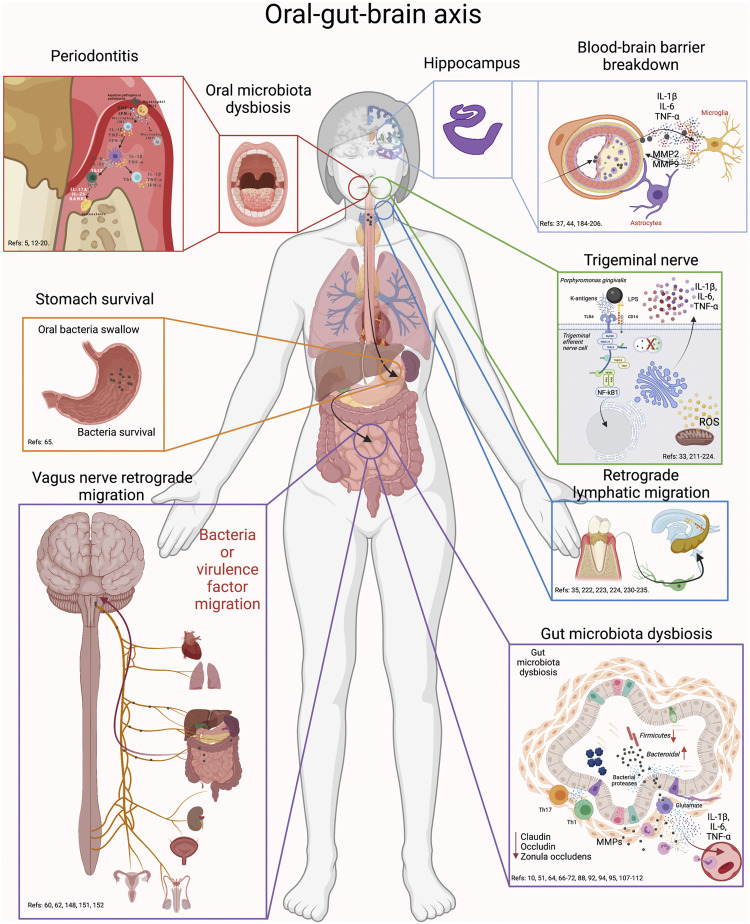
FIGURE 6.
Oral-gut-brain axis. During periodontitis, the exacerbated increase in anaerobic bacteria generates alterations in the intestinal microbiota. First, swallowed oral bacteria are significantly increased. These bacteria can survive the stomach pH and upon reaching the intestine, they can cause intestinal dysbiosis, alteration in the integrity of the intestinal barrier and inflammation. This effect will cause virulence factors or pro-inflammatory mediators to diffuse into the peripheral circulation and thus migrate to the brain. In addition, oral dysbiotic bacteria can migrate to the brain via the trigeminal nerve endings or through the lymphatic vessels. Another possible route of migration is through the fibers of the vagus nerve that innervate the intestine. Thus, the possible routes of migration of oral bacteria to the brain can be through oral-brain communication or through gut-brain communication. Thus, periodontitis could be associated with neuroinflammatory events by direct communication with the brain or, indirectly, by altering intestinal homeodynamics.