Abstract
Background
Patient-reported outcome measures (PROMs) are frequently used to assess treatment outcomes for hand and wrist conditions. To adequately interpret these outcomes, it is important to determine whether a statistically significant change is also clinically relevant. For this purpose, the minimally important change (MIC) was developed, representing the minimal within-person change in outcome that patients perceive as a beneficial treatment effect. Prior studies demonstrated substantial differences in MICs between condition-treatment combinations, suggesting that MICs are context-specific and cannot be reliably generalized. Hence, a study providing MICs for a wide diversity of condition-treatment combinations for hand and wrist conditions will contribute to more accurate treatment evaluations.
Questions/purposes
(1) What are the MICs of the most frequently used PROMs for common condition-treatment combinations of hand and wrist conditions? (2) Do MICs vary based on the invasiveness of the treatment (nonsurgical treatment or surgical treatment)?
Methods
This study is based on data from a longitudinally maintained database of patients with hand and wrist conditions treated in one of 26 outpatient clinics in the Netherlands between November 2013 and November 2020. Patients were invited to complete several validated PROMs before treatment and at final follow-up. All patients were invited to complete the VAS for pain and hand function. Depending on the condition, patients were also invited to complete the Michigan Hand outcomes Questionnaire (MHQ) (finger and thumb conditions), the Patient-rated Wrist/Hand Evaluation (PRWHE) (wrist conditions), or the Boston Carpal Tunnel Questionnaire (BCTQ) (nerve conditions). Additionally, patients completed the validated Satisfaction with Treatment Result Questionnaire at final follow-up. Final follow-up timepoints were 3 months for nonsurgical and minor surgical treatment (including trigger finger release) and 12 months for major surgical treatment (such as trapeziectomy). Our database included 55,651 patients, of whom we excluded 1528 who only required diagnostic management, 25,099 patients who did not complete the Satisfaction with Treatment Result Questionnaire, 3509 patients with missing data in the PROM of interest at baseline or follow-up, and 1766 patients who were part of condition-treatment combinations with less than 100 patients. The final sample represented 43% (23,749) of all patients and consisted of 36 condition-treatment combinations. In this final sample, 26% (6179) of patients were managed nonsurgically and 74% (17,570) were managed surgically. Patients had a mean ± SD age of 55 ± 14 years, and 66% (15,593) of patients were women. To estimate the MIC, we used two anchor-based methods (the anchor mean change and the MIC predict method), which were triangulated afterward to obtain a single MIC. Applying this method, we calculated the MIC for 36 condition-treatment combinations, comprising 22 different conditions, and calculated the MIC for combined nonsurgical and surgical treatment groups. To examine whether the MIC differs between nonsurgical and surgical treatments, we performed a Wilcoxon signed rank test to compare the MICs of all PROM scores between nonsurgical and surgical treatment.
Results
We found a large variation in triangulated MICs between the condition-treatment combinations. For example, for nonsurgical treatment of hand OA, the MICs of VAS pain during load clustered around 10 (interquartile range 8 to 11), for wrist osteotomy/carpectomy it was around 25 (IQR 24 to 27), and for nerve decompression it was 21. Additionally, the MICs of the MHQ total score ranged from 4 (nonsurgical treatment of CMC1 OA) to 15 (trapeziectomy with LRTI and bone tunnel), for the PRWHE total score it ranged from 2 (nonsurgical treatment of STT OA) to 29 (release of first extensor compartment), and for the BCTQ Symptom Severity Scale it ranged from 0.44 (nonsurgical treatment of carpal tunnel syndrome) to 0.87 (carpal tunnel release). An overview of all MIC values is available in a freely available online application at: https://analyse.equipezorgbedrijven.nl/shiny/mic-per-treatment/. In the combined treatment groups, the triangulated MIC values were lower for nonsurgical treatment than for surgical treatment (p < 0.001). The MICs for nonsurgical treatment can be approximated to be one-ninth (IQR 0.08 to 0.13) of the scale (approximately 11 on a 100-point instrument), and surgical treatment had MICs that were approximately one-fifth (IQR 0.14 to 0.24) of the scale (approximately 19 on a 100-point instrument).
Conclusion
MICs vary between condition-treatment combinations and differ depending on the invasiveness of the intervention. Patients receiving a more invasive treatment have higher treatment expectations, may experience more discomfort from their treatment, or may feel that the investment of undergoing a more invasive treatment should yield greater improvement, leading to a different perception of what constitutes a beneficial treatment effect.
Clinical Relevance
Our findings indicate that the MIC is context-specific and may be misleading if applied inappropriately. Implementation of these condition-specific and treatment-specific MICs in clinical research allows for a better study design and to achieve more accurate treatment evaluations. Consequently, this could aid clinicians in better informing patients about the expected treatment results and facilitate shared decision-making in clinical practice. Future studies may focus on adaptive techniques to achieve individualized MICs, which may ultimately aid clinicians in selecting the optimal treatment for individual patients.
Introduction
In recent years, the use of patient-reported outcome measures (PROMs) has become standard practice in clinical research and daily clinics for interpreting treatment results from the patient’s perspective [28]. Unfortunately, clinicians are often faced with evidence that is challenging to interpret clinically as conclusions about treatment effects are often made from a statistical point of view [15, 16, 23, 27]. Statistically significant changes do not provide information about the magnitude of a treatment effect and therefore may not be meaningful to patients or clinicians. To interpret whether a statistically significant treatment effect is also clinically relevant, the minimally important change (MIC) concept is essential [23, 30, 40]. The MIC refers to the smallest change from baseline to post-treatment that patients perceive as important. Although often used interchangeably with the minimum clinically important difference (MCID), the MCID indicates the importance of a difference in outcomes between treatment groups (such as, fasciectomy versus collagenase) and thus represents a distinct entity [23, 30, 40].
In hand surgery, the MIC has been determined for multiple PROMs, including the Michigan Hand outcomes Questionnaire (MHQ) [13, 18, 20-22, 35], the Patient-rated Wrist/Hand Evaluation (PRWHE) [31, 36], and Boston Carpal Tunnel Questionnaire (BCTQ) [21, 25, 32]. However, we noticed in previous evidence that MIC values for each PROM differ substantially not only between hand conditions, but also between different treatments for the same hand condition. For example, the MIC for the MHQ total score ranges from 9 for patients undergoing trigger finger release [13] to 18 for patients after proximal interphalangeal joint arthroplasty [22]. In addition, patients with carpal tunnel syndrome treated surgically yielded a higher MIC than patients receiving steroid injections [32].
Rationale
These findings suggest that MICs are context-specific and cannot always be reliably generalized to other condition-treatment combinations. For example, as treatments differ in invasiveness, rehabilitation periods, and discomfort experienced by patients, it is plausible that patients undergoing surgical treatment require a larger improvement before being satisfied compared with those undergoing nonsurgical treatment. Hence, a study providing specific MICs for various condition-treatment combinations for hand and wrist conditions will contribute to more accurate treatment evaluations in clinical research. As a result, this could aid clinicians in better informing patients about the expected treatment results, which may facilitate shared decision-making in clinical practice.
Therefore, we asked: (1) What are the MICs of the most frequently used PROMs for common condition-treatment combinations of hand and wrist conditions? (2) Do MICs vary based on the invasiveness of the treatment (nonsurgical treatment or surgical treatment)?
Patients and Methods
Study Design
This study is based on data from a longitudinally maintained database of patients with hand and wrist conditions (the Hand-Wrist Study Cohort), reported according to the Strengthening the Reporting of Observational Studies in Epidemiology statement [41]. The cohort and data collection [34] and their use in daily clinical care [11] have been described in more detail.
Setting
Between November 2013 and November 2020, we collected data at Xpert Clinics Hand and Wrist Care and Xpert Clinics Hand Therapy. Xpert Clinics currently comprises 26 locations, 23 European Board-certified hand surgeons, and more than 150 hand therapists. As part of routine outcome measurements, we invited all patients to complete PROMs before and at fixed timepoints after treatment based on the measurement track [34, 43].
Participants
For each outcome, we included all condition-treatment combinations consisting of at least 100 patients with data for the PROMs of interest at baseline and at the final follow-up examination. For nonsurgical treatments (such as hand therapy for thumb base osteoarthritis or a steroid injection for trigger finger) and minor surgical treatments (such as trigger finger release or carpal tunnel release), the final follow-up was at 3 months post-treatment. For major surgical treatments (for example, trapeziectomy or proximal row carpectomy), the final follow-up was 12 months post-treatment (Supplementary Table 1; http://links.lww.com/CORR/A707).
To prevent ceiling effects, we excluded patients with a baseline score of 90 or more points for the MHQ total or subscale scores or VAS pain, at most 10 points for the PRWHE total score or VAS hand function, 5 points or less for the PRWHE pain and hand function score, or no more than 1.4 points for the BCTQ subscales because this may result in an underestimation of the MIC [18]. The exact number of included patients for each PROM subscale and each condition-treatment combination can be found in our freely available online application at: https://analyse.equipezorgbedrijven.nl/shiny/mic-per-treatment/.
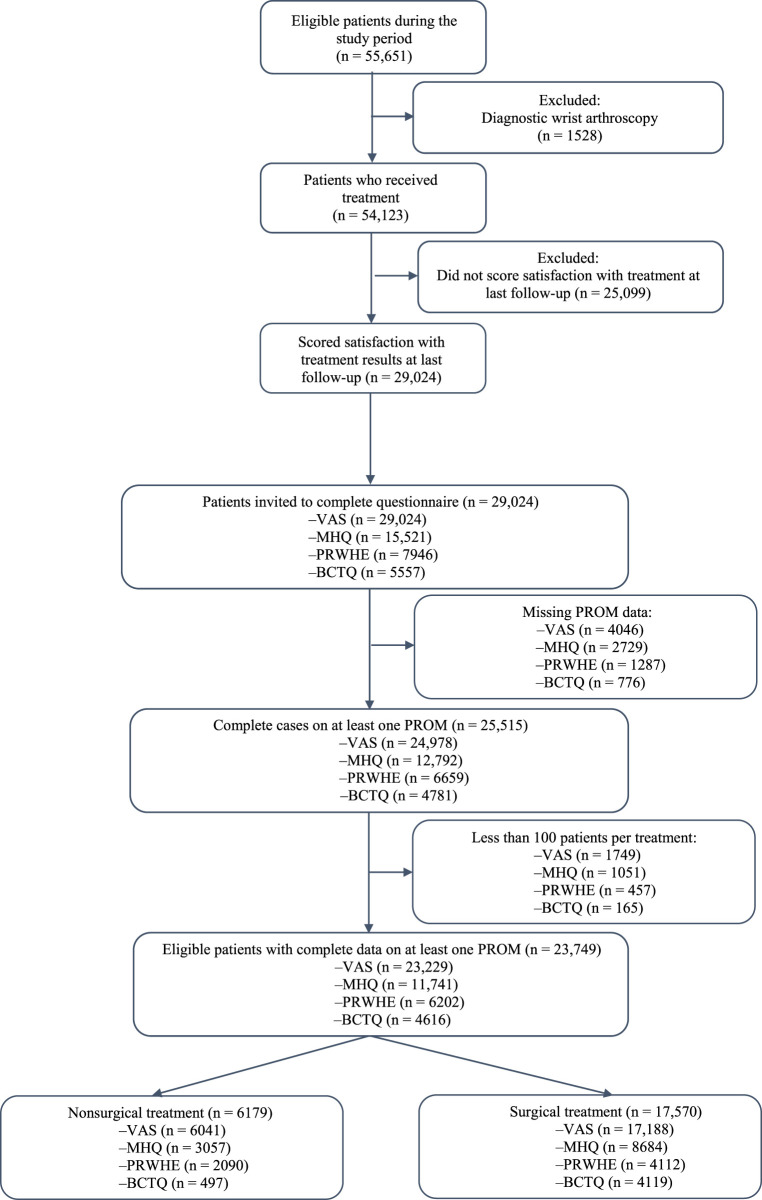
During the study period, 55,651 patients were treated for a hand or wrist condition. We excluded 1528 patients who only required diagnostic management (such as, diagnostic wrist arthroscopy), 25,099 patients who did not complete the Satisfaction with Treatment Result Questionnaire, 3509 patients with missing data in the PROM of interest at baseline or follow-up, and 1766 patients who were part of condition-treatment combinations with less than 100 patients. Our final sample represented 43% (23,749 of 55,651) of all patients and consisted of 36 condition-treatment combinations (Fig. 1). Of these, 26% (6179 of 23,749) received nonsurgical treatment and 74% (17,570 of 23,749) received surgical treatment (Table 1). The mean ± SD age of the nonsurgically managed patients was 57 ± 15 years, and 72% (4479) were women. The surgically managed patients had a mean ± SD age of 55 ± 14 years, and 63% (11,114) were women.
Fig. 1.
This flowchart shows the patients who were included in our study. As patients were invited to complete the VAS and one other PROM most suitable for their diagnosis, the total number indicated at the top of the box is less than the total number of PROM responses.
Table 1.
Patient characteristics per treatment group for patients with complete data for at least one PROM and satisfaction with treatment results
| Parameter | All included patients (n = 23,749) | Nonsurgical treatment (n = 6179) | Surgical treatment (n = 17,570) |
| Age in years | 55 ± 14 | 57 ± 15 | 55 ± 14 |
| Gender | |||
| Women | 66 (15,593) | 72 (4479) | 63 (11,114) |
| Duration of symptoms in months | 11 (5-24) | 6 (3-15) | 12 (6-24) |
| Hand dominance | |||
| Right | 88 (20,888) | 89 (5488) | 88 (15,400) |
| Left | 9 (2107) | 8 (500) | 9 (1607) |
| Both | 3 (754) | 3 (191) | 3 (563) |
| Affected side | |||
| Right | 55 (12,977) | 52 (3239) | 55 (9738) |
| Left | 43 (10,242) | 40 (2445) | 44 (7797) |
| Both | 2 (530) | 8 (495) | 0.2 (35) |
| Occupational intensity | |||
| Not employed | 38 (8920) | 35 (2134) | 39 (6786) |
| Light (such as working in an office) | 27 (6346) | 28 (1713) | 26 (4633) |
| Moderate (such as working in a shop) | 24 (5760) | 26 (1635) | 23 (4125) |
| Heavy (such as working in construction) | 11 (2723) | 11 (697) | 12 (2026) |
| Involved in a personal injury claima | |||
| Yes | 2 (311) | 2 (102) | 2 (209) |
Data presented as mean ± SD, % (n), or median (IQR).
This information was available for a selection of patients (all included patients: n = 17,413, nonsurgical treatment: n = 5193, surgical treatment: n = 12,220); PROM = patient-reported outcome measure.
Variables and Measurements
As part of routine follow-up, we invited all patients to complete the VAS for pain and hand function, regardless of the condition-treatment combination. Additionally, patients were invited to complete a more disease-specific PROM (the MHQ, the PRWHE, or the BCTQ). This was dependent on the condition-treatment combination and associated measurement track [34]. In brief, wrist conditions were assessed with the PRWHE, finger and thumb conditions with the MHQ, and nerve conditions with the BCTQ.
We used the VAS to examine pain (scale of 0-100; higher scores indicate more pain) and function (scale of 0-100; higher scores indicate poorer function). The VAS for pain was measured for three situations: pain at rest, pain during physical load, and average pain during the past week. The VAS has high test-retest reliability, good ability to detect change, and acceptable concurrent validity [12].
The MHQ consists of six domains (overall hand function, work performance, activities of daily living, pain, aesthetics, and satisfaction with hand function), each with a score ranging from 0 to 100 [4]. Higher scores indicate better performance, except for the subscale of pain. For interpretability, we reverted the pain subscale such that higher scores indicate less pain. We analyzed scores of the affected hand. The MHQ has been shown to have a high test-retest reliability, internal consistency, internal validity, and good responsiveness to change [4, 35].
The PRWHE is a validated questionnaire [19] with high internal consistency and reliability [26]. The PRWHE assesses the domains of pain and function, with scores ranging from 0 to 50 (higher scores indicate worse outcomes). The total score is calculated as the sum of both domains.
The BCTQ is a validated questionnaire comprising two domains: the Symptom Severity Scale and Functional Status Scale, with scores ranging from 1 to 5 (higher scores indicate more complaints) [17]. The BCTQ has good validity, reliability, and responsiveness [14].
To assess satisfaction with treatment results, we invited all patients to answer an additional question from the Satisfaction with Treatment Result Questionnaire: “How satisfied are you with the treatment result thus far? [7]. Responses were limited to one of the following items, scored on a Likert scale: excellent, good, fair, moderate, or poor. This questionnaire has recently been reported to be reliable and has good construct validity [7].
Primary and Secondary Study Outcomes
The primary aim of this study was to determine the MICs of four PROMs for a variety of condition-treatment combinations of hand and wrist conditions. To achieve this, we estimated the MICs of all PROMs for each condition-treatment combination using two anchor-based methods: the anchor mean change method and the MIC predict method [38, 39]. The weighted mean of both methods was considered to represent the MIC.
Our secondary aim was to examine whether the MIC differs based on the invasiveness of the treatment (nonsurgical treatment or surgical treatment). To achieve this, we performed a Wilcoxon signed rank test to compare the MICs of the PROM scores of nonsurgical and surgical treatments.
Ethical Approval
Ethical approval for this study was obtained from the Erasmus MC University Medical Center, Rotterdam, the Netherlands (MEC-2018-1088).
Study Size and Statistical Methods
To our knowledge, there are no recommendations regarding sample size for calculating an MIC. However, we considered that 100 patients would be sufficient to calculate a condition and treatment-specific MIC. In general, the MIC can be determined with distribution-based, anchor-based, or qualitative methods [33, 37]. Although the ideal method is still under discussion, anchor-based methods are the most frequently used and preferred approaches [15, 29, 33, 40]. We used two anchor-based methods to determine the MICs for each PROM: the anchor mean change method and the MIC predict method [38, 39]. For both methods, we used satisfaction with treatment result as an anchor.
Anchor mean change methods determine the MIC based on the group of patients reporting minimal improvement on the anchor question [29]. Using the satisfaction with the treatment result as anchor question, the response option “fair” was considered a minimal improvement. Hence, the MIC was defined as the mean change in the PROM of interest of patients rating their satisfaction with treatment results as fair in the anchor mean change method. To determine whether the anchor was suitable for further analyses, we calculated the Spearman correlation coefficient between the anchor question and change on the PROM of interest. Following current standards, an absolute correlation at least 0.3 was considered sufficient [29]. Because MIC values depend on baseline values [1], we also reported the baseline values of all PROMs before nonsurgical treatment, minor surgery, and major surgery (Table 2).
Table 2.
Baseline PROM scores per type of treatment are shown to provide a reference on symptom severity before treatment and the relativity of the MIC
| Parameter | PROM Range | Nonsurgical treatment, mean ± SD (n = 6179) | Surgical treatment, mean ± SD (n = 17,570) | Effect size |
| VAS pain during load | 0-100 | 59 ± 25 | 55 ± 30 | 0.15 |
| VAS pain at rest | 0-100 | 35 ± 26 | 38 ± 28 | -0.09 |
| VAS average pain | 0-100 | 49 ± 24 | 48 ± 27 | 0.07 |
| VAS hand function | 0-100 | 52 ± 25 | 50 ± 26 | 0.09 |
| MHQ total score | 0-100 | 62 ± 15 | 64 ± 18 | -0.19 |
| MHQ pain | 0-100 | 50 ± 19 | 56 ± 24 | -0.24 |
| MHQ hand function | 0-100 | 59 ± 18 | 62 ± 19 | -0.12 |
| MHQ work | 0-100 | 63 ± 26 | 69 ± 28 | -0.23 |
| MHQ ADL | 0-100 | 70 ± 20 | 74 ± 23 | -0.20 |
| MHQ aesthetics | 0-100 | 82 ± 20 | 79 ± 20 | 0.17 |
| MHQ satisfaction | 0-100 | 46 ± 23 | 49 ± 26 | -0.12 |
| PRWHE total score | 0-100 | 56 ± 21 | 60 ± 21 | -0.20 |
| PRWHE pain | 0-50 | 30 ± 11 | 32 ± 10 | -0.19 |
| PRWHE hand function | 0-50 | 26 ± 12 | 28 ± 12 | -0.19 |
| BCTQ symptom severity scale | 1-5 | 2.6 ± 0.7 | 2.9 ± 0.7 | -0.35 |
| BCTQ functional status scale | 1-5 | 2.3 ± 0.8 | 2.5 ± 0.8 | -0.19 |
PROM = patient-reported outcome measure; MIC = minimum important change; MHQ = Michigan Hand outcomes Questionnaire; ADL = activities of daily living; PRWHE = Patient-Rated Wrist/Hand Evaluation; BCTQ = Boston Carpal Tunnel Questionnaire.
The MIC predict method is a receiver operating characteristic method that provides more accurate estimates when the groups of satisfied and dissatisfied patients are not equal in size [38, 39]. Because receiver operating characteristic curve methods require dichotomization of the anchor question, patients rating their satisfaction with the treatment results as fair, good, or excellent were classified as satisfied. In contrast, we classified patients as dissatisfied if they rated their satisfaction as moderate or poor. We used the receiver operating characteristic curve method to determine the change in score on the PROM of interest that distinguished between satisfied and dissatisfied patients with the highest sensitivity and specificity, based on the Youden index [45]. Discriminative ability was considered sufficient if the area under the curve was at least 0.75 [10]. As mentioned, the MIC predict method allows for correction of imbalance in group sizes of satisfied and dissatisfied patients, because unequal group sizes may lead to biased MIC estimates [38, 39]. In our study, a larger proportion of patients were satisfied with their treatment (78% [4832 of 6179] for nonsurgical treatment and 86% [15,077 of 17,570] for surgical treatment). We therefore corrected the number of satisfied patients using logistic regression analysis, as described by Terluin et al. [38, 39]. To obtain a single MIC value, we triangulated the MIC estimates of both methods, assigning more weight (2:1) to the MIC predict method. The weighted mean of both methods was determined to represent the MIC.
To examine whether the MIC differs based on the invasiveness of the treatment, we compared the MICs of all PROM scores that were available for both nonsurgical and surgical treatment using a Wilcoxon signed rank test. We performed a nonresponder analysis to compare the characteristics of patients who completed all questionnaires of interest (47% [25,515 of 54,123] responders) and patients who did not (53% [28,608 of 54,123] nonresponders). For normally distributed continuous variables, we used t-tests. For nonnormally distributed continuous variables, we used the Wilcoxon test. Chi-square tests were used to compare categorical variables. Additionally, effect sizes for differences were calculated. We calculated the Cohen d for continuous variables and the Cliff delta for categorical variables. In the nonresponder analysis, we found differences in the type of treatment, age, gender, and duration of symptoms (Supplementary Table 2; http://links.lww.com/CORR/A708), with absolute effect sizes ranging from 0.00 to 0.14, indicating very small effects [5]. All analyses were performed using R statistical software, version 4.0.1 (R core team). A p value smaller than 0.05 was considered statistically significant.
Results
MICs for Common Condition-Treatment Combinations
We observed substantial variation in the MICs for different condition-treatment combinations. For example, the MICs of VAS pain during load for nonsurgical treatment of hand osteoarthritis (OA) (including CMC-1 OA, STT OA, and MCP/PIP/DIP OA) clustered around 10 (interquartile range 8 to 11), for wrist osteotomy/carpectomy (including corrective osteotomy distal radius, ulnar shortening osteotomy, and proximal row carpectomy) the MIC was around 25 (IQR 24 to 27), and for nerve decompression (including cubital tunnel release and carpal tunnel release) it was 21 (Table 3). Additionally, the MICs of the MHQ total score ranged from 4 (nonsurgical treatment of CMC1 OA) to 15 (trapeziectomy with LRTI and bone tunnel) (Table 4), for the PRWHE total score it ranged from 2 (nonsurgical treatment of STT OA) to 29 (release of first extensor compartment) (Table 5), and for the BCTQ Symptom Severity Scale it ranged from 0.44 (nonsurgical treatment of carpal tunnel syndrome) to 0.87 (carpal tunnel release) (Table 6).
Table 3.
Triangulated MIC values per treatment (group) for VAS subscales pain during load, pain at rest, average pain, and hand functiona
| Parameter | VAS pain during load (0-100) | VAS pain at rest (0-100) | VAS average pain (0-100) | VAS hand function (0-100) |
| All | 20 | 20 | 19 | 17 |
| Nonsurgical treatment | 13 | 12 | 11 | 10 |
| Surgical treatment | 23 | 23 | 23 | 19 |
| Nonsurgical treatment | ||||
| Carpal tunnel syndrome | 13 | 17 | 14 | NAb |
| Cubital tunnel syndrome | -3 | NAc | NAc | 4 |
| Tendinitis or tenosynovitis wrist | 19 | 15 | 18 | 16 |
| Trigger finger | 13 | 12 | 10 | 10 |
| Trigger thumb | 17 | 11 | 15 | 10 |
| CMC-1 OA | 8 | 9 | 8 | 6 |
| CMC-1 instability | 14 | 13 | 13 | 14 |
| STT OA | 10 | 10 | 6 | 8 |
| MCP/PIP/DIP OA | 11 | 12 | 11 | NAb |
| UCL/RCL/VP injury MCP/PIP/DIP | 19 | NAc | 16 | 15 |
| Mallet finger | NAc | NAb | NAc | 12 |
| Midcarpal instability or laxity | 15 | 15 | 14 | 12 |
| Minor surgical treatments | ||||
| Carpal tunnel release | 21 | 28 | 25 | 18 |
| Cubital tunnel release | 21 | 21 | 21 | 17 |
| Release of the first extensor compartment | 32 | 27 | 28 | 24 |
| Trigger finger release | 24 | 21 | 21 | 18 |
| Trigger thumb release | 28 | 23 | 25 | 22 |
| Excision of volar wrist ganglion | 22 | 23 | 21 | 21 |
| Excision of dorsal wrist ganglion | 24 | 24 | 21 | 16 |
| Mucoid cyst excision finger | 13 | 17 | 12 | 13 |
| Percutaneous needle aponeurotomy (possibly with lipofilling) | 12 | 14 | 14 | NAb |
| Major surgical treatments | ||||
| Corrective osteotomy distal radius | 25 | 20 | 23 | 26 |
| Ulnar shortening osteotomy | 24 | 22 | 22 | 24 |
| TFCC reinsertion | 25 | 22 | 22 | 22 |
| Proximal row carpectomy | 27 | 21 | 25 | 18 |
| Osteosynthesis for nonunion of scaphoid fracture | NAb | NAc | NAb | 22 |
| Pisiformectomy | 25 | 20 | 23 | 21 |
| Dorsal capsulodesis wrist (possibly combined with dorsal ganglion excision) | 27 | 23 | 26 | 19 |
| Three-ligament tenodesis (Brunelli) | 23 | 17 | 19 | 19 |
| Limited fasciectomy (possibly with skin graft) | 14 | 18 | 14 | 19 |
| Trapeziectomy with LRTI using the FCR (Weilby technique) | 29 | 26 | 28 | 21 |
| Trapeziectomy with LRTI using the FCR and bone tunnel (Burton-Pellegrini technique) | 32 | 31 | 27 | 23 |
| Other surgical treatments for CMC-1 OA | 33 | 27 | 33 | 23 |
| CMC-1 instability treated surgically | 25 | 20 | 23 | 19 |
| PIP prosthesis | 30 | NAb | NAb | 13 |
| UCL reinsertion MCP-1 | 25 | NAc | NAc | 23 |
aThese scores represent the MIC per condition-treatment combination and for nonsurgical and surgical treatment overall.
Insufficient correlation.
Insufficient number of patients; MIC = minimum important change; CMC-1 = first carpometacarpal joint; OA = osteoarthritis; STT = scaphotrapeziotrapezoid joint; MCP = metacarpal joint; PIP = proximal interphalangeal joint; DIP = distal interphalangeal joint; UCL = ulnar collateral ligament; RCL = radial collateral ligament; VP = volar plate; TFCC = triangular fibrocartilage complex; LRTI = ligament reconstruction and tendon interposition; FCR = flexor carpi radialis tendon.
Table 4.
Triangulated MIC values per treatment (group) for the MHQ total score and MHQ subscales
| Parameter | MHQ total score (0-100) | MHQ hand function (0-100) | MHQ work (0-100) | MHQ ADL (0-100) | MHQ pain (0-100) | MHQ aesthetics (0-100) | MHQ satisfaction (0-100) |
| All | 8 | 5 | 11 | 12 | 12 | 11 | 16 |
| Nonsurgical treatment | 5 | 3 | 8 | 6 | 8 | NAa | 11 |
| Surgical treatment | 9 | 7 | 13 | 15 | 13 | 12 | 20 |
| Nonsurgical treatment | |||||||
| Trigger finger | 7 | 5 | 7 | NAa | 11 | 8 | 14 |
| Trigger thumb | 7 | 5 | 10 | 7 | 12 | NAb | 14 |
| CMC-1 OA | 4 | 1 | 6 | 4 | 7 | NAa | 9 |
| CMC-1 instability | 5 | 7 | 12 | 6 | 10 | NAb | 14 |
| MCP/PIP/DIP OA | 6 | NAa | 7 | NAa | 9 | NAa | 12 |
| UCL/RCL/VP injury MCP/PIP/DIP | 7 | NAa | NAa | 12 | 8 | NAa | 11 |
| Mallet finger | 6 | NAb | NAb | NAb | NAb | NAb | 12 |
| Minor surgical treatments | |||||||
| Trigger finger release | 8 | 8 | 10 | 14 | 13 | 11 | 19 |
| Trigger thumb release | 11 | 6 | NAa | 16 | 16 | NAa | 20 |
| Mucoid cyst finger excision | 4 | 1 | NAa | NAa | 6 | 10 | 6 |
| Percutaneous needle aponeurotomy (possibly with lipofilling) | NAa | 5 | NAa | NAa | NAa | NAa | NAa |
| Major surgical treatments | |||||||
| Limited fasciectomy (possibly with skin graft) | 5 | 4 | 16 | 8 | 8 | 11 | 14 |
| Trapeziectomy with LRTI using the FCR (Weilby technique) | 14 | 9 | 12 | 19 | 19 | NAa | 24 |
| Trapeziectomy with LRTI using the FCR and bone tunnel (Burton-Pellegrini technique) | 15 | 9 | 16 | 19 | 18 | NAb | 24 |
| Other surgical treatments for CMC-1 OA | 15 | 10 | 112 | 21 | 22 | NAb | 25 |
| CMC-1 instability treated surgically | 13 | 9 | 18 | 13 | 18 | NAb | 21 |
| PIP prosthesis | 13 | 10 | NAa | 12 | 24 | 8 | 21 |
| UCL reinsertion MCP-1 | 14 | NAb | NAb | NAb | 21 | NAb | 19 |
Insufficient correlation.
Insufficient number of patients; MIC = minimum important change; MHQ = Michigan Hand outcomes Questionnaire; ADL = activities of daily living; CMC-1 = first carpometacarpal joint; OA = osteoarthritis; MCP = metacarpal joint; PIP = proximal interphalangeal joint; DIP = distal interphalangeal joint; UCL = ulnar collateral ligament; RCL = radial collateral ligament; VP = volar plate; LRTI = ligament reconstruction and tendon interposition; FCR = flexor carpi radialis tendon.
Table 5.
Triangulated MIC values per treatment (group) for the PRWHE total score and subscales
| Parameter | PRWHE total score (0-100) | PRWHE pain score (0-50) | PRWHE function score (0-50) |
| All | 20 | 10 | 11 |
| Nonsurgical treatment | 13 | 7 | 7 |
| Surgical treatment | 24 | 12 | 13 |
| Nonsurgical treatment | |||
| Tendinitis or tenosynovitis wrist | 17 | 9 | 10 |
| STT OA | 2 | 2 | 1 |
| Midcarpal instability or laxity | 10 | 6 | 5 |
| Minor surgical treatments | |||
| Release of the first extensor compartment | 29 | 14 | 16 |
| Excision of volar wrist ganglion | 16 | 9 | 9 |
| Excision of dorsal wrist ganglion | 20 | 11 | 10 |
| Major surgical treatments | |||
| Corrective osteotomy of the distal radius | 26 | 11 | 15 |
| Ulna shortening osteotomy | 22 | 10 | 12 |
| TFCC reinsertion | 24 | 12 | 13 |
| Proximal row carpectomy | 21 | 12 | 10 |
| Osteosynthesis for nonunion of scaphoid fracture | 26 | 12 | 15 |
| Pisiformectomy | 24 | 11 | 13 |
| Dorsal capsulodesis of the wrist (possibly combined with dorsal ganglion excision) | 21 | 11 | 11 |
| Three ligament tenodesis (Brunelli) | 22 | 11 | 12 |
MIC = minimum important change; PRWE = Patient-Rated Wrist/Hand Evaluation; STT = scaphotrapeziotrapezoid joint; OA = osteoarthritis; TFCC = triangular fibrocartilage complex.
Table 6.
Triangulated MIC values per treatment (group) for BCTQ symptom severity scale and BCTQ functional status scale
| BCTQ symptom severity scale (1-5) | BCTQ functional status scale (1-5) | |
| All | 0.79 | 0.52 |
| Nonsurgical treatment | 0.43 | 0.32 |
| Surgical treatment | 0.84 | 0.56 |
| Nonsurgical treatment | ||
| Carpal tunnel syndrome | 0.44 | 0.36 |
| Cubital tunnel syndrome | NAa | NAa |
| Surgical treatment | ||
| Carpal tunnel release | 0.87 | 0.57 |
| Cubital tunnel release | 0.60 | 0.47 |
Insufficient number of patients; MIC = minimum important change; BCTQ = Boston Carpal Tunnel Questionnaire.
MIC values per calculation method and triangulated MIC values are freely available in an online application at https://analyse.equipezorgbedrijven.nl/shiny/mic-per-treatment/. This online application allows users to select a treatment for which all MIC values and more details of the MIC calculation for all available PROM subscales are shown.
MICs Vary with the Invasiveness of Treatment
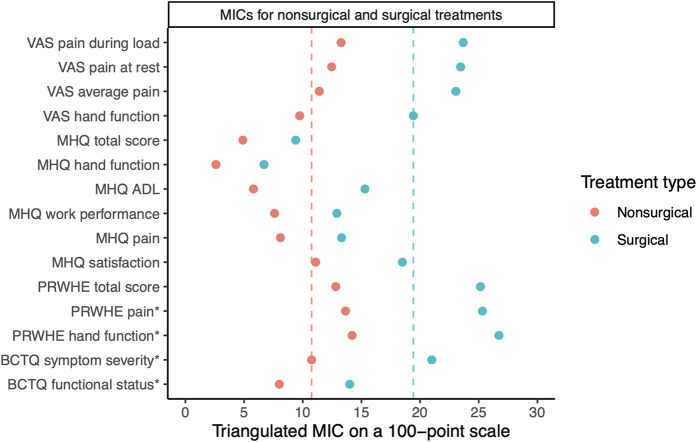
We found that MICs among the combined treatment groups were lower for nonsurgical treatment compared with surgical treatment (p < 0.001) (Fig. 2). The MICs for nonsurgical treatment can be approximated to be one-ninth (IQR 0.08 to 0.13) of the scale (approximately 11 on a 100-point instrument), and surgical treatment had MICs that were approximately one-fifth (IQR 0.14 to 0.24) of the scale (approximately 19 on a 100-point instrument).
Fig. 2.
This figure shows triangulated MIC values for the VAS, MHQ, PRWHE, and BCTQ, categorized by treatment group (nonsurgical and surgical). Results are presented as the triangulated MIC value (dots). For interpretability, we converted the PRWHE and BCTQ subscales (shown with an asterisk) to a 100-point scale. The dashed lines represent the median MIC values for nonsurgical (red) and surgical (blue) treatments. Overall, this figure shows that MIC values are higher for surgical treatments (median 19 points; IQR 14 to 24) compared with nonsurgical treatments (median 11 points; IQR 8 to 13). A color image accompanies the online version of this article.
Discussion
Because the use of PROMs has become standard practice in clinical research, further insight into MICs for specific conditions and treatments is essential to accurately interpret whether a change is clinically relevant. In this large, multicenter study, we were able to provide condition-specific and treatment-specific MICs of four commonly used PROMs for hand and wrist conditions. This study shows that MICs differ between condition-treatment combinations. Furthermore, we found higher MICs for surgical treatments than for nonsurgical treatments. These findings indicate that the MIC is context-specific and that it may be misleading if applied inappropriately. Implementation of these condition-specific and treatment-specific MICs in clinical research allows for a better study design to achieve more accurate treatment evaluations. Consequently, this could aid clinicians in better informing patients about the expected treatment results and facilitate shared decision-making in clinical practice.
Limitations
This study also has several limitations. One limitation is that the observational design of this study was associated with a large proportion of missing data. However, although 53% (28,608 of 54,123) of patients did not complete all questionnaires of interest, our nonresponder analysis indicated that the differences between responders and nonresponders had very small effect sizes. Hence, we are confident that these small differences did not affect our findings.
A second limitation of the observational design with routine outcome measurement data is that the actual treatment may have deviated from these protocols based on the clinician’s expertise and patient’s preference despite our standardized treatment protocols. For example, there may be differences between patients in the number of hand therapy sessions or steroid injections. Although readers should be aware that the MICs we provided may be influenced by some variation in treatment strategies, these deviations are highly representative of actual daily practice, resulting in more generalizable MIC values.
Third, we only performed analyses on the effect of treatment invasiveness on the MIC. It is plausible that MICs also vary depending on cultural or sociodemographic characteristics [2]. To address this, two previous studies evaluated factors contributing to differences in MICs of several questionnaires in patients with adult spinal deformity [3, 46]. Interestingly, they demonstrated that MICs did not vary based on age or sex, whereas they found substantial differences based on the baseline severity [3]. Moreover, consistent with our findings, they found considerably higher MICs for surgical treatment than nonsurgical treatment on all questionnaires, suggesting that the invasiveness of the treatment may be a more influential factor than the sociodemographic characteristics [46].
Fourth, it is well-known that MICs can vary depending on the method used [24]. In this study, we only used anchor-based methods. Although the ideal method is still under discussion, anchor-based methods are generally preferred as these take into account relevant changes from the patient’s perspective [15, 29, 33, 40]. We determined the MIC with an anchor question assessing satisfaction with the treatment result. Some authors recommend using an anchor question that is based on a scale that rates the change in outcome measured on that specific outcome domain [33]. However, the MIC is defined as “the smallest change in an outcome measure that patients perceive as important” [9]. Considering this definition, we believe that satisfaction with the treatment result is an accurate measure of patients’ perceived improvement. This is also in line with prior studies in hand surgery, in which patient-reported satisfaction was commonly used as an anchor question [13, 18, 20, 21, 35]. However, by using this anchor question, we were unable to determine the MIC for all subdomains of all PROMs for all hand conditions because of a low correlation with the anchor question. This was primarily the case for the MHQ subdomain of aesthetics. Because the most profound complaints in these specific hand conditions are pain and difficulties with hand function, this subdomain might be irrelevant to these specific conditions, accounting for the low correlation with satisfaction.
Finally, we were unable to determine the smallest detectable change because patients were only asked to complete the PROMs once during the last measurement, which occurred post-treatment. Some MIC values we reported are low, and it is unclear whether these MIC values exceed the smallest detectable change for this specific outcome. This mostly occurred for nonsurgical treatments in combination with outcome domains that may not be the most relevant for these patients and where little improvement may be expected with treatment (for example, the VAS during load for nonsurgical treatment of cubital tunnel syndrome and MHQ hand function for nonsurgical treatment of CMC-1 osteoarthritis). However, as MICs should mainly be used to interpret clinically relevant changes on a group level, comparisons with the smallest detectable changes may be less important, because random measurement error may be canceled out at the group level [2].
MICs for Condition-Treatment Combinations
We found large differences in MICs for different condition-treatment combinations, indicating that MICs cannot be reliably applied to other condition-treatment combinations. This is in line with prior evidence, demonstrating substantial variation in MICs for different condition-treatment combinations. However, MICs for specific condition-treatment combinations are comparable to those reported in the evidence, including MICs for the BCTQ in patients undergoing carpal tunnel release [6] or cubital tunnel release [21] and for the MHQ in patients with a PIP prosthesis [22] or trigger finger release [13].
The comprehensive overview of MIC values provided in this study contributes to the application of more accurate MICs in clinical research, resulting in better treatment evaluations, which may improve patient counseling and management strategies [40]. For example, MICs can be used as a threshold to determine the percentage of patients reaching the MIC in clinical research. Insight into these percentages could aid clinicians in informing patients about the expected treatment results and may facilitate shared decision-making in clinical practice. However, although the percentage of patients reaching the MIC will probably be correct on a group level, this threshold may not apply to individual patients as all patients have an individual threshold of what they consider an important change. Therefore, it is highly recommended to use the MIC as a probabilistic value rather than a deterministic cutoff when applied to individual patients. Future studies may focus on adaptive techniques to achieve individualized MICs as proposed by Zhou et al. [47], which may ultimately aid clinicians in selecting the most appropriate treatment for individual patients.
MICs Vary with the Invasiveness of Treatment
The finding that MICs differ depending on the invasiveness of the intervention indicates that a more invasive treatment requires a larger improvement in these subdomains for patients to experience satisfaction with the treatment result. Patients receiving surgical treatment might experience more disability and discomfort from their treatment than patients receiving nonsurgical treatment. Consequently, patients treated nonsurgically may be more satisfied with their treatment result when they experience only a small improvement, resulting in a lower MIC.
Although it is plausible that the treatment invasiveness accounts for the variation in MICs, one might also suggest that differences in the groups being compared cause the variation. For example, the follow-up periods differed from 3 months for nonsurgical and minor surgical treatments to 12 months for major surgical treatments. A study in patients receiving decompression of ulnar neuropathy demonstrated that the MIC of the BCTQ was lower at 3 months than at 6 months [21]. However, they found no difference in the MIC at 6 and 12 months postoperatively, suggesting that the MIC is stable if the functional recovery period is reached. The follow-up periods we used in this study align with the International Consortium for Health Outcomes Measurement standard set for hand and wrist conditions, representing the clinical endpoints of the specific treatments [43]. Hence, despite differences in the follow-up periods between treatments, we believe these clinical endpoints are most suitable for assessing the final treatment effects.
In addition, another factor potentially contributing to these differences is variation in baseline characteristics [8, 42]. A study comparing the baseline characteristics of patients with CMC-1 osteoarthritis treated surgically and those treated nonsurgically found that surgically treated patients had worse baseline PROM scores, worse illness perceptions and catastrophization, and higher treatment expectations [44]. Although we only observed small differences in baseline scores between surgical and nonsurgical treatment groups, we did not take into account psychological characteristics and treatment expectations. It is plausible that patients with a worse psychological profile or higher treatment expectations may need more improvement to be satisfied with treatment results, resulting in a higher MIC. Future studies may examine factors contributing to these differences in MICs to improve expectation management for individual patients.
Conclusion
MICs differ between diagnosis-treatment combinations and particularly differ depending on the invasiveness of the intervention. These findings indicate that the MIC is context-specific and may be misleading if applied inappropriately. Hence, implementation of these condition-specific and treatment-specific MICs in clinical research allows for a better study design to achieve more accurate treatment evaluations. Consequently, this could aid clinicians in better informing patients about the expected treatment results and facilitate shared decision-making in clinical practice. Future studies may focus on adaptive techniques to achieve individualized MICs reflecting clinically relevant change to individuals instead of groups, which may ultimately aid clinicians in selecting the most appropriate treatment for individual patients.
Group Authors
Members of the Hand-Wrist Study Group include: Dirk-Johannes Jacobus Cornelis van der Avoort MD, Richard Arjen Michiel Blomme MD, Herman Luitzen de Boer MD, Gijs Marijn van Couwelaar MD, Jan Debeij MD, PhD, Jak Dekker MSc, Alexandra Fink PT, Klazina Paulina de Haas MD, Kennard Harmsen MD, Steven Eric Ruden Hovius MD PhD, Rob van Huis PT, Richard Koch MD, Alexander Kroeze MD, Thybout Matthias Moojen MD, PhD, Mark Johannes Willem van der Oest PhD, Pierre-Yves Alain Adriaan Pennehouat PT, Willemijn Anna de Ridder PT, MSc, Johannes Pieter de Schipper MD, Karin Schoneveld PT, MSc, Berbel Jeannee Rinel Sluijter MD, PhD, Jeronimus Maria Smit MD, PhD, Xander Smit MD, PhD, John Sebastiaan Souer MD, PhD, Marloes Hendrina Paulina ter Stege MSc, Johannes Frederikes Maria Temming MD, Joris Sebastiaan Teunissen BSc, Jeroen Hein van Uchelen MD, PhD, Joris Jan Veltkamp PT, Guus Maarten Vermeulen MD, PhD, Erik Taco Walbeehm MD, PhD, Oliver Theodor Zöphel MD, PhD, Jelle Michiel Zuidam
Acknowledgments
We thank all the patients who participated and allowed their data to be anonymously used for the present study. In addition, we thank all caregivers and personnel of Xpert Clinics, Handtherapie Nederland and Equipe Zorgbedrijven for assisting in the routine outcome measurements that are the basis for this manuscript.
Footnotes
Members of the Hand-Wrist Study Group are listed in an Appendix at the end of this article.
Each author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Ethical approval for this study was obtained from the Erasmus MC University Medical Center, Rotterdam, the Netherlands (MEC-2018-1088).
This work was performed at the Erasmus MC University Medical Center, Rotterdam, the Netherlands.
Contributor Information
Jaimy Emerentiana Koopman, Email: j.koopman@erasmusmc.nl.
Yara Eline van Kooij, Email: yaravk@hotmail.com.
Reinier Feitz, Email: r.feitz@xpertclinics.nl.
Caroline Anna Hundepool, Email: c.hundepool@erasmusmc.nl.
Chao Zhou, Email: zhou.chao@me.com.
Harm Pieter Slijper, Email: harm.slijper@gmail.com.
Ruud Willem Selles, Email: r.selles@erasmusmc.nl.
Robbert Maarten Wouters, Email: r.wouters@erasmusmc.nl.
Collaborators: Dirk-Johannes Jacobus Cornelis van der Avoort, Richard Arjen Michiel Blomme, Herman Luitzen de Boer, Gijs Marijn van Couwelaar, Jan Debeij, Jak Dekker, Alexandra Fink, Klazina Paulina de Haas, Kennard Harmsen, Steven Eric Ruden Hovius, Rob van Huis, Richard Koch, Alexander Kroeze, Thybout Matthias Moojen, Mark Johannes Willem van der Oest, Pierre-Yves Alain Adriaan Pennehouat, Willemijn Anna de Ridder, Johannes Pieter de Schipper, Karin Schoneveld, Berbel Jeannee Rinel Sluijter, Jeronimus Maria Smit, Xander Smit, John Sebastiaan Souer, Marloes Hendrina Paulina ter Stege, Johannes Frederikes Maria Temming, Joris Sebastiaan Teunissen, Jeroen Hein van Uchelen, Joris Jan Veltkamp, Guus Maarten Vermeulen, Erik Taco Walbeehm, Oliver Theodor Zöphel, and Jelle Michiel Zuidam
References
- 1.Angst F, Aeschlimann A, Angst J. The minimal clinically important difference raised the significance of outcome effects above the statistical level, with methodological implications for future studies. J Clin Epidemiol. 2017;82:128-136. [DOI] [PubMed] [Google Scholar]
- 2.Arima H, Carreon LY, Glassman SD, et al. Cultural variations in the minimum clinically important difference thresholds for SRS-22R after surgery for adult spinal deformity. Spine Deform. 2019;7:627-632. [DOI] [PubMed] [Google Scholar]
- 3.Bahadir S, Yuksel S, Ayhan S, et al. Variation of minimum clinically important difference by age, gender, baseline disability, and change of direction in adult spinal deformity population: Is it a constant value? World Neurosurg. 2021;146:e1171-e1176. [DOI] [PubMed] [Google Scholar]
- 4.Chung KC, Pillsbury MS, Walters MR, Hayward RA. Reliability and validity testing of the Michigan Hand outcomes Questionnaire. J Hand Surg Am. 1998;23:575-587. [DOI] [PubMed] [Google Scholar]
- 5.Cohen J. Statistical Power Analysis For The Behavioral Sciences . Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 6.De Kleermaeker F, Boogaarts HD, Meulstee J, Verhagen WIM. Minimal clinically important difference for the Boston Carpal Tunnel Questionnaire: new insights and review of literature. J Hand Surg Eur Vol. 2019;44:283-289. [DOI] [PubMed] [Google Scholar]
- 7.De Ridder WA, van Kooij YE, Vermeulen GM, et al. Test-retest reliability and construct validity of the Satisfaction with Treatment Result Questionnaire in patients with hand and wrist conditions: a prospective study. Clin Orthop Relat Res. 2021;479:2022-2032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Vet HC, Foumani M, Scholten MA, et al. Minimally important change values of a measurement instrument depend more on baseline values than on the type of intervention. J Clin Epidemiol. 2015;68:518-524. [DOI] [PubMed] [Google Scholar]
- 9.de Vet HC, Terwee CB, Ostelo RW, Beckerman H, Knol DL, Bouter LM. Minimal changes in health status questionnaires: distinction between minimally detectable change and minimally important change. Health Qual Life Outcomes. 2006;4:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fan J, Upadhye S, Worster A. Understanding receiver operating characteristic (ROC) curves. CJEM. 2006;8 1:19-20. [DOI] [PubMed] [Google Scholar]
- 11.Feitz R, van Kooij YE, Ter Stege MHP, et al. Closing the loop: a 10-year experience with routine outcome measurements to improve treatment in hand surgery. EFORT Open Rev. 2021;6:439-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kahl C, Cleland JA. Visual analogue scale, numeric pain rating scale and the McGill pain Questionnaire: an overview of psychometric properties. Physical Therapy Reviews. 2005;10:123-128. [Google Scholar]
- 13.Koopman JE, van Kooij YE, Selles RW, et al. Determining the minimally important change of the Michigan Hand outcomes Questionnaire in patients undergoing trigger finger release. J Hand Ther. Published online June 23, 2021. DOI: 10.1016/j.jht.2021.06.003. [DOI] [PubMed]
- 14.Leite JC, Jerosch-Herold C, Song F. A systematic review of the psychometric properties of the Boston Carpal Tunnel Questionnaire. BMC Musculoskelet Disord. 2006;7:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leopold SS, Porcher R. Editorial: The minimum clinically important difference - the least we can do. Clin Orthop Relat Res. 2017;475:929-932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leopold SS, Porcher R. Editorial: Threshold p values in orthopaedic research - we know the problem. What is the solution? Clin Orthop Relat Res. 2018;476:1689-1691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levine DW, Simmons BP, Koris MJ, et al. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J Bone Joint Surg Am. 1993;75:1585-1592. [DOI] [PubMed] [Google Scholar]
- 18.London DA, Stepan JG, Calfee RP. Determining the Michigan Hand outcomes Questionnaire minimal clinically important difference by means of three methods. Plast Reconstr Surg. 2014;133:616-625. [DOI] [PubMed] [Google Scholar]
- 19.MacDermid JC, Turgeon T, Richards RS, Beadle M, Roth JH. Patient rating of wrist pain and disability: a reliable and valid measurement tool. J Orthop Trauma. 1998;12:577-586. [DOI] [PubMed] [Google Scholar]
- 20.Maia MV, de Moraes VY, Dos Santos JB, Faloppa F, Belloti JC. Minimal important difference after hand surgery: a prospective assessment for DASH, MHQ, and SF-12. SICOT J. 2016;2:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Malay S, Group SUNS, Chung KC. The minimal clinically important difference after simple decompression for ulnar neuropathy at the elbow. J Hand Surg Am. 2013;38:652-659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marks M, Hensler S, Wehrli M, Schindele S, Herren DB. Minimal important change and patient acceptable symptom state for patients after proximal interphalangeal joint arthroplasty. J Hand Surg Eur Vol. 2019;44:175-180. [DOI] [PubMed] [Google Scholar]
- 23.Marks M, Rodrigues JN. Correct reporting and interpretation of clinical data. J Hand Surg Eur Vol. 2017;42:977-979. [DOI] [PubMed] [Google Scholar]
- 24.Mouelhi Y, Jouve E, Castelli C, Gentile S. How is the minimal clinically important difference established in health-related quality of life instruments? Review of anchors and methods. Health Qual Life Outcomes. 2020;18:136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ozyurekoglu T, McCabe SJ, Goldsmith LJ, LaJoie AS. The minimal clinically important difference of the Carpal Tunnel Syndrome Symptom Severity Scale. J Hand Surg Am. 2006;31:733-738. [DOI] [PubMed] [Google Scholar]
- 26.Packham T, MacDermid JC. Measurement properties of the Patient-Rated Wrist and Hand Evaluation: Rasch analysis of responses from a traumatic hand injury population. J Hand Ther. 2013;26:216-223. [DOI] [PubMed] [Google Scholar]
- 27.Page P. Beyond statistical significance: clinical interpretation of rehabilitation research literature. Int J Sports Phys Ther. 2014;9:726-736. [PMC free article] [PubMed] [Google Scholar]
- 28.Porter ME. What is value in health care? N Engl J Med. 2010;363:2477-2481. [DOI] [PubMed] [Google Scholar]
- 29.Revicki D, Hays RD, Cella D, Sloan J. Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J Clin Epidemiol. 2008;61:102-109. [DOI] [PubMed] [Google Scholar]
- 30.Rodrigues JN. Different terminologies that help the interpretation of outcomes. J Hand Surg Eur Vol. 2020;45:97-99. [DOI] [PubMed] [Google Scholar]
- 31.Schmitt JS, Di Fabio RP. Reliable change and minimum important difference (MID) proportions facilitated group responsiveness comparisons using individual threshold criteria. J Clin Epidemiol. 2004;57:1008-1018. [DOI] [PubMed] [Google Scholar]
- 32.Schrier VJ, Gelfman R, Amadio PC. Minimal clinically important difference is lower for carpal tunnel syndrome patients undergoing injection versus surgery. J Hand Surg Eur Vol. 2020;45:90-92. [DOI] [PubMed] [Google Scholar]
- 33.Sedaghat AR. Understanding the minimal clinically important difference (MCID) of patient-reported outcome measures. Otolaryngol Head Neck Surg. 2019;161:551-560. [DOI] [PubMed] [Google Scholar]
- 34.Selles RW, Wouters RM, Poelstra R, et al. Routine health outcome measurement: development, design, and implementation of the Hand and Wrist Cohort. Plast Reconstr Surg. 2020;146:343-354. [DOI] [PubMed] [Google Scholar]
- 35.Shauver MJ, Chung KC. The minimal clinically important difference of the Michigan Hand outcomes Questionnaire. J Hand Surg Am. 2009;34:509-514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sorensen AA, Howard D, Tan WH, Ketchersid J, Calfee RP. Minimal clinically important differences of 3 patient-rated outcomes instruments. J Hand Surg Am. 2013;38:641-649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Staunton H, Willgoss T, Nelsen L, et al. An overview of using qualitative techniques to explore and define estimates of clinically important change on clinical outcome assessments. J Patient Rep Outcomes. 2019;3:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Terluin B, Eekhout I, Terwee CB. The anchor-based minimal important change, based on receiver operating characteristic analysis or predictive modeling, may need to be adjusted for the proportion of improved patients. J Clin Epidemiol. 2017;83:90-100. [DOI] [PubMed] [Google Scholar]
- 39.Terluin B, Eekhout I, Terwee CB, de Vet HC. Minimal important change (MIC) based on a predictive modeling approach was more precise than MIC based on ROC analysis. J Clin Epidemiol. 2015;68:1388-1396. [DOI] [PubMed] [Google Scholar]
- 40.Terwee CB, Peipert JD, Chapman R, et al. Minimal important change (MIC): a conceptual clarification and systematic review of MIC estimates of PROMIS measures. Qual Life Res. 2021;30:2729-2754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344-349. [DOI] [PubMed] [Google Scholar]
- 42.Wang YC, Hart DL, Stratford PW, Mioduski JE. Baseline dependency of minimal clinically important improvement. Phys Ther. 2011;91:675-688. [DOI] [PubMed] [Google Scholar]
- 43.Wouters RM, Jobi-Odeneye AO, de la Torre A, et al. A standard set for outcome measurement in patients with hand and wrist conditions: consensus by the International Consortium for Health Outcomes Measurement Hand and Wrist working group. J Hand Surg Am. 2021;46:841-855 e847. [DOI] [PubMed] [Google Scholar]
- 44.Wouters RM, Vranceanu AM, Slijper HP, et al. Patients with thumb-base osteoarthritis scheduled for surgery have more symptoms, worse psychological profile, and higher expectations than nonsurgical counterparts: a large cohort analysis. Clin Orthop Relat Res. 2019;477:2735-2746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3:32-35. [DOI] [PubMed] [Google Scholar]
- 46.Yuksel S, Ayhan S, Nabiyev V, et al. Minimum clinically important difference of the health-related quality of life scales in adult spinal deformity calculated by latent class analysis: is it appropriate to use the same values for surgical and nonsurgical patients? Spine J. 2019;19:71-78. [DOI] [PubMed] [Google Scholar]
- 47.Zhou Z, Zhao J, Bisson LJ. Estimation of data adaptive minimal clinically important difference with a nonconvex optimization procedure. Stat Methods Med Res. 2020;29:879-893. [DOI] [PubMed] [Google Scholar]