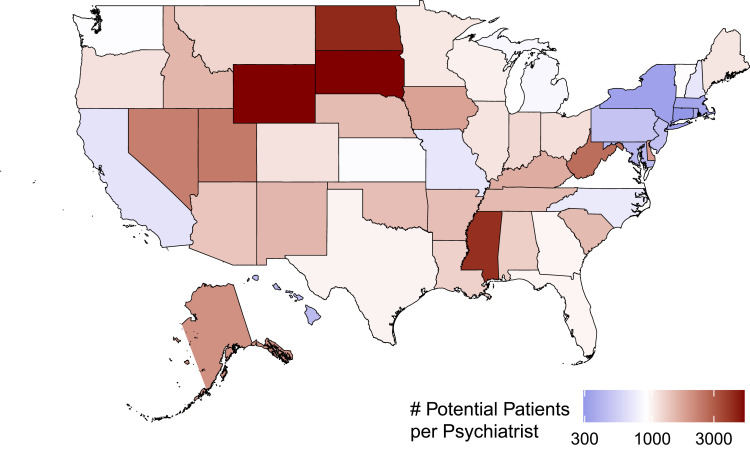
Figure 1.
Capacity of the geriatric psychiatry workforce to serve adults aged 65+ with depressive disorders in the US.
Notes: The authors created this figure with data from the following sources: 1) Maximum caseload for outpatient psychiatrist was ~900 patients estimated from the US Department of Veterans Affairs (VA). Data from Veterans Health Administration130 and McQuistion HL and Zinns R.131 2) Number of geriatric psychiatrists per state was estimated from US News and World Report’s provider list (n= 2758).129 3) Number of adults ages 65+ with depressive disorders (including major depressive disorder or dysthymia) per state was estimated from the Institute of Health Metrics and Evaluation’s Global Health Data Exchange (data from Global Burden of Disease Collaborative Network).1 This map likely underestimated the workforce shortage for various reasons: 1) typical caseload in the VA or in US community-based psychiatry is much lower than 900 (data from McQuistion HL and Zinns R131) 2) number of geriatric psychiatrists in the US News and World Report’s provider list (n= 2758); data from Geriatric Psychiatrist Near Me129 is almost twice as high as the number with currently active licenses (n= 1457); data from American Board of Psychiatry and Neurology, Inc.127 and 3) patients with mental illness other than depressive disorders, who may also need psychiatric care, were not included.