Fig 3.
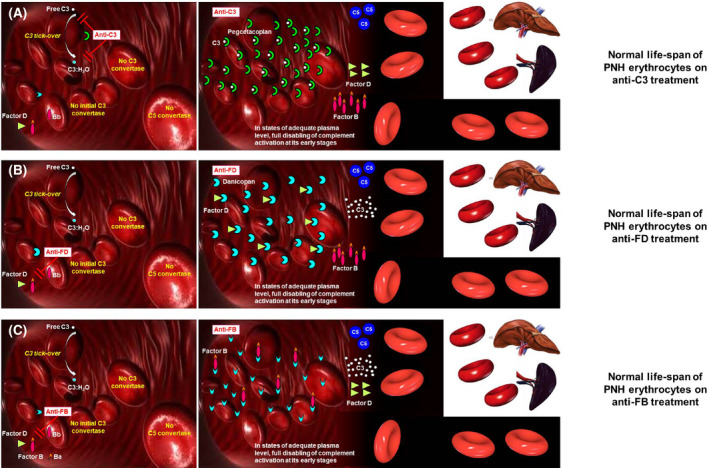
Biology of complement‐mediated haemolysis in PNH on proximal complement inhibitors. (A) Modulation of complement activation on PNH erythrocytes on C3 inhibitors. The C3 inhibitor pegcetacoplan binds C3 in its naive and activated forms, eventually preventing the generation of C3 convertases on the surface of PNH erythrocytes. If the inhibition is pharmacologically sustained, the complement cascade is disabled in its early phases, resulting in inhibition of the MAC‐mediated intravascular haemolysis, and in the prevention of C3 opsonization (and thus of extra‐vascular haemolysis). (B) Modulation of complement activation on PNH erythrocytes on factor D inhibitors. The factor D inhibitor danicopan binds factor D, eventually preventing the cleavage of factor B, which is needed to generate C3 convertases. If the inhibition is pharmacologically sustained, the complement cascade is disabled in its early phases, resulting in inhibition of the MAC‐mediated intravascular haemolysis, and in the prevention of C3 opsonization (and thus of extra‐vascular haemolysis). (C) Modulation of complement activation on PNH erythrocytes on anti‐factor B inhibitors. The factor B inhibitor iptacopan binds factor B, eventually preventing its cleavage needed to generate C3 convertases. If the inhibition is pharmacologically sustained, the complement cascade is disabled in its early phases, resulting in inhibition of the MAC‐mediated intravascular haemolysis, and in the prevention of C3 opsonization (and thus of extra‐vascular haemolysis). MAC, membrane attack complex; PNH, paroxysmal nocturnal haemoglobinuria.
