Abstract
Introduction:
COVID-19 requires methods for screening patients that adhere to physical distancing and other Centers for Disease Control and Prevention guidelines. There is little data on the use of on-demand telehealth to meet this need.
Methods:
The functional performance of on-demand telehealth as a COVID-19 remote patient screening approach was conducted by analysing 9270 patient requests.
Results:
Most on-demand telehealth requests (5712 of 9270 total requests; 61.6%) had a visit reason that was likely COVID-19 related. Of these, 79.1% (4518 of 5712) resulted in a completed encounter and 20.9% (1194 of 5712) resulted in left without being seen. Of the 4518 completed encounters, 19.1% were referred to an urgent care centre, emergency department or COVID-19 testing centre. The average completed encounter wait time was 26.5 min and the mean visit length was 8.8 min. For patients that completed an encounter 42.8% (1935 of 4518) stated they would have sought in-person care and 9.1% stated they would have done nothing if on-demand telehealth was unavailable.
Discussion:
On-demand telehealth can serve as a low-barrier approach to screen patients for COVID-19. This approach can prevent patients from visiting healthcare facilities, which reduces physical contact and reduces healthcare worker use of personal protective equipment.
Keywords: Telehealth, COVID-19, pandemic, screening
Introduction
On-demand telehealth, also called direct-to-consumer telehealth, provides patients with unscheduled access to a synchronous video and audio clinical encounter.1 Telehealth enables the safe screening and care of patients without physical contact or close proximity. This clinical modality decreases exposure of patients to each other and to healthcare staff, reduces use of personal protective equipment for clinicians and conforms to public health recommendations on physical distancing.2,3 On-demand telehealth enables care to be rendered in situations where patients have been told to stay at home or shelter in place. It also decreases a potentially frustrating occurrence of patients arriving at sites of care expecting to be tested for COVID-19 and being told they do not meet stringent criteria for testing given limited availability.4
However, there is little published on the functional performance of on-demand telehealth as an approach to remote patient screening. We analysed data from a large-scale on-demand telehealth programme that was offered through a healthcare system, using a commercial platform, at no cost to patients in the Mid-Atlantic region (Maryland, Virginia, and the District of Columbia) of the United States during the COVID-19 pandemic. The service was advertised through the healthcare system’s websites and through community health teams to reach specific populations in need. A telehealth encounter involved the patient enrolling in a telehealth application, requesting care, being placed in a virtual waiting room, receiving care from a provider by video and being dispositioned. Our descriptive analysis covers telehealth patient characteristics, measures of patient wait time and visit duration, technical success of the telehealth request and the post-visit trajectory of these patients.
Methods
On-demand telehealth requests made between 13 March 2020 to 3 April 2020 were analysed with a focus on those likely to be related to COVID-19. Each telehealth request was categorized by the patient’s stated reason for visit as likely COVID-19 related if it included any explicit mentions of ‘COVID’, ‘coronavirus’ or a variation of those terms or visit reasons that stated any of the symptoms that may be COVID-19 related, such as shortness of breath, fever, cough, flu like symptoms, bronchitis, pneumonia, congestion, upper respiratory infection, stuffy nose, hyperventilating and/or allergies. Each request was categorized as either a completed encounter in which the patient successfully saw the provider and was given clinical guidance, or an incomplete request in which the patient did not complete an encounter with the provider. Incomplete requests are referred to as ‘left without being seen’, a standard marker of operational performance for in-person acute care.5 Requests were completed by a physician (typically emergency medicine or primary care), physician assistant or nurse practitioner.
For completed encounters additional analyses were performed. These included analysis of the disposition of patients referred (called referrals) for in-person care to either an urgent care centre or emergency department or directly to a COVID-19 testing site. Patient wait time was measured as the moment the patient enters the virtual waiting room upon requesting care to the moment the patient is seen by the provider. Visit duration was measured as the time the patient and provider spent connected by video, not including any documentation or other work done by the provider outside of the video time. Following a completed encounter the patient was surveyed to determine what the patient would have done if on-demand telehealth was unavailable. The patient could choose not to respond or select one of the following options: go to an urgent care or retail clinic, the emergency department, my doctor’s office, or do nothing.
Patients may have multiple telehealth requests. We report at the level of requests, even if from the same patient, with unique patient count reported only as appropriate. This study was approved by the MedStar Health Research Institute institutional review board. The datasets analysed during the current study are available from the corresponding author on reasonable request.
Results
From 13 March to 3 April 2020 there were 9270 on-demand telehealth requests from 7112 unique patients. Average patient age was 38.6 years (standard deviation (SD) 14.9), 4511 (63.4%) were female and 2601 (36.6%) were male (Table 1). Patients under the age of 18 years could make a request under an account created by their parent or legal guardian. Most requests (5712 of 9270 total requests; 61.6%) had a visit reason categorized as likely COVID-19 related; 51% of these explicitly stated a variation of COVID-19 (2915 of 5712 total likely COVID-19 related requests) and the remaining requests described a COVID-19 related symptom.
Table 1.
Age and sex of all unique patient requests for on-demand telehealth visits.
| Patient age (y) | Female: count (%) | Male: count (%) | All patients: count (%) |
|---|---|---|---|
| Under 18 | 159 (2.2%) | 179 (2.5%) | 338 (4.7%) |
| 18–30 | 1290 (18.1) | 708 (10) | 1998 (28.1) |
| 31–40 | 1308 (18.4) | 753 (10.6) | 2061 (29) |
| 41–50 | 761 (10.7) | 425 (6) | 1186 (16.7) |
| 51–60 | 603 (8.5) | 346 (4.9) | 949 (13.3) |
| 61+ | 390 (5.5) | 190 (2.7) | 580 (8.2) |
| Total requests | 4511 (63.4) | 2601 (36.6) | 7112 (100) |
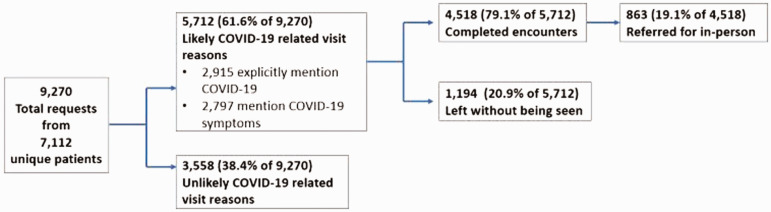
The majority (4518 of 5712 total likely COVID-19 related requests; 79.1%) of likely COVID-19 related requests were completed encounters and of these 19.1% (863 of 4518 total completed likely COVID-19 requests) were referred for in-person care or testing (Figure 1). The average completed encounter wait time was 26.5 min (median = 20.6, SD = 23.6, range = 268.8) and mean visit length was 8.8 min (median = 8, SD = 4.6, range = 45.3). There were 1194 requests (1194 of 5712 total likely COVID-19 related requests; 20.9%) that were categorized as left without being seen. Patients that left without being seen waited an average of 19.4 min before leaving (median = 13.13, SD = 21.3, range = 242); significantly less time than patients that were seen (1193) = –9.5, p <.001.
Figure 1.
Likely COVID-19 encounter trajectory.
Post completed encounter survey results indicated that if on-demand telehealth was unavailable 26.3% (1186 of 4518 completed likely COVID-19 related encounters) of patients would have gone to an urgent care or retail clinic, 10.7% (482) to their doctor’s office and 5.9% (267) to the emergency department. Four hundred and fifteen (9.1%) stated they would not have done anything. There was no response from 48% of completed encounters (2168 of 4518 completed likely COVID-19 encounters).
Discussion
We found that on-demand telehealth service at no cost to the patient can serve an important public health need in response to the COVID-19 pandemic with 61.6% of all telehealth request reasons being categorized as likely COVID-19 related. Average patient wait time was under 30 min and visit duration was under 9 min, providing convenient, low-barrier access to providers. Based on the survey asking what patients would have done had they not had access to on-demand telehealth, 1935 (42.8% of the 4518 COVID-19 related requests) COVID-19 completed encounters responded they would have sought in-person care. These patients who would have visited a healthcare facility, risking personal exposure, potentially exposing health care workers and diminishing supplies of personal protective equipment, were cared for in their homes in the first few weeks of this pandemic. There were also several COVID-19 related patients (9.1%) who stated they would have done nothing about their concerns. On-demand telehealth service met this population’s needs.
The referral rate for in-person care was 19.1%, which is considerably higher than our historical experience of referral to care, but the visit reasons, including concerns such as shortness of breath and chest pain, are of higher acuity than the historical experience of on demand telehealth and a direct order for testing has not typically been an available disposition.
The number of encounters that were categorized as left without being seen was 1194 or 20.9%; however, it should be noted that this stemmed from 557 unique patients. There is no widely agreed upon benchmarking for on-demand telehealth left without being seen as there is for in-person acute care settings such as urgent care centres and emergency departments. The high number of requests ending in left without being seen is likely because certain patients would log on and off the platform in search of short wait times that fitted their schedules. Our quality and safety process included follow-up outreach phone calls the next day to these patients.
Our study has several limitations. We did not analyse patient characteristics such as race, whether the patient had insurance or how the patient learned about the on-demand service. The reason for visit categorization as COVID-19 likely when COVID-19 was not explicitly mentioned is based on symptoms that may align with other conditions. Providers were given guidance to screen all patients with COVID-19 related symptoms for risk of COVID-19, so it is possible that patients who were not self-identifying as at risk were screened and categorized that way. Our analysis did not look at variability in referrals by provider. Finally, the reason for referral for in-person care was not analysed, we did not analyse whether referred patients were seen at the location they were referred to, and we did not analyse whether patients were tested and the test outcome.
Authors contribution
RR led the conceptualization, data analysis, and first draft of the manuscript. All authors supported conceptualization and review of the manuscript. AF and EB support data analysis.
Footnotes
Declaration of conflicting interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Raj M Ratwani https://orcid.org/0000-0002-8623-6123
References
- 1.Speedie SM, Ferguson AS, Sanders J, et al. Telehealth: The promise of new care delivery models. Telemed J E Health 2008; 14: 964–967. [DOI] [PubMed] [Google Scholar]
- 2.Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID-19. N Engl J Med2020; 382: 1679–1681. [DOI] [PubMed]
- 3.Bachireddy C, Chen C, Dar M. Securing the safety net and protecting public health during a pandemic: Medicaid’s response to COVID-19. JAMA. Epub ahead of print 19 March 2020. DOI: 10.1001/jama.2020.4272. [DOI] [PubMed]
- 4.Mehrotra A.The convenience revolution for treatment of low-acuity conditions. JAMA 2013; 310: 35–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hsia RY, Asch SM, Weiss RE, et al. Hospital determinants of emergency department left without being seen rates. Ann Emerg Med 2011; 58: 24–32. [DOI] [PMC free article] [PubMed] [Google Scholar]