1. Introduction
The Coronavirus Disease 2019 (COVID-19) pandemic has been considered a major health emergency with enormous physical and psychological consequences, including post-traumatic stress disorder (PTSD) (Bo et al., 2021). People infected with COVID-19 could develop dyspnea about a week from symptom onset (Huang et al., 2020). Numerous health care infrastructures in affected areas were overwhelmed by the rapid spread of COVID-19, leading to delays in seeking medical visits for people with COVID-19 symptoms. Gender differences were highlighted during the pandemic, with females suffering more from PTSD (Liu et al., 2020). However, evidence showed higher critical and mortality rates in males infected with COVID-19 (Remuzzi and Remuzzi, 2020). Additionally, the over-representation of females in most studies may lead to selection and conclusions bias. Therefore, the dynamic manifestation and trend of gender differences in PTSD patients who are potentially delayed in medical visits deserve to be further investigated.
2. Methods
From 2 designated hospitals in Wuhan, China, 258 COVID-19 patients were recruited from 26 February to 16 March 2020. Clinical data, including classification of disease severity, the minimum lymphocyte count, and the lowest Oxygen Saturation (SaO2), and the exact date of viral symptom onset, first medical visit, and hospitalization were extracted from electronic medical records. Post-traumatic stress symptoms (PTSS) and sleep quality were evaluated by the PTSD Checklist for DSM-5 (PCL-5) and 4 items of the Pittsburgh Sleep Quality Index (PSQI) with Cronbach’s α of 0.94 and 0.90, respectively (Liu et al., 2020). Data were collected by two clinicians who had prior professional training in psychometrics, and two psychiatrists served as consultants during the collection period. A head-to-head propensity score matching (PSM) analysis using a multivariate conditional logistic regression model with a caliper width of 0.1 was performed, yielding 82 males and 82 females with all demographic and baseline characteristics well matched.
3. Results
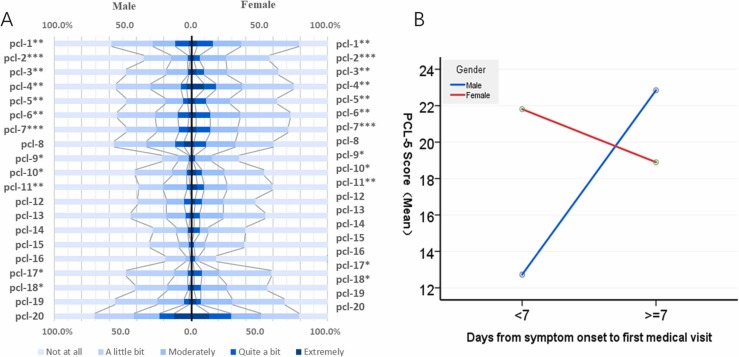
Among the 258 patients, forty-eight (18.6%) met the criteria of PTSD symptoms, 30 (62.5%) of them being females. The central symptoms of PTSD were sleeping difficulties, recurrent thoughts, psychological cue reactivity, avoidance of thoughts, difficulty concentrating, and avoidance of reminders, with the occurrence of each symptom more than 60%. Gender-stratified PTSS distribution is shown in Fig. 1 A, 12 out of 20 PTSD symptoms were more severe in females.
Fig. 1.
A, Gender-stratified PTSS distribution in 258 COVID-19 patients. Vertical coordinate are the corresponding items of PCL-5, each item represents one PTSD symptom. pcl-1: Recurrent thoughts; pcl-2: Nightmares; pcl-3: Flashbacks; pcl-4: Psychological cue reactivity; pcl-5: Physiological cue reactivity; pcl-6: Avoidance of thoughts; pcl-7: Avoidance of reminders; pcl-8: Amnesia; pcl-9: Negative beliefs; pcl-10: Distorted blame; pcl-11: Negative emotional state; pcl-12: Diminished interest; pcl-13: Detachment; pcl-14: Restricted affect; pcl-15: Irritability or anger; pcl-16: Reckless of self-destructive behavior; pcl-17: Hypervigilance; pcl-18: Exaggerated startle; pcl-19: Difficulty concentrating; pcl-20: Sleeping difficulties. * : P < 0.05; * *: P < 0.01; * ** : P < 0.001. B, Interaction of gender with delayed treatment on PCL-5 among 164 gender-matched COVID-19 patients. Delayed treatment status was defined by days from the onset of COVID-19 symptoms to first medical visit.
Among the 164 paired sample, hierarchical regression analysis showed that the difficulty falling asleep (β = 0.377, p < 0.01) and days from symptom onset to first medical visit (β = 0.444, p < 0.001) were risk factors of PTSS development in males, but not in females. Considering the effect of delayed medical treatment, univariate ANOVA revealed a significant gender * time-interval (days from symptom onset to first medical visit) interaction for the prevalence of PTSS (F=5.710, p < 0.05), with the main effects of gender (F=0.885, p = 0.348) and time-interval (F=1.745, p = 0.188) insignificant, see Fig. 1B. Females had significantly higher PCL-5 scores than males when time-interval was less than 7 days (21.81 vs. 12.72, t = −4.12, p < 0.001), whereas no such gender differences were found when the time interval was 7 days or more (18.89 vs. 22.85, t = 0.63, ns).
4. Discussion
This study investigated the prevalence, gender differences of PTSS, and its influencing factors in hospitalized COVID-19 patients during the peak of the COVID-19 epidemic in China, with strictly matching the gender through PSM analysis. The study indicated that the prevalence of PTSS was 18.6% in hospitalized COVID-19 patients, and the central PTSD symptoms were sleeping difficulties, recurrent thoughts, psychological cue reactivity, difficulty concentrating, and avoidance. This is consistent with previous studies emphasizing different central of PTSD symptomatology (Brewin et al., 2010; Hoorelbeke et al., 2021; Zhang et al., 2020). The most striking finding of this study is that male and female showed inconsistent trends in PTSS under delayed medical treatment. Females had higher PTSS levels immediately after the onset of COVID-19 symptoms, which is in line with previous studies(Liu et al., 2020). However, PTSS levels in males were lower at first and had a surge even surpassing that of females when they delay seeking medical treatment. The possible explanation is that women are more likely than men to seek medical attention in a timely manner (Mustard et al., 1998, Redondo-Sendino et al., 2006). Therefore, males tend to initially ignore the virus-like symptoms and refuse to seek medical help until anxiety increased rapidly as symptoms worsen one week later, leading to a sharp rise in PTSS levels.
5. Conclusions
The prevalence of PTSS among hospitalized COVID-19 patients was 18.6%, with a significantly higher prevalence among females. However, the deleterious impact of delayed medical treatment on the development of PTSS only occurred in males, where PTSS levels rose sharply when they delayed treatment by more than a week. These findings highlight the importance of careful monitoring, early identification, and treatment of viral symptoms and psychological disorders, especially in this case where early intervention might reduce the likelihood of developing PTSS in males.
Ethics approval and consent to participate
This study was done after agreement from the ethics committees of Naval Medical University and with the patients' informed consent.
Funding
This work was supported by the National Natural Science Foundation of China (No. 32071086) and the “13th Five-Year” Dual Construction Project (No. 2020SZ15).
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request. The personal information of the study participants is kept strictly confidential as mandated by the request of the study participants.
Author contributions
NL, ZS, XP contributed to the writing of this article and the statistical analysis of this article, who are co-first authors, WL, BY and YB led the whole study, including putting forward this study, carrying out the study, and was the co-corresponding author. XT, CX, WY contributed to performing the investigation and collection of all data.
Conflict of interest
The authors declare that they have no conflicts of interest.
Acknowledgments
The authors would like to acknowledge the volunteers who participated in the study and Yanpu Jia & Lili Wu for revising and polishing the manuscript. Some results of this research have been posted in the preprint servers, with DOI of 10.21203/rs.3.rs-39067/v1.
References
- Bo H.X., Li W., Yang Y., Wang Y., Zhang Q., Cheung T., Xiang Y.T. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol. Med. 2021;51(6):1052–1053. doi: 10.1017/s0033291720000999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewin C.R., Gregory J.D., Lipton M., Burgess N. Intrusive images in psychological disorders: characteristics, neural mechanisms, and treatment implications. Psychol. Rev. 2010;117(1):210–232. doi: 10.1037/a0018113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoorelbeke K., Sun X., Koster E.H.W., Dai Q. Connecting the dots: a network approach to post-traumatic stress symptoms in Chinese healthcare workers during the peak of the Coronavirus Disease 2019 outbreak. Stress Health. 2021 doi: 10.1002/smi.3027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/s0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu N., Zhang F., Wei C., Jia Y., Shang Z., Sun L., Liu W. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustard C.A., Kaufert P., Kozyrskyj A., Mayer T. Sex differences in the use of health care services. New Engl. J. Med. 1998;338(23):1678–1683. doi: 10.1056/nejm199806043382307. [DOI] [PubMed] [Google Scholar]
- Redondo-Sendino A., Guallar-Castillón P., Banegas J.R., Rodríguez-Artalejo F. Gender differences in the utilization of health-care services among the older adult population of Spain. BMC Public Health. 2006;6:155. doi: 10.1186/1471-2458-6-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remuzzi A., Remuzzi G. COVID-19 and Italy: what next. Lancet. 2020;395(10231):1225–1228. doi: 10.1016/s0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang F., Shang Z., Ma H., Jia Y., Sun L., Guo X., Liu W. Epidemic area contact history and sleep quality associated with posttraumatic stress symptoms in the first phase of COVID-19 outbreak in China. Sci. Rep. 2020;10(1):22463. doi: 10.1038/s41598-020-80649-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request. The personal information of the study participants is kept strictly confidential as mandated by the request of the study participants.