Abstract
Introduction
Interstitial pregnancy is a rare type of ectopic pregnancy. The aim of our publication is to describe the diagnosis and treatment of this entity.
Case report
We report the case of a ruptured interstitial pregnancy diagnosed in a 32 years old patient admitted for acute abdominal pain.
Discussion
The main symptom was severe pelvic pain in a context of amenorrhea. The ultrasound found the ectopic pregnancy in the form of an eccentric gestational sac with an empty uterine cavity as well as intraperitoneal effusion. A ruptured ectopic pregnancy was suspected and the patient was admitted immediately for emergency laparotomy with cornusotomy and salpingectomy.
Conclusion
Interstitial ectopic pregnancy is associated with high morbidity. Its diagnosis and management should be early and adequate in order to avoid complications and preserve fertility.
Keywords: Ectopic pregnancy, Haemoperitoneum, Laparotomy, Cornuostomy, Case report
Highlights
-
•
Interstitial ectopic pregnancy is a rare entity.
-
•
Diagnosis should be made in any woman of childbearing age presenting with pelvic pain and/or breakthrough bleeding.
-
•
Treatment is either surgical by laparoscopy or medical by administration of methotrexate.
1. Introduction
Interstitial pregnancy is a rare condition that accounts for 2–6.8% of ectopic pregnancies (EP) [1]. It is defined by the implantation of the gestational sac in the most proximal part of the fallopian tube (called interstitial part) inside the myometrium. It is therefore to be differentiated from a cornual pregnancy, which corresponds to implantation in the cavity of a rudimentary horn of the uterus, which may or may not communicate with the uterine cavity. The risk factors for interstitial pregnancy are those of ectopic pregnancy, notably a history of ectopic pregnancy, pelvic inflammatory disease, pelvic surgery and assisted reproduction techniques [2].
Interstitial ectopic pregnancy represents a particular diagnostic entity because of its non-specific clinical and paraclinical signs. Indeed, the classic triad (amenorrhea, abdominal pain, bleeding) is present in less than 40% of cases [3]. The diagnosis is based essentially on 2D ultrasound, which shows a bulge of myometrial tissue surrounding an eccentric gestational sac with an echogenic line extending into the uterine horn. Although this ultrasound appearance is quite specific, it is not very sensitive, hence the importance of completing the diagnosis with 3D ultrasound and MRI [4].
When diagnosed prematurely, interstitial EP can be treated medically with intramuscular or in-situ methotrexate. More often, the diagnosis is late and the treatment is then surgical by cornuostomy or cornual resection with salpingectomy. We report the case of a ruptured interstitial EP treated surgically [5].
2. Case report
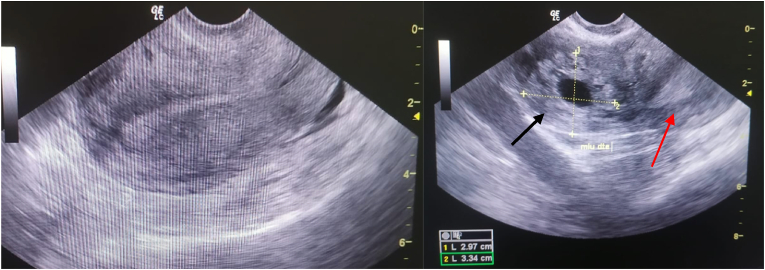
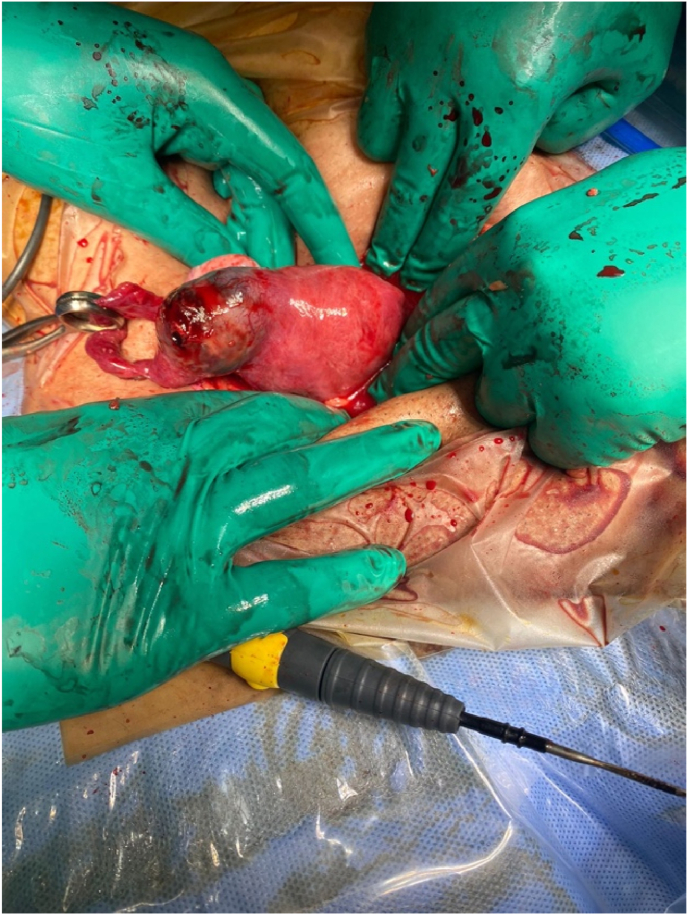
A 32-year-old patient, 2 gravida 1 para with a previous vaginal delivery, presented to the emergency department at 7 weeks of amenorrhea for pelvic pain. Clinical examination found a normal blood pressure with tachycardia at 130/min and a tender abdomen. The Bhcg level was 15,000 IU/L. Transvaginal ultrasound showed an empty uterus with a 30 × 33 mm gestational sac with no embryo, lateralized to the right, separated from the uterine cavity by a 3 mm myometrial rim, associated with a moderate intraperitoneal fluid effusion (Fig. 1). An emergency mini-laparotomy was indicated for suspicion of ruptured EP, which allowed the discovery of a hemoperitoneum with ruptured extra uterine pregnancy in the interstitial part of the right tube (Fig. 2). A cornuostomy with right salpingectomy was then successfully performed. Post operation recovery was uneventful.
Fig. 1.
Trasnvaginal ultrasound; left: absence of an intrauterine pregnancy on ultrasound. Right: eccentrically located gestational sac (black arrow) and the uterus (red arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Fig. 2.
Laparotomy showing an interstitial ectopic pregnancy.
3. Discussion
Interstitial EP, unlike tubal EP, is often diagnosed late and is associated with an increased risk of rupture and maternal morbidity. Clinically, pain is the main reason for consultation, which is the case for our patient. Metrorrhagia is not always constant [5].
The ultrasound finding was typical of interstitial pregnancy, including an eccentric gestational sac, surrounded by a myometrial rim, separated >1 cm from an empty uterine cavity [6]. Ackerman et al. also described the presence of an echogenic line, connecting the eccentric gestational sac with the endometrial cavity, representing the interstitial portion of the fallopian tube [5]. This sign was not found in our case, given the advanced gestational age of the pregnancy.
Management of interstitial pregnancies depends on gestational age, hemodynamic status, fertility desire, and surgeon experience [7]. For medical treatment, intra-muscular injection of methotrexate is the method of choice [5]. Unlike the Fernandez score for tubal EP, there is no threshold value for serum β-hCG levels below which the drug should not be used [2]. Medical treatment is increasingly used nowadays with variable success rates, especially for unruptured interstitial pregnancies. Nevertheless, the risk of failure and rupture is always present [5]. Surgical treatment is based on a rapid approach by laparoscopy or laparotomy to ensure haemostasis. The surgical technique consists of cornuostomy or cornual resection, with salpingectomy. It is indicated in cases of ruptured interstitial EP and/or a gestational sac >40mm, which was the case for our patient [8].
The main complications of treated interstitial pregnancies are recurrence and uterine rupture in subsequent pregnancies. Recurrence is the prerogative of medical treatment and cornuostomy, whereas uterine rupture is secondary to surgical treatment by cornual resection, probably due to the fragility of the uterine wall. Nevertheless, recent studies are more reassuring on this point and do not advocate systematic prophylactic c-section [7]. We plan close and early surveillance in case of pregnancy in our patient.
4. Conclusion
Interstitial ectopic pregnancy is different from cornual ectopic pregnancy because it occurs in women without a history of salpingectomy or malformed uterus. Its frequency is low and its diagnosis, which is often late, relies essentially on ultrasound. Associated with a higher risk of morbidity, its treatment must be early and appropriate in order to avoid complications and preserve fertility.
This case report has been reported in line with the SCARE Criteria [9].
Funding
This work did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Patient consent
Written informed consent was obtained from the patient for the publication of this case report.
Provenance and peer review
This article was not commissioned and was peer reviewed.
Please state any sources of funding for your research
There are no funding sources to be declared.
Ethical approval
Ethical approval from the hospital: Maternity of Souissi has been obtained to proceed with the current publication.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Sarah BOUJIDA made substantial contributions to management of the case, conception and design of the manuscript, acquisition of data, analysis and interpretation of data; she has been involved in drafting the manuscript and revising it critically for important intellectual content. Oumaima M’HAMDI and Hounaida MAHFOUD made substantial contributions to interpretation of data and they have been involved in drafting the manuscript and revising it critically for important intellectual content. Aziz BAYDADA and Aicha KHARBACH made substantial contributions to acquisition of data and supervised the redaction of the manuscript.
Registration of research studies
Name of the registry: ORCID
Unique identifying number or registration ID: 0000-0002-4398-8624
Hyperlink to your specific registration (must be publicly accessible and will be checked):
Guarantor
BOUJIDA Sarah.
Declaration of competing interest
The authors declare that they have no conflict of interest regarding the publication of this case report.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2022.104076.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Brincat M., Bryant-Smith A., Holland T.K. The diagnosis and management of interstitial ectopic pregnancies: a review. Gynecol. Surg. 2019;16:2. doi: 10.1186/s10397-018-1054-4. [DOI] [Google Scholar]
- 2.Stabile Guglielmo, et al. Interstitial ectopic pregnancy: the role of mifepristone in the medical treatment. Int. J. Environ. Res. Publ. Health. 17 Sep. 2021;18(18):9781. doi: 10.3390/ijerph18189781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dagar M., Srivastava M., Ganguli I., Bhardwaj P., Sharma N., Chawla D. Interstitial and cornual ectopic pregnancy: conservative surgical and medical management. J. Obstet. Gynaecol. India. 2018 Dec;68(6):471–476. doi: 10.1007/s13224-017-1078-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lin T.Y., Chueh H.Y., Chang S.D., Yang C.Y. Interstitial ectopic pregnancy: a more confident diagnosis with three-dimensional sonography. Taiwan. J. Obstet. Gynecol. 2021 Jan;60(1):173–176. doi: 10.1016/j.tjog.2020.11.028. [DOI] [PubMed] [Google Scholar]
- 5.Nadi M., Richard C., Filipuzzi L., Bergogne L., Douvier S., Sagot P. Grossesse interstitielle, angulaire et cornuale : diagnostic, traitement et futur obstétrical [Interstitial, angular and cornual pregnancies: diagnosis, treatment and subsequent fertility] Gynecol Obstet Fertil Senol. 2017 Jun;45(6):340–347. doi: 10.1016/j.gofs.2017.05.002. French. [DOI] [PubMed] [Google Scholar]
- 6.Timor-Tritsch I.E., Monteagudo A., Matera C., Veit C.R. Sonographic evolution of cornual pregnancies treated without surgery. Obstet. Gynecol. 1992 Jun;79(6):1044–1049. PMID: 1579304. [PubMed] [Google Scholar]
- 7.Douysset X., Verspyck E., Diguet A., Marpeau L., Chanavaz-Lacheray I., Rondeau S., Resch B., Sergent F. Grossesses interstitielles : traitement chirurgical, fertilité et devenir obstétrical. L’expérience rouennaise. Gynecol. Obstet. Fertil. 2014;42(4):216–221. doi: 10.1016/j.gyobfe.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 8.MacRae R., Olowu O., Rizzuto M.I., Odejinmi F. Diagnosis and laparoscopic management of 11 consecutive cases of cornual ectopic pregnancy. Arch. Gynecol. Obstet. 2008;280(1):59–64. doi: 10.1007/s00404-008-0872-4. [DOI] [PubMed] [Google Scholar]
- 9.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.