Summary
Background
The effect of different music interventions on depression in older adults is varied. We aimed to explore the comparative effect of different music intervention features on depression in older adults.
Methods
We searched PubMed, EMBASE, CENTRAL, CINAHL, and ProQuest Dissertations&Theses from inception to October 2021 for randomized controlled trials (RCTs) of music interventions in participants aged ≥60 years. Music interventions were classified based on the TIP (theme, intensity, and provider/platform) framework. The theme was divided into: 1) active music therapy (ACT); 2) receptive music therapy (Recep); and 3) music medicine (MM). The intensity was classified as high (>60 minutes/week), and low (≤60 minutes/week). The provider was classified as a music therapist (MT) or a non-music therapist (NonMT). Summary standardized mean differences (SMD) of level of depression with 95% confidence interval (CI) were estimated using a frequentist framework with a random-effects model. The certainty of evidence was evaluated using the Confidence in Network Meta-Analysis (CINeMA) approach. This study was registered with PROSPERO (CRD42021247165).
Findings
Fifteen RCTs involving 1,144 older adults (mean age 67.9-86.6 years) were included. When compared with usual care, the most effective music intervention was active music therapy >60 minutes/week by music therapist (Act/High/MT) (SMD -3.00; 95%CI, -3.64,-2.35), followed by music medicine >60 minutes/week by non-music therapist (MM/High/NonMT) (SMD -2.06; 95%CI, -2.78,-1.35) with moderate and high certainty of evidence, respectively. Depression scores in older adults treated with ACT/High/MT was also significantly lower than all other interventions, except MM/High/NonMT. Low intensity music interventions other than Act/Low/MT had no impact on depression.
Interpretation
Although active music therapy >60 minutes/week by music therapist is the most effective intervention to alleviate depression in older adults, music medicine by listening to music of older adult's own preference >60 minutes/week is an alternative approach in settings with limited resources.
Funding
None.
Keywords: Music intervention, Music therapy, Music medicine, Music listening, Depression, Older adults
Research in context.
Evidence before this study
Music interventions are one of the nonpharmacological approaches that has been shown to be effective in improving depression in the older adult population. Previous work suggests that music medicine (treatments that rely solely on the direct effects of music alone) exhibited a stronger effect in reducing depressive symptoms than music therapy (the use of music interventions to accomplish individualized goals within a therapeutic relationship by a credentialed professional). However, it is still inconclusive which is the most effective type of music intervention for depression and how to best deliver it, considering the variation in providing music interventions among the current literature.
Added value of this study
Our study used the theme, intensity, and provider/platform (TIP) framework to characterize different features of music therapy to overcome some of the limitations of prior studies, which lumped together music interventions with different features. To the best of our knowledge, our study is the first one that used a network meta-analysis approach on this topic, which showed that the provision of active music therapy >60 minutes/week by a music therapist was shown to be the most effective music therapy approach to reduce depression in older adults (moderate certainty of evidence). Music medicine by listening to music of older adult's own preference for >60 minutes per week should be considered as an alternative approach for settings with limited resources or which have no access to the service of a trained music therapist (high certainty of evidence). Although low intensity music interventions for ≤60 minutes per week by any specialty therapist had no impact on depression, active music therapy provided by a music therapist has been shown to improve depression in older adults. This finding supports the influential effect of a music therapist in providing active music therapy, even with low intensity.
Implications of all the available evidence
The advantage of music intervention is that it has less risk of causing serious side effects in the older adults as does the use of medication. Based on the comparative findings from the current evidence, we would suggest the use of active music therapy for >60 minutes per week by a music therapist to alleviate depression in the older adult population. Music medicine by listening to music of older adult's own preference for >60 minutes per week is an alternative approach for settings with limited resources or in settings that have no access to the services of a trained music therapist. Active music therapy for ≤60 minutes per week by a non-music therapist, or other low intensity music therapy by any specialty therapist were not different from usual care. To achieve the beneficial effects on depression in the older adult population, we suggest that the intensity of the music interventions should at least be increased to >60 minutes per week.
Alt-text: Unlabelled box
Introduction
At present, the life expectancy of the global population is increasing, and it is expected that the population of people aged 60 years or over will increase from 1 billion in 2020 to 2.1 billion by 2050.1 Depression is one of the most frequent mental health problems among older adults.2 Untreated depression has negative impacts on physical health, cognitive function, and quality of life.3 Although pharmacological interventions have proven to be effective and have been recommended in several clinical practice guidelines for depression,4 they are accompanied by unwanted side effects. Several non-pharmacological approaches, including music therapy, are shown to be effective in the treatment of older adults with depression.5
Although the term music therapy is widely used for music-based interventions, there are two main categories of music interventions, i.e. music therapy and music medicine. The American Music Therapy Association (AMTA) defines music therapy as “the clinical and evidence-based use of music interventions to accomplish individualized goals within a therapeutic relationship by a credentialed professional who has completed an approved music therapy program”.6 Further, music therapy is divided into two types based on musical interactions, i.e. active and receptive.7 In the active method, participants are ‘making music’ such as playing musical instruments, singing and improvising; in receptive music therapy, participants are ‘receiving’ (e.g. listening to) music. Interventions that rely solely on the direct effects of music alone, which do not depend upon a client-therapist relationship are called music medicine.8,9
Findings from previous systematic reviews have demonstrated the positive effect of music interventions on cognitive function10,11 and mental outcomes.12 The efficacy of music intervention on depression has also been explored using a meta-analysis approach in several population including patients with cancer,13,14 women with postpartum depression,15 adults receiving hemodialysis,16 and older adult population.2,5 Our study focused on the latter since older adults are accounted for a substantial group of population in the society who could benefit from music intervention. However, despite the existence of this evidence, which is the most effective type of music intervention for depression is still unclear. In addition, considering the variation in providing music interventions, there is a need for evidence to inform practice about how to best deliver this intervention. We conducted this study to address the aforementioned gap in knowledge with the specific objective to examine the comparative effect of different music intervention features on depression in older adults.
We employed the Theme, Intensity, and Provider/Platform (TIP) framework to characterize different features of music interventions. We developed the TIP framework and have used it in our previous works to synthesis evidence of health services interventions.17,18 In brief, we considered similar elements in health services interventions to be well matched with those of medication interventions that contribute to its effects. These elements are 1) “theme”, which is matched for active ingredient to specify the main element of the intervention; 2) “intensity”, which is the match for strength or concentration to indicate the strength of delivering the main element; and 3) “provider/platform”, which is the match for dosage form or route of administration to show how the main element is delivered. The latter two elements have taken into account ‘how’ to deliver the service.
Methods
We conducted this systematic review according to the Cochrane Collaboration guidelines for systematic reviews of interventions19 and following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension statement for reporting of systematic reviews incorporating network meta-analysis (NMA) of health care interventions.20 The protocol of this study was registered in PROSPERO (CRD42021247165) on 5 May 2021. After completing study selection step, we found a limited number of primary studies that meet our inclusion criteria. We then amended the protocol on 5 October for the following sections: 1) participants – changed from elderly with depression based on the geriatric depression scale (GDS) to participants aged 60 years or over; 2) outcome measures – to include measures for depression level other than GDS, and 3) searching – updated the search to October 2021 and removed OpenGrey database as ProQuest Dissertations & Theses is sufficient to cover grey literature.
Search strategy and selection criteria
We searched PubMed, EMBASE, Cochrane Central Register of clinical trials (CENTRAL), CINAHL and ProQuest Dissertations & Theses from inception of each database to December 2020 and updated in October 2021. Strategic search terms comprised three domains: 1) Older adults AND 2) Depression AND 3) Music therapy. A complete list of all search terms used, and search yields is available in Appendix 1. Previous systematic reviews related to music interventions for depression were used to identify potentially relevant studies that may not have been indexed in the above databases by scanning studies included in those systematic reviews.
Full articles of randomized controlled trials (RCTs) in the English language were included if they met the following criteria: 1) enrolled only participants aged 60 years or older; 2) explored the effects of one or more music interventions against usual care; and 3) measured level of depression using validated psychological scales. RCTs of music interventions as part of other non-pharmacological intervention were excluded.
Titles and abstracts of the identified publications were divided and independently screened by TD, TS, and NP. Full-text articles were independently reviewed by TD (all), TS and NP, who separately reviewed half of the articles. When disagreements regarding eligibility arose, they were resolved by discussions with the third reviewer (either NP or TS).
Data extraction was conducted by TD (all), TS and NP (who separately extracted half of the articles) using a data extraction form modified from the Cochrane Effective Practice and Organization of Care Group (EPOC) guideline.21
Classification of music interventions
Music interventions in the included trials were classified using the TIP framework. The theme was classified based on previous literature regards to the methods of music interventions,7, 8, 9 which are 1) active music therapy; 2) receptive music therapy; and 3) music medicine. The intensity of the music interventions was modified from findings from a previous systematic review that showed that both frequency (<3 times weekly) and duration per session (>60 minutes) affect depression outcome.22 Since some practices provide music intervention once a week, we decided to use this minimal frequency as a baseline and divided the intensity in our study into two groups based on the duration of the music interventions per week, i.e. high (>60 minutes/week), and low (≤60 minutes/week) intensity. According to the definition by AMTA,6 music therapy is the use of music by accredited professional for music therapy. We therefore classified the provider for the music interventions as a certified music therapist or a non-music therapist. The provider for music medicine is the person who prepared a pre-recorded list of songs to which the participant listened.
Data analysis
Included trials were independently assessed for methodological quality by TD (all), TS and NP, who separately assessed half of the articles using the EPOC risk of bias tool.21 This assessment tool evaluates bias in intervention studies based on sequence generation; adequacy of allocation concealment; comparative baseline outcome measurements and baseline provider characteristics; completeness of outcome data; blinding of outcome assessment; contamination minimization; and non-selective outcome reporting. The summary assessment of the risk of bias within a study was based on the risk of bias of key domains, which, in this study, were ‘comparative outcome measurements’, ‘completeness of outcome data’, and ‘adherence to intervention’. Each study was classified as being of low risk (low risk of bias for all key domains), high risk (high risk of bias for one or more key domains), or unclear risk (unclear risk of bias for one or more key domains). Disagreements between the reviewers were settled through discussion and consensus reached with the third reviewer (either TS or NP).
NMA comparing the effect of music interventions with usual care was conducted to estimate treatment effects and 95%confidence intervals (CI) using a random-effects model in the frequentist framework.23 Usual care was used as the common comparator in the NMA model. Both direct and indirect evidence were used in NMAs when direct comparisons between different types of self-care were available. Since the scale for each measure of depression level varies widely, we pooled data across different measures using the standardized mean difference (SMD). We conducted a sensitivity analysis by including only studies in patients with mild depression (as defined by the original trials). We also conducted another set of sensitivity analyses by comparing the effects on depression when music interventions were classified based on each of the TIP elements. Concomitant dementia was used as a criterion for a subgroup analysis.
We drew a network geometry to explore the comparative relationship among different features of music interventions and usual care. Global network inconsistency was assessed using a consistency-inconsistency model.24 Also, local inconsistency with all closed loops was evaluated using the node-splitting technique.24 Transitivity was explored by assessing the distribution of clinical and methodological variables that might affect the outcomes of interest. Publication bias was assessed using a comparison-adjusted funnel plot. In addition, the surface under the cumulative ranking (SUCRA)25,26 method in a Bayesian framework was used to hierarchically rank different features of music interventions to estimate the probability with which each treatment is best. All analyses were conducted using STATA 15 (College Station, TX).
The overall quality of evidence from this meta-analysis was evaluated according to the Confidence in Network Meta-Analysis (CINeMA) approach.27 Judgements across domains were summarized to obtain 4 levels of confidence for each relative treatment effect, i.e. very low, low, moderate, or high, which corresponds to the usual GRADE assessment.28
Role of the funding source
The authors received no specific funding for this research.
Results
Search results
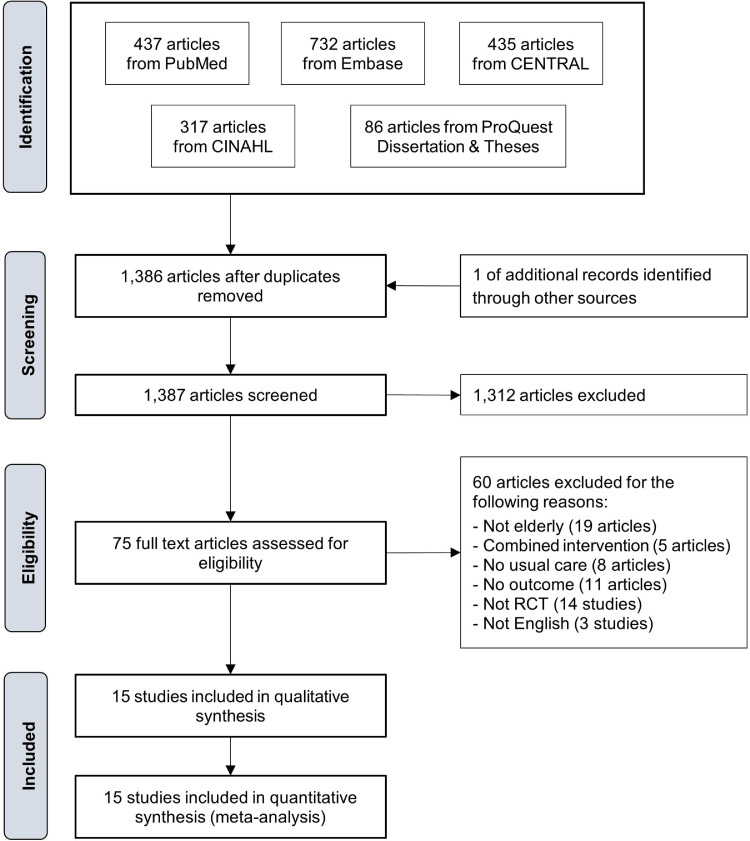
The search for published and grey literature yielded 1,386 articles after duplicates were removed (Figure 1). One additional trial was identified from references of previous relevant systematic reviews. Following title and abstract screening, 1,312 articles were removed. The remaining 75 articles underwent full text review for eligibility. A total of 15 trials29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43 met the inclusion criteria.
Figure 1.
PRISMA diagram.
Study characteristics
Nine of the fifteen trials were conducted in Asia, i.e. Hong Kong,29,30 Taiwan,31,36 Singapore,37,43 India,38 Japan,39 and Turkey33 (Table 1). The remaining six trials were conducted in Australia,42 France,34 Italy,41 Spain,40 UK,32 and the US.35 Four trials each were conducted in the older adult's homes30,34,35,43 and nursing homes.31,33,40,41 Other settings include: Day care centers,29,41 community singing clubs,32 veterans’ homes,36 a community research center,37 therapy room,39 and aged care facility.42 More than half (9 out of 15) of the included trials studied the effects of active music therapy,31,32,36,38, 39, 40, 41, 42, 43 whereas receptive music therapy and music medicine were studied in three33,35,37 and four trials,29,30,34,41 respectively. It should be noted that a trial by Raglio et al41 was a 3-arms RCT that studied the effects of active and receptive music therapy.
Table 1.
Characteristics of included studies.
| Study | Country | Setting | Sample size | Male (%) | Age (years) | Inclusion criteria | Exclusion criteria | Measure of depression | Baseline depression | Intervention period |
|---|---|---|---|---|---|---|---|---|---|---|
| Chan (2009)29 | Hong Kong | Day-care centers or homes | 50 | 44.7 | 75-79 years: 23% | Aged ≥60 years | NR | GDS | Int: 13.1 (5.2); Ctrl: 13.4 (4.4) | 4 |
| Chan (2010)30 | Hong Kong | Homes | 42 | 45.2 | 80+ years: 35.7% | Aged ≥60 years | Deaf; altered mental status; cognitive impairment; or had a recent death in the family | GDS-SF | Int: 4.1 (4.0); Ctrl: 1.8 (1.7) | 4 |
| Chu (2014)31 | Taiwan | Nursing homes | 100 | 47.0 | 82.0 (6.8) | Aged ≥60 years; diagnosis of dementia | Receptive language problem; inability to participate in an intervention for at least 30 min | C-CSDD | Int: 17.4 (9.6); Ctrl: 15.7 (10.2) | 6 |
| Coulton (2015)32 | UK | Community singing club | 258 | 16.1 | 69.2 (7.1) | Aged ≥60 years | Unable to provide informed consent | HADS | Int: 4.6 (3.5); Ctrl: 4.2 (3.5) | 14 |
| Gok Ugur (2017)33 | Turkey | Nursing homes | 64 | NR | 76.4 (NR) | People who had lived in a nursing home | Any visual or hearing loss | GDS-SF | Int: 8.1 (2.4); Ctrl: 8.5 (3.1) | 8 |
| Guetin (2009)34 | France | Homes | 30 | 26.7 | 86.1 (NR) | Aged 70-95 years; mild to moderate AD; MMSE score 12-25; HAS score ≥12 | Suffering from a life-threatening illness; neurological disorders, stroke PD, epilepsy, dementia; and psychiatric disorder | GDS | Int: 16.7 (6.2); Ctrl: 11.8 (7.4) | 16 |
| Hanser (1994)35 | US | Homes | 30 | 23.0 | 67.9 (NR) | Older adults; diagnosis of major or minor depression | NR | GDS | Int: 17.4 (6.7); Ctrl: 15.3 (5.8) | 8 |
| Liu (2021)36 | Taiwan | Veteran's homes | 50 | 100.0 | 86.6 (4.5) | Aged ≥75 years; mild to moderate AD; mild anxiety; receiving stable psychotropic or anxiolytic treatment for 3 months | NR | GDS-SF | Int: 4.7 (0.5); Ctrl: 4.7 (0.5) | 12 |
| Mahendran (2018)37 | Singapore | Community research center | 46 | 17.4 | 71.1 (NR) | Aged ≥75 years; mild cognitive impairment | Dementia/major neurocognitive disorder; major psychiatric disorder; terminal illness; visual and/or hearing impairment | GDS-SF | Int: 1.8 (2.2); Ctrl: 2.8 (2.9) | 36 |
| Mathew (2017)38 | India | Nursing homes | 80 | 50.0 | NR (all 65+) | Aged ≥65 years; GDS-SF score 5-8 | On anti-depressive medication, or other medications affecting sleep or mood disorders; hearing problems | GDS-SF | Int: 7.8 (1.1); Ctrl: 8.1 (0.9) | 3 |
| Murabayashi (2019)39 | Japan | Therapy rooms | 94 | 6.4 | 81.3 (5.5) | Aged 65-89 years; having one or more care needs regarding social withdrawal, dementia, or depression | NR | GDS-SF | NR | 12 |
| Perez-Ros (2019)40 | Spain | Nursing homes | 119 | 48.7 | 80.5 (7.4) | Aged ≥65 years; diagnosis of dementia | Terminally ill patients | CSDD | Int: 5.0 (4.5); Ctrl: 8.0 (5.9) | 8 |
| Raglio (2015)41 | Italy | Nursing homes and day care centers | 120 | 21.7 | 81.7 (NR) | Aged ≥65 years; diagnosis of dementia; MMSE ≤18 | Severe cardiovascular, pulmonary, or gastrointestinal disease | CSDD | Int 1: 9.0 (4.1); Int 2: 10.0 (4.8); Ctrl: 8.0 (6.7) | 10 |
| Robertson-Gillam (2008)42 | Australia | Aged care facility | 30 | 30.0 | 82.6 (5.8) | Resident of the aged care facility; diagnosis of dementia | NR | CSDD | Int: 10.5 (8.9); Ctrl: 8.9 (5.4) | 12 |
| Yap (2017)43 | Singapore | Homes | 31 | 6.0 | 74.6 (6.4) | Aged ≥65 years | On palliative care, bed-bound | CSDD-SF | Int: 3.5 (1.0, 6.0); † Ctrl: 6.0 (3.0, 8.0)† | 10 |
*Mean (standard deviation).
Interquartile range.
Abbreviations: AD=Alzheimer disease; C-CSDD=Chinese version of the Cornell Scale for Depression in Dementia; CSDD=Cornell Scale for Depression in Dementia; Ctrl=Control; GDS=Geriatric Depression Scale; GDS-SF= Geriatric Depression Scale Short Form; HADS=Hospital Anxiety and Depression Scale; HAS=Hamilton Anxiety Scale; Int=Intervention; MMSE=Mini Mental State Evaluation; NR=Not Reported.
A total of 1,144 older adults (31.8% male) participated in the 15 trials with the mean age ranging from 67.9 to 86.6 years. Six trials included patients with dementia (PWD),31,34,36,40, 41, 42 whilst the remaining trials did not measure and report dementia conditions among their participants. The majority of included trials (10 out of 15) were studied in older adults with mild depression (527 participants).29,30,33, 34, 35, 36,38,41, 42, 43 Three trials32,37,40 were studied in 423 older adults with an average normal level of depression; and one trial each were studied in older adults with major depression,31 and not reported baseline level of depression among participants.39
Detail of music interventions
The intervention protocol for active music therapy among the 9 trials varied and included singing,32,38,42 playing musical instruments or clapping hands,36,41,43 or a mix of singing and playing31,39,40 (Table 2). The choice of music compositions to listen in receptive music therapy was decided for each session based on participants’ emotional states.33,35 Participants in music medicine trials listened to music of their choosing before going to sleep,29 or in a comfortable and relaxed environment.30,34,41
Table 2.
Characteristics of music therapy interventions among included trials.
| Study | Music therapy |
Control | ||||
|---|---|---|---|---|---|---|
| Theme | Duration (interval) | Intensity (min/week) | Provider/platform | TIP Features | ||
| Chan (2009)29 | Music medicine: The music intervention consisted of a choice of four types of music, with each type played for approximately one 30-min session per week. The participants were encouraged to listen to the same type of music for 30 min every night before going to sleep. | 30 minutes (7/week) | 210 | Researcher | MM/High/NonMT | Participants were given an uninterrupted rest period. |
| Chan (2010)30 | Music medicine: The subjects were allowed to choose their preferred music. The researchers then asked the subjects to choose the most comfortable place to listen to the music, for example, in their bedroom. | 30 minutes (once a week) | 30 | Researcher | MM/Low/NonMT | Participants were given an uninterrupted rest period. |
| Chu (2014)31 | Active: A group music intervention with gross and fine motor movements performed to music, rhythm playing along with music, listening to popular music, rhythm playing with instrumental accompaniment, and singing with instrumental accompaniment. | 30 minutes (twice a week) | 60 | Music therapist | Act/Low/MT | Usual care activities involved watching television, afternoon tea, and taking walks. Participants were not exposed to other forms of therapy such as art therapy or tai chi. |
| Coulton (2015)32 | Active: The program was developmental, progressing from singing melody lines to harmonizing, layering and singing in rounds. | 90 minutes (once a week) | 90 | Trained facilitators | Act/High/NonMT | Participants continued with their normal activities. |
| Gok Ugur (2017)33 | Receptive: Music therapy sessions were held in the morning as an open group in a lounge of the nursing home with seating arrangement in the form of U shape. Sound and music system of the nursing home was used for the music therapy. During the music therapy sessions, older adults people were suggested to close their eyes and to imagine their happy memories. | 40 minutes (3/week) | 120 | Music therapist | Recep/High/MT | NR |
| Guetin (2009)34 | Music medicine: The patients were either in a supine position or seated in a comfortable armchair. They were also offered a mask so as to avoid visual stimuli, thus encouraging them to concentrate on the music. The style of music was chosen by a computer program and the standard musical sequence is broken down into several phases which gradually bring the patient into a state of relaxation according to the new ‘U sequence’ method. | 20 minutes (once a week) | 20 | Self-administered | MM/Low/NonMT | The patients took part in a different type of session (rest and reading), under the same conditions and at the same intervals. |
| Hanser (1994)35 | Receptive: Appropriate music was selected by the participants with the assistance of a music therapist to identify compositions which had been paired with meaningful memories. Participants were instructed to find some time each day when they could practice eight techniques* taught by the music therapist, who visit or call participants on a weekly basis. | Varies (7/week) | 185 | Music therapist | Recep/High/MT | Did not partake of therapy of any kind during the 8-week treatment period. |
| Liu (2021)36 | Active: Participants were asked to follow the instruction to play various kinds of percussion instruments (such as wrist bell, tambourine, maracas, triangle, double-tone woodblock, hand drum, castanet) by moving their upper extremities with their familiar songs. | 60 minutes (once a week) | 60 | Trained facilitators | Act/Low/NonMT | Patients participated in a rest and reading session, at the same intervals and under the same conditions. |
| Mahendran (2018)37 | Receptive: Listening, and recalling memories and experiences related to the music. The therapist prepared songs and used photographs or video clips to accompany the music, for discussion purposes. | 60 minutes (once a week) | 60 | Music therapist | Recep/Low/MT | Participants did not receive any intervention but continued life as usual. |
| Mathew (2017)38 | Active: Singing was initiated by the music therapist researcher and the subjects were encouraged to sing along and perform simple movements using hands depending on the theme. | 30 minutes (7/week) | 210 | Music therapist | Act/High/MT | Participants received no specific intervention. |
| Murabayashi (2019)39 | Active: The therapist initially played music to the participants and led them to join in. When participants sang and clapped their hands spontaneously at their own pitch and tempo, the therapists adjusted the pitch and tempo of the keyboard to match their playing and singing and accompanied their expressions. Small instruments of resonating sound were selected for instrumental activities to allow the participants to listen to their sounds connecting with others and to feel part of the group. | 50 minutes (once a week) | 50 | Music therapist | Act/Low/MT | NR |
| Perez-Ros (2019)40 | Active: A playlist of the preferred music was compiled. The music was played using an MP3 player and loudspeakers to all residents at once in the same room, allowing them to interact, sing, dance, clap, etc. | 60 minutes (5/week) | 300 | Nurses | Act/High/NonMT | Occupational therapy programs comprised training activities for maintaining the activities of daily living |
| Raglio (2015)41 | Active: Patient were presented with a similar group of instruments at each session and encouraged to pick them up and interact with them. The music therapist followed the patients’ rhythm and music production to create nonverbal communication. During the session, the music therapist built a relationship with the patients by singing and using melodic and rhythmic instruments (improvisation), facilitating the expression of the PWD's emotions and promoting “affect attunement” moments | 30 minutes (twice a week) | 60 | Music therapist | Act/Low/MT | Educational and occupational (e.g., reading the newspaper, playing cards, personal care) and physical (motor rehabilitation sessions) activities performed daily with the supervision of specialized professionals |
| Music medicine: the PWD listened to music from a preferred playlist without any interaction with a music therapist. The PWDs did not wear earphones and remained in their rooms or in a quiet, private place. The music therapist had created the playlists on the basis of interviews with the PWD and caregivers. | 30 minutes (twice a week) | 60 | Music therapist | MM/Low/MT | ||
| Robertson-Gillam (2008)42 | Active: The choir therapy began with a period of silence followed by relaxation; then vocal improvisation (individually and as a group); singing and speech exercises; learning new song material; and singing well-known songs. | 60 minutes (twice a week) | 120 | Researcher | Act/High/NonMT | Ordinary care |
| Yap (2017)43 | Active: The participant seated comfortably and the drum or percussion instrument within reach in front of them. The instructors facilitated free play and encouraged the participants to express themselves and interact with each other through the active playing of the instruments. | 60 minutes (once a week) | 60 | Experience instructor | Act/Low/NonMT | NR |
Intervention types: Act/High/MT, active music therapy >60 minutes/week by music therapist; Act/High/NonMT, active music therapy >60 minutes/week by non-music therapist; Act/Low/MT, active music therapy ≤60 minutes/week by music therapist; Act/Low/NonMT, active music therapy ≤60 minutes/week by non-music therapist; Recep/High/MT, receptive music therapy >60 minutes/week by music therapist; Recep/High/Self, Receptive music therapy >60 minutes/week by self-administration; Recep/Low/MT, receptive music therapy ≤60 minutes/week by music therapist; Recep/Low/Self, Receptive music therapy ≤60 minutes/week by self-administration.
Abbreviations: Act=Active; MT=Music therapist; NonMT=Non-music therapist; NR=Not reported; PWD=Patient with dementia; Recep=Receptive; Self=Self-administered; TIP=Theme, intensity, and provider or platform; *The eight techniques were: gentle exercise, facial massage, progressive muscle relaxation, guided imagery, special imagery, slow music to enhance falling asleep, rhythmic music to enhance energy, and music listening in conjunction with other activities to identify talents.
According to the characterization based on the TIP framework, there were 12 possible features of music interventions (Table 3). However, with three combinations of features missing from the current literature, there were a total of 9 music intervention features identified: 1) active music therapy >60 minutes/week by music therapist, ACT/High/MT (1 trial);38 2) active music therapy >60 minutes/week by non-music therapist, ACT/High/NonMT (3 trials);32,40,42 3) active music therapy ≤60 minutes/week by music therapist, ACT/Low/MT (3 trials);31,39,41 4) active music therapy ≤60 minutes/week by non-music therapist, ACT/Low/NonMT (2 trials);36,43 5) receptive music therapy >60 minutes/week by music therapist, Recep/High/MT (2 trials);33,35 6) receptive music therapy ≤60 minutes/week by music therapist, Recep/Low/MT (1 trial);37 7) music medicine >60 minutes/week with the song list prepared by non-music therapist, MM/High/NonMT (1 trial);29 8) music medicine ≤60 minutes/week with the song list prepared by music therapist, MM/Low/MT (1 trial);41 and 9) music medicine ≤60 minutes/week with the song list prepared by non-music therapist, MM/Low/NonMT (2 trials).30,34
Table 3.
Music therapy features according to theme, intensity, and provider (TIP).
| Theme | Intensity | Provider/Platform | Music therapy feature |
|---|---|---|---|
| Active music therapy: Participants are ‘making music’ (e.g. playing musical instruments, singing, and improvisation) and interacting with therapists | High: >60 minutes per week |
Music therapist |
Act/High/MT |
| Non-music therapist | Act/High/NonMT | ||
| Low: ≤60 minutes per week |
Music therapist |
Act/Low/MT |
|
| Non-music therapist | Act/Low/NonMT | ||
| Receptive music therapy: Participants are ‘receiving’ (e.g. listening to) music and interacting with therapists | High: >60 minutes per week |
Music therapist |
Recep/High/MT |
| Non-music therapist | Recep/High/NonMT | ||
| Low: ≤60 minutes per week |
Music therapist |
Recep/Low/MT |
|
| Non-music therapist | Recep/Low/NonMT | ||
| Music medicine: Participants are listening to music that had been prepared by therapist or at their own preference | High: >60 minutes per week |
Music therapist |
MM/High/MT |
| Non-music therapist | MM/High/NonMT | ||
| Low: ≤60 minutes per week |
Music therapist |
MM/Low/MT |
|
| Non-music therapist | MM/Low/NonMT | ||
Act=Active music therapy; MM=Music medicine; MT=Music therapist; NonMT=Non-music therapist; Recep=Receptive music therapy.
Usual care among the included trials were slightly varied, although three trials33,39,43 did not describe the details of usual care. Many of the remaining trials (6 out of 12)31,32,35,37,38,42 stated no specific interventions or allowed participants to continue their normal activities. Four trials had given participants uninterrupted rest periods,29,30 or rest and reading.32,36 The last two trials40,41 had employed occupational therapy programs with various activities.
Quality of included studies
Twelve trials29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39,42 reported no differences of baseline level of depression among intervention and control groups, whereas two trials41,43 failed to test the differences among studied groups and were justified as having unclear risk of bias. One trial40 reported difference in baseline depression among intervention and control groups and was rated as being of high risk of bias. Incomplete outcome data were identified in two trials42,43 and was not reported in one trial,36 which were then scored as being of high risk and unclear risk in this domain, respectively. The remaining 12 trials29, 30, 31, 32, 33, 34, 35,37, 38, 39, 40, 41 were rated as being of as being of low risk for the incomplete outcome data domain. Six trials29,31, 32, 33,35,40 clearly described the protocol to ensure that music therapy providers, including self-administration by participants, complied with the intervention protocol, whereas the other nine trials30,34,36, 37, 38, 39,41, 42, 43 did not report such a protocol and scored unclear risk of bias. Considering the risk of bias from the above three key domains, the overall risk of bias was low in 5 trials,29,31, 32, 33,35 unclear in 7 trials,30,34,36, 37, 38, 39,41 and high in 3 trials.40,42,43 Risks of bias for other non-key domains are presented in Appendix 2.
Effects on depression
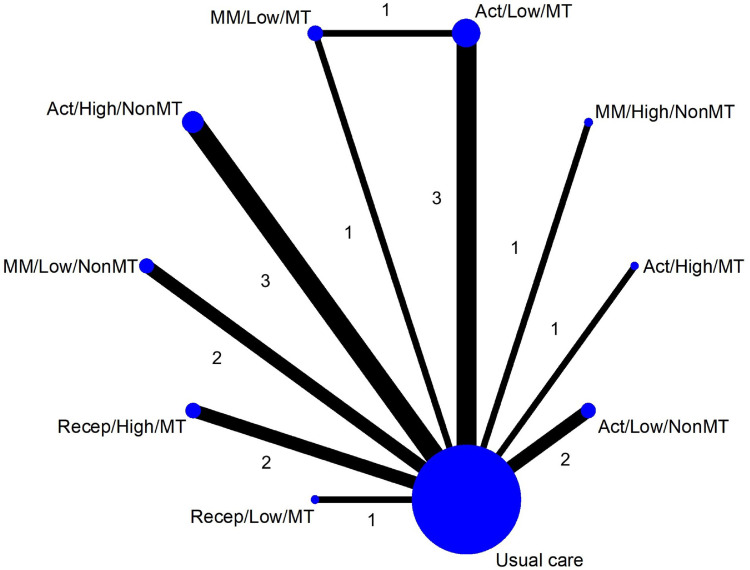
Nine different features of music interventions were used to establish a network geometry (Figure 2). The estimated effects on level of depression, based on direct and indirect comparisons of all treatment pairs, are presented as SMD [95%CI] in a league table (Table 4) and the SMD of each included trial is presented in Appendix 3. The level of depression of five music intervention features were significantly lower than usual care, with the highest estimated effects from ACT/High/MT (-3.00 [-3.64,-2.35]), followed by MM/High/NonMT (-2.06 [-2.78,-1.35]), Recep/High/MT (-0.75 [-1.18,-0.32]), Act/High/NonMT (-0.57 [-0.78,-0.36]), and Act/Low/MT (-0.42 [-0.67,-0.17]). The certainty of evidence was high for MM/High/NonMT and Recep/High/MT; and moderate for Act/High/MT, ACT/High/NonMT and ACT/Low/MT (Appendix 4).
Figure 2.
Network geometry of treatment comparisons of music therapy Intervention types: Act/High/MT, active music therapy >60 minutes/week by music therapist; Act/High/NonMT, active music therapy >60 minutes/week by non-music therapist; Act/Low/MT, active music therapy ≤60 minutes/week by music therapist; Act/Low/NonMT, active music therapy ≤60 minutes/week by non-music therapist; MM/High/NonMT, music medicine >60 minutes/week with the song lists prepared by non-music therapist; MM/Low/MT, music medicine ≤60 minutes/week with the song lists prepared by music therapist; MM/Low/NonMT, music medicine ≤60 minutes/week with the song lists prepared by non-music therapist; Recep/High/MT, receptive music therapy >60 minutes/week by music therapist; Recep/Low/MT, receptive music therapy ≤60 minutes/week by music therapist.
Abbreviations: Act=Active music therapy; MM=Music medicine; MT=Music therapist; NonMT=Non-music therapist; Recep=Receptive music therapy; The numerical values indicate the number of trials that provide evidence on particular treatment arms.
Table 4.
League table comparing effects of different features of music therapy.✝
| Act/High/MT | |||||||||
| -0.93 (-1.90,0.03) | MM/High/NonMT | ||||||||
| -2.25 (-3.02,-1.47)* | -1.31 (-2.15,-0.48)* | Recep/High/MT | |||||||
| -2.43 (-3.11,-1.75)* | -1.49 (-2.24,-0.74)* | -0.18 (-0.66,0.30) | Act/High/NonMT | ||||||
| -2.58 (-3.27,-1.89)* | -1.64 (-2.40,-0.88)* | -0.33 (-0.82,0.16) | -0.15 (-0.48,0.17) | Act/Low/MT | |||||
| -2.70 (-3.44,-1.96)* | -1.76 (-2.57,-0.96)* | -0.45 (-1.01,0.11) | -0.27 (-0.69,0.14) | -0.12 (-0.55,0.32) | Act/Low/NonMT | ||||
| -2.84 (-3.63,-2.06)* | -1.91 (-2.75,-1.07)* | -0.60 (-1.21,0.01) | -0.42 (-0.90,0.07) | -0.27 (-0.71,0.18) | -0.15 (-0.71,0.42) | MM/Low/MT | |||
| -2.83 (-3.63,-2.04)* | -1.90 (-2.75,-1.04)* | -0.59 (-1.22,0.05) | -0.41 (-0.92,0.10) | -0.25 (-0.78,0.27) | -0.13 (-0.72,0.45) | 0.01 (-0.63,0.65) | MM/Low/NonMT | ||
| -2.75 (-3.65,-1.86)* | -1.82 (-2.77,-0.87)* | -0.50 (-1.26,0.25) | -0.33 (-0.98,0.33) | -0.17 (-0.84,0.49) | -0.05 (-0.77,0.66) | 0.09 (-0.66,0.85) | 0.08 (-0.69,0.86) | Recep/Low/MT | |
| -3.00 (-3.64,-2.35)* | -2.06 (-2.78,-1.35)* | -0.75 (-1.18,-0.32)* | -0.57 (-0.78,-0.36)* | -0.42 (-0.67,-0.17)* | -0.30 (-0.66,0.06) | -0.15 (-0.59,0.29) | -0.17 (-0.63,0.30) | -0.25 (-0.87,0.37) | Usual care |
Intervention types: Act/High/MT, active music therapy >60 minutes/week by music therapist; Act/High/NonMT, active music therapy >60 minutes/week by non-music therapist; Act/Low/MT, active music therapy ≤60 minutes/week by music therapist; Act/Low/NonMT, active music therapy ≤60 minutes/week by non-music therapist; MM/High/NonMT, music medicine >60 minutes/week with the song lists prepared by non-music therapist; MM/Low/MT, music medicine ≤60 minutes/week with the song lists prepared by music therapist; MM/Low/NonMT, music medicine ≤60 minutes/week with the song lists prepared by non-music therapist; Recep/High/MT, receptive music therapy >60 minutes/week by music therapist; Recep/Low/MT, receptive music therapy ≤60 minutes/week by music therapist.
Abbreviations: Act=Active music therapy; MM=Music medicine; MT=Music therapist; NonMT=Non-music therapist; Recep=Receptive music therapy.
Statistically significant.
The value in each cell indicates the standardized mean difference (95% confidence interval) between treatment pair.
We have also conducted further analysis by using a mean difference (MD) to aid interpretation of our findings on the same scale. Of the five tools that were used among the 15 included trials, GDS15 was the most reported outcome with the scale range from 0 (normal) to 15 (severe depression). The MD [95%CI] of the following three out of six music intervention features from 7 trials were significantly lower than usual care: ACT/High/MT (-2.22 [-2.67,-1.77]); Recep/High/MT (-1.97 [-3.36,-0.58]); and Act/Low/MT (-1.47 [-2.94,-0.00]).
In addition, ACT/High/MT was also shown to be significantly associated with lower depression score when compared with all other music interventions, except MM/High/NonMT, with moderate certainty of evidence for 7 comparisons and low certainty for 1 comparison. The level of depression in older adults treated with MM/High/NonMT was also significantly lower than those receiving other features of music interventions, except Act/High/MT. The certainty of evidence of the positive effects of MM/High/NonMT on depression compared with other music interventions was rated as high for 3 comparison pairs and moderate for 4 comparison pairs.
Significant differences in the level of depression were not observed among other 26 comparison pairs. The overall certainty of evidence of these comparisons was judged as low for 25 comparisons, and very low for 1 comparison. Evidence levels were most often downgraded for imprecision and within-study bias. Findings of the cumulative probability of being the best intervention from the SUCRA coincided with the above findings as Act/High/MT revealed the highest probability of 99.7%, followed by MM/High/NonMT (89.2%) and Recep/High/MT (71.9%) (Appendix 5).
No inconsistency between direct and indirect evidence was observed in both the node splitting test (p=0.126, and p=0.126), and the global inconsistency test (chi2=2.34, p=0.1259). Intransitivity, based on the distributions of the proportion of patients with dementia and intervention duration, was observed in a limited number of treatment comparisons (Appendix 6). Publication bias was not evident according to the symmetry comparison-adjusted funnel plot (Appendix 7).
Sensitivity analysis
A sensitivity analysis of ten trials in older adults with mild depression confirmed the robustness of the main analysis as it showed consistent findings that ACT/High/MT provided the highest estimated effect of -3.00 [-3.64, -2.35] with a SUCRA of 99.6%; followed by MM/High/NonMT with an SMD of -2.06 [-2.78, -1.35]) and 87.8% SUCRA; and Recep/High/MT (-0.75 [-1.18, -0.32]) with a 70.7% SUCRA.
When music interventions were classified based solely on the ‘Theme’ element, only active music therapy was shown to reduce depression when compared with usual care (-0.71 [-1.22, -0.20]), whereas music medicine (-0.64, [-1.42, 0.13]) and receptive music therapy (-0.60 [-1.52, 0.33]) showed no significant difference from usual care (Appendix 8). High intensity music intervention, irrespective of the theme and provider, was shown to dominate with an SMD of -0.87 [-1.55, -0.19] and -1.22 [-1.76, -0.68] when compared to low intensity and usual care. This was supported by a substantial SUCRA of 99.7% for high intensity compared to 47.7% for low intensity music interventions. When music interventions were classified based only on the ‘Provider’ element, both music and non-music therapists were shown to alleviate depression when compared to usual care. However, the effect on depression from interventions provided by a music therapist appeared to be relatively larger than by a non-music therapist, with SMD of -0.82 [-1.40, -0.24] and -0.56 [-1.11, -0.02], respectively.
Subgroup analysis: dementia condition
Of the 15 included trials, six (449 participants)31,34,36,40, 41, 42 studied in PWD which involved five different music intervention features, i.e. ACT/High/NonMT, ACT/Low/MT, ACT/Low/NonMT, MM/Low/MT, and MM/Low/NonMT (Appendix 9). No music intervention features showed a lower depression level when compared with usual care. Similar to the main analysis, findings of the remaining 9 trials (695 participants)29,30,32,33,35,37, 38, 39,43 that studied in older adults without dementia found that ACT/High/MT and MM/High/NonMT were associated with lower depression scores when compared with usual care with an SMD [95%CI] of -3.00 [-3.64,-2.35] and -2.06 [-2.78,-1.35], respectively.
Discussion
According to the comparative findings from current evidence, the provision of active music therapy >60 minutes/week by a music therapist was shown to be the most effective music intervention feature to reduce depression in older adults. The second effective approach was music medicine, provided for >60 minutes/week. The certainty of evidence was high to moderate certainty when compared with other music intervention features. The findings of our study also suggest that the provision of active music therapy by a non-music therapist or other types of music interventions by any therapists were not significantly different from usual care in reducing depression scores in the older adult population if the intervention intensity is ≤60 minutes per week.
Our study overcomes some of the limitations of prior studies, which lumped together music interventions with different features. Although such an approach provides useful evidence about the effect of music interventions, the implications of applying to practice is relatively limited, as healthcare providers would have insufficient information about which is the most effective type of music interventions and how to deliver such intervention to achieve the best outcome.
Among previous systematic reviews of music interventions on depression, only a few explored the effects of different types of music therapy. Two meta-analyses8,22 that undertook sub-group analyses of music therapy and music medicine showed that music medicine exhibited a stronger effect in reducing depressive symptoms than music therapy. However, a study by Tang et al. acknowledged that music intervention methods and the characters of music interventions were associated with the therapeutic effect.22
Although there are several possible categorization options, our study intended to explore what is the most effective intervention and how to best deliver such intervention at the same time. We are convinced that using the TIP framework to characterize different features of music intervention based on theme, intensity, and provider/platform has suited the study's objective since it allowed us to take these elements into account in a combined fashion. In contrast with findings from previous studies,8,22 when the intensity and provider were matched (high intensity provided by a music therapist), we found a stronger effect of active music therapy than music medicine and receptive music therapy in reducing the level of depression.
The superior effect of active music therapy on depression seems to be multifactorial, which is possibly due to its active form that helps to connect participants with a therapist or other people and to express difficult feelings. A specific method of active music therapy such as singing has been shown to improve emotional status as well as immunity,44 well-being, physical and physiological performance,45 and quality of life.46 It has been suggested that the use of musical instruments provides opportunities for the expression of emotions among participants, induces positive mood states, and improves psychological and physical quality of life.47
Unlike simply listening to music as in music medicine, receptive music therapy involves an interaction with therapist to decide appropriate music for individual clients together with a variety of approaches during music listening such as recalling memories and experiences related to music and special imagery related to music. However, the higher effect of music medicine over receptive music therapy identified in this study suggests that the therapeutic effect of music medicine is mainly the result of music, not the direct interaction with the therapist. Further head-to-head trials comparing music medicine and receptive music therapy are warranted to confirm our findings of an indirect comparison.
When music medicine was matched with receptive music therapy for the same ‘high’ intensity, larger effect size and SUCRA was still observed in music medicine even without the therapeutic role from music therapist. Of note is that despite being classified as ‘high’ intensity, the actual time that older adults listen to music in the trial on music medicine (210 minutes/week)29 seems higher than the time in the trials on receptive music therapy (ranged from 120-195 minutes/week).33,35 This suggests a dose-response relationship and coincides with findings from a previous meta-analysis, which showed that the effects of music therapy are related to the number of sessions provided.9 A meta-analysis by Tang et al also suggested that music therapy with more time per session may yield stronger therapeutic effect on depression.22 Results in our study support these previous findings that high intensity music interventions are associated with higher effect estimates when compared with low intensity music therapy and music medicine. Our findings also add further information regarding the effect of intensity that active music therapy by a non-music therapist, receptive music therapy, and music medicine for ≤60 minutes/week were not significantly different from usual care.
The provision of active music therapy by music therapist, who is an expert in the field, enables participants to engage in several music activities that are specifically designed to target individuals needs and capabilities. The influential effect of a music therapist was evidenced in our study when other elements of music interventions in the TIP framework were matched. Specifically, low intensity active music therapy can significantly reduce depression scores when it is provided by a music therapist, whereas the provision by a non-music therapist showed no significant difference from usual care.
A previous network meta-analysis of non-pharmacological interventions for older adults by Chen et al5 reported that the effect of music intervention to improve depressive symptoms (mean difference, MD 2.6; 95% credible interval, CrI 0.84, 4.35) was higher than other non-pharmacological interventions such as life review (MD 1.92; 95%CrI 0.71, 3.14), cognitive behavioral therapy (MD 1.27; 95%CrI 0.23, 2.38), aerobic (MD 1.84; 95%CrI 0.39, 3.36) and resistance training (MD 1.72; 95%CrI 0.06, 3.42). However, the finding in Chen et al study was only derived from 5 trials of music interventions and used a lumping approach to group music intervention with different features together. It is worth to explore further if comparative findings of music and other non-pharmacological interventions would alter if music interventions were characterize based on the TIP framework. The interpretation of subgroup analyses based on dementia condition is challenging due to a small number of trials in each group to enable a direct assessment between subgroups of the same treatment pairs. However, based on the limited evidence, none of the studied music interventions have influential effects on depression in patients with dementia. This may partly due to the fact that there is a high prevalence of depression in patients with dementia.48 Of note is that our finding was different from a previous systematic review, which showed that music therapy significantly improved depression in patients with dementia.49 It is plausible that the previous review may have possessed higher power to detect the differences as all music interventions were lumped into one intervention and compared to usual care. Also, evidence had emphasized the positive effects of music on the brain in various aspects including learning attention,50 emotion and cognition, and as provoking sensation and pleasure.51 In patients with dementia, music intervention has been shown to improve disruptive behavior,10 and cognitive function.52 Further trials on the effective music intervention features found in this study, such as high intensity music therapy by a music therapist and high intensity music medicine, should be conducted in older adults with dementia to identify the appropriate music interventions that improve not only depression, but also other dementia-related outcomes such as cognitive function, and behavioral and psychological symptoms in this group of participant.
Although the TIP framework allows us to characterize music interventions into groups with similar features, it should be noted that there are several possible categorizations based on the criteria being used. It is plausible that findings may be different if the criteria for characterization is changed, such as altering the cut-off point for intensity from 60 minutes per week to other thresholds. The limited number of trials in some treatment nodes and the shortage of direct evidence of head-to-head trials of different music interventions, together with the small number of participants in each trial, may have an impact on the variation of the effect estimates. However, this is not the case in our study as we can still observe consistent significant effects of certain music interventions. Another limitation is that we had to perform a meta-analysis using SMD since the included trials used different tools to measure the level of depression. The pooled estimate was difficult to interpret because it was reported in the unit of standard deviation rather than that of measurement scales. Nevertheless, the use of SMD was the only valid approach in our study to pool findings with various measurement scales. Since intransitivity was observed among treatment pairs, we suggest our findings should be interpreted with caution. The overall unclear and high risk of bias among the majority of included trials has also affected the certainty of evidence, which could be improved with the conduct of further well design studies in this field. Although we did not set restriction criteria for participant characteristics, the evidence generated in this study cannot apply to older adults in critical ill conditions or those with psychiatric problems since the current available trials did not cover these populations. Last, there were still variations in the intervention protocols even within the same music therapy method. However, it would be impossible to have identical music interventions among the current literature. We therefore believe that it is sensible to classify the theme of music interventions based on the interaction with music as active music therapy, receptive music therapy, and music medicine.
High intensity music medicine by older adult's own preference has shown to be the second most effective feature of music intervention. Therefore, it is reasonable to consider this as an alternative approach in settings with limited resources since it demands less intense economic and opportunity cost. However, further economic evaluation for this music intervention would be helpful as supportive evidence for this recommendation. Findings from our study serve as evidence for one of the non-pharmacological managements for depression. On area worthy of further exploration is to compare effects of other types of interventions in depression such as pharmacological vs non-pharmacological interventions. Based on the TIP framework, not all the 12 possible features of music interventions were identified from the current literature. This is due to a limited number of trials in the field. There is a need for more clinical studies to strengthen findings from our studies, specifically, to explore the effects of other music intervention features as well as to provide direct evidence of head-to-head comparisons of different music interventions.
Considering the variation of music interventions, our study has sought to identify the most effective intervention and how to best deliver it to alleviate depression in the older adult population. The use of the TIP framework enables us to characterize and compare different features of music interventions. Findings based on the current literature suggest that active music therapy for >60 minutes per week by a music therapist is the most effective music intervention in improving depression in the older adult population. The evidence also suggests that low intensity, active music therapy for ≤60 minutes per week by a non-music therapist, or other music interventions by any specialty therapist had no impact on depression. For settings with limited resources or those that have no access to the services of a trained music therapist, music medicine by listening to music of older adult's own preference for >60 minutes per week should be considered as an alternative approach. If a music intervention is deemed appropriate for older adults, we encourage clinician and caregivers to consider our findings when deciding music interventions protocol to achieve the best outcome on depression.
Contributors
TD updated the search, undertook study selection, data extraction, quality assessment, and data analysis. TS and NP performed the original search and divided the task to undertook study selection, data extraction, and quality assessment. TD wrote the first draft of the manuscript with TT, NC and BD. All authors revised and approved the final version of the manuscript. All authors had full access to all the data in the study. TD and TS have accessed and verified the data.
Data sharing statement
Extracted data are available on request to the corresponding author.
Declaration of interests
All authors have declared no conflict of interest.
Funding
None.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2022.101509.
Appendix. Supplementary materials
References
- 1.World Health Organization . World Health Organization; Geneva: 2021. Ageing and Health [Internet], 2021.https://www.who.int/news-room/fact-sheets/detail/ageing-and-health [cited 2021 Oct 30]; Available from: [Google Scholar]
- 2.Zhao K, Bai ZG, Bo A, Chi I. A systematic review and meta-analysis of music therapy for the older adults with depression. Int J Geriatr Psychiatry. 2016;31:1188–1198. doi: 10.1002/gps.4494. [DOI] [PubMed] [Google Scholar]
- 3.Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annu Rev Clin Psychol. 2009;5:363–389. doi: 10.1146/annurev.clinpsy.032408.153621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gabriel FC, de Melo DO, Fráguas R, Leite-Santos NC, Mantovani da Silva RA, Ribeiro E. Pharmacological treatment of depression: a systematic review comparing clinical practice guideline recommendations. PLoS One. 2020;15 doi: 10.1371/journal.pone.0231700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen YJ, Li XX, Pan B, et al. Non-pharmacological interventions for older adults with depressive symptoms: a network meta-analysis of 35 randomized controlled trials. Aging Ment Health. 2021;25:773–786. doi: 10.1080/13607863.2019.1704219. [DOI] [PubMed] [Google Scholar]
- 6.American Music Therapy Association. American music therapy association standards of clinical practice [Internet]. Silver Spring (MD): American music therapy association. 2015. 2021 [cited 2021 Nov 11]; Available from: https://www.musictherapy.org/about/standards/
- 7.Aalbers S, Fusar-Poli L, Freeman RE, et al. Cochrane Database of Systematic Reviews. 2017. Music therapy for depression. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bradt J, Dileo C, Myers-Coffman K, Biondo J. Music interventions for improving psychological and physical outcomes in people with cancer. Cochrane Database Syst Rev. 2021;10 doi: 10.1002/14651858.CD006911.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gold C, Solli HP, Krüger V, Lie SA. Dose-response relationship in music therapy for people with serious mental disorders: systematic review and meta-analysis. Clin Psychol Rev. 2009;29:193–207. doi: 10.1016/j.cpr.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 10.Zhang Y, Cai J, An L, et al. Does music therapy enhance behavioral and cognitive function in elderly dementia patients? A systematic review and meta-analysis. Ageing Res Rev. 2017;35:1–11. doi: 10.1016/j.arr.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 11.Dorris JL, Neely S, Terhorst L, VonVille HM, Rodakowski J. Effects of music participation for mild cognitive impairment and dementia: A systematic review and meta-analysis. J Am Geriatr Soc. 2021;69:2659–2667. doi: 10.1111/jgs.17208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mileski M, Brooks M, Kirsch A, Lee F, LeVieux A, Ruiz A. Positive physical and mental outcomes for residents in nursing facilities using music: a systematic review. Clin Interv Aging. 2019;14:301–319. doi: 10.2147/CIA.S189486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nguyen KT, Xiao J, Chan DNS, Zhang M, Chan CWH. Effects of music intervention on anxiety, depression, and quality of life of cancer patients receiving chemotherapy: a systematic review and meta-analysis. Support Care Cancer. 2022 doi: 10.1007/s00520-022-06881-2. [DOI] [PubMed] [Google Scholar]
- 14.Tsai HF, Chen YR, Chung MH, et al. Effectiveness of music intervention in ameliorating cancer patients' anxiety, depression, pain, and fatigue: a meta-analysis. Cancer Nurs. 2014;37:E35–E50. doi: 10.1097/NCC.0000000000000116. [DOI] [PubMed] [Google Scholar]
- 15.Yang WJ, Bai YM, Qin L, et al. The effectiveness of music therapy for postpartum depression: a systematic review and meta-analysis. Complement Ther Clin Pract. 2019;37:93–101. doi: 10.1016/j.ctcp.2019.09.002. [DOI] [PubMed] [Google Scholar]
- 16.Yangöz Ş T, Özer Z. Effects of music intervention on physical and psychological problems in adults receiving haemodialysis treatment: a systematic review and meta-analysis. J Clin Nurs. 2022 doi: 10.1111/jocn.16199. [DOI] [PubMed] [Google Scholar]
- 17.Dhippayom T, Boonpattharatthiti K, Thammathuros T, Dilokthornsakul P, Sakunrag I, Devine B. Clinical outcomes of different warfarin self-care strategies: a systematic reviews and network meta-analysis. J Thromb Haemost. 2021 doi: 10.1055/a-1677-9608. [DOI] [PubMed] [Google Scholar]
- 18.Dhippayom T, Wateemongkollert A, Mueangfa K, Im H, Dilokthornsakul P, Devine B. Comparative efficacy of strategies to support self-management in patients with asthma: a systematic review and network meta-analysis. J Allergy Clin Immunol Pract. 2021 doi: 10.1016/j.jaip.2021.09.049. [DOI] [PubMed] [Google Scholar]
- 19.Higgins JPT, Green S. The Cochrane Collaboration. 2011. Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]www.cochrane-handbook.orb editors. Available from: [Google Scholar]
- 20.Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–784. doi: 10.7326/M14-2385. [DOI] [PubMed] [Google Scholar]
- 21.Cochrane Effective Practice and Organisation of Care. Summary assessments of the risk of bias. EPOC resources for review authors [Internet]. c 2020. [cited 2020 Oct 15]; Available from: https://epoc.cochrane.org/resources/epoc-resources-review-authors
- 22.Tang Q, Huang Z, Zhou H, Ye P. Effects of music therapy on depression: a meta-analysis of randomized controlled trials. PLoS One. 2020;15 doi: 10.1371/journal.pone.0240862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.White IR. Network Meta-analysis. The Stata Journal. 2015;15:951–985. [Google Scholar]
- 24.Dias S, Welton NJ, Caldwell DM. Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med. 2010;29:932–944. doi: 10.1002/sim.3767. [DOI] [PubMed] [Google Scholar]
- 25.Salanti G. Indirect and mixed-treatment comparison, network, or multiple-treatments meta-analysis: many names, many benefits, many concerns for the next generation evidence synthesis tool. Res Synth Methods. 2012;3:80–97. doi: 10.1002/jrsm.1037. [DOI] [PubMed] [Google Scholar]
- 26.Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G. Graphical tools for network meta-analysis in STATA. PLoS One. 2013;8:e76654. doi: 10.1371/journal.pone.0076654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nikolakopoulou A, Higgins JPT, Papakonstantinou T, et al. CINeMA: An approach for assessing confidence in the results of a network meta-analysis. PLoS Med. 2020;17 doi: 10.1371/journal.pmed.1003082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Puhan MA, Schünemann HJ, Murad MH, et al. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ: British Medical Journal. 2014;349:g5630. doi: 10.1136/bmj.g5630. [DOI] [PubMed] [Google Scholar]
- 29.Chan MF, Chan EA, Mok E, Kwan Tse FY. Effect of music on depression levels and physiological responses in community-based older adults. Int J Ment Health Nurs. 2009;18:285–294. doi: 10.1111/j.1447-0349.2009.00614.x. [DOI] [PubMed] [Google Scholar]
- 30.Chan MF, Chan EA, Mok E. Effects of music on depression and sleep quality in elderly people: A randomised controlled trial. Complement Ther Med. 2010;18:150–159. doi: 10.1016/j.ctim.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 31.Chu H, Yang CY, Lin Y, et al. The impact of group music therapy on depression and cognition in elderly persons with dementia: a randomized controlled study. Biological Res Nurs. 2014;16:209–217. doi: 10.1177/1099800413485410. [DOI] [PubMed] [Google Scholar]
- 32.Coulton S, Clift S, Skingley A, Rodriguez J. Effectiveness and cost-effectiveness of community singing on mental health-related quality of life of older people: randomised controlled trial. Br J Psychiatry. 2015;207:250–255. doi: 10.1192/bjp.bp.113.129908. [DOI] [PubMed] [Google Scholar]
- 33.H Gök Ugur, Y Yaman Aktaş, Orak OS, Saglambilen O, İ Aydin Avci. The effect of music therapy on depression and physiological parameters in elderly people living in a Turkish nursing home: a randomized-controlled trial. Aging Ment Health. 2017;21:1280–1286. doi: 10.1080/13607863.2016.1222348. [DOI] [PubMed] [Google Scholar]
- 34.Guétin S, Portet F, Picot MC, et al. Effect of music therapy on anxiety and depression in patients with Alzheimer's type dementia: randomised, controlled study. Dement Geriatric Cognitive Disord. 2009;28:36–46. doi: 10.1159/000229024. [DOI] [PubMed] [Google Scholar]
- 35.Hanser SB, Thompson LW. Effects of a music therapy strategy on depressed older adults. J Gerontol. 1994;49:P265–P269. doi: 10.1093/geronj/49.6.p265. [DOI] [PubMed] [Google Scholar]
- 36.Liu MN, Liou YJ, Wang WC, et al. Group music intervention using percussion instruments to reduce anxiety among elderly male veterans with alzheimer disease. Med Sci Monit. 2021;27 doi: 10.12659/MSM.928714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mahendran R, Gandhi M, Moorakonda RB, et al. Art therapy is associated with sustained improvement in cognitive function in the elderly with mild neurocognitive disorder: findings from a pilot randomized controlled trial for art therapy and music reminiscence activity versus usual care. Trials. 2018;19:615. doi: 10.1186/s13063-018-2988-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mathew D, Sundar S, Subramaniam E, Parmar P. Music therapy as group singing improves Geriatric Depression Scale score and loneliness in institutionalized geriatric adults with mild depression: a randomized controlled study. Int J Educ Psychol Res. 2017;3:6–10. [Google Scholar]
- 39.Murabayashi N, Akahoshi T, Ishimine R, Saji N, Takeda C, Nakayama H, et al. Effects of music therapy in frail elderlies: controlled crossover study. Dementia and Geriatric Cognitive Disorders Extra. 2019:87-99.
- 40.Pérez-Ros P, Cubero-Plazas L, Mejías-Serrano T, Cunha C, Martínez-Arnau FM. Preferred music listening intervention in nursing home residents with cognitive impairment: a randomized intervention study. J Alzheimers Dis. 2019;70:433–442. doi: 10.3233/JAD-190361. [DOI] [PubMed] [Google Scholar]
- 41.Raglio A, Bellandi D, Baiardi P, et al. Effect of active music therapy and individualized listening to music on dementia: a multicenter randomized controlled trial. J Am Geriatrics Soc. 2015;63:1534–1539. doi: 10.1111/jgs.13558. [DOI] [PubMed] [Google Scholar]
- 42.Robertson-Gillam K. University of Western Sydney (Australia); 2008. The Effects of Singing in a Choir Compared with Participating in a Reminiscence Group on Reducing Depression in People with Dementia [M.A.]. [Ann Arbor] p. 147. [Google Scholar]
- 43.Yap AF, Yu Heng K, Chuen Seng T, Ibrahim S. Seng Bin A. Rhythm-centred music making in community living elderly: a randomized pilot study. BMC Complement Alternat Med. 2017;17:1–8. doi: 10.1186/s12906-017-1825-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kreutz G, Bongard S, Rohrmann S, Hodapp V, Grebe D. Effects of choir singing or listening on secretory immunoglobulin A, cortisol, and emotional state. J Behav Med. 2004;27:623–635. doi: 10.1007/s10865-004-0006-9. [DOI] [PubMed] [Google Scholar]
- 45.Moss H, Lynch J, O'Donoghue J. Exploring the perceived health benefits of singing in a choir: an international cross-sectional mixed-methods study. Perspect Public Health. 2018;138:160–168. doi: 10.1177/1757913917739652. [DOI] [PubMed] [Google Scholar]
- 46.Johnson JK, Louhivuori J, Stewart AL, Tolvanen A, Ross L, Era P. Quality of life (QOL) of older adult community choral singers in Finland. Int Psychogeriatr. 2013;25:1055–1064. doi: 10.1017/S1041610213000422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Seinfeld S, Figueroa H, Ortiz-Gil J, Sanchez-Vives MV. Effects of music learning and piano practice on cognitive function, mood and quality of life in older adults. Front Psychol. 2013;4:810. doi: 10.3389/fpsyg.2013.00810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bennett S, Thomas AJ. Depression and dementia: cause, consequence or coincidence? Maturitas. 2014;79:184–190. doi: 10.1016/j.maturitas.2014.05.009. [DOI] [PubMed] [Google Scholar]
- 49.Li HC, Wang HH, Lu CY, Chen TB, Lin YH, Lee I. The effect of music therapy on reducing depression in people with dementia: a systematic review and meta-analysis. Geriatr Nurs. 2019;40:510–516. doi: 10.1016/j.gerinurse.2019.03.017. [DOI] [PubMed] [Google Scholar]
- 50.Román-Caballero R, Arnedo M, Triviño M, Lupiáñez J. Musical practice as an enhancer of cognitive function in healthy aging - a systematic review and meta-analysis. PLoS One. 2018;13 doi: 10.1371/journal.pone.0207957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Moreno-Morales C, Calero R, Moreno-Morales P, Pintado C. Music therapy in the treatment of dementia: a systematic review and meta-analysis. Front Med (Lausanne) 2020;7:160. doi: 10.3389/fmed.2020.00160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bian X, Wang Y, Zhao X, Zhang Z, Ding C. Does music therapy affect the global cognitive function of patients with dementia? A meta-analysis. NeuroRehabilitation. 2021;48:553–562. doi: 10.3233/NRE-210018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.