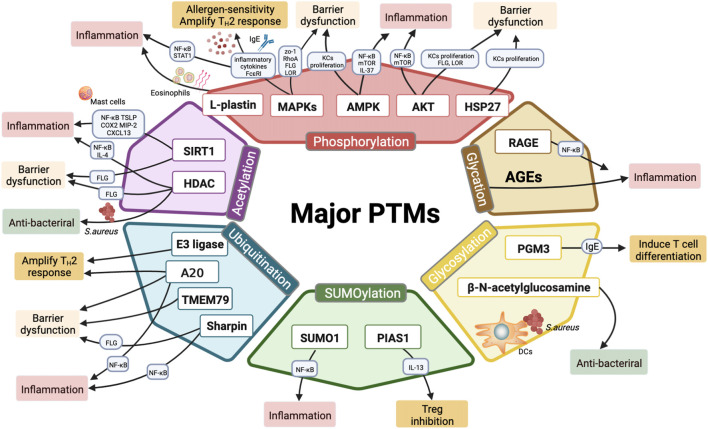
FIGURE 2.
Major PTMs involved in the pathogenesis of AD. Six major classes of PTMs involved in AD include phosphorylation, acetylation, ubiquitination, SUMOylation, glycosylation, o-glycosylation, and glycation. Phosphorylation of PTM-related enzymes (MAPKs, AKT and AMPK) and l-plastin may regulate epidermal inflammation and TH2 immune response by modulating inflammatory cytokine secretion (IL-9, IL-25, IL-31, IL-33, TSLP, and IL-37), promoting eosinophils migration, and activating AD-related pathways (such as NF-κB, JAK-STAT, mTOR signaling). Moreover, MAPK p38 phosphorylation upregulates FcεRI and results in allergen-induced hypersensitivity; besides, MAPK phosphorylation inhibits epidermal proteins (FLG, LOR) and tight junction proteins (RhoA, ZO-1), thereby disrupting the barrier functions. Meanwhile, both AKT phosphorylation and AMPK phosphorylation are involved in epidermal barrier function. Phosphorylation of AKT and HSP27 are required for KCs differentiation and epidermis formation. Histone deacetylases (SIRT1, HDAC) play paramount importance in regulating inflammation and maintaining skin barrier functions. Additionally, HDAC inhibitors exhibit antibacterial properties in AD treatment. Multiple E3 ubiquitin ligases are linked to dysregulated T-cell activation and excessive inflammatory infiltration. Ubiquitination editing enzyme A20 maintains skin barrier hemostatic and alleviates inflammation. Other ubiquitination-related proteins (TMEM79, Sharpin) act as mediators in inflammation responses and barrier repair as well. MiR-146 targets SUMO1 to regulate epidermal inflammation, whereas PIAS1 restricts the differentiation of Tregs by elevating IL-13. PGM3 reduces inflammation by inhibiting IgE production and T cell differentiation. β-N-acetylglucosamine modifications promote the identification and the interaction of LCs with S. aureus, thereby triggering bacterial skin infections. AGEs are formed by glycation process and exacerbating inflammatory responses via releasing proinflammatory factors; RAGE, the receptor of AGEs, stimulates skin inflammation via activating NF-κB phosphorylation.