FIGURE 4.
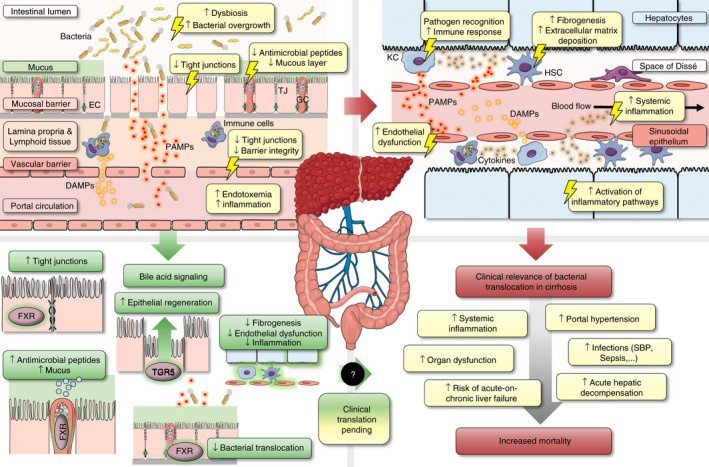
Bacterial translocation in cirrhosis: Pathophysiological aspects and therapeutic implications of bile acid signalling in the gut‐liver axis. Left upper panel: Advanced chronic liver disease (or cirrhosis) is associated with increased bacterial translocation, which is characterised by (i) dysbiosis and small intestinal bacterial overgrowth, (ii) reduced excretion of antibacterial peptides and mucus thickness, (iii) disruption of epithelial integrity associated with reduced expression of tight junction (TJ) proteins, and (iv) an impaired gut‐vascular barrier, which enables the translocation of gut bacteria and danger/pathogen associated molecular patterns (PAMPs/DAMPs) into the portal circulation. Right upper panel: Bacterial translocation induces—directly or indirectly—an intrahepatic inflammatory response, which comprises (i) activation of Kupffer cells (KC) and other immune cells associated with increased shedding of cytokines and systemic inflammation, (ii) activation of hepatic stellate cells (HSC) and induction of fibrogenesis and (iii) endothelial dysfunction of liver sinusoidal epithelial cells (LSEC) which aggravates portal hypertension. Left lower panel: Bile acid signaling may ameliorate intestinal barrier integrity and bacterial translocation via FXR‐ and TGR5‐mediated upregulation of antibacterial defense, TJ proteins, epithelial regeneration, which ultimately leads to amelioration of fibrogenesis, endothelial dysfunction and systemic inflammation in cirrhosis (data based on experimental studies in animals). Right lower panel: The clinical relevance of bacterial translocation in cirrhosis is underlined by the association of portal hypertension and systemic inflammation with the incidence of clinical complications that are associated with increased mortality. Abbreviations: DAMPs/PAMPs, danger/pathogen associated molecular patterns; EC, enterocyte; FXR, farnesoid X receptor; GC, goblet cell; HSC, hepatic stellate cell; KC, Kupffer cell; LSEC, liver sinusoidal epithelial cell; TGR5, transmembrane G protein‐coupled receptor‐5; TJ, tight junction
