs/MAs, all were considered to be of very low quality because more than one key item was missing from the SRs/MAs included in the quality assessment. Methodological quality limitations come from the following items: item 2 (none of the SR/MA registers the study protocol), item 7 (no SR/MA provided by SR/MA provided for exclusion), and item 13 (when interpreting the evaluation results, only 2 SRs/MAs [34, 36] considered the risk of bias in the main study). The evaluation details of the included SRs/MAs on the AMSTAR-2 are shown in Table 3.
Table 3.
Result of the AMSTAR-2 assessments. Note: Y: yes; PY: partial yes; N: no; VL: very low; L: low. Note: key items are marked in italic.
| Author, year (country) | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Q14 | Q15 | Q16 | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mengyao Chao, 2018 (China) [33] | Y | PY | Y | Y | Y | Y | N | Y | Y | N | Y | Y | N | Y | Y | Y | VL |
| Myeong Soo Lee, 2015 (South Korea) [34] | Y | PY | Y | Y | Y | Y | N | Y | Y | N | Y | Y | Y | Y | N | Y | VL |
| Shuai Guo, 2021 (China) [35] | Y | PY | Y | Y | Y | Y | N | Y | Y | N | Y | Y | N | Y | N | Y | VL |
| Ting-Wei Xia, 2019 (China) [36] | Y | PY | Y | Y | Y | Y | N | Y | Y | N | Y | Y | Y | Y | Y | Y | VL |
| Zonglei Zhou, 2019 (China) [37] | Y | PY | Y | Y | Y | Y | N | Y | Y | N | Y | Y | N | Y | Y | Y | VL |
| Yao Ge, 2020 (China) [38] | Y | PY | Y | PY | Y | Y | N | N | Y | N | Y | Y | N | Y | N | Y | VL |
| Yongjin Liu, 2017 (China) [39] | Y | PY | Y | PY | Y | Y | N | Y | Y | N | Y | Y | N | Y | Y | Y | VL |
| Qing Tang, 2017 (China) [40] | Y | PY | Y | PY | Y | Y | N | Y | Y | N | Y | Y | N | Y | N | Y | VL |
3.3.2. Risk of Bias of the Included SRs/MAs
Regarding the results of the ROBIS assessment, phase 1 assessed the relevance of the study topic and domain 1, and all SRs/MAs were rated as low risk of bias in both items. Five [33–37] of the SRs/MAs were assessed as low risk in domain 2, 5 SRs/MAs [33, 35–37, 39] were assessed as low risk of bias in domain 3, and only 3 SRs/MAs [33, 36, 39] were assessed as low risk of bias in domain 4. In phase 3, only 2 SRs/MAs [34, 36] had a low risk of bias. The evaluation details of the included SRs/MAs on the ROBIS scale are shown in Table 4.
Table 4.
Results of the ROBIS assessments. Note: √: low risk; ×: high risk.
| Author, year (country) | Phase 1 | Phase 2 | Phase 3 | |||
|---|---|---|---|---|---|---|
| Assessing relevance | Domain 1: study eligibility criteria | Domain 2: identification and selection of studies | Domain 3: collection and study appraisal | Domain 4: synthesis and findings | Risk of bias in the review | |
| Mengyao Chao, 2018 (China) [33] | √ | √ | √ | √ | √ | × |
| Myeong Soo Lee, 2015 (South Korea) [34] | √ | √ | √ | × | × | √ |
| Shuai Guo, 2021 (China) [35] | √ | √ | √ | √ | × | × |
| Ting-Wei Xia, 2019 (China) [36] | √ | √ | √ | √ | √ | √ |
| Zonglei Zhou, 2019 (China) [37] | √ | √ | √ | √ | × | × |
| Yao Ge, 2020 (China) [38] | √ | √ | × | × | × | × |
| Yongjin Liu, 2017 (China) [39] | √ | √ | × | √ | √ | × |
| Qing Tang, 2017 (China) [40] | √ | √ | × | × | × | × |
3.3.3. Report Quality of the Included SRs/MAs
The results of the PRISMA inventory evaluation are shown in Table 5. 22 out of 27 items have a “yes” response rate of more than 70%, and this shows that the report was relatively complete. However, there were some reporting deficiencies in other items. The reports of item 5 (protocol and registration), item 8 (search), and item 15 (risk of bias across studies, methods) were incomplete (the “yes” response rate was less than 50%).
Table 5.
Results of the PRISMA checklist. Note: Y: yes; N: no.
| Section/topic | Items | Mengyao Chao, 2018 (China) [33] | Myeong Soo Lee, 2015 (South Korea) [34] | Shuai Guo, 2021 (China) [35] | Ting-Wei Xia, 2019 (China) [36] | Zonglei Zhou, 2019 (China) [37] | Yao Ge, 2020 (China) [38] | Yongjin Liu, 2017 (China) [39] | Qing Tang, 2017 (China) [40] | Number of yes (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Title | Q1. Title | Y | Y | Y | Y | Y | Y | Y | Y | 100% |
|
| ||||||||||
| Abstract | Q2. Structured summary | Y | Y | Y | Y | Y | Y | Y | Y | 100% |
|
| ||||||||||
| Introduction | Q3. Rationale | Y | Y | Y | Y | Y | Y | Y | Y | 100% |
| Q4. Objectives | Y | Y | Y | Y | Y | Y | Y | Y | 100% | |
|
| ||||||||||
| Methods | Q5. Protocol and registration | N | N | N | N | N | N | N | N | 0% |
| Q6. Eligibility criteria | Y | Y | Y | Y | Y | Y | Y | Y | 100% | |
| Q7. Information sources | Y | Y | Y | Y | Y | Y | Y | Y | 100% | |
| Q8. Search | N | N | Y | N | Y | N | N | N | 25% | |
| Q9. Study selection | Y | Y | Y | Y | Y | Y | Y | Y | 100% | |
| Q10. Data collection process | Y | Y | Y | Y | Y | Y | Y | Y | 100% | |
| Q11. Data items | Y | Y | Y | Y | Y | Y | Y | Y | 100% | |
| Q12. Risk of bias in individual studies | Y | Y | Y | Y | Y | Y | Y | Y | 100% | |
| Q13. Summary measures | Y | Y | Y | Y | Y | Y | Y | Y | 100% | |
| Q14. Synthesis of results | Y | Y | Y | Y | Y | Y | Y | Y | 100% | |
| Q15. Risk of bias across studies | N | N | N | Y | Y | N | N | N | 25.00% | |
| Q16. Additional analyses | Y | N | Y | Y | Y | N | N | Y | 62.50% | |
|
| ||||||||||
| Results | Q17. Study selection | Y | Y | Y | Y | Y | Y | Y | Y | 100% |
| Q18. Study characteristics | Y | Y | Y | Y | Y | N | Y | Y | 88% | |
| Q19. Risk of bias within studies | Y | Y | Y | Y | Y | Y | Y | Y | 100% | |
| Q20. Results of individual studies | Y | Y | Y | Y | Y | Y | Y | Y | 100% | |
| Q21. Synthesis of results | Y | Y | Y | Y | Y | Y | Y | Y | 100% | |
| Q22. Risk of bias across studies | Y | N | N | Y | Y | N | Y | N | 50.00% | |
| Q23. Additional analysis | Y | N | Y | Y | Y | N | Y | Y | 75.00% | |
|
| ||||||||||
| Discussion | Q24. Summary of evidence | Y | Y | Y | Y | Y | Y | Y | Y | 100% |
| Q25. Limitations | Y | Y | Y | Y | Y | Y | Y | Y | 100% | |
| Q26. Conclusions | Y | Y | Y | Y | Y | Y | Y | Y | 100% | |
|
| ||||||||||
| Funding | Q27. Funding | Y | Y | Y | Y | Y | Y | Y | Y | 100% |
3.3.4. Evidence Quality of the Included SRs/MAs
The 8 SRs/MAs included 65 outcomes related to the effectiveness of TC for T2DM. By means of the GRADE evaluation, 1 was rated as high quality, 7 moderate quality, 10 low quality, and 47 very low quality in terms of the quality of evidence for all outcome indicators. Risk of bias (n = 58) was the most common downgrading factor, followed by publication bias (n = 47), inconsistency (n = 37), imprecision (n = 37), and indirectness (n = 0). GRADE-specific assessment details are shown in Table 6.
Table 6.
Results of evidence quality. ①The included studies have a large bias in methodology such as randomization, allocation concealment, and blinding. ②The confidence interval overlaps less, or the I2 value of the combined results was larger. ③The sample size from the included studies does not meet the optimal sample size, or the 95% confidence interval crosses the invalid line. ④The funnel chart is asymmetry. ∗The 95% confidence interval does not cross the invalid line.
| Author, year (Country) | Outcomes | Studies (participants) | Limitations | Inconsistency | Indirectness | Imprecision | Publication bias | Relative effect (95% CI) | Quality |
|---|---|---|---|---|---|---|---|---|---|
| Mengyao Chao, 2018 (China) [28] | FBG (tai chi versus nonexercise) | 10 (489) | -1① | -1② | 0 | 0 | -1④ | MD = −1.39 (-1.95, -0.84)∗ | Very low |
| FBG (tai chi versus other aerobic exercises) | 7 (342) | -1① | -1② | 0 | -1③ | -1④ | MD = −0.21 (-0.61, 0.19) | Very low | |
| HbA1c (tai chi versus nonexercise) | 7 (293) | -1① | 0 | 0 | -1③ | -1④ | MD = −0.73 (-0.95, -0.52)∗ | Very low | |
| HbA1c (tai chi versus other aerobic exercises) | 7 (372) | -1① | -1② | 0 | -1③ | -1④ | MD = −0.19 (-0.37, 0.00)∗ | Very low | |
| PBG (tai chi versus nonexercise) | 5 (162) | -1① | 0 | 0 | -1③ | -1④ | MD = −2.07 (-2.89, -1.26)∗ | Very low | |
| PBG (tai chi versus other aerobic exercises) | 3 (84) | -1① | 0 | 0 | -1③ | -1④ | MD = −0.44 (-1.42, 0.54) | Very low | |
|
| |||||||||
| Myeong Soo Lee, 2015 (South Korea) [29] | HbA1c (tai chi versus ST) | 3 (127) | -1① | 0 | 0 | -1③ | -1④ | MD = −0.54 (−1.23, 0.15) | Very low |
| HbA1c (tai chi versus other aerobic exercises) | 2 (148) | -1① | 0 | 0 | -1③ | -1④ | MD = 0.00 (−0.31, 0.31) | Very low | |
| HbA1c (no) | 2 (84) | -1① | -1② | 0 | -1③ | -1④ | MD = −1.58 (−3.83, 0.67) | Very low | |
| FBG (tai chi versus ST) | 4 (188) | -1① | 0 | 0 | -1③ | -1④ | MD = −1.57 (−2.34, −0.80)∗ | Very low | |
| FBG (tai chi versus other aerobic exercises) | 4 (212) | -1① | 0 | 0 | -1③ | -1④ | MD = −0.03 (−0.49, 0.42) | Very low | |
|
| |||||||||
| Shuai Guo, 2021 (China) [30] | FBG (tai chi versus ST) | 15 (1,023) | -1① | -1② | 0 | 0 | -1④ | MD = −1.04 (-1.42, -0.66)∗ | Very low |
| FBG (tai chi versus other aerobic exercises) | 8 (619) | -1① | -1② | 0 | -1③ | -1④ | MD = −0.03 (-0.30, 0.23) | Very low | |
| HbA1c (tai chi versus ST) | 9 (749) | -1① | -1② | 0 | 0 | -1④ | MD = −0.73 (-1.03, -0.43)∗ | Very low | |
| HbA1c (tai chi versus other aerobic exercises) | 5 (504) | -1① | 0 | 0 | 0 | -1④ | MD = −0.33 (-0.61, 0.04)∗ | Low | |
| PBG (tai chi versus ST) | 2 (260) | -1① | 0 | 0 | -1③ | -1④ | MD = −1.58 (-1.94,-1.22)∗ | Very low | |
| TCL (tai chi versus ST) | 11 (868) | -1① | -1② | 0 | 0 | -1④ | MD = −0.51 (-0.88, -0.14)∗ | Very low | |
| TCL (tai chi versus other aerobic exercises) | 5 (423) | -1① | 0 | 0 | -1③ | -1④ | MD = −0.08 (-0.24, 0.09) | Very low | |
| TG (tai chi versus ST) | 9 (745) | -1① | -1② | 0 | 0 | -1④ | MD = −0.40 (-0.72, -0.07)∗ | Very low | |
| TG (tai chi versus other aerobic exercises) | 4 (332) | -1① | -1② | 0 | -1③ | -1④ | MD = 0.04 (−0.22, 0.31) | Very low | |
| HDL (tai chi versus ST) | 9 (798) | -1① | -1② | 0 | 0 | -1④ | MD = 0.39 (0.14, 0.63)∗ | Very low | |
| HDL (tai chi versus other aerobic exercises) | 5 (538) | -1① | 0 | 0 | 0 | -1④ | MD = 0.24 (0.07, 0.41)∗ | Low | |
| LDL (tai chi versus ST/other aerobic exercises) | 9 (730) | -1① | -1② | 0 | 0 | -1④ | MD = −0.79 (-1.27, -0.30)∗ | Very low | |
| BMI (tai chi versus ST) | 5 (358) | -1① | 0 | 0 | 0 | -1④ | MD = −1.15 (-1.79, -0.51)∗ | Low | |
| SBP (tai chi versus ST) | 5 (390) | -1① | 0 | 0 | -1③ | -1④ | MD = −11.86 (-14.47, -9.25)∗ | Very low | |
| DBP (tai chi versus ST) | 5 (390) | -1① | -1② | 0 | -1③ | -1④ | MD = −7.93 (-12.39, -3.46)∗ | Very low | |
| FINs (tai chi versus ST) | 3 (255) | -1① | 0 | 0 | -1③ | -1④ | MD = −1.02 (-1.39, -0.64)∗ | Very low | |
| HOMA-IR (tai chi versus ST) | 3 (255) | -1① | -1② | 0 | -1③ | -1④ | MD = −0.65 (-1.01, -0.30)∗ | Very low | |
|
| |||||||||
| Ting-Wei Xia, 2019 (China) [31] | FBG | 13 (616) | -1① | -1② | 0 | 0 | -1④ | SMD = −0.54 (-0.91, -0.16)∗ | Very low |
| HbA1c | 9 (517) | -1① | -1② | 0 | 0 | -1④ | SMD = −0.68 (-1.17, -0.19)∗ | Very low | |
| TCL | 8 (343) | -1① | 0 | 0 | -1③ | -1④ | SMD = −0.35 (-0.54, -0.16)∗ | Very low | |
| TG | 8 (359) | -1① | 0 | 0 | -1③ | -1④ | SMD = −0.19 (-0.31, -0.07)∗ | Very low | |
| HDL | 6 (290) | -1① | 0 | 0 | -1③ | -1④ | SMD = 0.04 (− 0.01, 0.09) | Very low | |
| LDL | 6 (290) | -1① | -1② | 0 | -1③ | -1④ | SMD = −0.49 (− 1.06, 0.08) | Very low | |
| BMI | 6 (296) | -1① | 0 | 0 | -1③ | -1④ | SMD = −0.61 (− 0.85, − 0.38)∗ | Very low | |
|
| |||||||||
| Zonglei Zhou, 2019 (China) [32] | FBG | 21 (1,115) | -1① | -1② | 0 | 0 | 0 | SMD = −0.67 (-0.87, -0.47)∗ | Low |
| HbA1c | 12 (714) | 0 | 0 | 0 | 0 | 0 | MD = −0.53 (-0.62, -0.44)∗ | High | |
| FINs | 8 (500) | -1① | -1② | 0 | -1③ | 0 | SMD = −0.32 (-0.71, 0.07) | Very low | |
| HOMA-IR | 5 (332) | 0 | 0 | 0 | -1③ | 0 | MD = −0.41 (-0.78, -0.04)∗ | Moderate | |
| TCL | 10 (658) | -1① | -1② | 0 | 0 | 0 | SMD = −0.59 (-0.90, -0.27)∗ | Low | |
| BMI | 7 (388) | 0 | 0 | 0 | -1③ | 0 | MD = −0.82 (-1.28, -0.37)∗ | Moderate | |
| Balance | 2 (107) | 0 | -1② | 0 | -1③ | 0 | MD = 2.71 (-3.29, 8.71) | Low | |
| SBP | 5 (290) | 0 | -1② | 0 | -1③ | 0 | MD = −10.03 (-15.78, -4.29)∗ | Low | |
| DBP | 5 (290) | 0 | 0 | 0 | -1③ | 0 | MD = −4.85 (-8.23, -1.47)∗ | Moderate | |
| Physical function | 5 (389) | -1① | -1② | 0 | -1③ | 0 | MD = 7.07 (0.79, 13.35)∗ | Very low | |
| Bodily pain | 5 (389) | -1① | 0 | 0 | -1③ | 0 | MD = 4.30 (0.83, 7.77)∗ | Low | |
| Social function | 6 (426) | 0 | -1② | 0 | 0 | 0 | MD = 13.84 (6.22, 21.47)∗ | Moderate | |
|
| |||||||||
| Yao Ge, 2020 (China) [33] | FBG | 9 (560) | -1① | -1② | 0 | 0 | -1④ | SMD = −0.607 (-0.930, -0.284)∗ | Very low |
| HbA1c | 7 (434) | -1① | -1② | 0 | 0 | -1④ | SMD = −0.585 (-0.784, -0.386)∗ | Very low | |
| TCL | 7 (533) | -1① | -1② | 0 | -1③ | -1④ | SMD = −0.418 (-0.897, 0. 061) | Very low | |
| TG | 6 (480) | -1① | -1② | 0 | 0 | -1④ | SMD = −0.833 (-1.383, -0.283)∗ | Very low | |
| HDL | 4 (420) | -1① | -1② | 0 | 0 | -1④ | SMD = 0.458 (0. 063, 0.852)∗ | Very low | |
| LDL | 3 (76) | -1① | -1② | 0 | -1③ | -1④ | SMD = −1.252 (-2.305, -0.199) | Very low | |
|
| |||||||||
| Yongjin Liu, 2017 (China) [34] | FBG | 9 (727) | -1① | 0 | 0 | 0 | 0 | SMD = −0.39 (-0.54, -0.24)∗ | Moderate |
| HbA1c | 7 (645) | -1① | 0 | 0 | 0 | 0 | MD = −0.59 (-0.73, -0.44)∗ | Moderate | |
| TCL | 7 (612) | -1① | -1② | 0 | -1③ | 0 | SMD = −0.24 (-0.58, 0.10) | Very low | |
| TG | 7 (612) | -1① | -1② | 0 | 0 | 0 | SMD = −0.52 (-0.85, -0.19)∗ | Low | |
| HDL | 6 (566) | -1① | 0 | 0 | 0 | 0 | SMD = 0.31 (0.14, 0.47)∗ | Moderate | |
| LDL | 6 (462) | -1① | -1② | 0 | 0 | 0 | MD = −0.32 (-0.59, -0.05)∗ | Low | |
|
| |||||||||
| Qing Tang, 2017 (China) [35] | FBG | 7 (354) | -1① | -1② | 0 | -1③ | -1④ | MD = −0.74 (-1.32, -0.16)∗ | Very low |
| HbA1c | 7 (572) | -1① | -1② | 0 | 0 | -1④ | MD = −0.77 (-1.16, -0.39)∗ | Very low | |
| BMI | 4 (316) | -1① | 0 | 0 | -1③ | -1④ | MD = −1.64, (-2.35, -0.92)∗ | Very low | |
| TG | 6 (518) | -1① | -1② | 0 | 0 | -1④ | MD = −0.33 (-0.49, -0.17)∗ | Very low | |
| TCL | 6 (518) | -1① | -1② | 0 | 0 | -1④ | MD = −0.08 (-0.33, -0.48)∗ | Very low | |
| Quality of Life | 2 (264) | -1① | 0 | 0 | -1③ | -1④ | MD = 45.47 (18.24, 72.71)∗ | Very low | |
3.4. Summary Results of the Included Studies
The result indicators extracted from the included studies are listed in Table 6.
3.4.1. Outcomes Related to Glucose Metabolism
Eight SRs/MAs [33–40] reported the effect of TC on FGB in patients with T2DM, and all SRs/MAs indicated that TC could significantly reduce FGB. However, 3 subreports [33–35] also showed that compared with other aerobic exercises, TC had no significant effect on FGB. Eight SRs/MAs [33–40] reported the effect of TC on HbA1c in T2DM patients, of which 7 SRs/MAs [33, 35–40] indicated that TC could significantly reduce HbA1c levels. Two SRs/MAs [33, 35] reported the effect of TC on PBG in T2DM patients. Two reports [33, 35] showed that TC could significantly reduce PBG level, and 1 report [33] showed that TC had no significant effect on PBG compared with other aerobic exercises. Two SRs/MAs [33, 37] reported the effect of TC on FINs, and one SR/MA [35] showed that TC was beneficial for lowering FINs. In addition, 2 SRs/MAs [33, 37] reported that TC reduced HOMA-IR in T2DM patients.
3.4.2. Outcome-Related Lipid Metabolism
Six SRs/MAs [35–40] reported the effect of TC on TCL in T2DM patients, of which 4 reports [35–37, 40] showed that TC could significantly reduce TCL level, while 3 reports [35, 38, 39] showed that the effect of TC on TCL was not statistically significant. Five SRs/MAs [35, 36, 38–40] reported the effect of TC on TG in T2DM patients. Five reports [35, 36, 38–40] suggested that TC could significantly reduce TG level, while 1 report [35] showed that TC had no significant effect on TG compared with other aerobic exercises. Four SRs/MAs [35, 36, 38, 39] reported the effect of TC on LDL in patients with T2DM, of which 2 SRs/MAs [36, 38] showed that TC could significantly lower LDL levels. Four SRs/MAs [35, 36, 38, 39] reported the effect of TC on HDL in patients with T2DM, and 3 of the SRs/MAs [35, 38, 39] indicated that TC could significantly improve HDL levels.
3.4.3. Other Outcomes
Four SRs/MAs [35–37, 40] reported that TC reduced BMI in T2DM patients. One SR/MA [37] reported that TC reduced SBP and DBP in T2DM patients. Two SRs/MAs [37, 40] reported that TC could improve the quality of life of patients with T2DM. One SR/MA [37] result showed that TC had no statistically significant effect on balance.
3.4.4. Adverse Event
There are 3 SR/MA narrative reviews suggesting that TC is safe.
4. Discussion
Exercise therapy is recommended for T2DM management because regular physical activity improves glycemic control as well as lipid index, blood pressure, cardiovascular disease, and quality of life [41]. TC is a low-to-moderate-intensity mind-body exercise that originated in China and is very popular around the world [42]. This overview is the first comprehensive and systematic assessment of the SRs/MAs associated with TC intervention for T2DM and will help to establish a clear link between the need to resolve uncertainty and prior clinical knowledge [43].
4.1. Summary of the Main Findings
This overview includes 8 SRs/MAs on the impact of TC on T2DM. All SRs/MAs are based on RCTs and published from 2015 to 2021. Among them, 7 (7/8, 87.5%) SRs/MAs were published in the past five years, indicating that the improvement effect of TC on T2DM has attracted increasing attention over the years.
Based on the results of the AMSTAR-2 evaluation in this overview, the methodological quality of all SRs/MAs was assessed as very low, especially in item 2 (protocol registration, 0/8, 0%), item 7 (exclusion list, 0/8, 0%), and item 13 (RoB account, 2/8, 25%). None of the SR/MA registered study protocols. No SR/MA contained initial research protocol registrations, which could lead to greater than expected adjustments to the research process, increasing the risk of bias and impacting the rigor and credibility of the final SR/MA results [44]. None of the SR/MA provides a complete exclusion of the lists for each study, which may affect the reliability of the results and assessment of publication bias. Providing a list of exclusion researches is a more strong demonstration of the rigor of the literature screening process. The authors of the 6 SRs/MAs did not consider the risk of bias of including RCTs when interpreting or discussing the study results, which may reduce the reliability of the final results. The risk of bias assessment of the ROBIS scale indicated that only one SR/MA was at low risk. Further analysis revealed that inadequate interpretation of the risk of bias and inadequate evaluation of publication bias were the main factors contributing to the high risk of bias. Similar to the results of the AMSTAR-2, the PRISMA assessment results indicate a lack of registration of programs. In addition, the included literatures only provided search keywords without elaborating specific search strategies, which reduces the reproducibility and credibility of the research.
According to the evidence quality assessment for the 65 outcomes by means of GRADE, 1 was rated as high quality, 7 moderate quality, 10 low quality, and 47 very low quality. Further generalization revealed the following common pitfalls in the inclusion of RCTs: only randomization was mentioned, without elaborating specific randomization method; allocation was not concealed; and only single blinding was performed. Therefore, the low methodological quality of the included trials was the underlying factor contributing to the decline of evidence quality. Besides, the lack of publication bias assessment was also an important reason for the downgrading of the evidence quality. The high heterogeneity of relevant outcome measures may be related to the unreasonable design of the original study. In addition, the insufficient scale included in the RCTs was also an important downgrading factor. Descriptive analysis showed that TC is an effective and safe method for the treatment of T2DM. Due to the low quality of methodology and evidence from the included studies, the conclusions of SRs/MAs may differ from real results, so we cannot draw firm conclusions about TC for T2DM.
4.2. Implications for Practice and Research
As a regular small-to-medium-intensity aerobic exercise, the main benefit of TC is not to consume calories but to promote the metabolism of cells and tissues, enhance cardiopulmonary function, activate antioxidant and anti-inflammatory activities, promote blood return to the heart, and improve the body's ability to respond to glucose. It can improve the utilization rate of target cells, improve the body's glucose tolerance, prevent the composition of HbA1c, and accelerate the combination of hemoglobin and oxygen [45]. In addition to this, the antioxidant effect of TC can be explained by the excitatory process, in which TC acts as a moderate exercise and the continuous stimulation of ROS generated by the adaptive process promotes the antioxidant response [46]. In this case, the main associated proteins are MAPK and FNkB [47] and the antioxidant gene Nrf2. Regular exercise leads to the upregulation of endogenous antioxidant defenses and counteracts the harmful effects of ROS [48]. Given the nature of TC exercise, the antioxidant effects may be attributed not only to the described excitatory processes but also to the interplay among several mechanisms related to meditation and diaphragmatic respiration. Studies have shown that psychological stress is positively correlated with increased production of free radicals and OS [49]. As for diaphragmatic breathing exercise, one study showed that the relaxation induced by diaphragmatic breathing increases the antioxidant defense status of athletes after exhaustive exercise [50].
In conclusion, when using the AMSTAR-2, PRISMA, ROBIS, and GRADE assessments to assess and standardize various aspects of the included SR/MA, researchers are expected to register or publish research protocols in advance when conducting SRs/MAs to minimize the risk of bias and ensure the accuracy of SRs/MAs results, and they should also provide a list of excluded literatures to ensure transparency and avoid publication bias. For literatures at high risk of bias, researchers should conduct separate analyses and provide reasonable explanations to ensure the quality of the evidence. In addition, a complete assessment of publication bias would also improve the accuracy of the meta-analysis results. Although the peculiarities of TC therapy can make blinding difficult to implement, a carefully designed and rigorously implemented RCT can minimize or avoid bias, which is the gold standard for evaluating interventions [51]. Clinical researchers should improve the top-level design of clinical trials through comprehensive evaluation and sophisticated analysis. Notably, Consolidated Standards of Reporting Trials (CONSORT) should be used to improve the quality of evidence from RCTs [52]. In view of the low evidence quality regarding the effect of TC exercise on T2DM, researchers should strictly describe all stages of their research, specify the research scheme, and register study protocols in their future researches, so as to facilitate publication and subsequent inclusion in SRs/MAs. At the same time, during SRs/MAs, researchers should also strictly follow relevant methodologies to improve the evidence system.
Although TC originated from traditional Chinese medicine theory, the duration, frequency, and mode of TC movement vary greatly in different studies. Therefore, we propose to use a standardized TC training program, where duration, frequency, and pattern are formalized, so as to better study the impact of TC on T2DM. Researchers should also pay attention to the effect of TC on related biochemical indicators in T2DM patients, including indicators related to OS. In addition to this, most studies focused on the therapeutic effects of TC on T2DM, but it still remains unclear whether TC can reduce the risk of associated complications in individuals with T2DM. Further research on the relationship between TC and the risk of developing various complications of T2DM is recommended.
4.3. Strength and Limitations
Our overview is the first to use AMSTAR2, ROBIS, PRISMA, and GRADE to evaluate SRs/MAs regarding the impact of TC on T2DM. Based on the current results, TC may be an effective adjunctive replacement therapy for T2DM. Furthermore, the evaluation process revealed clear limitations of the current relevant SRs/MAs and RCTs, which may help guide future high-quality clinical studies. However, this overview has certain limitations because the assessment is subjective. While our assessments were assessed and reviewed by two independent assessors, different assessors may have their personal judgment on each factor, so the results may vary.
5. Conclusion
In conclusion, TC is beneficial and safe for T2DM. However, due to the generally low methodological and evidentiary quality of the included SRs/MAs, clinicians should approach these findings with caution in their practice.
Acknowledgments
The study was financially supported by the Natural Science Foundation of Shandong Province (ZR2020MH361), Shandong Medical and Health Science and Technology Development Plan Project (2019WS562), and project funded by the China Postdoctoral Science Foundation (2021M692750).
Contributor Information
Wenbo Wang, Email: wangvenbo@126.com.
Yujie Li, Email: liyujie.11@163.com.
Data Availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Authors' Contributions
LYJ, WWB, and SGM participated in the research design. SHS, DCD, WD, and, LPL conducted a literature search and screened data extraction. LPL, ZYF, and WD analyzed the data, did a statistical analysis, and wrote a manuscript. SHS, WWB, and LPL participated in the correction of the manuscript. The manuscript was revised by WST. All authors reviewed the manuscript. All authors read and approved the final version of the manuscript. Hongshuo Shi and Shaoting Wang are the co-first authors.
References
- 1.DeFronzo R. A., Ferrannini E., Groop L., et al. Type 2 diabetes mellitus. Nature Reviews Disease Primers . 2015;1(1, article 15019) doi: 10.1038/nrdp.2015.19. [DOI] [PubMed] [Google Scholar]
- 2.Rehman K., Akash M. S. H. Mechanism of generation of oxidative stress and pathophysiology of type 2 diabetes mellitus: how are they interlinked? Journal of Cellular Biochemistry . 2017;118(11):3577–3585. doi: 10.1002/jcb.26097. [DOI] [PubMed] [Google Scholar]
- 3.Federation ID. IDF Diabetes Atlas, 9th edn. 2019. July 2020, http://www.diabetesatlas.org.
- 4.Yin B., Bi Y. M., Fan G. J., Xia Y. Q. Molecular mechanism of the effect of Huanglian Jiedu decoction on type 2 diabetes mellitus based on network pharmacology and molecular docking. Journal of Diabetes Research . 2020;2020:24. doi: 10.1155/2020/5273914.5273914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang Y., Fu F. H. Effects of 14-week Tai Ji Quan exercise on metabolic control in women with type 2 diabetes. The American Journal of Chinese Medicine . 2008;36(4):647–654. doi: 10.1142/S0192415X08006119. [DOI] [PubMed] [Google Scholar]
- 6.Powers S. K., Deminice R., Ozdemir M., Yoshihara T., Bomkamp M. P., Hyatt H. Exercise-induced oxidative stress: friend or foe? Journal of Sport and Health Science . 2020;9(5):415–425. doi: 10.1016/j.jshs.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oguntibeju O. O. Type 2 diabetes mellitus, oxidative stress and inflammation: examining the links. International Journal of Physiology, Pathophysiology and Pharmacology . 2019;11(3):45–63. [PMC free article] [PubMed] [Google Scholar]
- 8.Butkowski E. G., Jelinek H. F. Hyperglycaemia, oxidative stress and inflammatory markers. Redox Report . 2017;22(6):257–264. doi: 10.1080/13510002.2016.1215643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Poblete-Aro C., Russell-Guzmán J., Parra P., et al. Efecto del ejercicio físico sobre marcadores de estrés oxidativo en pacientes con diabetes mellitus tipo 2. Revista Médica de Chile . 2018;146(3):362–372. doi: 10.4067/s0034-98872018000300362. [DOI] [PubMed] [Google Scholar]
- 10.Zheng H., Zhang D., Zhu Y., Wang Q. Effect of tai chi exercise on lower limb function and balance ability in patients with knee osteoarthritis: a protocol of a randomized controlled trial. Medicine . 2021;100(46, article e27647) doi: 10.1097/MD.0000000000027647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang Z. G., Feng Y. H., Li Y. H., Lv C. S. Systematic review and meta-analysis: tai chi for preventing falls in older adults. BMJ Open . 2017;7(2, article e013661) doi: 10.1136/bmjopen-2016-013661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosado-Pérez J., Castelán-Martínez O. D., Mújica-Calderón A. J., Sánchez-Rodríguez M. A., Mendoza-Núñez V. M. Effect of tai chi on markers of oxidative stress: systematic review and meta-analysis. International Journal of Environmental Research and Public Health . 2021;18(7):p. 3458. doi: 10.3390/ijerph18073458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Diabetes Association. 4. Lifestyle management: standards of medical care in diabetes-2018. Diabetes Care . 2018;41(Suppl 1):S38–S50. doi: 10.2337/dc18-S004. [DOI] [PubMed] [Google Scholar]
- 14.Higgins J. P. T., Green S. Cochrane handbook for systematic reviews of interventions . London, UK: Cochrane; 2011. Cochrane Book Series Naunyn-Schmiedebergs Archiv für Experimentelle Pathologie Und Pharmakologie. [Google Scholar]
- 15.Pussegoda K., Turner L., Garritty C., et al. Systematic review adherence to methodological or reporting quality. Systematic Reviews . 2017;6(1):p. 131. doi: 10.1186/s13643-017-0527-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pollock M., Fernandes R. M., Becker L. A., Featherstone R., Hartling L. What guidance is available for researchers conducting overviews of reviews of healthcare interventions? A scoping review and qualitative metasummary. Systematic Reviews . 2016;5(1):p. 190. doi: 10.1186/s13643-016-0367-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cumpston M., Li T., Page M. J., et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database of Systematic Reviews . 2019;10, article ED000142 doi: 10.1002/14651858.ED000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shi H., Wang D., Chen W., Li Y., Si G., Yang T. Quality of evidence supporting the role of supplement curcumin for the treatment of ulcerative colitis: an overview of systematic reviews. Gastroenterology Research and Practice . 2022;2022 doi: 10.1155/2022/3967935. Published 2022 Feb 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu N., Zhang T., Sun J., et al. An overview of systematic reviews of Chinese herbal medicine for Alzheimer's disease. Frontiers in Pharmacology . 2021;12 doi: 10.3389/fphar.2021.761661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shen M., Huang J., Qiu T. Quality of the evidence supporting the role of acupuncture for stable angina pectoris: an umbrella review of systematic reviews. Frontiers in Cardiovascular Medicine . 2021;8 doi: 10.3389/fcvm.2021.732144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Atkins D., Best D., Briss P. A., et al. Grading quality of evidence and strength of recommendations. BMJ . 2004;328(7454):p. 1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu F., Chen X., Nie P., et al. Can tai chi improve cognitive function? A systematic review and meta-analysis of randomized controlled trials. Journal of Alternative and Complementary Medicine . 2021;27(12):1070–1083. doi: 10.1089/acm.2021.0084. [DOI] [PubMed] [Google Scholar]
- 23.Yang J., Zhang L., Tang Q., et al. Tai chi is effective in delaying cognitive decline in older adults with mild cognitive impairment: evidence from a systematic review and meta-analysis. Evidence-based Complementary and Alternative Medicine . 2020;2020 doi: 10.1155/2020/3620534. Published 2020 Mar 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gu R., Gao Y., Zhang C., Liu X., Sun Z. Effect of tai chi on cognitive function among older adults with cognitive impairment: a systematic review and meta-analysis. Evidence-based Complementary and Alternative Medicine . 2021;2021:9. doi: 10.1155/2021/6679153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee M. S., Choi T. Y., Lim H. J., Ernst E. Tai chi for management of type 2 diabetes mellitus: a systematic review. Chinese Journal of Integrative Medicine . 2011;17(10):789–793. doi: 10.1007/s11655-011-0812-1. [DOI] [PubMed] [Google Scholar]
- 26.Palermi S., Sacco A. M., Belviso I., et al. Effectiveness of tai chi on balance improvement in type 2 diabetes patients: a systematic review and meta-analysis. Journal of Aging and Physical Activity . 2020;28(5):787–797. doi: 10.1123/japa.2019-0242. [DOI] [PubMed] [Google Scholar]
- 27.Qin J., Chen Y., Guo S., et al. Effect of tai chi on quality of life, body mass index, and waist-hip ratio in patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Frontiers in Endocrinology . 2021;11, article 543627 doi: 10.3389/fendo.2020.543627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yan J. H., Gu W. J., Pan L. Lack of evidence on tai chi-related effects in patients with type 2 diabetes mellitus: a meta-analysis. Experimental and Clinical Endocrinology & Diabetes . 2013;121(5):266–271. doi: 10.1055/s-0033-1334932. [DOI] [PubMed] [Google Scholar]
- 29.Yu X., Chau J. P. C., Huo L. The effectiveness of traditional Chinese medicine-based lifestyle interventions on biomedical, psychosocial, and behavioral outcomes in individuals with type 2 diabetes: a systematic review with meta-analysis. International Journal of Nursing Studies . 2018;80:165–180. doi: 10.1016/j.ijnurstu.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 30.Yeting Z., Bin Z., Chuikun L. Effect of shadowboxing on patients with type 2 diabetes mellitus -- meta analysis. Sports Science and Technology Literature Bulletin . 2016;24(8):135–136. doi: 10.19379/j.cnki. [DOI] [Google Scholar]
- 31.Chau J. P. C., Leung L. Y. L., Liu X., et al. Effects of tai chi on health outcomes among community-dwelling adults with or at risk of metabolic syndrome: a systematic review. Complementary Therapies in Clinical Practice . 2021;44, article 101445 doi: 10.1016/j.ctcp.2021.101445. [DOI] [PubMed] [Google Scholar]
- 32.Zhongjun S., Ping H. Meta-analysis of the effect of Taijiquan on glucose metabolism in patients with dysglycemia. Journal of Shaanxi Normal University . 2019;47(3):38–47. doi: 10.15983/j.cnki. [DOI] [Google Scholar]
- 33.Chao M., Wang C., Dong X., Ding M. The effects of tai chi on type 2 diabetes mellitus: a meta-analysis. Journal of Diabetes Research . 2018;2018:9. doi: 10.1155/2018/7350567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee M. S., Jun J. H., Lim H. J., Lim H. S. A systematic review and meta-analysis of tai chi for treating type 2 diabetes. Maturitas . 2015;80(1):14–23. doi: 10.1016/j.maturitas.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 35.Guo S., Xu Y., Qin J., et al. Effect of tai chi on glycaemic control, lipid metabolism and body composition in adults with type 2 diabetes: a meta-analysis and systematic review. Journal of Rehabilitation Medicine . 2021;53(3, article jrm00165) doi: 10.2340/16501977-2799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xia T. W., Yang Y., Li W. H., Tang Z. H., Li Z. R., Qiao L. J. Different training durations and styles of tai chi for glucose control in patients with type 2 diabetes: a systematic review and meta-analysis of controlled trials. BMC Complementary and Alternative Medicine . 2019;19(1):p. 63. doi: 10.1186/s12906-019-2475-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhou Z., Zhou R., Li K., et al. Effects of tai chi on physiology, balance and quality of life in patients with type 2 diabetes: a systematic review and meta-analysis. Journal of Rehabilitation Medicine . 2019;51(6):405–417. doi: 10.2340/16501977-2555. [DOI] [PubMed] [Google Scholar]
- 38.Yao G., Chao Q., Xixi G., Yazhuo X. Meta analysis of the effect of Taijiquan on blood glucose and lipoprotein metabolism in patients with T2DM. Journal of Taishan Medical College . 2020;41(2):103–105. [Google Scholar]
- 39.Yongjin L., Bo D. Systematic review on effect of tai chi regarding to glucolipid metabolism and life quality of type 2 diabetes mellitus. Journal of Rehabilitation . 2017;27(4):55–59. doi: 10.3724/SP.J.1329.2017.04055. [DOI] [Google Scholar]
- 40.Qing T., Yujie G., Ping L. Meta analysis of the effect of shadowboxing on patients with type 2 diabetes mellitus. Modern Preventive Medicine . 2017;44(14):2516–2521. [Google Scholar]
- 41.Lebrun C. Exercise and type 2 diabetes: American College of Sports Medicine and the American Diabetes Association joint position statement. Diabetes Care . 2010;42:2692–2696. doi: 10.2337/dc10-1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lan C., Chen S. Y., Lai J. S., Wong A. M. Tai chi chuan in medicine and health promotion. Evidence-based Complementary and Alternative Medicine . 2013;2013 doi: 10.1155/2013/502131.502131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lavis J. N. How can we support the use of systematic reviews in policymaking? PLoS Medicine . 2009;6(11, article e1000141) doi: 10.1371/journal.pmed.1000141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stewart L., Moher D., Shekelle P. Why prospective registration of systematic reviews makes sense. Systematic Reviews . 2012;1(1):p. 7. doi: 10.1186/2046-4053-1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Powers S. K., Radak Z., Ji L. L. Exercise-induced oxidative stress: past, present and future. The Journal of Physiology . 2016;594(18):5081–5092. doi: 10.1113/JP270646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ji L. L. Redox signaling in skeletal muscle: role of aging and exercise. Advances in Physiology Education . 2015;39(4):352–359. doi: 10.1152/advan.00106.2014. [DOI] [PubMed] [Google Scholar]
- 47.Done A. J., Traustadóttir T. Nrf2 mediates redox adaptations to exercise. Redox Biology . 2016;10:191–199. doi: 10.1016/j.redox.2016.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang L., Muxin G., Nishida H., Shirakawa C., Sato S., Konishi T. Psychological stress-induced oxidative stress as a model of sub-healthy condition and the effect of TCM. Evidence-based Complementary and Alternative Medicine . 2007;4(2):195–202. doi: 10.1093/ecam/nel080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Martarelli D., Cocchioni M., Scuri S., Pompei P. Diaphragmatic breathing reduces exercise-induced oxidative stress. Evidence-based Complementary and Alternative Medicine . 2011;2011 doi: 10.1093/ecam/nep169.932430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen S. C., Ueng K. C., Lee S. H., Sun K. T., Lee M. C. Effect of t'ai chi exercise on biochemical profiles and oxidative stress indicators in obese patients with type 2 diabetes. Journal of Alternative and Complementary Medicine . 2010;16(11):1153–1159. doi: 10.1089/acm.2009.0560. [DOI] [PubMed] [Google Scholar]
- 51.Moher D., Hopewell S., Schulz K. F., et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. International Journal of Surgery . 2012;10(1):28–55. doi: 10.1016/j.ijsu.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 52.Liang Z., Chen X., Shi J., Hu H., Xue Y., Ung C. O. L. Efficacy and safety of traditional Chinese medicines for non-alcoholic fatty liver disease: a systematic literature review of randomized controlled trials. Chinese Medicine . 2021;16(1):p. 9. doi: 10.1186/s13020-020-00422-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed during the current study are available from the corresponding author on reasonable request.


