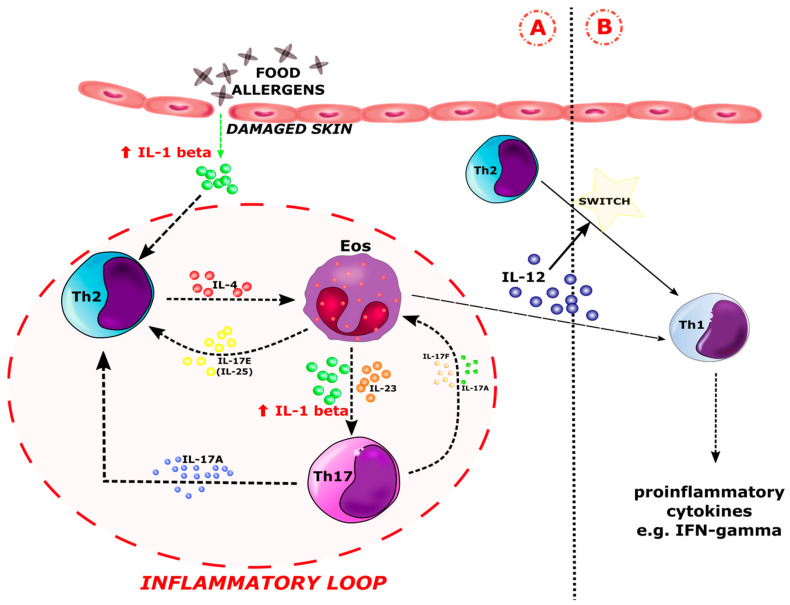
Figure 6.
Involvement of IL-1 beta in the inflammatory response in patients with food allergy (FA) and atopic dermatitis (AD). There is an increased concentration of IL-1 beta in (A) IgE-mediated hypersensitivity along the Th2 pathway, similar to the acute phase of AD. There are two possible sources of IL-1 beta. The first is damaged skin. In response to the contact of food allergens with damaged tissue, IL-1 beta is released, leading to the increased production of Th2 cells. On the other hand, IL-1 beta is produced and released by recruited eosinophils that migrate to inflammatory sites in response to type 2 cytokines, e.g., IL-4 [89]. Increased concentration of IL-1 beta leads to the polarization of naive Th cells into the Th17 lineage. The resulting Th17 lymphocytes release the cytokines IL-17A and IL-17F, which affect both the Th2 cells and the eosinophils. In addition to IL-1 beta, eosinophils release, among others, IL-25 (IL-17E), which enhances the production of Th2 inflammatory mediators. The interaction of Th2 cells, eosinophils, and Th17 via their cytokines drives the inflammatory loop. The inflammatory loop is marked with a dashed red line. IL-1 beta is the major initiator of the inflammatory loop cascade (A). Otherwise, eosinophils are able to switch between the Th2 and Th1 pathway via IL-12. It is the site of transition for (B) delayed food allergy along the Th1 pathway, similar to chronic AD. Eos–eosinophil; Th2–type 2 helper T cell; Th17–type 17 helper T cell; Th1–type 1 helper T cell.