Abstract
Background
Synovial chondromatosis (SC) of the shoulder is rare, with limited literature on its management. This systematic review of literature aimed to characterize common arthroscopic techniques for the treatment of shoulder SC and patient outcomes. We hypothesized that arthroscopy is an effective operative modality for the management of shoulder SC.
Methods
PubMed and Embase databases were searched for articles on arthroscopic management of shoulder SC, published before 6 August 2020. All articles meeting inclusion criteria received an independent full-text review by two authors.
Results
An initial search found 64 articles. Following duplicate removal and title, abstract, and full-text reviews, 27 articles (48 patients) remained eligible. The mean age of patients was 33.0 years, with 2:1 male-to-female ratio. The mean follow-up was 41.8 months. SC was found to affect various intra- and extra-articular locations of the shoulder. Overall, arthroscopic treatment of shoulder SC was successful in 70.8%. Treatment failure was common in SC involving the bicipital tendon sheath. Disease recurrence was seen in 14.7%.
Conclusion
Literature on arthroscopic management of shoulder SC is limited, and significant heterogeneity in arthroscopic techniques was observed. Although arthroscopic management of shoulder SC is effective, further optimization is necessary to minimize treatment failure and disease recurrence.
Keywords: Synovial chondromatosis, shoulder, arthroscopy, arthroscopic, management
Introduction
Synovial chondromatosis (SC) is a rare, benign monoarticular disease of synovial joints that affects males two to three times more commonly than females.1–3 SC is characterized by the presence of cartilaginous loose bodies in the involved joint, bursa or tendon sheath4,5 that cause pain, decreased range of motion (ROM), intermittent catching/locking, and/or crepitation.6 Larger loose bodies can cause erosion of the surrounding cartilage and may lead to early-onset osteoarthritis.1,7 The knee (70%) and the hip (20%) joints are most commonly involved, with less frequent involvement of the elbow, wrist, ankle, and shoulder.3
The exact pathogenesis of SC is yet to be elucidated; however, it is commonly believed that synovial cells undergo chondrocytic metaplasia to produce small nodules of cartilage that detach to form multiple loose bodies in the affected tissue.3 These loose bodies may subsequently undergo endochondral ossification, leading to osteochondromatosis.8 In severe cases, SC can lead to the formation of over 100 loose bodies.7
Classically, the mainstay treatment for SC of the shoulder has been open arthrotomy and removal of loose bodies, followed by either complete synovectomy, or partial synovectomy removing the affected tissue.7 With advances in sports medicine and arthroscopic surgical techniques in recent decades, arthroscopy has become a viable modality for the treatment of shoulder SC that may potentially reduce post-operative morbidity.9 However, due to the rarity of SC of the shoulder, no study has compared the patient outcomes between open versus arthroscopic approaches to date. In addition, scarcity of literature surrounding arthroscopic management of SC of the shoulder poses a significant challenge to orthopedic surgeons when deciding on an optimal treatment approach for patients with SC of the shoulder.
In the current study, we performed a systematic review of literature for arthroscopic management of SC of the shoulder to characterize commonly used arthroscopic surgical techniques and patient outcomes. We hypothesized that arthroscopy is an effective operative modality for the management of SC of the shoulder with high success and low complication and recurrence rates.
Methods
Two authors (JPP and YM) independently performed PubMed and Embase database searches for articles relating to arthroscopic management of SC of the shoulder, published on or before 5 August 2020. The following subject headings and their related key terms were used: “synovial chondromatosis,” “arthroscopy,” “shoulder.”
Inclusion criteria for the systematic review consisted of: (1) all levels of evidence, (2) patients of all ages, (3) SC of the shoulder, and (4) English language of publication. Exclusion criteria included: (1) review articles, (2) surgical technique articles, (3) non-arthroscopic management (i.e. conservative management or open surgery), (4) articles available in abstract form only, and (5) SC involving joints other than the shoulder.
Title and abstract of articles were independently screened by the two authors for their eligibility for inclusion. Articles deemed to meet the criteria received a full-text review by the same two authors independently to ensure that the articles meet the outlined inclusion and exclusion criteria. Subsequently, relevant information from the included studies were retrieved and entered into a Microsoft Excel spreadsheet (Microsoft Excel for Mac, Version 16.4, Microsoft, Redmond, WA, USA). These included journal/article information (authors, year of publication, study design, level of evidence, sample size), patient demographics and clinical characteristics (age, gender, affected side, clinical features, primary tissue affected, location of the lesion), procedure characteristics (intraoperative patient positioning, arthroscopic portals, procedure), and post-operative data (duration of follow-up, patient outcomes, complications, recurrence).
Success rate of arthroscopic treatment, defined as complete excision of loose bodies and affected synovium intra-operatively without the need for conversion to open surgery, was the primary outcome, while recurrence rate was the secondary outcome. Due to the heterogeneity across the studies found, meta-analysis was not feasible; instead, a qualitative assessment was performed.
Results
Systematic review and article characteristics
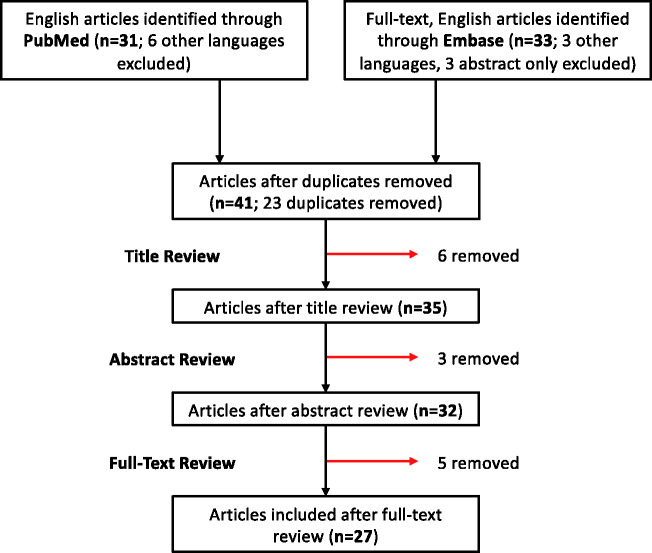
Upon search of PubMed and Embase databases, a total of 64 articles were found. Of these, 23 articles were duplicates and were thus removed. The resulting 41 articles underwent title and abstract review, which led to exclusion of 6 and 3 articles, respectively. After excluding 5 additional articles after full-text review, 27 articles were included in our final review (Figure 1). The two reviewers (JPP and YM) had no disagreements throughout all stages of the systematic review. Among the 27 articles, 23 were case reports (Table 1) and 4 were case series (Table 2). All articles were of level IV evidence. A total of 48 cases were presented in these articles.
Figure 1.
Flowchart of the article screening process and studies included in the systematic review.
Table 1.
Summary of the 23 case reports (23 patients) included in the systematic review.
| Article characteristics |
Patient demographics and clinical characteristics |
Procedure characteristics |
Post-operative data |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author/Year | Study design (level of evidence) | Sample size (n) | Mean age (years) | Gender | Side | Clinical features | Primary tissue affected | Location | Position | Portals | Procedure | Follow-up (months) | Outcome | Complications | Recurrence |
| Aydogan et al. (2013)10 | Case Report (IV) | 1 | 48 | M | R | Pain, decreased ROM, associated anterior labral tear | Synovium | Subacromial bursa, subdeltoid region | Beach chair | P, A, L | ELB, subacromial bursectomy, labral tear repair | 6 | Full ROM, RTW | No | No |
| Buess and Friedrich (2001)11 | Case Report (IV) | 1 | 22 | M | R | Pain × 5 years | Synovium | Axillary recess, subscapular recess, BTS | NR | NR | Conversion to ventral arthrotomy, ELB, partial synovectomy, BTS decompression | 12 | Failed arthroscopic treatment Asymptomatic, full ROM, RTW | No | No |
| Chillemi et al. (2005)12 | Case Report (IV) | 1 | 18 | M | R | Pain × 1 year, stiffness, decreased ROM | Synovium | GHJ, subscapular recess, BTS | NR | P, A | ELB, partial synovectomy, bicipital tendon synovectomy | 24 | Asymptomatic | No | No |
| Colanese et al. (2016)13 | Case Report (IV) | 1 | 44 | F | L | Pain × 7 years, decreased ROM, rotator cuff atrophy | Synovium | GHJ, subscapular recess | NR | NR | Conversion to limited open deltopectoral approach, ELB | 6 | Failed arthroscopic treatment Asymptomatic, full ROM | No | No |
| Covall and Fowble (1993)14 | Case Report (IV) | 1 | 22 | M | L | Pain × 1 year | Synovium | GHJ | NR | NR | ELB, partial synovectomy | 18 | Near asymptomatic | No | Yes |
| David and Drez (2000)15 | Case Report (IV) | 1 | 23 | F | R | Pain × 1 month, stiffness, decreased ROM | Synovium | GHJ, subscapular recess, BTS | NR | P, A | ELB, partial synovectomy, open decompression of BTS | 24 | Failed arthroscopic treatment Asymptomatic | No | No |
| Duymus et al. (2015)1 | Case Report (IV) | 1 | 33 | F | R | Pain × 4 years, decreased ROM | Synovium | GHJ | Beach chair | P, A-S, A-I | ELB, partial synovectomy | 12 | Asymptomatic, full ROM | No | No |
| Fowble and Levy (2003)9 | Case Report (IV) | 1 | 24 | M | L | Pain × 10 years, palpable loose bodies, decreased ROM | Synovium | GHJ, subscapular recess, BTS | Beach chair | P, A-S, A-I | ELB, partial synovectomy, debridement of degenerative labrum | NR | Minimal pain, improved ROM, RTW | No | No |
| Francesca and Ronquillo (2018)16 | Case Report (IV) | 1 | 23 | M | R | Pain × 2 years, stiffness, palpable solid masses, decreased ROM | Synovium | GHJ, subcoracoid space, biceps tract distal to the bicipital groove | NR | NR | ELB, partial synovectomy, conversion to open deltopectoral approach, capsular shift | 12 | Failed arthroscopic treatment Constant score: 90 (post-op) vs. 45 (pre-op), ASES score: 98 (post-op) vs. 20 (pre-op) | No | No |
| Fukuda et al. (2020)17 | Case Report (IV) | 1 | 13 | M | R | Pain, locking, effusion | Synovium | Axillary recess, subscapular recess | Beach chair | P, A | ELB, partial synovectomy | 60 | Asymptomatic | No | No |
| Hamada et al. (2005)18 | Case Report (IV) | 1 | 14 | F | R | Pain × 1.5 years, catching | Synovium | GHJ, axillary recess, subscapular recess | NR | NR | ELB | 36 | Asymptomatic | No | No |
| Jeon et al. (2004)19 | Case Report (IV) | 1 | 15 | F | L | Pain, decreased ROM, grinding, catching | Synovium | Rotator interval, subscapular recess, BTS | NR | P, A | ELB, partial synovectomy, BTS decompression | 18 | Asymptomatic, full ROM | No | Yes |
| Jimenez-Martin et al. (2014)2 | Case Report (IV) | 1 | 53 | M | NR | Pain, decreased ROM | Synovium | Labrum, subacromial bursa | NR | NR | ELB, partial synovectomy, subacromial bursectomy | 24 | Asymptomatic, full ROM | No | No |
| Jung et al. (2007)20 | Case Report (IV) | 1 | 19 | M | L | Pain × 6 months, decreased ROM | Synovium | Subscapular recess, axillary recess | NR | P, A | ELB, partial synovectomy | 12 | Asymptomatic, RTW | No | No |
| Maier et al. (2014)21 | Case Report (IV) | 1 | 26 | M | R | Pain, decreased ROM | Synovium | GHJ, subscapular recess, BTS | Lateral decubitus | P, A-S, A-I | ELB, partial synovectomy | 3 | Asymptomatic, Constant score: 100 (post-op) vs. 91 (pre-op) | No | No |
| Park et al. (2007)8 | Case Report (IV) | 1 | 45 | M | R | Pain × 3 years | Synovium | Subacromial bursa | Beach chair | P, A, L | ELB, partial subacromial bursectomy | 16 | Asymptomatic, RTW | No | No |
| El Rassi et al. (2015)22 | Case Report (IV) | 1 | 57 | F | L | Discomfort × 9 years, swelling, decreased ROM | Synovium | Subacromial space | Beach chair | P, A, L | ELB, complete synovectomy, CA ligament resection, acromioplasty | 12 | Full ROM | No | No |
| Raval et al. (2016)7 | Case Report (IV) | 1 | 52 | M | L | Pain × 3 years, clicking, grinding, decreased ROM | Synovium | GHJ | Beach chair | P, A, A-S, P-L | ELB, synovectomy | 3 | Asymptomatic, full ROM | No | No |
| Richman and Rose (1990)23 | Case Report (IV) | 1 | 35 | M | R | Pain × 15 years, clicking, decreased ROM | Synovium | GHJ, subscapular recess, BTS | NR | P, A | ELB, partial synovectomy, debridement of degenerative labrum | 24 | Asymptomatic, full ROM, RTW | No | No |
| Tokis et al. (2007)24 | Case Report (IV) | 1 | 24 | M | R | Pain × 6 months, decreased ROM | Synovium | GHJ, BTS | Beach chair | P, A, S, I | ELB, partial synovectomy | 12 | Asymptomatic, full ROM, RTW | No | No |
| Wahab et al. (2019)3 | Case Report (IV) | 1 | 20 | M | R | Pain × 2 years | Synovium | GHJ, subacromial space, proximal medial humerus | NR | NR | ELB, partial synovectomy | 24 | Asymptomatic, full ROM | No | No |
| Witwity et al. (1991)25 | Case Report (IV) | 1 | 62 | M | R | Pain × 3 years, swelling, locking, decreased ROM | Synovium | GHJ, subacromial space | Lateral decubitus | NR | ELB, partial synovectomy | 15 | Asymptomatic, improved ROM | No | No |
| Xu et al. (2015)26 | Case Report (IV) | 1 | 40 | F | R | Pain × 4 years, decreased ROM | Synovium | Subacromial space | Lateral decubitus | P, A, A-S | ELB, subacromial bursa partial synovectomy, acromioplasty | 14 | Asymptomatic, full ROM | No | No |
A: anterior; A-I: anteroinferior; A-S: anterosuperior; BTS: bicipital tendon sheath; ELB: excision of loose bodies; GHJ: glenohumeral joint; I: inferior; L: lateral; NR: not reported; P: posterior; P-L: posterolateral; ROM: range of motion; RTW: return to work; S: superior. Bold indicates the cases that had failed arthroscopic management.
Table 2.
Summary of the four case series (25 patients) included in the systematic review.
| Article characteristics |
Patient demographics and clinical characteristics |
Procedure characteristics |
Post-operative data |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author/Year | Study design (level of evidence) | Sample size (n) | Mean age (years) | Gender | Side | Clinical features | Primary tissue affected | Location | Position | Portals | Procedure | Follow-up (months) | Outcome | Complications | Recurrence |
| Lunn et al. (2007)4 | Retrospective case series (IV) | 15 | 40 | M | NR | Pain (93%), locking (40%), decreased ROM (40%) | Synovium | NR | Beach chair | P, A, + /– accessory portals PRN | ELB, anterior release | 63.6 (27.6–198) | Constant score: improvement in pain (11.3 post-op vs. 8.9 pre-op) and ADLs (18.7 post-op vs. 12.9 pre-op) | Arthritis (severe) | No |
| 28 | F | Synovium | Beach chair | 1) ELB + synovectomy 2) ELB + synovectomy 3) ELB 4) synovectomy + tenodesis | Incomplete excision of loose bodies | Yes (3 years post-op) | |||||||||
| 27 | F | Synovium | Beach chair | 1) ELB 2) ELB + synovectomy + tenodesis | Arthritis (mild) | No | |||||||||
| 18 | F | Synovium | Beach chair | ELB, synovectomy, tenodesis | Arthritis (mild) | No | |||||||||
| 34 | F | Synovium | Beach chair | ELB, synovectomy | Incomplete excision of loose bodies | No | |||||||||
| 18 | F | Synovium | Beach chair | ELB, synovectomy, tenodesis | No | No | |||||||||
| 19 | F | Synovium | Beach chair | 1) ELB 2) ELB + synovectomy 3) ELB + synovectomy | Arthritis (mild) | Yes (12 years post-op) | |||||||||
| 41 | M | Synovium | Beach chair | ELB | Arthritis (moderate) | No | |||||||||
| 42 | M | Synovium | Beach chair | ELB, synovectomy, tenodesis | Arthritis (severe) | No | |||||||||
| 42 | M | Synovium | Beach chair | ELB, synovectomy | Arthritis (moderate) | No | |||||||||
| 33 | F | Synovium | Beach chair | ELB, synovectomy, tenodesis | Arthritis (severe) | No | |||||||||
| 20 | M | Synovium | Beach chair | 1) ELB 2) ELB | Incomplete excision of loose bodies, arthritis (mild) | No | |||||||||
| 49 | M | Synovium | Beach chair | ELB, synovectomy | Arthritis (moderate) | No | |||||||||
| 47 | M | Synovium | Beach chair | ELB, synovectomy | No | No | |||||||||
| 41 | M | Synovium | Beach chair | ELB, synovectomy, tenodesis | Arthritis (severe) | No | |||||||||
| Ranalletta et al. (2009)27 | Case series (IV) | 3 | 35 | M | R | Pain × 2 years, decreased ROM | Synovium | GHJ | NR | NR | ELB, partial synovectomy | 59 | Significant improvements in shoulder ROM, patient satisfaction, VAS, UCLA, DASH, Constant scores | No | No |
| 29 | M | L | Pain × 5 years, stiffness, decreased ROM | Synovium | GHJ | NR | NR | ELB, partial synovectomy, arthroscopic capsulotomy, subacromial bursa adhesiolysis | 28 | Significant improvements in shoulder ROM, patient satisfaction, VAS, UCLA, DASH, Constant scores | No | No | |||
| 24 | M | R | Pain, stiffness, locking × 14 years, decreased ROM, severe deltoid and biceps atrophy | Synovium | GHJ | NR | NR | ELB, partial synovectomy, arthroscopic capsulotomy | 26 | Significant improvements in shoulder ROM, patient satisfaction, VAS, UCLA, DASH, Constant scores | No | No | |||
| Urbach et al. (2008)28 | Case series (IV) | 5 | 28 | M | L | Pain, decreased ROM | Synovium | NR | Lateral decubitus | P, A | ELB, partial synovectomy | 108 | Constant score: 96 (post-op) vs. 100 (unaffected side) | No | No |
| 30 | M | L | Synovium | NR | Lateral decubitus | 108 | Constant score: 100 (post-op) vs. 100 (unaffected side) | No | Yes | ||||||
| 22 | M | R | Synovium | NR | Lateral decubitus | 96 | Constant score: 100 (post-op) vs. 100 (unaffected side) | No | Yes | ||||||
| 30 | M | R | Synovium | NR | Lateral decubitus | 84 | Constant score: 98 (post-op) vs. 100 (unaffected side) | No | No | ||||||
| 34 | F | R | Synovium | NR | Lateral decubitus | 48 | Constant score: 91 (post-op) vs. 100 (unaffected side) | No | No | ||||||
| Utashima et al. (2020)5 | Case series (IV) | 2 (of 10 underwent arthroscopic management | 57 | F | NR | Pain × 1 year | Synovium | GHJ, bicipital groove | Beach chair | P, A | ELB | 36 | Constant score: 78 (post-op) vs. 65 (pre-op) | No | No |
| 65 | M | NR | Pain × 6 months | Synovium | Subacromial space | Beach chair | P, L | ELB, acromioplasty | 30 | Constant score: 90 (post-op) vs. 58 (pre-op) | No | No | |||
A: anterior; A-I: anteroinferior; A-S: anterosuperior; BTS: bicipital tendon sheath; ELB: excision of loose bodies; GHJ: glenohumeral joint; I: inferior; L: lateral; NR: not reported; P: posterior; P-L: posterolateral; PRN: as needed; ROM: range of motion; RTW: return to work; S: superior. ADL: activity of daily living; DASH: the disabilities of the arm, shoulder and hand score; UCLA: The University of California Los Angeles shoulder rating scale; VAS: visual analog score. Bold indicates the cases that had failed arthroscopic management.
Patient demographics and clinical characteristics
The mean age of patients was 33.0 years (range = 13–65). Thirty-two (67%) patients were male while 16 (33%) were female. Among patients with affected side reported (n = 30), 20 (66.7%) developed SC in their right shoulder, while 10 (33.3%) developed the disease in their left shoulder.
Pain was the most common presenting symptom, seen in 47 (97.9%) patients, followed by decreased ROM (n = 31; 64.5%), mechanical symptoms including locking, catching and grinding (n = 13; 27%) and shoulder stiffness (n = 5; 10.4%). In few cases, there were palpable solid masses (n = 2; 4.2%), swelling (n = 2; 4.2%), and muscle atrophy (n = 2; 4.2%).
In all cases, synovium was the primarily affected tissue. Glenohumeral joint (GHJ) was the most commonly affected location (n = 19; 39.6%), followed by subscapular recess (n = 12; 25.0%), bicipital tendon sheath (BTS; n = 9; 18.8%), and subacromial space (n = 5; 10.4%). Axillary recess and subacromial bursa were involved in four (8.3%) and three (6.3%) cases, respectively. There were various, less frequently affected locations (Tables 1 and Table 2). Affected location was not specified in 20 (41.7%) cases.
Procedure characteristics
Thirty-three cases (68.8%) had intraoperative patient positioning reported. Among these, beach chair position was the preferred patient position, used in 75.8% (n = 25) of cases. Lateral decubitus position was used in the remaining 24.2% (n = 8) of cases.
Posterior and anterior was the most common arthroscopic portal setup (n = 12; 32.4%). Other arthroscopic portal setups included posterior, anterior and lateral (n = 3; 8%), and posterior, anterosuperior and anteroinferior (n = 3; 8%). One study with 15 patients (40.5%) reported employing posterior, anterior, and accessory portals as needed; however, the accessory portals used in each case were not specified. Portal setups were not reported in 11 cases (22.9%). Four other portal setups were used with one patient in each case (Tables 1 and 2).
In all cases (n = 48), excision of loose bodies was performed. In addition, synovectomy was performed in 39 cases (81.3%). Among these, 25 (52.1%) were partial synovectomy, 1 (2.1%) was complete synovectomy, and 13 (27.1%) were synovectomy without specification of partial or complete. Biceps tenodesis was performed in seven cases (14.6%). In a small number of cases, other procedures were also indicated, such as acromioplasty, subacromial bursectomy, debridement of degenerative labrum, decompression of BTS, and capsulotomy (Tables 1 and 2).
Clinical outcomes and recurrences
Arthroscopic treatment of SC of the shoulder was successful in 34 (70.8%) cases. Fourteen (29.2%) cases had failed arthroscopic treatment, in which three (6.3%) were converted to open surgery, two (4.2%) required partial open surgery for SC involving the BTS, seven (14.6%) required open biceps tenodesis, and three (6.3%) had incomplete excision of loose bodies as seen on early postoperative radiographs. One of the patients had both open biceps tenodesis and incomplete excision of loose bodies.
Among 47 patients with reported duration of follow-up, the mean follow-up duration was 41.8 months (range = 3–108 months). One patient did not have a reported duration of follow-up; however, his post-operative outcomes were reported. Therefore, among 48 patients, disease recurrence was seen in 6 patients (12.5%). Among 34 patients with successful arthroscopic treatment as defined previously, 5 (14.7%) developed recurrence of disease.
Discussion
Surgical excision of loose bodies and synovectomy is the mainstay treatment for SC.3 Historically, this was achieved through open arthrotomy followed by retrieval of visible loose bodies, irrigation, and “milking” to further evacuate loose bodies from locations that are difficult to visualize and/or access.9,29 Despite the historical preference, the success rate or recurrence rate following open arthrotomy for the treatment of SC is poorly reported, likely due to the relative rarity of SC involving the shoulder joint. In recent decades, arthroscopy has been successfully adopted to treat various orthopedic sports injuries and other joint pathologies. Arthroscopy has also been utilized to treat SC arising in various joints, including the knee, hip, elbow, and shoulder. Nevertheless, literature on arthroscopic management of shoulder SC is lacking, and no study to date has compared patient outcomes following open arthrotomy or arthroscopic approach, thus presenting a major surgical challenge.10
From our systematic review, SC of the shoulder had a 2:1 male-to-female ratio and the mean age of 33 years, consistent with the current understanding of its epidemiology.1,3,7 In addition to the more common clinical presentations outlined above, muscle atrophy was seen in just two patients with chronic shoulder pain (7 and 14 years of symptom duration) likely due to delayed patient presentation and/or diagnosis of SC.
In contrast to the belief that extra-articular localization of shoulder SC is rare,17 SC was found to affect various intra- and extra-articular locations of the shoulder. The most commonly affected sites were the GHJ, subscapular recess, BTS, and subacromial space. In many of these cases, arthroscopic approach potentially has a significant advantage of adequate visualization and access to locations without the need for subscapularis tenotomy as in the case for open arthrotomy.8,10,17,26,27 In addition, arthroscopic approach for the management of SC is thought to provide low post-operative morbidity, while allowing early joint mobilization and recovery.7,9,17,29 Although this needs to be confirmed with comparative studies, they may be challenging to undertake given the seemingly low incidence of SC of the shoulder.
Overall, arthroscopic treatment of shoulder SC was successful in 70.8% of cases. Three cases had failed arthroscopic management due to the need for a total conversion to open surgery. Buess and Friedrich reported that radical extraction of over 50 loose bodies, measuring up to 8 mm, from the axillary and subscapular recesses and the BTS was difficult, thus the authors opted to perform a ventral arthrotomy via a deltopectoral approach and additionally opening the BTS.11 Colanese et al. opted for a conversion to a limited deltopectoral approach to completely excise a lesion measuring 4 × 3 × 1 cm from the subscapular recess extending medially under the coracoid.13 Francesca and Ronquillo also reported needing to convert to an open deltopectoral approach with a subdeltoid extension to completely excise 53 loose bodies with a maximum diameter up to 25 mm from the GHJ and BTS.16 Two other studies successfully removed loose bodies from the GHJ and subscapular recess using arthroscopy; however, they performed open debridement of BTS.12,15 In a case series by Lunn et al., seven patients also underwent an open subpectoral biceps tenodesis for the treatment of inflamed or damaged bicipital tendon associated with loose bodies in the bicipital groove.4 Based on these findings, arthroscopic management of SC arising in the BTS appears more challenging, with a potentially higher risk of requirement for an open procedure. Nevertheless, Maier et al. recently published an optimized biceps tenoscopy technique for the treatment of SC arising in the BTS, which may further prevent the need for open debridement and synovectomy of the BTS.21 Notably, incomplete excision of loose bodies from the GHJ was observed in 3 of 15 patients from the case series by Lunn et al.4 Incomplete excision of loose bodies was not observed in other studies. As all procedures in the case series by Lunn et al. were performed by a single surgeon,4 it is difficult to determine whether arthroscopic management of shoulder SC is significantly associated with the risk of incomplete loose body excision.
Following successful arthroscopic management (n = 34), radiological evidence of disease recurrence was observed in five patients (14.7%). Interestingly, all five patients had initially underwent arthroscopic excision of loose bodies in combination with synovectomy. Although synovectomy is believed to reduce the recurrence rate by removing the primarily affected synovium, no study to date has demonstrated a clear benefit of combined loose body excision and synovectomy over excision of loose bodies alone.27 Nevertheless, a small number of cases with loose body excision alone precludes drawing any meaningful conclusion with clinical significance. Given that estimated 1%–5% of SC may undergo malignant transformation into chondrosarcoma, often associated with preceding disease recurrence,16 factors that may influence disease recurrence should be further investigated. Of note, there was no reported case of malignant transformation among the articles identified by our systematic review.
We identified the following limitations in our study: first, existing literature on arthroscopic management of SC of the shoulder is limited, with a total of 27 studies to date. Most of these articles were case reports. Therefore, it is possible that cases with suboptimal outcomes may have been underreported. Nevertheless, with the exception of the case series by Lunn et al.,4 the outcomes following arthroscopic management of shoulder SC were good (84.8% success rate; 14.3% recurrence rate) and no arthroscopy-related complications were observed. Second, there is significant heterogeneity in the arthroscopic techniques utilized by the authors, which likely influences the procedure outcomes and recurrence rates. To overcome these limitations, comparative studies including a larger number of cases with arthroscopic management and long-term follow-up duration are needed to develop a standardized, gold-standard arthroscopic approach with higher success rates.
Conclusion
Literature on arthroscopic management of SC of the shoulder is scarce. Among 48 patients from 27 articles, arthroscopic treatment was successful in 70.8%, and resulted in disease recurrence in 14.7%. Significant heterogeneity in arthroscopic techniques was observed, necessitating a larger number of cases to develop a standardized procedure. Although arthroscopic approach for the management of shoulder SC is safe and effective with good visualization/access, low morbidity, early post-operative joint mobility and rehabilitation, further optimization is necessary to avoid failure of treatment and recurrence of disease.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor: JPP.
Contributorship: JPP researched literature, was involved in the conceptualization of the project, and wrote the first draft of the manuscript. YM researched literature, was involved in the conceptualization of the project, and contributed in the preparation of the first draft of the manuscript. SMA was involved in the conceptualization of the project, and contributed in the preparation of figures and tables. MLB was involved in the conceptualization of the project, and provided supervision. PAM was involved in the conceptualization of the project, and provided supervision. All authors reviewed and edited the manuscript, and approved the final version of the manuscript.
ORCID iD: J. Patrick Park https://orcid.org/0000-0002-4864-3270
References
- 1.Duymus TM, Yucel B, Mutlu S, et al. Arthroscopic treatment of synovial chondromatosis of the shoulder: a case report. Ann Med Surg 2015; 4: 179–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jiménez-Martín A, Zurera-Carmona M, Santos-Yubero FJ, et al. Arthroscopic treatment of synovial chondromatosis, an unusual cause of shoulder pain. Reumatol Clin 2014; 10: 416–417. [DOI] [PubMed] [Google Scholar]
- 3.Wahab H, Hasan O, Habib A, et al. Arthroscopic removal of loose bodies in synovial chondromatosis of shoulder joint, unusual location of rare disease: a case report and literature review. Ann Med Surg 2019; 37: 25–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lunn JV, Castellanos-Rosas J, Walch G. Arthroscopic synovectomy, removal of loose bodies and selective biceps tenodesis for synovial chondromatosis of the shoulder. J Bone Joint Surg Br 2007; 89: 1329–1335. [DOI] [PubMed] [Google Scholar]
- 5.Utashima D, Matsumura N, Suzuki T, et al. Clinical results of surgical resection and histopathological evaluation of synovial chondromatosis in the shoulder: a retrospective study and literature review. Clin Orthop Surg 2020; 12: 68–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bruggeman NB, Sperling JW, Shives TC. Arthroscopic technique for treatment of synovial chondromatosis of the glenohumeral joint. Arthroscopy 2005; 21: 633–633. [DOI] [PubMed] [Google Scholar]
- 7.Raval P, Vijayan A, Jariwala A. Arthroscopic retrieval of over 100 loose bodies in shoulder synovial chondromatosis: a case report and review of literature. Orthop Surg 2016; 8: 511–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park JH, Noh HK, Bada LP, et al. Arthroscopic treatment for synovial chondromatosis of the subacromial bursa: a case report. Knee Surg Sports Traumatol Arthrosc 2007; 15: 1258–1260. [DOI] [PubMed] [Google Scholar]
- 9.Fowble VA, Levy HJ. Arthroscopic treatment for synovial chondromatosis of the shoulder. Arthroscopy 2003; 19: E2–E2. [DOI] [PubMed] [Google Scholar]
- 10.Aydogan NH, Kocadal O, Ozmeric A, et al. Arthroscopic treatment of a case with concomitant subacromial and subdeltoid synovial chondromatosis and labrum tear. Case Rep Orthop 2013; 2013: 636747–636747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Buess E, Friedrich B. Synovial chondromatosis of the glenohumeral joint: a rare condition. Arch Orthop Trauma Surg 2001; 121: 109–111. [DOI] [PubMed] [Google Scholar]
- 12.Chillemi C, Marinelli M, de Cupis V. Primary synovial chondromatosis of the shoulder: clinical, arthroscopic and histopathological aspects. Knee Surg Sports Traumatol Arthrosc 2005; 13: 483–488. [DOI] [PubMed] [Google Scholar]
- 13.Colanese J, Cil A, Egekeze N, et al. Case report of mimicry between synovial hemangioma and synovial chondromatosis of the shoulder. J Orthop Case Rep 2016; 6: 88–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Covall DJ, Fowble CD. Arthroscopic treatment of synovial chondromatosis of the shoulder and biceps tendon sheath. Arthroscopy 1993; 9: 602–604. [DOI] [PubMed] [Google Scholar]
- 15.David T, Drez DJ. Synovial chondromatosis of the shoulder and biceps tendon. Orthopedics 2000; 23: 611–613. [DOI] [PubMed] [Google Scholar]
- 16.Francesca J, Ronquillo JC. Primary synovial chondromatosis of the shoulder with concomitant intra-articular and extra-articular involvement: more than a simple removal of loose bodies. Tech Shoulder Elbow Surg 2018; 19: 18–23. [Google Scholar]
- 17.Fukuda A, Uemura T, Nishimura A, et al. Arthroscopic treatment of primary synovial chondromatosis of the subscapular bursa: a case report. J Orthop Case Rep 2020; 9: 40–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hamada J, Tamai K, Koguchi Y, et al. Case report: a rare condition of secondary synovial osteochondromatosis of the shoulder joint in a young female patient. J Shoulder Elbow Surg 2005; 14: 653–656. [DOI] [PubMed] [Google Scholar]
- 19.Jeon I-H, Ihn J-C, Kyung H-S. Recurrence of synovial chondromatosis of the glenohumeral joint after arthroscopic treatment. Arthroscopy 2004; 20: 524–527. [DOI] [PubMed] [Google Scholar]
- 20.Jung KA, Kim SJ, Jeong JH. Arthroscopic treatment of synovial chondromatosis that possibly developed after open capsular shift for shoulder instability. Knee Surg Sports Traumatol Arthrosc 2007; 15: 1499–1503. [DOI] [PubMed] [Google Scholar]
- 21.Maier D, Izadpanah K, Jaeger M, et al. Biceps tenoscopy in arthroscopic treatment of primary synovial chondromatosis of the shoulder. Arthrosc Tech 2014; 3: e539–e545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rassi El G, Matta J, Hijjawi A, et al. Extra-articular synovial chondromatosis eroding and penetrating the acromion. Arthrosc Tech 2015; 4: e443–e448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Richman JD, Rose DJ. The role of arthroscopy in the management of synovial chondromatosis of the shoulder. A case report. Clin Orthop Relat Res 1990; 8: 91–93. [PubMed] [Google Scholar]
- 24.Tokis AV, Andrikoula SI, Chouliaras VT, et al. Diagnosis and arthroscopic treatment of primary synovial chondromatosis of the shoulder. Arthroscopy 2007; 23: 1023.e1–1023.e5. [DOI] [PubMed] [Google Scholar]
- 25.Witwity T, Uhlmann R, Nagy MH, et al. Shoulder rheumatoid arthritis associated with chondromatosis, treated by arthroscopy. Arthroscopy 1991; 7: 233–236. [DOI] [PubMed] [Google Scholar]
- 26.Xu C, Yang X, Zhao J. Arthroscopic treatment for synovial chondromatosis of the subacromial bursa associated with partial rotator cuff tear. Knee Surg Sports Traumatol Arthrosc 2015; 23: 600–602. [DOI] [PubMed] [Google Scholar]
- 27.Ranalletta M, Bongiovanni S, Calvo JM, et al. Arthroscopic treatment of synovial chondromatosis of the shoulder: report of three patients. J Shoulder Elbow Surg 2009; 18: e4–e8. [DOI] [PubMed] [Google Scholar]
- 28.Urbach D, McGuigan FX, John M, et al. Long-term results after arthroscopic treatment of synovial chondromatosis of the shoulder. Arthroscopy 2008; 24: 318–323. [DOI] [PubMed] [Google Scholar]
- 29.Aramberri M, Tiso G, Haeni DL. Arthroscopic and endoscopic technique for subcoracoid synovial chondromatosis of the shoulder through a medial transpectoral portal. Arthrosc Tech 2018; 7: e279–e283. [DOI] [PMC free article] [PubMed] [Google Scholar]