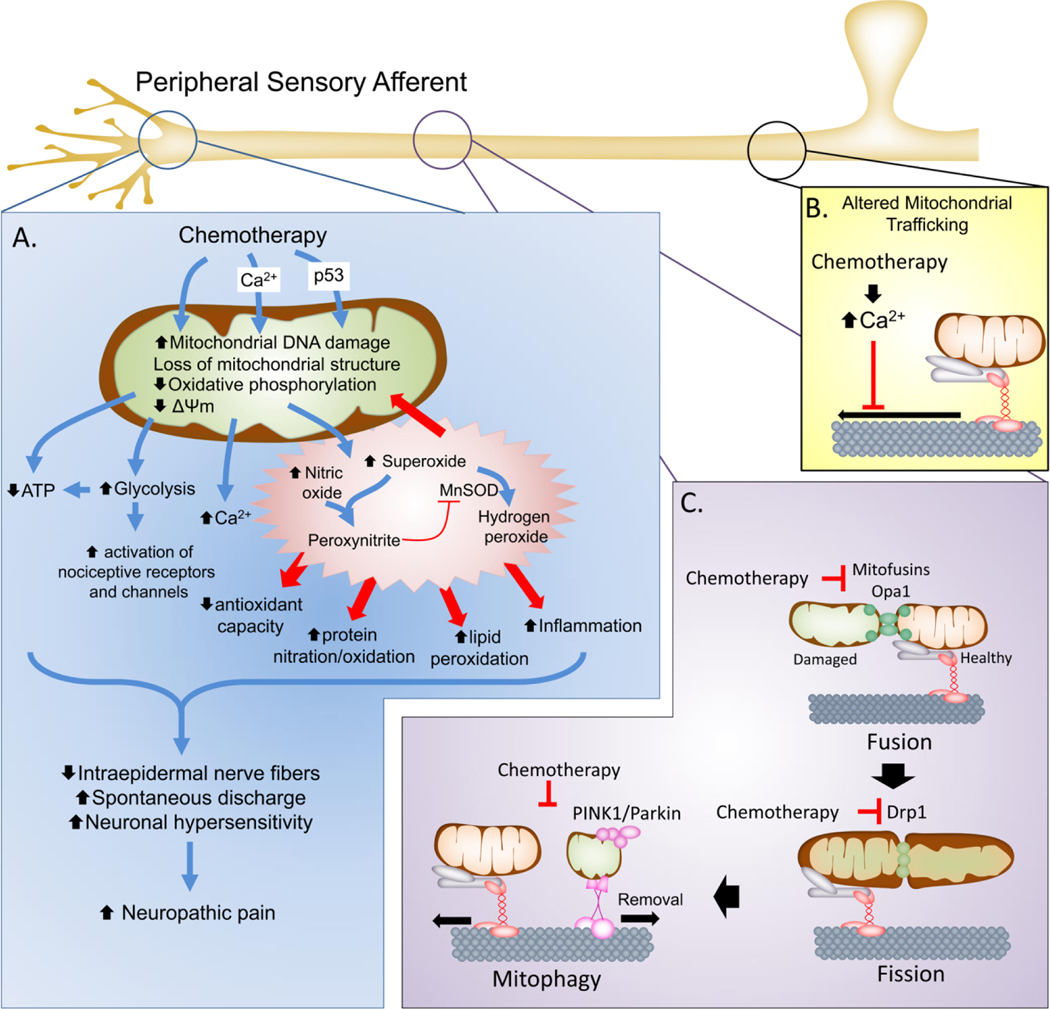
Figure 1. Mitochondrial dysfunction in chemotherapy-induced neuropathy.
A. In the peripheral sensory neurons, chemotherapeutic agents can cause direct or indirect (e.g., through Ca2+ influx or p53 accumulation) injury to mitochondria that include damage to mitochondrial DNA, loss of mitochondrial morphology and disruption of oxidative phosphorylation and mitochondrial membrane potential. This leads to reduced ATP production and increased reliance on glycolysis that result the net reduction of cellular bioenergetic capacity to respond to increase cellular activity and potential activation of nociceptive receptors and channels. Moreover, mitochondrial dysfunction also leads to increased production of SO and PN to drive nitroxidative stress that initiate protein, lipid and nucleic acid modification to further drive nitro-oxidative stress and mitochondrial dysfunction as well as contribute to neuronal signaling pathways and inflammation. Collectively this leads to reduced axonal growth, loss of IENFs and increased spontaneous discharge and neuronal hypersensitivity that contribute to establishment of the chronic neuropathic pain state. B. Chemotherapeutics also contribute to mitochondrial dysfunction by altering the axonal transport of mitochondria to the axon terminals, depriving the axonal terminals of bioenergetics support. C. The health of mitochondria is maintained in part by mitochondrial fission and fusion processes that allow healthy mitochondria to fuse and mix with damage mitochondria to sort the damaged areas for removal (mitophagy). In addition to altering transport, chemotherapeutics may down regulate the expression of mitochondrial fusion (mitofusins and Opa1) and fission (Drp1) proteins to disrupt the renewal of mitochondria in the axonal terminals and prevent mitophagy resulting in the accumulation of abnormal, dysfunctional mitochondria.