Abstract
Objective
To explore the correlation between the incidence of atrial fibrillation (AF) and thyroid dysfunction in patients with hypertrophic obstructive cardiomyopathy (HOCM).
Methods
Thyroid function testing in 755 consecutive patients with HOCM were examined at the National Center for Cardiovascular Diseases (China) from October 2009 to December 2013. Patients were divided into four groups according to the TSH levels: TSH<0.55 mIU/L(n=37)、0.55~2.49 mIU/L (n=490)、2.50~9.9 mIU/L (n=211) and >10.00mIU/L(n=17).
Results
A total of 107 patients were diagnosed with AF (14%).(1) Compared to HOCM patients without AF,HOCM patients with AF have older age (P<0.001), higher NT-proBNP (P=0.002), higher Cr (P=0.005), larger left atrial diameter(P=0.001), lower FT3 (P=0.046), higher FT4 (P=0.004).(2) In the four groups according to the TSH levels: TSH<0.55 mIU/L, 0.55~2.49mIU/L, 2.50~9.9mIU/L and ≥10.00mIU/L, the incidence of AF was 27.02%(10/37),10.20%(50/490), 19.43%(41/211), and 35.29%(6/17), respectively. Both high and low TSH levels were associated with an increased incidence of AF. After adjusting for the common risk factor (age, NT-proBNP, and so on), stepwise multiple logistic regression analysis revealed that TSH levels were significantly related to AF incidence.Compared to patients with TSH 0.55~2.49 mlU/L, the adjusted odds ratio of AF for TSH<0.55, 2.50~9.99, ≥10.00 mIU/L were 1.481 (95% CI 0.485~4.518,P=0.490), 1.977 (95%CI 1.115~3.506, p=0.02), 4.301 (95%CI 1.059~17.476, P=0.041), respectively.
Conclusion
Our results suggested that thyroid dysfunction was associated with an increased risk of AF in patients with HOCM.
Keywords: thyroid dysfunction, hypertrophic obstructive cardiomyopathy, atrial fibrillation, TSH, risk factors
Introduction
More and more studies have shown that thyroid dysfunction is a significant risk factor for the progression of cardiovascular disease (1, 2). Our previous research and other clinical evidence suggest (3, 4), The level of thyroid hormone is related to the deterioration of cardiac function and the occurrence of arrhythmia. Hypertrophic cardiomyopathy (HCM) is a kind of cardiomyopathy characterized by asymmetric myocardial hypertrophy, which usually occurs at the base of the interventricular septum and the lateral wall of the left ventricle (5). HCM has a variety of clinical manifestations, can occur in all age groups and has a familial genetic tendency, which is a common cause of sudden cardiac death. Heart failure and electrophysiological disorders may occur in the later stage of the disease (6–8). Atrial fibrillation is the most common persistent arrhythmia in patients with HCM. It has been found that 2% to 3.8% of HCM patients are newly diagnosed with atrial fibrillation each year, which increases the risk of heart failure, stroke/embolism, and death, especially in patients with hypertrophic obstructive cardiomyopathy with left ventricular outflow tract obstruction (9). Left ventricular filling in patients with HCM mainly depends on atrial contraction. Atrial fibrillation will shorten the left ventricular filling time and damage the left ventricular diastolic function, resulting in frequent hospitalization and declining quality of life. Atrial fibrillation is one of the risk factors for the poor prognosis of HCM. Therefore, the clinical management of hypertrophic cardiomyopathy complicated with atrial fibrillation is a very important topic (10).
However, only a few clinical studies have shown that thyroid dysfunction is related to left ventricular diastolic dysfunction in patients with HCM (11). There is no study on the role of thyroid function in predicting atrial fibrillation in patients with HCM. This study was based on 756 patients with hypertrophic obstructive cardiomyopathy to investigate the relationship between thyroid function and atrial fibrillation in patients with hypertrophic obstructive cardiomyopathy.
Methods
Ethics Statement
The study followed the ethical guidelines of the declaration of Helsinki and China’s regulations and policies on good clinical practice. The Ethics Committee approved it of the Fuwai Hospital. Before the study, we got written informed consent from all participants.
Study Patients
All patients in this study were evaluated at the Fuwai Hospital (National Center of Cardiovascular Diseases, China). Between October 1, 2009, and December 31, 2013, a total of 824 patients (age≥16 years) were diagnosed with HOCM. Among those participants, 755 subjects, with complete information on thyroid function, clinical information, and medical history, in the absence of any other cardiac or systemic disease capable of producing the magnitude of hypertrophy evident, such as uncontrolled hypertension (home blood pressure monitoring ≥140/90 mmHg), congenital heart disease, cardiac valve disease, and amyloidosis, were selected. The diagnosis of HOCM was based on (12, 13): (1) Echocardiography showed asymmetric interventricular septal thickening > 13 mm, and interventricular septal (IVS)/left posterior ventricular wall (LVPW) > 1.3 or left ventricular apical or free wall localized thickening > 15 mm. (2) tissue Doppler echocardiography, and MRI showed hypertrophy of apical and near apical IVS, dense myocardium or disordered interstitial arrangement. (3) echocardiography showed that the pressure difference of the left ventricular outflow tract was ≥ 30mmHg.
This study passed the review of the Medical Ethics Committee of Fuwai Hospital of the Chinese Academy of Medical Sciences, and all the subjects signed informed consent forms.
Collect Clinical Data
The demographic data (age, sex, weight, height), lifestyle (smoking history, drinking history), basic heart disease history, concomitant diseases (hypertension, diabetes, stroke, ventricular arrhythmia), (NYHA) cardiac function classification of New York Cardiology Association, electrocardiogram (admission ECG, postoperative ECG) and echocardiography were collected through the electronic medical record system of Fuwai Hospital. Thyroid hormone determination equipment adopts ADVIA immune detection system produced by Siemens. The levels of serum thyrotropin (TSH), free triiodothyronine (FT3), free thyroid hormone (FT4), total triiodothyronine (TT3), and total thyroid hormone (TT4) were detected by the Immunochemical luminescence method. The kit used was a Siemens kit. The normal reference values of thyroid hormones are as follows: TSH:0.55~4.78mIU/L, FT3:2.76~6.30 pmol/L.FT4:1.23~2.90pmoL/L,TT3:1.00~2.94nmol/L.TT4:55.34~160.86nmol/L.All subjects received a full set of laboratory tests simultaneously, including blood lipids, liver and kidney function, blood glucose, NT-proBNP, and so on.
Definition of Thyroid Function and Diagnosis of Atrial Fibrillation
TSH, FT3, FT4, TT3, and TT4 are all defined as normal thyroid function in the normal reference range. Hypothyroidism (hypothyroidism) is elevated TSH levels, with FT3, FT4, TT3, and TT4 levels within or below the normal reference range. In contrast, hyperthyroidism (hyperthyroidism) decreases TSH levels, with FT3, FT4, TT3, and TT4 levels in or above the normal reference range. In addition to the routine grouping methods (clinical and subclinical hyperthyroidism, clinical and subclinical hypothyroidism, and normal thyroid function), some researchers carry out grouping analysis according to TSH level, based on these previous literature reports and expert consensus (14). In this study, TSH, the most sensitive indicator of thyroid function, was divided into three groups: TSH < 0.55, 0.55 ± 2.49, 2.50 ± 9.99, and > 10.00mIU/L. The diagnosis of paroxysmal atrial fibrillation and persistent atrial fibrillation was based on the 2010 European ESC guidelines for diagnosing and treating atrial fibrillation (15).
Data Analysis
Statistical analysis was assessed with SPSS 21.0 statistical package for Windows. All continuous variables are presented as means ± SD, and analysis of variance was used to compare means across multiple groups. The relationships between parametric variables were assessed by multiple linear regression analysis. Initial differences in baseline characteristics between achieved treatment groups were sought in a bivariable investigation using χ2 tests, Fisher exact tests, and Student t-tests. Univariate and multivariate logistic regression analysis was used to explore the relationship between thyroid function and atrial fibrillation in patients with hypertrophic cardiomyopathy.
Results
Study Population and Baseline Clinical Characteristics
Seven hundred fifty-six people were included in this study, including 456 males and 300 females. Table 1 summarizes all the selected subjects’ general clinical data, thyroid hormone levels, and echocardiography. The patients were divided into two groups according to whether they had atrial fibrillation or not: hypertrophic obstructive cardiomyopathy with atrial fibrillation (n=107) and hypertrophic obstructive cardiomyopathy without atrial fibrillation (n = 649). The incidence of atrial fibrillation in this study population was 14%. Patients with hypertrophic obstructive cardiomyopathy with atrial fibrillation were older than patients with simple hypertrophic obstructive cardiomyopathy (p<0.001). The levels of serum creatinine, NT-proBNP, and FT4 were higher (p<0.05), but the level of FT3 was lower (p=0.046) ( Table 1 ).
Table 1.
Clinical baseline characteristics of patients with hypertrophic obstructive cardiomyopathy with or without atrial fibrillation.
| Hypertrophic obstructive cardiomyopathy with atrial fibrillation (n= 107) | Hypertrophic obstructive cardiomyopathy without atrial fibrillation (n=648) | P-value | |
|---|---|---|---|
| Age (years) | 56.99±11.73 | 50.18±12.81 | <0.001 |
| Female (n, %) | 43 (40.19) | 257 (39.60) | 0.908 |
| BMI (kg/m2) | 26.00±5.10 | 25.73±5.94 | 0.688 |
| Hypertension disease (n, %) | 41 (38.32) | 221 (34.05) | 0.403 |
| Diabetes history (n, %) | 6 (5.61) | 42 (6.47) | 0.729 |
| History of hyperlipidemia (n, %) | 32 (29.90) | 191 (29.43) | 0.935 |
| A clear family history of HCM (n, %) | 9 (8.41) | 40 (6.16) | 0.396 |
| Drinking history (n, %) | 33 (30.84) | 186 (28.66) | 0.680 |
| Smoking history (n, %) | 48 (44.86) | 294 (45.30) | 0.879 |
| Systolic blood pressure (mmHg) | 122.10±18.00 | 120.98±5.94 | 0.563 |
| Diastolic pressure (mmHg) | 74.59±11.47 | 73.90±11.43 | 0.560 |
| Heart rate (b.p.m.) | 71.50±13.13 | 71.69±27.59 | 0.944 |
| LDL-C (mmol/L,x±s) | 2.48±0.89 | 2.35±0.93 | 0.186 |
| HDL-C (mmol/L,x±s) | 0.96±0.30 | 0.97±0.33 | 0.809 |
| Triglyceride (mmol/L,x±s) | 1.59±0.88 | 1.68±0.98 | 0.354 |
| Total cholesterol (mmol/L,x±s) | 4.12±1.11 | 4.02±1.11 | 0.428 |
| NT-proBNP (fmol/mL) | 2476.08±1808.93 | 1814.85±1712.95 | 0.002 |
| Serum creatinine (µmol/L) | 82.77±23.73 | 76.56±20.05 | 0.005 |
| TSH (mIU/L) | 3.02±3.82 | 2.45±4.10 | 0.180 |
| FT4 (ng/dL) | 1.26±0.26 | 1.18±0.23 | 0.002 |
| FT3 (pg/mL) | 2.88±0.59 | 2.99±0.54 | 0.046 |
| TT4 (ng/mL) | 8.00±1.93 | 7.81±1.79 | 0.322 |
| TT3 (ug/dL) | 1.02±0.33 | 1.08±0.29 | 0.092 |
| Echocardiography | |||
| RV end-diastolic diameter (mm) | 21.74±5.77 | 20.28±4.38 | 0.003 |
| LA diameter (mm) | 44.82±8.04 | 39.25±13.28 | 0.001 |
| Interventricular septal thickness (mm) |
19.79±4.52 | 20.27±5.68 | 0.415 |
| LV end-diastolic diameter (mm) | 42.65±6.21 | 42.49±6.02 | 0.801 |
| LV posterior wall thickness (mm) | 11.86±2.77 | 11.94±2.90 | 0.780 |
| LV ejection fraction (%) | 67.07±8.52 | 68.14±8.91 | 0.248 |
| LV outflow tract gradient, at rest (mmHg) | 63.42±32.70 | 74.56±33.42 | 0.002 |
The data in the table is expressed in the form of "mean ±SD" or "n (%)". BMI, body mass index; NT-proBNP, amino terminal pro-brain natriuretic peptide; TSH, thyrotropin; FT3, free triiodothyronine; FT4, free thyroxine; TT3, serum total triiodothyronine; TT4, serum total thyroxine.
Baseline Data and Indicators of Patients Grouped by Different TSH Levels
According to the plasma TSH level, the patients were divided into four groups: TSH < 0.55,0.55 ~ 2.49,2.50 ~ 9.99and ≥ 10.00 mIU/L groups. There were significant differences in sex, smoking history, TC, LDL-C, TSH, FT3, FF4, left ventricular end-diastolic diameter, LVEF, and the incidence of atrial fibrillation among different TSH levels groups. The incidence of atrial fibrillation in the TSH (0.55~2.49mlU/L) group was the lowest (10.20%), while TSH(> 10.00 mIU/L) group was the highest (35.29%). In TSH (< 0.55 mlU/L) group and TSH(2.50 ~ 9.99 mIU/L) group, the incidence of atrial fibrillation was 27.02% and 19.43%, respectively. There was a significant difference between those four groups (P < 0.001). In addition, compared with the TSH (0.55 ~ 2.49 mIU/L) group (normal control group), the average level of total cholesterol and LDL-C in the abnormal TSH group was higher (p<0.05), but there was no significant difference in NT-proBNP, creatine kinase isoenzyme (CK-MB), uric acid, LAEDD and LVEDD (P > 0.05) ( Table 2 ).
Table 2.
General clinical data of patients with different TSH levels.
| TSH level (mlU/L) | P-value | ||||
|---|---|---|---|---|---|
| <0.55 (n=37) | 0.55~2.49 (n=490) | 2.50~9.99 (n=211) | ≥10.00 (n=17) | ||
| Age (years) | 53.79±15.78 | 50.95±12.26 | 50.86±13.82 | 53.31±10.26 | 0.522 |
| Female (n, %) | 20 (54.05) a | 162 (33.06) | 100 (47.39) a | 7 (41.18) | <0.001 |
| BMI (kg/m2) | 25.15±4.44 | 26.16±6.68 | 24.94±3.64 a | 26.38±3.19 | 0.099 |
| Hypertension disease (n, %) | 14 (37.84) | 173 (35.31) | 70 (33.18) | 4 (23.53) | 0.699 |
| Diabetes history (n, %) | 1 (2.70) | 32 (6.53) | 13 (6.16) | 2 (11.76) | 0.637 |
| History of hyperlipidemia (n, %) | 9 (24.32) | 142 (28.98) | 68 (32.23) | 4 (23.53) | 0.672 |
| A clear family history of HCM (n, %) | 2 (5.40) | 32 (6.53) | 13 (6.16) | 2 (11.76) | 0.836 |
| Drinking history (n, %) | 11 (29.73) | 150 (30.61) | 55 (26.07) | 3 (17.65) | 0.450 |
| Smoking history (n, %) | 18 (48.65) | 249 (50.82) | 68 (13.88) a | 7 (41.18) | <0.001 |
| Systolic blood pressure (mmHg) | 122.03±19.83 | 121.43±18.38 | 120.70±18.51 | 117.24±17.94 | 0.803 |
| Diastolic pressure (mmHg) | 72.58±10.36 | 74.17±11.37 | 73.70±11.65 | 75.29±13.40 | 0.797 |
| Heart rate (b.p.m.) | 71.97±13.47 | 72.24±31.11 | 69.92±10.06 | 75.65±22.61 | 0.667 |
| LDL-C (mmol/L,x±s) | 2.09±0.76 | 2.38±0.92 | 2.33±0.92 | 3.10±1.20 | 0.002 |
| HDL-C (mmol/L,x±s) | 0.93±0.32 | 0.97±0.35 | 0.97±0.29 | 1.09±0.33 | 0.415 |
| Triglyceride (mmol/L,x±s) | 1.83±1.41 | 1.66±0.95 | 1.66±0.95 | 1.65±0.43 | 0.792 |
| Total cholesterol (mmol/L,x±s) | 3.80±0.86 | 4.04±1.10 | 3.99±1.11 | 4.84±1.38 a | 0.012 |
| NT-proBNP (fmol/mL) | 2265.36±1910.45 | 1802.25±1625.36 | 2008.33±1841.96 | 2326.71±2364.00 | 0.264 |
| Serum creatinine (µmol/L) | 78.34±28.65 | 77.47±18.88 | 75.92±20.54 | 83.18±19.56 | 0.466 |
| TSH (mIU/L) | 0.29±0.19 a | 1.45±0.51 | 3.73±1.15 a | 23.56±14.68 a | <0.001 |
| FT4 (ng/dL) | 1.38±0.58 a | 1.20±0.18 | 1.16±0.20 a | 0.96±0.26 a | <0.001 |
| FT3 (pg/mL) | 3.25±1.77 a | 3.00±0.38 | 2.91±0.40 a | 2.61±0.45 a | <0.001 |
| TT4 (ng/mL) | 8.22±2.91 | 7.93±1.71 | 7.70±1.54 | 6.32±2.95 a | 0.001 |
| TT3 (ug/dL) | 1.12±0.68 | 1.07±0.26 | 1.05±0.26 | 1.05±0.28 | 0.566 |
| Echocardiography | |||||
| RV end-diastolic diameter (mm) | 21.00±4.83 | 20.61±4.74 | 20.07±4.42 | 20.94±3.42 | 0.457 |
| LA diameter (mm) (mm) | 38.69±9.07 | 39.79±6.66 | 40.67±21.63 | 41.76±5.79 | 0.706 |
| Interventricular septal thickness (mm) |
20.54±7.36 | 20.17±5.29 | 20.16±5.76 | 20.88±5.76 | 0.934 |
| LV end-diastolic diameter (mm) | 45.32±7.20 | 42.87±5.92 | 41.13±5.55 a | 41.88±7.01 a | <0.001 |
| LV posterior wall thickness (mm) | 11.60±2.88 | 11.96±2.83 | 11.93±2.91 | 11.58±3.63 | 0.864 |
| LV ejection fraction (%) | 62.99±14.24 a | 68.36±8.54 | 67.97±7.93 | 70.69±5.28 | 0.002 |
| LV outflow tract gradient, at rest (mmHg) | 71.37±42.35 | 72.886±33.62 | 73.94±32.22 | 71.70±27.65 | 0.968 |
| AF (n, %) | 10 (27.02%) a | 50 (10.20%) | 41 (19.43%) a | 6 (35.29%) a | <0.001 |
is compared with TSH 0.55~2.49mIU/L group (normal control group).
Univariate Logistic Regression Analysis of Thyroid Hormone Level and Atrial Fibrillation in Patients With Hypertrophic Obstructive Cardiomyopathy
Age: (OR: 1.045, 95%CI: 1.027~1.063,p<0.001), NT-proBNP(Per 100 fmol/mL):(OR: 1.017,95%CI:1.006~1.029,p=0.003),serum-creatinine:(OR:1.013, 95%CI:1.004~1.022,p=0.006),FT3:(OR:0.616,95%CI:0.392~0.968,p=0.035),FT4:(OR: 3.336, 95%CI:1.483~7.503,p=0.004) ( Table 3 ).
Table 3.
Univariate logistic regression analysis of atrial fibrillation in patients with HOCM.
| OR | 95%CI | P-value | |
|---|---|---|---|
| Female | 1.025 | 0.675-1.555 | 0.908 |
| Age (years) | 1.045 | 1.027-1.063 | <0.001 |
| NT-proBNP (per 100 fmol/mL) | 1.017 | 1.006-1.029 | 0.003 |
| Serum creatinine (µmol/L) | 1.013 | 1.004-1.022 | 0.006 |
| FT3 (pg/mL) | 0.616 | 0.392-0.968 | 0.035 |
| FT4 (ng/dL) | 3.336 | 1.483-7.503 | 0.004 |
Multivariate Logistic Regression Analysis of TSH Level and the Risk of Atrial Fibrillation
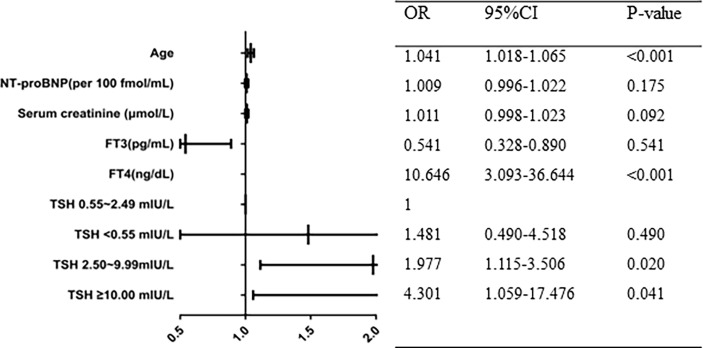
After adjusting for the common risk factor (age, NT-proBNP, serum creatinine, FT3, and FT4), stepwise multiple logistic regression analysis revealed that TSH levels were significantly related to AF incidence.Compared to patients with TSH (0.55 ~ 2.49 mIU/L) group, the adjusted odds ratio of AF for TSH(<0.55) group, TSH (2.50~9.99) group, TSH (≥10.00 mIU/L) group were 1.481 (95% CI 0.485~4.518,P=0.490), 1.977 (95%CI 1.115~3.506, p=0.02), 4.301 (95%CI 1.059~17.476, P=0.041), respectively ( Figure 1 ).
Figure 1.
Multivariate logistic regression analysis of atrial fibrillation in patients with HOCM.
Discussion
This study explored the relationship between thyroid function and atrial fibrillation in patients with hypertrophic obstructive cardiomyopathy. In this study, the incidence of hypertrophic obstructive cardiomyopathy complicated with atrial fibrillation was about 14%, which was significantly higher than that of 2% - 4% in the general population (16), but lower than the previous hypertrophic cardiomyopathy in which the incidence rate of atrial fibrillation is 18-32% (17). Previous studies have shown that the prevalence and incidence rate of atrial fibrillation are different in different regions. The incidence rate of atrial fibrillation in the Asian population is lower than that in North America or Europe (18). This difference may be related to the underestimation of the prevalence of atrial fibrillation in the Asia Pacific region. At the same time, it also suggests that we should pay attention to the screening of atrial fibrillation in patients with hypertrophic cardiomyopathy.
This study found that the increase or decrease of TSH as a sensitive indicator of thyroid function can increase the occurrence of atrial fibrillation. In patients with hypertrophic obstructive cardiomyopathy complicated with abnormal TSH, the high incidence of atrial fibrillation may be due to the local or systemic effect of inflammatory mediators. At the same time, in univariate logistic regression analysis, it was found that the increase in age, the rise of NT-proBNP level, the rise in serum creatinine level, and the abnormality of FT3 and FT4 were significantly related to AF incidence. After adjusting for age, NT-proBNP, serum creatinine, FT3, FT4, and other risk factors, multivariate logistic regression analysis showed that the increase of TSH was an independent risk factor for atrial fibrillation in patients with hypertrophic obstructive cardiomyopathy and had predictive value for the prognosis of hypertrophic obstructive cardiomyopathy. This study further supports the hypothesis of thyroid hormone levels on hypertrophic cardiomyopathy.
In this study,the incidence of atrial fibrillation in TSH (0.55~2.49mlU/L) group was the lowest (10.20%), while TSH(> 10.00 mIU/L) group was the highest (35.29%). In TSH (< 0.55 mlU/L) group and TSH(2.50 ~ 9.99 mIU/L) group, the incidence of atrial fibrillation was 27.02% and 19.43%, respectively. It seemed that the incidence of atrial fibrillation in patients with hypothyroidism was higher than in patients with hyperthyroidism. The trend of my research results is similar to some previous studies. In a cohort study of 18021 patients with atrial fibrillation, 89% had normal thyroid function, 9% had hypothyroidism, and 2% had hyperthyroidism, suggesting that many patients with hypothyroidism also develop atrial fibrillation (19). Patients with hypothyroidism have abnormally high TSH levels and often insufficient T4 levels. Hypothyroidism also increases the risk of atrial fibrillation. With the deepening of research, researchers also realized that both hyperthyroidism and hypothyroidism will increase the risk of atrial fibrillation. This evidence involves thyroid hormone-induced changes in autoantibodies, inflammation, and ion channels. However, the mechanism of atrial fibrillation in patients with hyperthyroidism or hypothyroidism is very different. The arrhythmia of hyperthyroidism may be mainly due to the up-regulation of hyperdynamic circulation, cardiac structural and functional proteins, ion channels, and gap junction proteins (20–22). Hypothyroidism is associated with a variety of cardiovascular risk factors, such as metabolic syndrome, obesity, hypertensive heart disease, diabetes, and oxidative stress, which in turn can lead to atrial fibrillation (23–25). Hypothyroidism can reduce heart rate, prolong the atrial effective refractory period, increase atrial collagen in hypothyroid animals, and promote myocardial fibrosis. This leads to conduction heterogeneity and QT dispersion, which increases the risk of atrial fibrillation (26).
Some studies of non hypertrophic cardiomyopathy found that there is a certain relationship between TSH and the prevalence of atrial fibrillation. A previous study showed that (27), an apparent linear relationship between levels of thyroid dysfunction and atrial fibrillation risk—that is, a low atrial fibrillation risk in hypothyroid patients, a high risk in hyperthyroidism, and a TSH level-dependent (a dose-response relation) increased risk of atrial fibrillation in all levels of hyperthyroid disease, even in high normal euthyroid subjects. Notably, in subjects with reduced serum TSH levels but normal free thyroid hormone levels the risk of developing atrial fibrillation was increased by approximately 10% in individuals with high normal thyroid function and increased about 40% in those with subclinical hyperthyroidism with suppressed TSH levels. Another study shows that (28), the risk of AF increased with low normal TSH levels and slightly decreased with higher TSH levels (but remaining close to a hazard ratio [HR] of 1.0) compared to the reference level of 3.5mIU/l.
Previous studies have confirmed that different types of hypothyroidism, including subclinical hypothyroidism, low T3 syndrome, and clinical hypothyroidism, can affect the long-term prognosis of cardiovascular disease (29, 30). Animal experiments have confirmed that thyroid hormone has many effects on the cardiovascular system (31). Thyroid hormone can directly affect the metabolism and functional protein expression of cardiomyocytes and the remodeling of myocardial interstitium and microcirculation and electrophysiological disorders (32). In the state of hyperthyroidism, myocardial hypertrophy and a decrease of collagen fibers in the myocardial interstitium can be observed, which is related to the increase of matrix metalloproteinase-1 by thyroid hormone (33). Under the condition of hypothyroidism, collagen accumulation occurred in myocardial tissue. Thyroid hormone must affect the role of myocardial matrix collagen (34). In animal experiments, hypothyroidism has been shown to contribute to myocardial fibrosis and cause electrophysiological disorders (35). In 1992, Yao J et al. first reported that thyroid hormone could induce cardiac hypertrophy. This pathological change was characterized by reduced biosynthesis at type I collagen’s mRNA and protein levels (32). In vitro experiments conducted by Chen WJ et, al. showed that hypothyroidism could lead to an increase in the concentration of mRNA expressing pro-α1 (I) collagen, and this response can be inhibited by thyroid hormone receptors (TR-β1) (34). The conclusion of our study is consistent with that of the above basic research. It is well known that T3 is important for cardiac remodeling. In our study, for patients with obstructive hypertrophic cardiomyopathy complicated with atrial fibrillation, the FT4 value is high, but the FT3 value is low, and the possible mechanisms are diverse. Previous studies have shown that there may be obstacles in the process of T4 to T3 in the state of heart failure (36), We speculate that a similar mechanism may exist in patients with hypertrophic cardiomyopathy complicated with atrial fibrillation.
In this study, elevated TSH was an independent risk factor for atrial fibrillation in patients with HOCM. Therefore, the level of thyroid function should be regarded as an essential factor in evaluating the prognosis of HOCM. In addition, animal studies have shown that thyroid hormone replacement therapy can inhibit or even reverse cardiac cardiomyocyte fibrosis, which provides a further reference for the Future Treatment of hypertrophic cardiomyopathy, prevention of atrial fibrillation, and improvement of its prognosis (37, 38).
This study is a cross-sectional study; the sample size is limited, and there are some limitations. A large cohort study needs to verify further the correlation between thyroid hormone levels and survival and myocardial injury in patients with hypertrophic cardiomyopathy. However, this study found that abnormal TSH can predict the risk of atrial fibrillation in patients with hypertrophic obstructive cardiomyopathy, which can provide a reference for clinicians in the prognosis and treatment of patients with hypertrophic cardiomyopathy.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by The Ethics Committee approved it of the Fuwai Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
Study concept and design: Y-DT, W-YW, XM, X-LW. Acquisition, analysis, or interpretation of data: Y-DT, XM, W-YW, KZ, JG, J-LZ, Z-YZ. Drafting of the manuscript: XM, X-LW, W-YW, KZ, CS, Y-DT, Z-YZ. Critical revision of the manuscript for important intellectual content: all authors. English language editing: KZ. Statistical analysis: XM, W-YW, X-LW, Y-PL, J-JW. Obtained funding: Y-DT. Study supervision: Y-DT.
Funding
This work was supported by the National Key Research and Development Program of China (2020YFC2004700, 2020YFC2004705), National Natural Science Foundation of China (81800327, 81900272,81825003, 91957123), Beijing Municipal Commission of Science and Technology (Z181100006318005), and the Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (CIFMS 2016-I2M-1-009), Project of Henan Medical Science and Technology Research Program 2019 (LHGJ20190781), Beijing Municipal Commission of Science and Technology (Z171100000417021).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1. Cappola AR, Fried LP, Arnold AM, Danese MD, Kuller LH, Burke GL, et al. Thyroid Status, Cardiovascular Risk, and Mortality in Older Adults. JAMA (2006) 295(9):1033–41. doi: 10.1001/jama.295.9.1033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Walsh JP, Bremner AP, Bulsara MK, O'Leary P, Leedman PJ, Feddema P, et al. Subclinical Thyroid Dysfunction as a Risk Factor for Cardiovascular Disease. Arch Intern Med (2005) 165(21):2467–72. doi: 10.1001/archinte.165.21.2467 [DOI] [PubMed] [Google Scholar]
- 3. Wang WY, Tang YD, Yang M, Cui C, Mu M, Qian J, et al. Free Triiodothyronine Level Indicates the Degree of Myocardial Injury in Patients With Acute ST-Elevation Myocardial Infarction. Chin Med J (Engl) (2013) 126(20):3926–9. doi: 10.3760/cma.j.issn.0366-6999.20130087 [DOI] [PubMed] [Google Scholar]
- 4. Xu Y, Guo Y, Wang WY, Xun Y, Kuo Z, Min Y, et al. Thyroid Dysfunction is Associated With Atrial Fibrillation in Patients With Stable Angina Pectoris. Chin J Cardiovasc Dis (2014) 42(5):374–8. doi: 10.3760/cmiLj.issn.0253-3758.2014.05.005 [DOI] [PubMed] [Google Scholar]
- 5. Liu YI, Zou Y-B, Sun K, Wang JZ, Wang XJ, Yuan JQ, et al. Comparison of Clinical Characteristics Between Apical Hypertrophic Cardiomyopathy and Typical Hypertrophic Cardiomyopathy. Chin J Cardiovasc Dis (2011) 39(3):228–32. doi: 10.3760/cma.j.issn.0253-3758.2011.03.013 [DOI] [PubMed] [Google Scholar]
- 6. Tang Y, Tang B, Fang Q, Xiaowei Y. Retrospective Analysis of Clinical Characteristics and Long-Term Prognosis of Hypertrophic Cardiomyopathy. Chin J Geriatric Cardiovasc Cerebrovascular Dis (2008) 10(3):170–2. doi: 10.3969/j.issn.1009-0126.2008.03.004 [DOI] [Google Scholar]
- 7. Meng X, Liang M, Shi Y, Zhang W, Zhou S, Gao C. Effects of Surgical Septal Myectomy on Survival in Patients With Hypertrophic Obstructive Cardiomyopathy[J]. Anatol J Cardiol (2020) 23(6):342–8. doi: 10.14744/AnatolJCardiol.2020.05043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Meng X, Wang WY, Gao J, Zhang K, Zheng J, Wang JJ, et al. Hypertrophic Obstructive Cardiomyopathy: Comparison of Outcomes After Myectomy or Alcohol Ablation. Front Cardiovasc Med (2022) 9:755376. doi: 10.3389/fcvm.2022.755376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Olivotto I, Cecchi F, Casey SA, Dolara A, Traverse JH, Maron BJ. Impact of Atrial Fibrillation on the Clinical Course of Hypertrophic Cardiomyopathy. Circulation (2001) 104(21):2517–24. doi: 10.1161/hc4601.097997 [DOI] [PubMed] [Google Scholar]
- 10. Xu Z, Zhu W, Ma J, Hu J, Honeysuckle . Hypertrophic Cardiomyopathy Complicated With Atrial Fibrillation. Chin J Cardiovasc Dis (2017) 45(Issue 9):743–37. doi: 10.3760/cma.j.issn.0253-3758.2017.09.00 [DOI] [Google Scholar]
- 11. Chen S, Yuan J, Qiao S, Tian Y, Duan F, Hu F, et al. A High-Normal Thyrotropin Level is Associated With the Severity of Left Ventricular Diastolic Dysfunction in Patients With Hypertrophic Cardiomyopathy. Kardiol Pol (2013) 71(2):143–51. doi: 10.5603/KP.2013.0007 [DOI] [PubMed] [Google Scholar]
- 12. Cardiovascular Society of Chinese Medical Association, Cardiomyopathy CwGodato . Diagnosis and Treatment of Cardiomyopathy. Chin J Cardiovasc Dis (2007) 35:5–16. doi: 10.3760/j:issn:0253-3758.2007.01.003 [DOI] [Google Scholar]
- 13. Gersh BJ, Maron BJ, Bonow RO, Dearani JA, Fifer MA, Link MS, et al. 2011 ACCF/AHA Guideline for the Diagnosis and Treatment of Hypertrophic Cardiomyopathy: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation (2011) 124(24):e783–831. doi: 10.1161/CIR.0b013e318223e2bd [DOI] [PubMed] [Google Scholar]
- 14. Rodondi N, Den Elzen WP, Bauer DC, Cappola AR, Razvi S, Walsh JP, et al. Subclinical Hypothyroidism and the Risk of Coronary Heart Disease and Mortality. JAMA (2010) 304(12):1365–74. doi: 10.1001/jama.2010.1361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lip GYH, Halperin JL, Tse HF. The 2010 European Society of Cardiology Guidelines on the Management of Atrial Fibrillation: An Evolution or Revolution? Chest (2011) 139(4):738–41. doi: 10.1378/chest.10-2763 [DOI] [PubMed] [Google Scholar]
- 16. Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation (2019) 139(10):e56–e528. doi: 10.1161/cir.0000000000000659 [DOI] [PubMed] [Google Scholar]
- 17. Macintyre C, Lakdawala NK. Management of Atrial Fibrillation in Hypertrophic Cardiomyopathy. Circulation (2016) 133(19):1901–5. doi: 10.1161/circulationaha.115.015085 [DOI] [PubMed] [Google Scholar]
- 18. Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, et al. Worldwide Epidemiology of Atrial Fibrillation: A Global Burden of Disease 2010 Study. Circulation (2014) 129(8):837–47. doi: 10.1161/circulationaha.113.005119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Goldstein SA, Green J, Huber K, Wojdyla DM, Lopes RD, Alexander JH, et al. Characteristics and Outcomes of Atrial Fibrillation in Patients With Thyroid Disease (From the ARISTOTLE Trial). Am J Cardiol (2019) 124(9):1406–12. doi: 10.1016/j.amjcard.2019.07.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jia G, Sowers JR. Autoantibodies of β-Adrenergic and M2 Cholinergic Receptors: Atrial Fibrillation in Hyperthyroidism. Endocrine (2015) 49(2):301–3. doi: 10.1007/s12020-015-0556-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kahaly GJ, Bartalena L, Hegedüs L, Leenhardt L, Poppe K, Pearce SH. 2018 European Thyroid Association Guideline for the Management of Graves' Hyperthyroidism. Eur Thyroid J (2018) 7(4):167–86. doi: 10.1159/000490384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kahaly GJ, Dillmann WH. Thyroid Hormone Action in the Heart. Endocr Rev (2005) 26(5):704–28. doi: 10.1210/er.2003-0033 [DOI] [PubMed] [Google Scholar]
- 23. Ogbera AO, Kuku S, Dada O. The Metabolic Syndrome in Thyroid Disease: A Report From Nigeria. Indian J Endocrinol Metab (2012) 16(3):417–22. doi: 10.4103/2230-8210.95688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Benjamin EJ, Levy D, Vaziri SM, D'Agostino RB, Belanger AJ, Wolf PA. Independent Risk Factors for Atrial Fibrillation in a Population-Based Cohort. The Framingham Heart Study. JAMA (1994) 271(11):840–4. doi: 10.1001/jama.271.11.840 [DOI] [PubMed] [Google Scholar]
- 25. Wang JJ, Zhuang ZH, Shao CL, Yu CQ, Wang WY, Zhang K, et al. Assessment of Causal Association Between Thyroid Function and Lipid Metabolism: A Mendelian Randomization Study. Chin Med J (Engl) (2021) 134(9):1064–9. doi: 10.1097/cm9.0000000000001505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Zhang Y, Dedkov EI, Teplitsky D, Weltman NY, Pol CJ, Rajagopalan V, et al. Both Hypothyroidism and Hyperthyroidism Increase Atrial Fibrillation Inducibility in Rats. Circ Arrhythm Electrophysiol (2013) 6(5):952–9. doi: 10.1161/circep.113.000502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Selmer C, Olesen JB, Hansen ML, Lindhardsen J, Olsen AM, Madsen JC, et al. The Spectrum of Thyroid Disease and Risk of New Onset Atrial Fibrillation: A Large Population Cohort Study. Bmj (2012) 345:e7895. doi: 10.1136/bmj.e7895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Baumgartner C, Da Costa BR, Collet TH, Feller M, Floriani C, Bauer DC, et al. Thyroid Function Within the Normal Range, Subclinical Hypothyroidism, and the Risk of Atrial Fibrillation. Circulation (2017) 136(22):2100–16. doi: 10.1161/circulationaha.117.028753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wang W, Guan H, Gerdes AM, Iervasi G, Yang Y, Tang YD. Thyroid Status, Cardiac Function, and Mortality in Patients With Idiopathic Dilated Cardiomyopathy. J Clin Endocrinol Metab (2015) 100(8):3210–8. doi: 10.1210/jc.2014-4159 [DOI] [PubMed] [Google Scholar]
- 30. Zhang K, Meng X, Wang W, Zheng J, An S, Wang S, et al. Prognostic Value of Free Triiodothyronine Level in Patients With Hypertrophic Obstructive Cardiomyopathy. J Clin Endocrinol Metab (2018) 103(3):1198–205. doi: 10.1210/jc.2017-02386 [DOI] [PubMed] [Google Scholar]
- 31. Gerdes AM, Ojamaa K. Thyroid Hormone and Cardioprotection. Compr Physiol (2016) 6(3):1199–219. doi: 10.1002/cphy.c150012 [DOI] [PubMed] [Google Scholar]
- 32. Yao J, Eghbali M. Decreased Collagen Gene Expression and Absence of Fibrosis in Thyroid Hormone-Induced Myocardial Hypertrophy. Response of Cardiac Fibroblasts to Thyroid Hormone In Vitro. Circ Res (1992) 71(4):831–9. doi: 10.1161/01.res.71.4.831 [DOI] [PubMed] [Google Scholar]
- 33. Ghose Roy S, Mishra S, Ghosh G, Bandyopadhyay A. Thyroid Hormone Induces Myocardial Matrix Degradation by Activating Matrix Metalloproteinase-1. Matrix Biol (2007) 26(4):269–79. doi: 10.1016/j.matbio.2006.12.005 [DOI] [PubMed] [Google Scholar]
- 34. Chen WJ, Lin KH, Lee YS. Molecular Characterization of Myocardial Fibrosis During Hypothyroidism: Evidence for Negative Regulation of the Pro-Alpha1(I) Collagen Gene Expression by Thyroid Hormone Receptor. Mol Cell Endocrinol (2000) 162(1-2):45–55. doi: 10.1016/S0303-7207(00)00203-3 [DOI] [PubMed] [Google Scholar]
- 35. Tang YD, Kuzman JA, Said S, Anderson BE, Wang X, Gerdes AM. Low Thyroid Function Leads to Cardiac Atrophy With Chamber Dilatation, Impaired Myocardial Blood Flow, Loss of Arterioles, and Severe Systolic Dysfunction. Circulation (2005) 112(20):3122–30. doi: 10.1161/CIRCULATIONAHA.105.572883 [DOI] [PubMed] [Google Scholar]
- 36. Olivares EL, Marassi MP, Fortunato RS, da Silva AC, Costa-e-Sousa RH, Araujo IG, et al. Thyroid Function Disturbance and Type 3 Iodothyronine Deiodinase Induction After Myocardial Infarction in Rats a Time Course Study. Endocrinology (2007) 148(10):4786–92. doi: 10.1210/en.2007-0043 [DOI] [PubMed] [Google Scholar]
- 37. Chen J, Ortmeier SB, Savinova OV, Nareddy VB, Beyer AJ, Wang D, et al. Thyroid Hormone Induces Sprouting Angiogenesis in Adult Heart of Hypothyroid Mice Through the PDGF-Akt Pathway. J Cell Mol Med (2012) 16(11):2726–35. doi: 10.1111/j.1582-4934.2012.01593.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Khalife WI, Tang YD, Kuzman JA, Thomas TA, Anderson BE, Said S, et al. Treatment of Subclinical Hypothyroidism Reverses Ischemia and Prevents Myocyte Loss and Progressive LV Dysfunction in Hamsters With Dilated Cardiomyopathy. Am J Physiol Heart Circ Physiol (2005) 289(6):H2409–2415. doi: 10.1152/ajpheart.00483.2005 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.