Abstract
Context
In the multifaceted COVID-19 clinical scenario characterized by a multi-system disorder with negative implications not only on respiratory function but also on cardiac, hematological, neurological and endocrine-metabolic systems, a distinctive osteo-metabolic phenotype with an independent influence on disease severity and recovery of patients affected was early reported.
Aim
To summarize and update the main evidences regarding the distinct components of this phenotype in acute and Long COVID-19, reinforcing its clinical relevance and discussing the main pathophysiological and clinical-therapeutic implications of the most recent reported findings.
Results
This emerging phenotype is characterized by a widespread acute hypocalcemia and hypovitaminosis D with an impaired compensatory parathyroid hormone response, and a high prevalence of skeletal complications such as vertebral fractures. The clinical relevance of this osteo-metabolic phenotype on acute COVID-19 is well characterized, and novel seminal evidences are progressively highlighting its importance also in predicting patient’s long-term outcomes and Long COVID-19 occurrence.
Conclusions
These findings reinforced the central role of a multidisciplinary team, including endocrinologists, in evaluating these patients for a proactive search of each aspect of the osteo-metabolic phenotype components since they may represent suitable therapeutic targets to prevent SARS-CoV-2 infection, poor COVID-19 outcomes, Long COVID-19 occurrence and even possibly better responses to COVID-19 vaccination.
Keywords: Osteo-metabolic phenotype, Vertebral fractures, COVID-19, Hypocalcemia, Long-COVID, Vitamin D
Introduction
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has led to a long-lasting pandemic with a dramatic impact worldwide. During the early pandemic spread, several emerging findings have progressively defined COVID-19 as a multi-system disorder and not only as a respiratory disease, with negative implications on cardiac, hematological, neurological, gastrointestinal and, not surprisingly, also on endocrine and metabolic system [1–5]. Diabetes mellitus and obesity were early identified as frequent comorbidities and independent risk factors for severe COVID-19 [6]. Thyroid and pituitary disorders were reported as disease complications possibly due to the inflammatory-(auto)immune dysfunctions and/or direct viral damage since the ubiquitous tissue presence of the angiotensin-converting enzyme 2 (ACE2), the main recognized receptor for SARS-CoV-2 entry [7–9]. In this multifaceted COVID-19 endocrine scenario, a distinctive osteo-metabolic phenotype with an independent influence on disease severity and recovery of patients affected, was early reported [10]. This phenotype is characterized by a widespread acute hypocalcemia, hypovitaminosis D with an impaired compensatory parathyroid hormone (PTH) response, and high prevalence of skeletal complications such as vertebral fractures (VFs).
Aim of this review is to summarize and update the main evidences regarding the distinct components of the osteo-metabolic phenotype in COVID-19, discussing main pathophysiological and clinical-therapeutic implications of the most recent reported findings and understanding if this phenotype is somewhat strengthened and reinforced in its clinical relevance by recent literature.
Hypocalcemia
During the first pandemic spread in Europe, low calcium levels early appeared as a very common biochemical finding. Starting from the first seminal observation showing a case of severe acute hypocalcemia in an Italian patient previously thyroidectomized with SARS-CoV-2 infection [11], several studies conducted worldwide, in order to evaluate the possible causal or casual relationship between COVID-19 and hypocalcemia, reported an unexpected high prevalence of low calcium levels, ranging from 62.6 to 87.2% of patients, depending on the hypocalcemia definition used [12–15].
Hypocalcemia was identified as a distinctive specific feature of COVID-19 reported more frequently in patients affected by SARS-CoV-2 infection than in those with other viral or bacterial pneumonia presenting with the same baseline clinical parameters [16, 17]. Moreover, hypocalcemia was highly prevalent even in non-severe COVID-19 patients, possibly implying that it was intrinsic to the disease and not-only influenced by acute illness [18].
Calcium levels were negatively associated with inflammatory, coagulopathy and organ-injury parameters, and hypocalcemia was recognized as an independent risk factor for COVID-19 worse outcomes [13–15], representing a strongly reliable and easy-to-measure biomarker of disease severity. These findings were confirmed by following systematic reviews and meta-analyses reporting that hypocalcemia was significantly associated with disease severity, hospitalization, length of hospitalization, admission to the intensive care unit and mortality risk [19, 20].
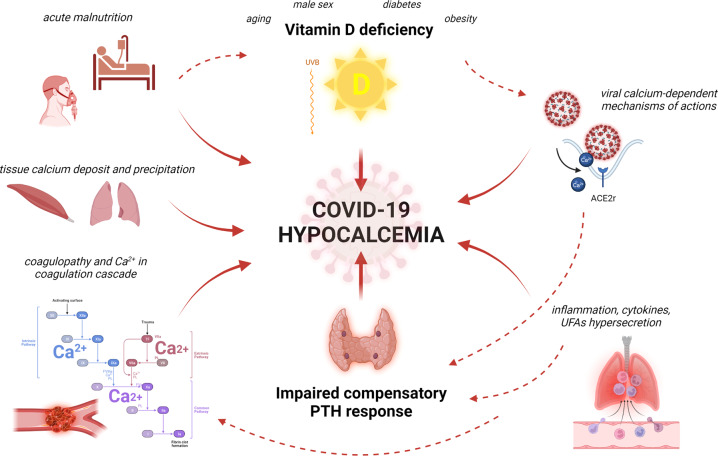
Several pathophysiological factors have been hypothesized to potentially play a role in determining hypocalcemia in COVID-19 [12, 21] (Fig. 1). These mechanisms include calcium-dependent viral mechanisms of action determining intra and extra-cellular cation dysmetabolism [22–24], tissues calcium deposits detected at autoptic evaluation [25], acute muscle calcium precipitation [26], calcium role in coagulation and prothrombotic status [27, 28], acute malnutrition during critical illness [29], high levels of unbound and unsaturated fatty acids in inflammatory responses [30] and high prevalence of hypovitaminosis D with an impaired compensatory PTH response [31]. Furthermore, severe hypocalcemia, although not frequently found in COVID-19 [3, 13], may compromise outcome per se due to its additional negative cardiovascular and neurological impact [3, 13]. Thus, since hypocalcemia is a frequent biochemical finding in patients with acute COVID-19 predicting poor clinical outcomes, we find reasonable to measure in these patients calcium levels at hospital admission, and to monitor them during hospitalization. In particular, severe and acute hypocalcemia can represent a life-threatening emergency with possible negative cardiovascular and neurological complications potentially fatal in hospitalized patients with severe COVID-19 who are per se at risk of developing such complications [32]. Therefore, despite the absence of specific guidelines [33], it can be considered to provide an adequate replacement treatment in those with moderate to severe or symptomatic hypocalcemia according to published recommendations for treatment of hypoparathyroidism [34] which based on the severity of hypocalcemia range from oral calcium and Vitamin D3 or active Vitamin D (VD) supplements to intravenous calcium gluconate.
Fig. 1.
The proposed pathophysiological mechanisms underlying hypocalcemia in COVID-19. Red solid arrow lines indicate the negative influence of the main pathophysiological mechanisms (Vitamin D deficiency; Impaired compensatory PTH response; viral calcium-dependent mechanisms of actions; cytokines and UFAs hypersecretion; acute malnutrition; coagulopathy; tissue calcium deposit) on hypocalcemia occurrence; red dashed arrow lines indicate the negative influence between each of these mechanisms
Finally, in COVID-19 survivors, more than 3 months after negative test for SARS-CoV-2, a non-significant difference in calcium levels was observed compared to healthy matched for age and sex subjects, possibly confirming the casual relationship between COVID-19 and hypocalcemia, and its transient nature once the patient recovered from the acute viral syndrome [35]. These data does not entirely support a routine estimation of serum calcium in all post-COVID-19 patients [36]. However, it appears reasonable to assess calcium and VD levels in the follow-up of patients with symptomatic hypocalcemia during the acute disease and eventually consider to supplement VD in those with persistently altered biochemical results.
Hypovitaminosis D
A tight link between VD and COVID-19 was hypothesized from the early pandemic spreading due to the VD well known involvement in immune response and immunocompetence both regarding innate and adaptive immunity [37, 38]. VD is known to have antimicrobial roles and antiviral mechanisms of actions, and to regulate the adaptive immune response promoting a shift from proinflammatory to tolerogenic state downregulating the immune responses mediated by T-helper-1 lymphocytes cells, inhibiting the production of pro-inflammatory cytokines and promoting regulatory T cells maturation [39, 40].
Due to its important immune-modulating role and its widespread deficiency particularly in European Mediterranean Countries (which were heavily impacted by the pandemic), hypovitaminosis D was early reported as a possible risk factor for SARS-CoV-2 infection, severe COVID-19 and worse clinical outcomes. These only-observational findings were confirmed by several large systematic reviews and meta-analyses involving nearly 2 million adults, strongly suggesting the negative impact of hypovitaminosis D in COVID-19 patients [41–44].
In the light of the known pathophysiological role of VD and hypovitaminosis D underlying the main conditions and comorbidities related to severe COVID-19, such as older age [45], male sex [46, 47], diabetes mellitus [6, 48, 49], visceral adiposity/overweight/obesity [50, 51], and hypocalcemia, VD deficiency was suggested to represent the possible common denominator of the endocrine phenotype of COVID-19 [52], as confirmed also by the observational data reporting high prevalence of low VD levels particularly in older, male, diabetic and overweight patients [53, 54]. Given these data, VD was suggested to have a primary role in the prevention of infection and severe disease and reaching an adequate VD level especially in the population at high risk of both hypovitaminosis D and COVID-19 was recommended as a preventive measure [55, 56]. The effect of VD supplementation in general population and in COVID-19 patients was evaluated by several observational studies and randomized controlled trials, with different treatment strategies, reporting initially contrasting results. However, recent systematic reviews and meta-analyses concluded that VD supplementation was strongly effective in reducing rates of viral test positivity and COVID-19 severity [57–60].
Besides the above reported role of hypovitaminosis D in acute COVID-19, its function in patients’ recovery after acute infection and in the pathophysiology of the Long-COVID or Post-acute COVID-19 syndrome characterized especially by neuromuscular, respiratory, and nutritional disorders [61, 62] is still poorly evaluated. VD is known to play key-roles in several metabolic pathways involved in musculoskeletal health [51], and, in previous studies, VD supplementation was proven to provide a muscle recovery benefit after intense physical and damaging stress [63–65]. VD levels were also reported to predict and influence illness duration and time until recovery after acute severe pneumonia [66]. To date, the VD role in Long-COVID occurrence was investigated by only few small studies. A recent pilot-study that included elderly patients after acute COVID-19 reported the efficacy of a six-weeks 2.000 IU/day cholecalciferol therapy vs placebo in reducing creatinine kinase values and in showing a positive improvement trend in the general and physical health status [67]. In two other recent studies, no associations between VD levels and the post-COVID symptoms were observed [68, 69].
Nevertheless, it is widely recommended that an appropriate nutritional status evaluation and a personalized dietary management, including VD supplementation, may represent one the best strategy to facilitate COVID-19 survivors’ recovery [70].
Finally, based on the VD immunomodulatory effects, a possible role of hypovitaminosis D in regulating the anti-SARS-CoV-2 vaccination response and the possible VD deficiency-related vaccine side effects [71], should be investigated, although recent findings on anti-COVID vaccination and previous studies on other vaccinations reported contrasting results [72–76].
Impaired compensatory PTH response and hypoparathyroidism
Among the pathophysiological mechanisms underlying hypocalcemia occurrence in COVID-19, in addition to the high prevalence of VD deficiency, a not-adequate compensatory PTH response was recently proposed. VD is a crucial hormone for calcium homeostasis increasing its intestinal absorption and, in subjects with hypovitaminosis D, the increase in PTH (secondary hyperparathyroidism) generally maintains eucalcemia [77].
Severe acute hypocalcemia cases in COVID-19 patients due to the worsening of previous controlled postsurgical and/or primary hypoparathyroidism have been reported [11, 78], suggesting that hypocalcemia in COVID-19 could occur due the acute combination of low VD levels not adequately compensated by PTH response.
Interestingly, a recent study reported that hypocalcemia occurred prevalently in a context of a marked hypovitaminosis D not adequately compensated by secondary hyperparathyroidism, since, despite most of patients presented with quite severe VD deficiency and hypocalcemia, only one-fifth of them had secondary hyperparathyroidism [31]. Other observational studies seem to confirm this evidence: in fact, PTH median levels of 44.2 pg/mL were reported in 162 COVID-19 patients with VD levels below 20 ng/mL [79] and secondary hyperparathyroidism occurred in only 43.3% of 97 COVID-19 patients characterized by a median VD level of 21 ng/mL [80].
The mechanism underlying this impaired PTH response to hypovitaminosis D and hypocalcemia in COVID-19 is yet to be understood. Parathyroid gland function may be impaired during systemic inflammatory response with increased circulating cytokines [81]. In addition, respiratory alkalosis, typically observed in COVID-19, was reported to increase the PTH resistance at renal receptor level, resulting in hypocalcemia without increase in PTH levels [82]. Moreover, previous autoptic studies conducted during SARS epidemic identified viral RNA and antigenic materials in parathyroid gland cells, and expression of ACE2 receptors in parathyroid glands cells has been, although not consistently, reported [83, 84]. Therefore, SARS-CoV-2 may potentially directly affect the parathyroid glands by binding the ACE2 receptors. Supporting this hypothesis, in the literature also three case reports of new-onset primary hypoparathyroidism due to SARS-CoV-2 infection have been reported [85–87]. Finally, both hypermagnesemia and severe hypomagnesemia were reported in COVID-19 patients [88, 89]. Since altered magnesium levels may suppress PTH secretion it can be hypothesized that they may play a role in the determinism of functional hypoparathyroidism [90].
Skeletal complications and vertebral fractures
Morphometric VFs are one of the most relevant clinical manifestations of osteoporosis and skeletal fragility and have been recently reported to be highly prevalent in COVID-19 patients [91]. In the literature, VFs are associated with decreased survival, reduction of respiratory function and impaired quality of life in the general population [91, 92].
In a previous study, COVID-19 patients presenting with VFs required noninvasive mechanical ventilation more frequently and their mortality rate was almost doubled compared to non-fractured patients [84]. Following studies conducted on different patient cohorts partly confirmed these data showing a high prevalence of VFs in COVID-19 patients and a negative influence of lower bone mineral density (BMD) on patient outcomes [93–95].
In fact, in hospitalized COVID-19 patients, several concomitant factors may lead to an increased fracture risk [96–99], such as advanced age and comorbidities including diabetes, cardiovascular diseases and hypertension [100].
Moreover, as reported above, hospitalized COVID-19 patients frequently show hypovitaminosis D, which is known to be associated with lower BMD and increased fractures risk [77]. However, in the available studies on VFs in COVID-19, VD levels were not so far reported.
VFs and decreased BMD are known to increase risk of pneumonia and to impair respiratory function leading to a restrictive pulmonary dysfunction in general population [101–103]. A very recent study, assessing the clinical impact of VFs in COVID-19 survivors on their medium term follow-up respiratory recovery, reported that patients with VFs, detected at hospital admission, had impaired respiratory function compared to those without VFs showing worse spirometric parameters and higher rate of pulmonary function tests abnormalities at six-month follow-up, despite patients in both groups presenting similar acute infectious lung involvement at hospital admission [104]. Therefore, VFs appear to also influence the medium-term impaired respiratory function of COVID-19 survivors which, in turn, may significantly influence their recovery and contribute to Long-COVID occurrence.
These findings suggest that VFs assessment at baseline may help in identifying patients at higher risk of worse clinical outcomes and those needing a more intensive respiratory follow-up. Moreover, patients showing persistent respiratory impairment without evidence of pulmonary disease may benefit from a VFs assessment to prevent the vicious circle of further fractures and respiratory deterioration. Therefore, as anti-osteoporotic treatments, including denosumab, do not only appear to cause an increased predisposition to COVID-19 [105] but even seem to reduce disease risk [106, 107], they should be continued during the pandemic and vaccination campaigns to avoid an increased fracture risk, detrimental in the context of COVID-19 [108].
Conclusions
In conclusion, in the context of the endocrine and metabolic complications of COVID-19, recent literature confirmed the existence, strengthening its clinical relevance, of a distinct osteo-metabolic phenotype which we originally and seminally reported. Specifically, it has recently emerged that high rate of acute hypocalcemia likely occurs in the context of a widespread hypovitaminosis D and of a not adequate compensatory PTH response possibly due also to a direct involvement of the parathyroids in SARS-CoV-2 infection. Moreover, high prevalence of VFs was recently highlighted not only as predictor of poor outcome in acute COVID-19 but also of inadequate respiratory recovery in COVID-19 survivors. The clinical relevance of the osteo-metabolic phenotype on short- and long-term outcomes of the disease confirms the important role of the endocrinologist in the COVID-19 multidisciplinary team [109] for proactive search of the different contributing components since they may all represent suitable therapeutic targets to prevent SARS-CoV-2 infection, poor COVID-19 outcomes, Long-COVID occurrence and even possibly better responses to COVID-19 vaccination.
Author contributions
All authors contributed equally.
Compliance with ethical standards
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gupta A, Madhavan MV, Sehgal K, et al. Extrapulmonary manifestations of COVID-19. Nat. Med. 2020;26(7):1017–1032. doi: 10.1038/s41591-020-0968-3. [DOI] [PubMed] [Google Scholar]
- 2.Puig-Domingo M, Marazuela M, Giustina A. COVID-19 and endocrine diseases. A statement from the European Society of Endocrinology. Endocrine. 2020;68(1):2–5. doi: 10.1007/s12020-020-02294-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Puig-Domingo M, Marazuela M, Yildiz BO, Giustina A. COVID-19 and endocrine and metabolic diseases. An updated statement from the European Society of Endocrinology. Endocrine. 2021;72(2):301–316. doi: 10.1007/s12020-021-02734-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marazuela M, Giustina A, Puig-Domingo M. Endocrine and metabolic aspects of the COVID-19 pandemic [published correction appears in Rev Endocr Metab Disord. 2021 Mar;22(1):145] Rev. Endocr. Metab. Disord. 2020;21(4):495–507. doi: 10.1007/s11154-020-09569-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giustina A, Bilezikian JP. Revisiting the endocrine and metabolic manifestations of COVID-19 two years into the pandemic. Rev. Endocr. Metab. Disord. 2022;23(2):133–136. doi: 10.1007/s11154-022-09716-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou Y, Chi J, Lv W, Wang Y. Obesity and diabetes as high-risk factors for severe coronavirus disease 2019 (Covid-19) Diabetes Metab. Res. Rev. 2021;37(2):e3377. doi: 10.1002/dmrr.3377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scappaticcio L, Pitoia F, Esposito K, Piccardo A, Trimboli P. Impact of COVID-19 on the thyroid gland: an update. Rev. Endocr. Metab. Disord. 2021;22(4):803–815. doi: 10.1007/s11154-020-09615-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Frara S, Allora A, Castellino L, di Filippo L, Loli P, Giustina A. COVID-19 and the pituitary. Pituitary. 2021;24(3):465–481. doi: 10.1007/s11102-021-01148-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frara S, Loli P, Allora A, et al. COVID-19 and hypopituitarism. Rev. Endocr. Metab. Disord. 2022;23(2):215–231. doi: 10.1007/s11154-021-09672-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.di Filippo L, Frara S, Giustina A. The emerging osteo-metabolic phenotype of COVID-19: clinical and pathophysiological aspects. Nat. Rev. Endocrinol. 2021;17(8):445–446. doi: 10.1038/s41574-021-00516-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bossoni S, Chiesa L, Giustina A. Severe hypocalcemia in a thyroidectomized woman with Covid-19 infection. Endocrine. 2020;68(2):253–254. doi: 10.1007/s12020-020-02326-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.di Filippo L, Doga M, Frara S, Giustina A. Hypocalcemia in COVID-19: Prevalence, clinical significance and therapeutic implications. Rev. Endocr. Metab. Disord. 2022;23(2):299–308. doi: 10.1007/s11154-021-09655-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Di Filippo L, Formenti AM, Rovere-Querini P, et al. Hypocalcemia is highly prevalent and predicts hospitalization in patients with COVID-19. Endocrine. 2020;68(3):475–478. doi: 10.1007/s12020-020-02383-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu J, Han P, Wu J, Gong J, Tian D. Prevalence and predictive value of hypocalcemia in severe COVID-19 patients. J. Infect. Public Health. 2020;13(9):1224–1228. doi: 10.1016/j.jiph.2020.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sun JK, Zhang WH, Zou L, et al. Serum calcium as a biomarker of clinical severity and prognosis in patients with coronavirus disease 2019. Aging (Albany NY) 2020;12(12):11287–11295. doi: 10.18632/aging.103526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.di Filippo L, Formenti AM, Doga M, et al. Hypocalcemia is a distinctive biochemical feature of hospitalized COVID-19 patients. Endocrine. 2021;71(1):9–13. doi: 10.1007/s12020-020-02541-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mehta M, Ghani H, Chua F, et al. Retrospective case-control study to evaluate hypocalcaemia as a distinguishing feature of COVID-19 compared with other infective pneumonias and its association with disease severity. BMJ Open. 2021;11(12):e053810. doi: 10.1136/bmjopen-2021-053810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pal R, Ram S, Zohmangaihi D, et al. High prevalence of hypocalcemia in non-severe COVID-19 patients: a retrospective case-control study. Front. Med. (Lausanne) 2021;7:590805. doi: 10.3389/fmed.2020.590805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alemzadeh E, Alemzadeh E, Ziaee M, Abedi A, Salehiniya H. The effect of low serum calcium level on the severity and mortality of Covid patients: a systematic review and meta-analysis. Immun. Inflamm. Dis. 2021;9(4):1219–1228. doi: 10.1002/iid3.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Martha JW, Wibowo A, Pranata R. Hypocalcemia is associated with severe COVID-19: a systematic review and meta-analysis. Diabetes Metab. Syndr. 2021;15(1):337–342. doi: 10.1016/j.dsx.2021.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.di Filippo L, Formenti AM, Giustina A. Hypocalcemia: the quest for the cause of a major biochemical feature of COVID-19. Endocrine. 2020;70(3):463–464. doi: 10.1007/s12020-020-02525-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhou Y, Frey TK, Yang JJ. Viral calciomics: interplays between Ca2+ and virus. Cell Calcium. 2009;46(1):1–17. doi: 10.1016/j.ceca.2009.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berlansky S, Sallinger M, Grabmayr H, et al. Calcium signals during SARS-CoV-2 infection: assessing the potential of emerging therapies. Cells. 2022;11(2):253. doi: 10.3390/cells11020253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cavezzi A, Menicagli R, Troiani E, Corrao S. COVID-19, cation dysmetabolism, sialic acid, CD147, ACE2, viroporins, hepcidin and ferroptosis: a possible unifying hypothesis. F1000Res. 2022;11:102. doi: 10.12688/f1000research.108667.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.COVID-19 Autopsy Electronic address: anapat.hrc@salud.madrid.org. The first COVID-19 autopsy in Spain performed during the early stages of the pandemic. Rev. Esp. Patol. 2020;53(3):182–187. doi: 10.1016/j.patol.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kalbhenn J, Knoerlein J. Intramuscular deposit of calcium is a potential reason for hypocalcaemia in COVID-19. Endocrine. 2021;72(1):24–26. doi: 10.1007/s12020-021-02708-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brass EP, Forman WB, Edwards RV, Lindan O. Fibrin formation: effect of calcium ions. Blood. 1978;52(4):654–658. doi: 10.1182/blood.V52.4.654.654. [DOI] [PubMed] [Google Scholar]
- 28.Qi X, Kong H, Ding W, et al. Abnormal coagulation function of patients with COVID-19 is significantly related to hypocalcemia and severe inflammation. Front. Med. (Lausanne) 2021;8:638194. doi: 10.3389/fmed.2021.638194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Di Filippo L, De Lorenzo R, D’Amico M, et al. COVID-19 is associated with clinically significant weight loss and risk of malnutrition, independent of hospitalisation: a post-hoc analysis of a prospective cohort study. Clin. Nutr. 2021;40(4):2420–2426. doi: 10.1016/j.clnu.2020.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Singh VP, Khatua B, El-Kurdi B, Rood C. Mechanistic basis and therapeutic relevance of hypocalcemia during severe COVID-19 infection. Endocrine. 2020;70(3):461–462. doi: 10.1007/s12020-020-02530-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.di Filippo L, Allora A, Locatelli M, et al. Hypocalcemia in COVID-19 is associated with low vitamin D levels and impaired compensatory PTH response. Endocrine. 2021;74(2):219–225. doi: 10.1007/s12020-021-02882-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.A. Linglart, A.S. Lambert, Approach to patient with severe hypocalcaemia. In Oxford Textbook of Clinical Nephrology, 4th edn, ch. 38, pp 378–383. N. Turner, N. Lameire, D. Goldsmith, C. Winearls, J. Himmelfarb & G. Remuzzi, Eds New York, NY: Oxford University Press, 2015
- 33.Gittoes NJ, Criseno S, Appelman-Dijkstra NM, et al. Endocrinology in the time of COVID-19: Management of calcium metabolic disorders and osteoporosis. Eur. J. Endocrinol. 2020;183(2):G57–G65. doi: 10.1530/EJE-20-0385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tecilazich F, Formenti AM, Frara S, Giubbini R, Giustina A. Treatment of hypoparathyroidism. Best. Pr. Res Clin. Endocrinol. Metab. 2018;32(6):955–964. doi: 10.1016/j.beem.2018.12.002. [DOI] [PubMed] [Google Scholar]
- 35.Gameil MA, Marzouk RE, Elsebaie AH, Rozaik SE. Long-term clinical and biochemical residue after COVID-19 recovery. Egypt Liver J. 2021;11(1):74. doi: 10.1186/s43066-021-00144-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pal R, Joshi A, Bhadada SK, Banerjee M, Vaikkakara S, Mukhopadhyay S. Endocrine follow-up during post-acute COVID-19: Practical recommendations based on available clinical evidence. Endocr. Pr. 2022;28(4):425–432. doi: 10.1016/j.eprac.2022.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.A. Giustina, A.M. Formenti (2020) Does hypovitaminosis D play a role in the high impact of COVID infection in Italy? British Medical Journal Available at: https://www.bmj.com/content/368/bmj.m810/rr-36
- 38.Bouillon R, Marcocci C, Carmeliet G, et al. Skeletal and extraskeletal actions of vitamin D: current evidence and outstanding questions. Endocr. Rev. 2019;40(4):1109–1151. doi: 10.1210/er.2018-00126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bilezikian JP, Bikle D, Hewison M, et al. Mechanisms in endocrinology: vitamin D and COVID-19. Eur. J. Endocrinol. 2020;183(5):R133–R147. doi: 10.1530/EJE-20-0665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Charoenngam N, Holick MF. Immunologic effects of vitamin D on human health and disease. Nutrients. 2020;12(7):2097. doi: 10.3390/nu12072097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dissanayake HA, de Silva NL, Sumanatilleke M, et al. Prognostic and therapeutic role of vitamin D in COVID-19: systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 2022;107(5):1484–1502. doi: 10.1210/clinem/dgab892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hopefl R, Ben-Eltriki M, Deb S. Association between vitamin D levels and inflammatory markers in COVID-19 patients: a meta-analysis of observational studies. J. Pharm. Pharm. Sci. 2022;25:124–136. doi: 10.18433/jpps32518. [DOI] [PubMed] [Google Scholar]
- 43.Chiodini I, Gatti D, Soranna D, et al. Vitamin D status and SARS-CoV-2 infection and COVID-19 clinical outcomes. Front Public Health. 2021;9:736665. doi: 10.3389/fpubh.2021.736665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Akbar MR, Wibowo A, Pranata R, Setiabudiawan B. Low Serum 25-hydroxyvitamin D (Vitamin D) level is associated with susceptibility to COVID-19, severity, and mortality: a systematic review and meta-analysis [published correction appears in Front Nutr. 2021 Sep 27;8:754539] Front Nutr. 2021;8:660420. doi: 10.3389/fnut.2021.660420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Giustina A, Adler RA, Binkley N, et al. Controversies in vitamin D: summary statement from an international conference. J. Clin. Endocrinol. Metab. 2019;104(2):234–240. doi: 10.1210/jc.2018-01414. [DOI] [PubMed] [Google Scholar]
- 46.Giustina A, Adler RA, Binkley N, et al. Consensus statement from 2nd International Conference on Controversies in Vitamin D. Rev. Endocr. Metab. Disord. 2020;21(1):89–116. doi: 10.1007/s11154-019-09532-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brandi ML, Giustina A. Sexual dimorphism of coronavirus 19 morbidity and lethality. Trends Endocrinol. Metab. 2020;31(12):918–927. doi: 10.1016/j.tem.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Maddaloni E, Cavallari I, Napoli N, Conte C. Vitamin D and diabetes mellitus. Front Horm. Res. 2018;50:161–176. doi: 10.1159/000486083. [DOI] [PubMed] [Google Scholar]
- 49.Tecilazich F, Formenti AM, Giustina A. Role of vitamin D in diabetic retinopathy: pathophysiological and clinical aspects. Rev. Endocr. Metab. Disord. 2021;22(4):715–727. doi: 10.1007/s11154-020-09575-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Conte C, Esposito A, De Lorenzo R, et al. Epicardial adipose tissue characteristics, obesity and clinical outcomes in COVID-19: a post-hoc analysis of a prospective cohort study. Nutr. Metab. Cardiovasc Dis. 2021;31(7):2156–2164. doi: 10.1016/j.numecd.2021.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Di Filippo L, De Lorenzo R, Giustina A, Rovere-Querini P, Conte C. Vitamin D in osteosarcopenic obesity. Nutrients. 2022;14(9):1816. doi: 10.3390/nu14091816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Giustina A. Hypovitaminosis D and the endocrine phenotype of COVID-19. Endocrine. 2021;72(1):1–11. doi: 10.1007/s12020-021-02671-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hutchings N, Babalyan V, Baghdasaryan S, et al. Patients hospitalized with COVID-19 have low levels of 25-hydroxyvitamin D. Endocrine. 2021;71(2):267–269. doi: 10.1007/s12020-020-02597-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.di Filippo L, Allora A, Doga M, et al. Vitamin D levels are associated with blood glucose and BMI in COVID-19 patients, predicting disease severity. J. Clin. Endocrinol. Metab. 2022;107(1):e348–e360. doi: 10.1210/clinem/dgab599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ulivieri FM, Banfi G, Camozzi V, et al. Vitamin D in the Covid-19 era: a review with recommendations from a G.I.O.S.E.G. expert panel. Endocrine. 2021;72(3):597–603. doi: 10.1007/s12020-021-02749-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bilezikian JP, Formenti AM, Adler RA, et al. Vitamin D: dosing, levels, form, and route of administration: does one approach fit all? Rev. Endocr. Metab. Disord. 2021;22(4):1201–1218. doi: 10.1007/s11154-021-09693-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.K. Shah, V.P. Varna, U. Sharma, D. Mavalankar, Does vitamin D supplementation reduce COVID-19 severity? - a systematic review [published online ahead of print, 2022 Feb 15]. QJM. 2022;hcac040. 10.1093/qjmed/hcac040 [DOI] [PMC free article] [PubMed]
- 58.S.R. Varikasuvu, B. Thangappazham, A. Vykunta, et al. COVID-19 and vitamin D (Co-VIVID study): a systematic review and meta-analysis of randomized controlled trials [published online ahead of print, 2022 Feb 3]. Expert Rev Anti Infect Ther. 2022;1–7. 10.1080/14787210.2022.2035217 [DOI] [PMC free article] [PubMed]
- 59.Tentolouris N, Samakidou G, Eleftheriadou I, Tentolouris A, Jude EB. The effect of vitamin D supplementation on mortality and intensive care unit admission of COVID-19 patients. A systematic review, meta-analysis and meta-regression. Diabetes Metab. Res Rev. 2022;38(4):e3517. doi: 10.1002/dmrr.3517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pal R, Banerjee M, Bhadada SK, Shetty AJ, Singh B, Vyas A. Vitamin D supplementation and clinical outcomes in COVID-19: a systematic review and meta-analysis. J. Endocrinol. Invest. 2022;45(1):53–68. doi: 10.1007/s40618-021-01614-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nalbandian A, Sehgal K, Gupta A, et al. Post-acute COVID-19 syndrome. Nat. Med. 2021;27(4):601–615. doi: 10.1038/s41591-021-01283-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Di Filippo L, De Lorenzo R, Cinel E, et al. Weight trajectories and abdominal adiposity in COVID-19 survivors with overweight/obesity. Int J. Obes. (Lond.) 2021;45(9):1986–1994. doi: 10.1038/s41366-021-00861-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Heaton LE, Davis JK, Rawson ES, et al. Selected in-season nutritional strategies to enhance recovery for team sport athletes: a practical overview. Sports Med. 2017;47(11):2201–2218. doi: 10.1007/s40279-017-0759-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Barker T, Schneider ED, Dixon BM, Henriksen VT, Weaver LK. Supplemental vitamin D enhances the recovery in peak isometric force shortly after intense exercise. Nutr. Metab. (Lond) 2013;10(1):69. doi: 10.1186/1743-7075-10-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.El-Hajj Fuleihan G, Nabulsi M, Tamim H, et al. Effect of vitamin D replacement on musculoskeletal parameters in school children: a randomized controlled trial. J. Clin. Endocrinol. Metab. 2006;91(2):405–412. doi: 10.1210/jc.2005-1436. [DOI] [PubMed] [Google Scholar]
- 66.Haugen J, Basnet S, Hardang IM, et al. Vitamin D status is associated with treatment failure and duration of illness in Nepalese children with severe pneumonia. Pediatr. Res. 2017;82(6):986–993. doi: 10.1038/pr.2017.71. [DOI] [PubMed] [Google Scholar]
- 67.Caballero-García A, Pérez-Valdecantos D, Guallar P, et al. Effect of vitamin D supplementation on muscle status in old patients recovering from COVID-19 infection. Med. (Kaunas) 2021;57(10):1079. doi: 10.3390/medicina57101079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Townsend L, Dyer AH, McCluskey P, et al. Investigating the relationship between vitamin D and persistent symptoms following SARS-CoV-2 infection. Nutrients. 2021;13(7):2430. doi: 10.3390/nu13072430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mohamed Hussein AAR, Galal I, Amin MT, et al. Prevalence of vitamin D deficiency among patients attending Post COVID-19 follow-up clinic: a cross-sectional study. Eur. Rev. Med Pharm. Sci. 2022;26(8):3038–3045. doi: 10.26355/eurrev_202204_28635. [DOI] [PubMed] [Google Scholar]
- 70.Barrea L, Grant WB, Frias-Toral E, et al. Dietary recommendations for post-COVID-19 syndrome. Nutrients. 2022;14(6):1305. doi: 10.3390/nu14061305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.di Filippo L, Castellino L, Giustina A. Occurrence and response to treatment of Graves’ disease after COVID vaccination in two male patients. Endocrine. 2022;75(1):19–21. doi: 10.1007/s12020-021-02919-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Piec I, Cook L, Dervisevic S, et al. Age and vitamin D affect the magnitude of the antibody response to the first dose of the SARS-CoV-2 BNT162b2 vaccine [published online ahead of print, 2022 Mar 16] Curr. Res. Transl. Med. 2022;70(3):103344. doi: 10.1016/j.retram.2022.103344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chillon TS, Demircan K, Heller RA, et al. Relationship between vitamin D status and antibody response to COVID-19 mRNA vaccination in healthy adults. Biomedicines. 2021;9(11):1714. doi: 10.3390/biomedicines9111714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lee MD, Lin CH, Lei WT, et al. Does vitamin D deficiency affect the immunogenic responses to influenza vaccination? a systematic review and meta-analysis. Nutrients. 2018;10(4):409. doi: 10.3390/nu10040409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lalor MK, Floyd S, Gorak-Stolinska P, et al. BCG vaccination: a role for vitamin D? PLoS One. 2011;6(1):e16709. doi: 10.1371/journal.pone.0016709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zitt E, Sprenger-Mähr H, Knoll F, Neyer U, Lhotta K. Vitamin D deficiency is associated with poor response to active hepatitis B immunisation in patients with chronic kidney disease. Vaccine. 2012;30(5):931–935. doi: 10.1016/j.vaccine.2011.11.086. [DOI] [PubMed] [Google Scholar]
- 77.Giustina A, Bouillon R, Binkley N, et al. Controversies in vitamin D: a statement from the Third International Conference. JBMR. 2020;4(12):e10417. doi: 10.1002/jbm4.10417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bonnet JB, Berchoux E, Sultan A. Decompensated primary hypoparathyroidism in a patient with COVID-19. Ann. Endocrinol. 2021;82(2):123–124. doi: 10.1016/j.ando.2021.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hernández JL, Nan D, Fernandez-Ayala M, et al. Vitamin D status in hospitalized patients with SARS-CoV-2 infection. J. Clin. Endocrinol. Metab. 2021;106(3):e1343–e1353. doi: 10.1210/clinem/dgaa733. [DOI] [PubMed] [Google Scholar]
- 80.Mazziotti G, Lavezzi E, Brunetti A, et al. Vitamin D deficiency, secondary hyperparathyroidism and respiratory insufficiency in hospitalized patients with COVID-19. J. Endocrinol. Invest. 2021;44(10):2285–2293. doi: 10.1007/s40618-021-01535-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kelly A, Levine MA. Hypocalcemia in the critically ill patient. J. Intensive Care Med. 2013;28(3):166–177. doi: 10.1177/0885066611411543. [DOI] [PubMed] [Google Scholar]
- 82.Krapf R, Jaeger P, Hulter HN. Chronic respiratory alkalosis induces renal PTH-resistance, hyperphosphatemia and hypocalcemia in humans. Kidney Int. 1992;42(3):727–734. doi: 10.1038/ki.1992.340. [DOI] [PubMed] [Google Scholar]
- 83.Ding Y, He L, Zhang Q, et al. Organ distribution of severe acute respiratory syndrome (SARS) associated coronavirus (SARS-CoV) in SARS patients: implications for pathogenesis and virus transmission pathways. J. Pathol. 2004;203(2):622–630. doi: 10.1002/path.1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.He L, Ding Y, Zhang Q, et al. Expression of elevated levels of pro-inflammatory cytokines in SARS-CoV-infected ACE2+ cells in SARS patients: relation to the acute lung injury and pathogenesis of SARS. J. Pathol. 2006;210(3):288–297. doi: 10.1002/path.2067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Elkattawy S, Alyacoub R, Ayad S, Pandya M, Eckman A. A novel case of hypoparathyroidism secondary to SARS-CoV-2 infection. Cureus. 2020;12(8):e10097. doi: 10.7759/cureus.10097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Dianatfar M, Sanjari M, Dalfardi B. Hypoparathyroidism After COVID-19 pneumonia. Magnesium. 2021;33(30-100):7. [Google Scholar]
- 87.Georgakopoulou VE, Avramopoulos P, Papalexis P, et al. COVID-19 induced hypoparathyroidism: a case report. Exp. Ther. Med. 2022;23(5):346. doi: 10.3892/etm.2022.11276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Trapani V, Rosanoff A, Baniasadi S, et al. The relevance of magnesium homeostasis in COVID-19. Eur. J. Nutr. 2022;61(2):625–636. doi: 10.1007/s00394-021-02704-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Sharma R, Heidari A, Johnson RH, Advani S, Petersen G. Serum magnesium levels in hospitalized patients with SARS-CoV-2. J. Investig. Med. 2022;70(2):409–414. doi: 10.1136/jim-2021-001948. [DOI] [PubMed] [Google Scholar]
- 90.Vetter T, Lohse MJ. Magnesium and the parathyroid. Curr. Opin. Nephrol. Hypertens. 2002;11(4):403–410. doi: 10.1097/00041552-200207000-00006. [DOI] [PubMed] [Google Scholar]
- 91.di Filippo L, Formenti AM, Doga M, Pedone E, Rovere-Querini P, Giustina A. Radiological thoracic vertebral fractures are highly prevalent in COVID-19 and predict disease outcomes. J. Clin. Endocrinol. Metab. 2021;106(2):e602–e614. doi: 10.1210/clinem/dgaa738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Jalava T, Sarna S, Pylkkänen L, et al. Association between vertebral fracture and increased mortality in osteoporotic patients. J. Bone Min. Res. 2003;18(7):1254–1260. doi: 10.1359/jbmr.2003.18.7.1254. [DOI] [PubMed] [Google Scholar]
- 93.Battisti S, Napoli N, Pedone C, et al. Vertebral fractures and mortality risk in hospitalised patients during the COVID-19 pandemic emergency. Endocrine. 2021;74(3):461–469. doi: 10.1007/s12020-021-02872-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kottlors J, Große Hokamp N, Fervers P, et al. Early extrapulmonary prognostic features in chest computed tomography in COVID-19 pneumonia: Bone mineral density is a relevant predictor for the clinical outcome - a multicenter feasibility study. Bone. 2021;144:115790. doi: 10.1016/j.bone.2020.115790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Tahtabasi M, Kilicaslan N, Akin Y, et al. The prognostic value of vertebral bone density on chest CT in hospitalized COVID-19 patients. J. Clin. Densitom. 2021;24(4):506–515. doi: 10.1016/j.jocd.2021.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Napoli N, Elderkin AL, Kiel DP, Khosla S. Managing fragility fractures during the COVID-19 pandemic. Nat. Rev. Endocrinol. 2020;16(9):467–468. doi: 10.1038/s41574-020-0379-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Emkey GR, Epstein S. Secondary osteoporosis: pathophysiology & diagnosis. Best. Pr. Res Clin. Endocrinol. Metab. 2014;28(6):911–935. doi: 10.1016/j.beem.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 98.Mazziotti G, Baracca M, Doga M, Porcelli T, Vescovi PP, Giustina A. Prevalence of thoracic vertebral fractures in hospitalized elderly patients with heart failure. Eur. J. Endocrinol. 2012;167(6):865–872. doi: 10.1530/EJE-12-0566. [DOI] [PubMed] [Google Scholar]
- 99.S. Boussaid, Y. Makhlouf, S. Jammali, H. Sahli, M. Elleuch, S. Rekik, Association of SARS-COV2 and lumbar spine fractures: causal or coincidental? [published online ahead of print, 2021 Nov 26]. J Clin Densitom. 2021;S1094–6950(21)00095-0. 10.1016/j.jocd.2021.11.006 [DOI] [PMC free article] [PubMed]
- 100.Mazziotti G, Bilezikian J, Canalis E, Cocchi D, Giustina A. New understanding and treatments for osteoporosis. Endocrine. 2012;41(1):58–69. doi: 10.1007/s12020-011-9570-2. [DOI] [PubMed] [Google Scholar]
- 101.Kim B, Kim J, Jo YH, et al. Risk of pneumonia after vertebral compression fracture in women with low bone density: a population-based study. Spine (Philos. Pa 1976) 2018;43(14):E830–E835. doi: 10.1097/BRS.0000000000002536. [DOI] [PubMed] [Google Scholar]
- 102.Watanabe R, Shiraki M, Saito M, Okazaki R, Inoue D. Restrictive pulmonary dysfunction is associated with vertebral fractures and bone loss in elderly postmenopausal women. Osteoporos. Int. 2018;29(3):625–633. doi: 10.1007/s00198-017-4337-0. [DOI] [PubMed] [Google Scholar]
- 103.Krege JH, Kendler D, Krohn K, et al. Relationship between vertebral fracture burden, height loss, and pulmonary function in postmenopausal women with osteoporosis. J. Clin. Densitom. 2015;18(4):506–511. doi: 10.1016/j.jocd.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 104.L. di Filippo, N. Compagnone, S. Frara, et al. Vertebral fractures at hospitalization predict impaired respiratory function during follow-up of COVID-19 survivors [published online ahead of print, 2022 Jun 8]. Endocrine. 2022. 10.1007/s12020-022-03096-7 [DOI] [PubMed]
- 105.Formenti AM, Pedone E, di Filippo L, Ulivieri FM, Giustina A. Are women with osteoporosis treated with denosumab at risk of severe COVID-19. Endocrine. 2020;70(2):203–205. doi: 10.1007/s12020-020-02500-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Blanch-Rubió J, Soldevila-Domenech N, Tío L, et al. Influence of anti-osteoporosis treatments on the incidence of COVID-19 in patients with non-inflammatory rheumatic conditions. Aging (Albany NY) 2020;12(20):19923–19937. doi: 10.18632/aging.104117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Atmaca A, Demirci I, Haymana C, et al. No association of anti-osteoporosis drugs with COVID-19-related outcomes in women: a nationwide cohort study. Osteoporos. Int. 2022;33(1):273–282. doi: 10.1007/s00198-021-06067-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Tsourdi E, Yu EW, Jan de Beur SM, Drake MT. Vaccination for Coronavirus Disease 2019 (COVID-19) and relationship to osteoporosis care: current evidence and suggested approaches. J. Bone Min. Res. 2021;36(6):1042–1047. doi: 10.1002/jbmr.4304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Giustina A, Marazuela M, Reincke M, Yildiz BO, Puig-Domingo M. One year of the pandemic - how European endocrinologists responded to the crisis: a statement from the European Society of Endocrinology. Eur. J. Endocrinol. 2021;185(2):C1–C7. doi: 10.1530/EJE-21-0397. [DOI] [PMC free article] [PubMed] [Google Scholar]