Abstract
Background: Bleeding in Dacryocystorhinostomy (DRC) limits the surgeon’s sight and access. Tranexamic acid, Remifentanil, and Hydralazine reduce intraoperative blood loss. However, no study has been carried out to compare the efficacy of the latter drugs during DCR surgery. Methods: Ninety healthy candidates for DCR surgery with chronic Dacryocystitis (aging 20-80) were randomly assigned in groups of 30 to receive low doses of Tranexamic acid (TXA) (10 mg/kg with a maximum dose of 1000 mg), Remifentanil (0.1 µ/kg), or Hydralazine (0.1 mg/kg). All drugs were infused over 15 minutes before the initiation of surgery. The primary outcome was the bleeding volume during the surgery and until 2 hours in recovery. This study was approved by the Iranian Registry of Clinical Trials with the code of IRCT20210614051574N10 (https://en.irct.ir/trial/62759). Results: Thirty patients (mean age ± SD: 50.48±13.4) were investigated. Mean blood loss volume was lower in Remifentanil and Hydralazine groups compared with the TXA group (P<0.05); there was no significant difference (P>0.05) in bleeding volume between Remifentanil and Hydralazine groups (Tranexamic acid group: 146.83±91 ml, Remifentanil group: 77.6±52.1 ml, Hydralazine group: 80.0±48.7 ml, 95% confidence interval, P<0.05). Conclusion: Our results show that Remifentanil and Hydralazine are more effective than Tranexamic acid in bleeding control.
Keywords: Blood loss, dacryocystorhinostomy, hemorrhage, induced hypotension
Introduction
Dacryocystorhinostomy (DCR) surgery is a common ophthalmic surgery. The sources of bleeding during the DCR could be angular vein, soft tissue, periosteum, nutrient arteries of the bone, sac, or dissected nasal mucosa. Since the operating field is minimal, bleeding can reduce the surgeon’s sight and access [1,2]. Dacryocystorhinostomy (DCR) is a procedure for treating a blocked tear duct or nasolacrimal duct obstruction. Typically, a DCR procedure is performed if there is a complete or near-complete duct obstruction. During DCR, a new tear drain is created between the eye and nose to bypass the blocked tear drain [1]. The indications for DCR surgery are functional epiphoria secondary to Dacryolithiasis, chronic Dacryocystitis, persistent congenital nasolacrimal duct obstruction resistant to previous treatments, acquired nasolacrimal duct occlusion [3].
Limited information is available regarding the descriptions of intraoperative bleeding during the DCR surgery [4]. However, the standard procedures for control of bleeding include local injection of lidocaine/adrenaline, hypotensive anesthesia, head-up position, careful dissecting of soft tissues, cauterization, nasal packing with Epinephrine [5].
Tranexamic acid (TXA) is a medication used to control bleeding [6]. The antifibrinolytic effect of TXA takes place mainly by the reversible blockade of lysine binding sites on plasminogen molecules. TXA is associated with reductions in blood loss in upper gastrointestinal bleeding, menorrhagia and various surgeries. Patient compliance is good; nausea and diarrhea are the most common adverse events. The drug’s increased risk of thrombosis has not been demonstrated in clinical trials [7,8]. There are case reports of thrombosis associated with TXA; however, in one study, no thrombosis was reported with intraoperative use [9].
Induced hypotension (IH) during anesthesia has been used to reduce blood loss during surgery. A significant decrement in hemorrha=ge irrespective of the absolute blood pressure has been observed when the mean arterial pressure (MAP) is reduced to less than 20% of baseline Map [10]. However, it is a critical issue to investigate and compare the side effects of common drugs used for IH. Remifentanil and Hydralazine are two drugs used in (IH) [10]. Remifentanil is a new synthetic opioid with rapid onset and a short half-life, even in renal or hepatic failure patients. These characteristics make it a suitable drug for IH since no prolonging recovery happens when used in high doses, and the short half-life of the drug facilitates titration of dose to effect [11]. Metabolites have a weak activity that does not contribute to the effects of Remifentanil. The disadvantages could be (a) in case of accidental interruption of the infusion, rapid loss of analgesic and anesthetic effects happen, (b) infusion must be continuous, (c) lyophilized drug must be mixed with a diluent, and (d) there is complexity in determining the dose of another opioid needed for pain control after surgery. Although Remifentanil is likely to cost higher than other opioids, the shorter half-life of Remifentanil contributes to shorter recovery stays and lower overall costs [12,13].
Hydralazine with an action-onset of about 20 minutes is a direct vasodilator, acts mainly on arterioles or resistance vessels; hence less possibility of orthostatic hypotension is expected. Reflex tachycardia, nausea, dizziness, palpitation, and lupus-like syndrome in patients with slow hepatic acetylation have been reported [14,15].
To the best of our knowledge, no study has been carried out to compare the effect of TXA, Remifentanil, and Hydralazine on the controlling of perioperative blood loss during DCR surgery. Therefore, the present study aims to compare the effect of TXA, Hydralazine, and Remifentanil in bleeding control during DCR surgery.
Methods and material
Study design
This study is a double-blinded randomized clinical trial comparing the effect of TXA, Hydralazine and Remifentanil in patients undergoing DCR surgery, approved by the Ethics and Research Committee of Isfahan University of Medical Sciences (IR.MUI.MED.REC.1397.373, Iranian Registry of Clinical Trials (IRCT) code: IRCT20210614051574N10).
Inclusion and exclusion criteria
The inclusion criteria were age between 20 and 80 years, being a candidate for DCR surgery due to chronic dacryocystitis, having a score of I or II based on the American Society of Anesthesiologists (ASA) physical status classification, and signing the written informed consent to participate in this study. The exclusion criteria were uncontrolled systemic disease (ASA≥III), history of hematologic disease coagulation disorders, history of malignant hyperthermia, hypersensitivity to any of the drugs TXA or Remifentanil or Hydralazine, respiratory rate ≥24 in minutes, heart rate ≥100 bpm, MAP ≤70 mmHg, oxygen saturation ≤90% in room air, refusing to continue participating in the study and incidence of any complication during surgery leading to ICU admission or death.
Randomization
The enrolled patients were randomly allocated to three equal groups, receiving TXA, Hydralazine, and Remifentanil. Computer-generated block randomization (using Stratified Layered Blocking randomization for gender) was employed to randomize the patients in blocks of 30 with an equal proportion of male to female ratio.
Before the surgery, the goal of the experiment and the used drugs were explained to the patients. However, no information was given to the patients about the received medicine. In addition, neither patients nor surgeon knew about the study groups.
The other anesthesiologist who was not involved in the data analysis and recording administered the study drugs, and he was aware of the study groups in order to prevent any unwanted adverse effects of the drugs.
Study protocol
All surgeries were performed at the Feiz Hospital by a single surgeon and anesthesiologist with the same protocol. A detailed pre-anesthetic and pre-operative evaluation was carried out and recorded in all patients.
We prohibited patients from eating from 8 hours preoperatively. All three groups received the same general anesthesia induction method: intravenous administration of 0.03 mg Midazolam, 2 µg/kg Fentanyl, 5 mg/kg Sodium thiopental, and 0.5 mg/kg Atracurium. The anesthesia was maintained by Isoflurane 1.2% Mack with oxygen and N2O in equal proportions. Toprevent hypotension during anesthesia, all patients received 5 cc/kg Ringer lactate serum before induction of anesthesia. Patients did not need any blood transfusion during or after the surgery. To observe and prevent any bradycardia or hypotension, we continuously monitored the patient’s vital signs i.e., Heart rate, respiratory rate, systolic and diastolic blood pressure and mean arterial pressure and, oxygen saturation from the beginning of surgery until the end of recovery.
Interventions
Ten minutes before the starting of the operation, patients in the Remifentanil group received 0.1 µ/kg Remifentanil [16], patients in the Hydralazine group received a dose of 0.1 mg/kg Hydralazine [17], and in case the blood pressure increased more than 20% beyond the base the dose was repeated. Patients in the TXA group received 10 mg/kg TXA, with a maximum dose of 1000 mg; all study drugs were prescribed in 100 cc Dextrose water 5% serum over 15 minutes via intravenous infusion. In addition, the infusion dose of Hydralazine and Remifentanil was increased until the blood pressure was maintained in the 20% normal range.
Data assessments
The amount of bleeding was determined by measuring the blood collected in the suction bottle at the end of surgery and subtracting the volume of saline used for irrigation during the surgery. Maximum allowed blood loss was calculated using this formula:
(Hct * patient - Hct target) × weight × EBV **/Hctpatient
*Hct: Hematocrit; **EBV: Estimated blood volume.
In case of bleeding less than MABL (maximum allowed blood loss), the bleeding volume was replaced with a crystalloid (either Normal Saline or Ringer Lactate) to a triple amount; in bleedings more than MABL, the bleeding volume was replaced by half the amount with packed red blood cell.
In the case of mean arterial pressure (MAP) below 70 mmHg, the Trendelenburg maneuver was first used; secondly, the intravenous injection of Sodium chloride 0.9% was administered until a systolic blood pressure of above 70 mmHg was reached.
The end time of recovery was determined if the patient scored 9 or greater based on the modified Aldrete scoring system (Table 1).
Table 1.
Modified Aldrete scoring system
| Variable evaluated | Scoring |
|---|---|
| Activity | |
| Able to move four extremities on command | 2 |
| Able to move two extremities on command | 1 |
| Able to move no extremities on command | 0 |
| Breathing | |
| Able to breathe deeply and cough freely | 2 |
| Dyspnea | 1 |
| Apnea | 0 |
| Circulation | |
| Systemic blood pressure ±20% of the pre-anesthetic level | 2 |
| Systemic blood pressure ±20% to 49% of the pre-anesthetic level | 1 |
| Systemic blood pressure ±50% of the pre-anesthetic level | 0 |
| Consciousness | |
| Fully awake | 2 |
| Arousal | 1 |
| Not responding | 0 |
| Oxygen saturation | |
| ≤92% While breathing room air | 2 |
| Needs supplemental oxygen to maintain saturation ≥90% | 1 |
| ≤90% even with supplemental oxygen | 0 |
Data collection and variables
The parameters evaluated were age, gender, heart rate, respiratory rate, systolic, diastolic blood pressure, mean arterial pressure (from non-invasive blood pressure monitoring), and oxygen saturation (from pulse oximetry) at 15-minute intervals during surgery and until 2 hours during recovery. We also recorded the duration of anesthesia (defined as the interval from anesthesia induction until stopping the anesthesia medications), duration of surgery (defined as the interval from the first incision until completion of suturing), extubation time (defined as the interval from stopping the anesthesia medications until extubation), systolic blood pressure (SBP), diastolic blood pressure (DBP), MAP and SPO2. At the end of the surgery, we measured the surgeon’s satisfaction using a sequential qualitative scale (with grading: very good, good, moderate, weak, and very weak).
We measured the bleeding volume by deducting the saline volume used for irrigating from the total volume of fluid collected in the suction bottle 2 hours after surgery. Gender, age, and the study drug group were considered independent parameters.
Data analysis
Data were analyzed using SPSS version 20.0 (Chicago, Illinois, USA). The effects of using the study drugs on bleeding and hemodynamic parameters were investigated using one-way ANOVA, followed by the Tukey’s HSD post hoc and t-test. To understand the correlation between all the parameters, Pearson correlation was used. Quantitative variables were stated as mean ± SD (standard deviation). A P value of less than .05 is supposed to be significant.
Results
Study population
Ninety patients (mean age ± SD: 50.48±13.4) with chronic Dacryocystitis were randomly assigned to three groups receiving TXA, Remifentanil, and Hydralazine. All groups had 30 patients, including 15 men and 15 women. The mean values are shown in Table 2. Regarding the Tukey test, all the parameters except bleeding volume had no significant difference in all three groups (P>0.05); hence, all patient groups were operated in a similar condition Table 2.
Table 2.
Mean values, standard deviation and range of parameters
| Group | Mean ± Std | Range | P value | |
|---|---|---|---|---|
| Age, y | Ra | 46.2±13.4 | 20-84 | .074 |
| Ha | 53.9±13.5 | 31-81 | ||
| Ta | 51.3±13.3 | 26-69 | ||
| Gender | Ra | 50%M/F | - | .56 |
| Ha | 50%M/F | - | ||
| Ta | 50%M/F | - | ||
| Duration of recovery, min | Ra | 97.0±20.8 | 60-120 | 1.00 |
| Ha | 94.3±9.2 | 80-120 | ||
| Ta | 69.8±13.0 | 60-120 | ||
| Duration of surgery, min | Ra | 70.5±15.1 | 35-120 | .14 |
| Ha | 64.1±18.7 | 20-120 | ||
| Ta | 72.4±15.7 | 45-90 | ||
| Duration of anesthesia, min | Ra | 85.1±15.2 | 50-120 | .30 |
| Ha | 82.6±17.6 | 55-120 | ||
| Ta | 89.3±18.8 | 60-125 | ||
| Extubation time, min | Ra | 10.1±3.1 | 5-15 | .77 |
| Ha | 10.6±3.1 | 5-15 | ||
| Ta | 10.5±2.0 | 5-15 | ||
| Blood loss volume, ml | Ra | 77.6±52.1 | 10-200 | ≤.05¥ |
| Ha | 80.0±48.7 | 10-200 | ||
| Ta | 146.83±91 | 0-450 | ||
| Surgeon satisfaction | Ra | 4.2±0.5 | 3-5 | .470 |
| Ha | 4.3±.4 | 4-5 | ||
| Ta | 4.1±.6 | 3-5 | ||
| Mean SBP during surgery, mmHg | Ra | 107.23±8.34 | 95.80-123.40 | 0.058 |
| Ha | 112.08±7.79 | 93.83-129.50 | ||
| Ta | 111.94±8.06 | 97.50-128.67 | ||
| Mean DBP during surgery, mmHg | Ra | 71.71±10.16 | 61.60-104.40 | 0.67 |
| Ha | 73.68±8.65 | 61.50-99.25 | ||
| Ta | 72.37±8.03 | 58.14-85.20 | ||
| Mean MAP during surgery, mmHg | Ra | 83.55±9.26 | 73.93-110.73 | 0.35 |
| Ha | 86.48±7.65 | 76.67-105.08 | ||
| Ta | 85.49±7.64 | 72.17-99.00 | ||
| Mean HR during surgery, mmHg | Ra | 77.35±6.24 | 67.17-91.25 | 0.32 |
| Ha | 80.10±8.02 | 69.57-95.00 | ||
| Ta | 78.45±7.89 | 69.17-95.50 | ||
| Mean SPO2 during surgery | Ra | 98.25±1.18 | 95.40-100.00 | 0.54 |
| Ha | 97.21±1.21 | 94.67-98.71 | ||
| Ta | 98.59±1.36 | 94.57-100.00 | ||
| Mean SBP during recovery, mmHg | Ra | 1.16±13.85 | 93.20-134.40 | 0.90 |
| Ha | 1.16±10.80 | 95.20-134.20 | ||
| Ta | 1.15±13.14 | 91.20-136.60 | ||
| Mean DBP during recovery, mmHg | Ra | 77.15±11.23 | 60.0-99.80 | 0.27 |
| Ha | 73.29±7.94 | 59.80-91.60 | ||
| Ta | 76.06±9.65 | 61.20-100.20 | ||
| Mean MAP during recovery, mmHg | Ra | 90.10±11.85 | 71.87-111.33 | 0.64 |
| Ha | 87.73±7.69 | 72.40-105.80 | ||
| Ta | 89.12±10.46 | 71.87-112.27 | ||
| Mean HR during recovery, mmHg | Ra | 76.76±6.15 | 66.60-88.40 | 0.26 |
| Ha | 79.88±7.97 | 67.20-95.80 | ||
| Ta | 78.34±8.65 | 67.00-96.00 | ||
| Mean SPO2 during recovery | Ra | 97.56±1.74 | 93.40-100.00 | 0.68 |
| Ha | 97.87±1.74 | 90.00-99.00 | ||
| Ta | 97.80±2.20 | 91.40-100.00 |
abbreviation of group name.
The group blocks with different superscripts have significant difference (P value <.05).
SBP: systolic blood pressure, DBP: diastolic blood pressure, MAP: mean arterial pressure, HR: heart rate, SPO2: saturation of peripheral capillary oxygen by pulse oximetry.
Study variables
Mean blood loss volume in Remifentanil, Hydralazine, and TXA group were 77.6±52.1, 80.0±48.7, and 146.83±91, respectively. Mean blood loss volume was lower in Remifentanil and Hydralazine groups compared with the TXA group; there was no significant difference (P<0.05) between Remifentanil and Hydralazine groups. Blood loss was significantly more in women (119.44±82.04) than men (83.55±60.21) using a t-Test (P<0.05). In addition, there was no significant bleeding during the recovery period in all study groups (P<0.05). The monitored vital signs, considered outcomes of our interventions, are shown in Table 2. There is no significant relation between mean heart rate and an average MAP with blood loss during surgery or recovery (P<0.05).
Relationships
The relationship between other demographic parameters is investigated using the Pearson correlation test and shown in Table 3. Although there is a mild reduction in elder patients according to the SPO2 percentage during the surgery and recovery (P-value =0.010 and 0.019, respectively), mean values of this parameter are in an acceptable range, and no excessive drop in SPO2 percentage was observed. Mean SBP in recovery is significantly higher in older ages but still lies in the 20% normal range of blood pressure (P<0.05). There was no significant difference in the surgeon’s satisfaction between the groups (P<0.05).
Table 3.
Relevance of each parameter in respective of P value. Blocks with P value less than 0.05 are filled in blue color
| variable | Age, y | Gender | Bleeding volume, ml | Duration of surgery, min | Duration of recovery, min | Extubation time, min | Duration of Anesthesia, min | Mean SBP S, mmHg | Mean SBP R, mmHg | Mean DBP S, mmHg | Mean DBP R, mmHg | Mean MAP S, mmHg | Mean MAP R, mmHg | Mean HR S, bpm | Mean HR R, bpm | Mean SPO2%, S | Mean SPO2%, R |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age, y | - | .592 | .595 | .129 | .528 | .597 | .472 | .476 | +.041 | .524 | .339 | .459 | .145 | .085 | .533 | -.010 | -.019 |
| Gender | - | .024 | .244 | .505 | .477 | .059 | .869 | .582 | .421 | .596 | .507 | .569 | .291 | .794 | .116 | .236 | |
| Bleeding volume, ml | - | .241 | .092 | .872 | .256 | .741 | .639 | .753 | .173 | .734 | .285 | .950 | .879 | .315 | .823 |
Table abbreviations: y, year. ml, milliliter. bpm, beats per minute. min, minute. SBP, Mean systolic blood pressure. DBP, Mean diastolic blood pressure during recovery. S, during surgery. R, during recovery. MAP, mean arterial pressure. HR, heart rate. SPO2 saturation of peripheral capillary oxygen by pulse oximetry. P values less than .05 are shown in blue blocks and are considered significant. Minus sign (-) and positive sign (+) show negative and positive relations respectively.
There was no severe bleeding needing transfusion. There were no severe fluctuations in heart rate, oxygen saturation, or systolic and diastolic blood pressures needing drug administration.
There was no significant difference in all vital signs within the study groups (Figures 1, 2, 3, 4 and 5).
Figure 1.
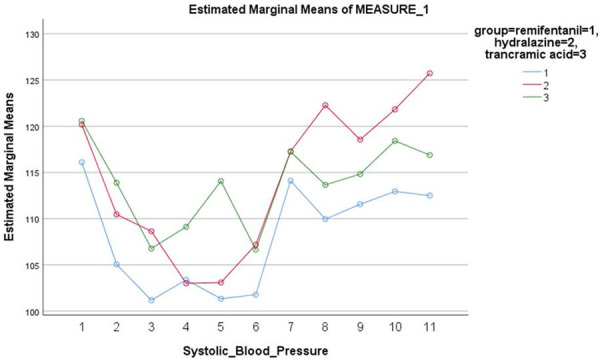
Systolic blood pressure between the three study groups. 1: before the surgery, 2: 15 min during surgery, 3: 30 min during surgery, 4: 45 min during surgery, 5: 60 min during surgery, 6: 75 min during surgery, 7: at the moment of recovery entry, 8: 15 min in recovery, 9: 30 min in recovery, 10: 45 min in recovery, 11: 60 min in recovery.
Figure 2.
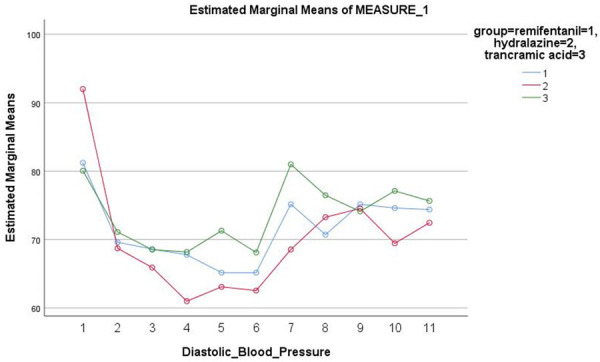
Diastolic blood pressure between the three study groups. 1: before the surgery, 2: 15 min during surgery, 3: 30 min during surgery, 4: 45 min during surgery, 5: 60 min during surgery, 6: 75 min during surgery, 7: at the moment of recovery entry, 8: 15 min in recovery, 9: 30 min in recovery, 10: 45 min in recovery, 11: 60 min in recovery.
Figure 3.
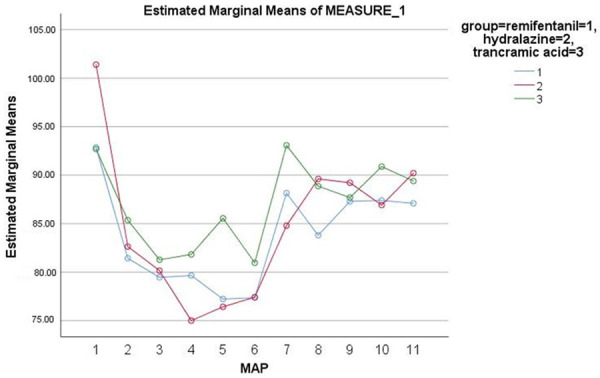
MAP between the three study groups. 1: before the surgery, 2: 15 min during surgery, 3: 30 min during surgery, 4: 45 min during surgery, 5: 60 min during surgery, 6: 75 min during surgery, 7: at the moment of recovery entry, 8: 15 min in recovery, 9: 30 min in recovery, 10: 45 min in recovery, 11: 60 min in recovery.
Figure 4.
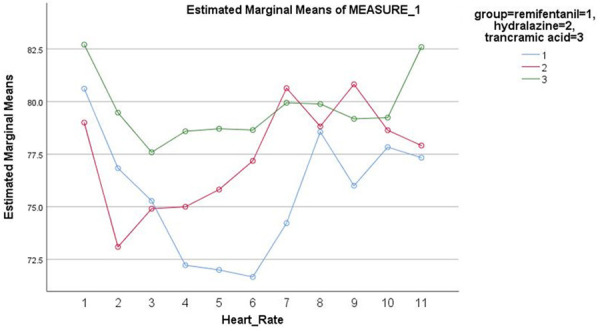
Heart rate between the three study groups. 1: before the surgery, 2: 15 min during surgery, 3: 30 min during surgery, 4: 45 min during surgery, 5: 60 min during surgery, 6: 75 min during surgery, 7: at the moment of recovery entry, 8: 15 min in recovery, 9: 30 min in recovery, 10: 45 min in recovery, 11: 60 min in recovery.
Figure 5.
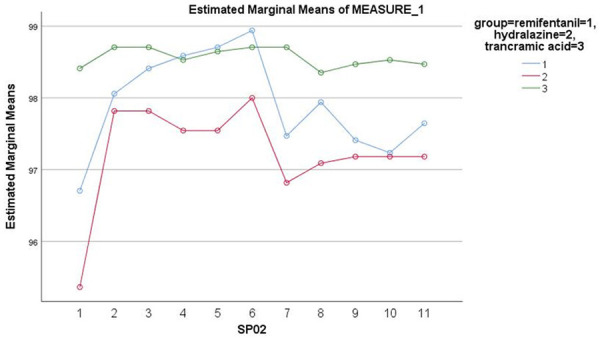
SPO2 between the three study groups. 1: before the surgery, 2: 15 min during surgery, 3: 30 min during surgery, 4: 45 min during surgery, 5: 60 min during surgery, 6: 75 min during surgery, 7: at the moment of recovery entry, 8: 15 min in recovery, 9: 30 min in recovery, 10: 45 min in recovery, 11: 60 min in recovery.
Discussion
This study shows that Remifentanil and Hydralazine were more effective than TXA for intra and postoperative blood loss reduction (mean blood loss is 77.6±52.1, 80.0±48.7, and 146.83±91, respectively). In a comparison between Remifentanil and Hydralazine groups.
There was no significant difference in SBP before the surgery and mean and standard deviation of SBP during the surgery between any of the three groups. This might be because of bleeding in DCR surgery does not frequently happen; therefore the use of hypotensive agents has not been frequent enough to have a significant effect on the mean values of hemodynamic parameters. Another study on Remifentanil also stated similar results [18].
Remifentanil and Hydralazine have been used as agents for induced hypotension for intraoperative bleeding control [19]. Induced hypotension can be considered a safe method provided that patient selection and appropriate monitoring are carried out [20]; however, cases of cerebral complications have been reported [21] and no significant difference in their efficacy was found in our study. Compared to Hydralazine, Remifentanil is easily titrated due to the short duration of action; hence, excessive hypotension could be avoided [22].
In a study by Koshika and colleagues in rabbits, Remifentanil reduced tissue blood perfusion in a dose-dependent manner [23]. Although several studies have successfully used Remifentanil for bleeding control in spinal and orthognathic surgeries, case reports of asystole and bradycardia after using Remifentanil over a 90 second bolus have been reported [24]. The mechanism is most likely due to Vague nerve stimulation in patients with weakened V node response due to beta adrenergic antagonists or calcium-channel blockers or a vagotonic procedure such as laryngoscopy. In our study, we used a low dose of 0.1 µ/kg Remifentanil infused carefully over 15 minutes before surgery and none of the complications were developed. Regarding a rabbit study by Koshika and colleagues [23], showing a dose-dependent effect of Remifentanil in bleeding control, further studies are required to assess whether there is a dose-dependent relation in humans. There was no significant difference in heart rate between the groups; hence, heart rate as a component of cardiac output is not related to bleeding control.
In this study, bleeding volume tends to increase in older ages; however, the relation only approached significance (P=0.595). More extensive studies are required to investigate whether there is a significant relation.
TXA, an anti-fibrinolytic, has been successfully used in surgeries with mass blood loss [25]. Low doses of TXA have been shown to have similar effects compared to massive amounts [26]; hence using low doses of TXA is safe and effective. With the exclusion of all patients with any medical disease, especially those with a high risk of developing thrombosis, no thromboembolic complications were found in this study, as stated similarly in another study [27]; thus, low dose TXA is possibly safe in healthy adults. High doses of TXA enhance neuronal excitation in a dose-dependent manner leading to convulsions and non-ischemic clinical seizures even in patients with no previous history of seizures. Based on a study by Ji and colleagues [28], we used a single dose of 10 mg/kg (maximum: 1000 mg) in 100 ml of Dextrose water 5% over 15 minutes before surgery and excluded all patients with a seizure history; no clinical seizure was encountered during hospital stays. Further studies are required to assess the long-term neurologic outcomes of TXA by electroencephalogram tests and to determine the safe lower limit of effective dosing.
Our age range of participants (ages 20 to 80) might limit the generalizability of this study; also, this study had quite broad exclusion criteria. Future studies are needed to investigate the effect of the latter drugs in other surgeries.
Conclusion
This study shows that Remifentanil and Hydralazine are more effective than TXA in bleeding control during DCR surgery. There is no significant difference between Remifentanil and Hydralazine.
Disclosure of conflict of interest
None.
Abbreviations
- ASA
American society of anesthesiologists
- DBP
diastolic blood pressure
- DCR
Dacryocystorhinostomy
- MAP
mean arterial pressure
- SBP
systolic blood pressure
- TXA:
Tranexamic Acid
References
- 1.Sobel RK, Aakalu VK, Wladis EJ, Bilyk JR, Yen MT, Mawn LA. A comparison of endonasal dacryocystorhinostomy and external dacryocystorhinostomy: a report by the American Academy of Ophthalmology. Ophthalmology. 2019;126:1580–1585. doi: 10.1016/j.ophtha.2019.06.009. [DOI] [PubMed] [Google Scholar]
- 2.Kang MG, Shim WS, Shin DK, Kim JY, Lee JE, Jung HJ. A systematic review of benefit of silicone intubation in endoscopic dacryocystorhinostomy. Clin Exp Otorhinolaryngol. 2018;11:81. doi: 10.21053/ceo.2018.00031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DeParis SW, Tian J, Rajaii F. Practice patterns in orbital decompression surgery among American Society of Ophthalmic Plastic and Reconstructive Surgery members. Ophthalmol Ther. 2019;8:541–8. doi: 10.1007/s40123-019-00206-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Do Hyun Kim SIK, Jin HJ, Kim S, Hwang SH. The clinical efficacy of silicone stents for endoscopic dacryocystorhinostomy: a meta-analysis. Clin Exp Otorhinolaryngol. 2018;11:151. doi: 10.21053/ceo.2017.01781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tooley AA, Klingler KN, Bartley GB, Garrity JA, Woog JJ, Hodge D, Bradley EA. Dacryocystorhinostomy for acquired nasolacrimal duct stenosis in the elderly (≥ 80 years of age) Ophthalmology. 2017;124:263–267. doi: 10.1016/j.ophtha.2016.10.018. [DOI] [PubMed] [Google Scholar]
- 6.Rohrich RJ, Cho MJ. The role of tranexamic acid in plastic surgery: review and technical considerations. Plast Reconstr Surg. 2018;141:507–515. doi: 10.1097/PRS.0000000000003926. [DOI] [PubMed] [Google Scholar]
- 7.Ramirez RJ, Spinella PC, Bochicchio GV. Tranexamic acid update in trauma. Crit Care Clin. 2017;33:85–99. doi: 10.1016/j.ccc.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 8.Myles PS, Smith JA, Forbes A, Silbert B, Jayarajah M, Painter T, Cooper DJ, Marasco S, McNeil J, Bussières JS. Tranexamic acid in patients undergoing coronary-artery surgery. N Engl J Med. 2017;376:136–148. doi: 10.1056/NEJMoa1606424. [DOI] [PubMed] [Google Scholar]
- 9.Goobie S. Tranexamic acid: still far to go. Br J Anaesth. 2017;118:293–295. doi: 10.1093/bja/aew470. [DOI] [PubMed] [Google Scholar]
- 10.Matsuura N, Okamura T, Ide S, Ichinohe T. Remifentanil reduces blood loss during orthognathic surgery. Anesth Prog. 2017;64:3–7. doi: 10.2344/anpr-63-03-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kisilewicz M, Rosenberg H, Vaillancourt C. Remifentanil for procedural sedation: a systematic review of the literature. Emerg Med J. 2017;34:294–301. doi: 10.1136/emermed-2016-206129. [DOI] [PubMed] [Google Scholar]
- 12.Chow JJ, Beckmann JS. Remifentanil-food choice follows predictions of relative subjective value. Drug Alcohol Depend. 2021;218:108369. doi: 10.1016/j.drugalcdep.2020.108369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zakhary W, Turton E, Flo Forner A, von Aspern K, Borger M, Ender J. A comparison of sufentanil vs. remifentanil in fast-track cardiac surgery patients. Anaesthesia. 2019;74:602–608. doi: 10.1111/anae.14572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eshghpour M, Samieirad S, Attar AS, Kermani H, Seddigh S. Propofol versus remifentanil: which one is more effective in reducing blood loss during orthognathic surgery? A randomized clinical trial. J Oral Maxillofac Surg. 2018;76:1882. doi: 10.1016/j.joms.2018.05.012. [DOI] [PubMed] [Google Scholar]
- 15.Antza C, Dimou C, Doundoulakis I, Akrivos E, Stabouli S, Haidich AB, Goulis DG, Kotsis V. The flipside of hydralazine in pregnancy: a systematic review and meta-analysis. Pregnancy Hypertens. 2020;19:177–186. doi: 10.1016/j.preghy.2020.01.011. [DOI] [PubMed] [Google Scholar]
- 16.Santonocito C, Noto A, Crimi C, Sanfilippo F. Remifentanil-induced postoperative hyperalgesia: current perspectives on mechanisms and therapeutic strategies. Local Reg Anesth. 2018;11:15. doi: 10.2147/LRA.S143618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Collins KS, Raviele AL, Elchynski AL, Woodcock AM, Zhao Y, Cooper-DeHoff RM, Eadon MT. Genotype-guided hydralazine therapy. Am J Nephrol. 2020;51:764–776. doi: 10.1159/000510433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hirata A, Kasahara M, Matsuura N, Ichinohe T. Remifentanil decreases oral tissue blood flow while maintaining internal carotid artery blood flow during sevoflurane anesthesia in rabbits. J Vet Med Sci. 2018;80:354–360. doi: 10.1292/jvms.17-0319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matsuura N, Okamura T, Ide S, Ichinohe T. Remifentanil reduces blood loss during orthognathic surgery. Anesth Prog. 2017;64:3–7. doi: 10.2344/anpr-63-03-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mei A, Qiu L. The efficacy of tranexamic acid for orthognathic surgery: a meta-analysis of randomized controlled trials. Int J Oral Maxillofac Surg. 2019;48:1323–1328. doi: 10.1016/j.ijom.2018.07.027. [DOI] [PubMed] [Google Scholar]
- 21.Chen Y, Ma L, Yang S, Burkhardt JK, Lu J, Ye X, Jiang W, Ren Z, Wang R, Chen X. Quantitative angiographic hemodynamic evaluation after revascularization surgery for moyamoya disease. Transl Stroke Res. 2020;11:871–881. doi: 10.1007/s12975-020-00781-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Santos DMD, Da Silva EAP, Oliveira JYS, Marinho YYM, Santana IR, Heimfarth L, Pereira EWM, Júnior LJQ, Assreuy J, Menezes IAC, Santos MRVD. The therapeutic value of hydralazine in reducing inflammatory response, oxidative stress, and mortality in animal sepsis: involvement of the PI3K/AKT pathway. Shock. 2021;56:782–792. doi: 10.1097/SHK.0000000000001746. [DOI] [PubMed] [Google Scholar]
- 23.Koshika K, Ichinohe T, Kaneko Y. Dose-dependent remifentanil decreases oral tissue blood flow during sevoflurane and propofol anesthesia in rabbits. J Oral Maxillofac Surg. 2011;69:2128–2134. doi: 10.1016/j.joms.2010.12.056. [DOI] [PubMed] [Google Scholar]
- 24.Aygun N, Sarıdemir D, Bas K, Tunca F, Arici C, Uludag M. Transient asystole related to carbon dioxide embolism during transoral endoscopic parathyroidectomy vestibular approach. Head Neck. 2021;43:E51–E55. doi: 10.1002/hed.26855. [DOI] [PubMed] [Google Scholar]
- 25.Peck J, Kepecs DM, Mei B, Safir OA, Backstein D, Gross AE, Kuzyk PR. The effect of preoperative administration of intravenous tranexamic acid during revision hip arthroplasty: a retrospective study. JBJS. 2018;100:1509–1516. doi: 10.2106/JBJS.17.01212. [DOI] [PubMed] [Google Scholar]
- 26.Sun H, Deng L, Deng J, Wang J, Zhang H, Chen K, Li H, Ning X, Yang H. The efficacy and safety of prophylactic intravenous tranexamic acid on perioperative blood loss in patients treated with posterior lumbar interbody fusion. World Neurosurg. 2019;125:e198–e204. doi: 10.1016/j.wneu.2019.01.040. [DOI] [PubMed] [Google Scholar]
- 27.Xie J, Lenke LG, Li T, Si Y, Zhao Z, Wang Y, Zhang Y, Xiao J. Preliminary investigation of high-dose tranexamic acid for controlling intraoperative blood loss in patients undergoing spine correction surgery. Spine J. 2015;15:647–654. doi: 10.1016/j.spinee.2014.11.023. [DOI] [PubMed] [Google Scholar]
- 28.Ji J, Lee H, Argiropoulos B, Dorrani N, Mann J, Martinez-Agosto JA, Gomez-Ospina N, Gallant N, Bernstein JA, Hudgins L. DYRK1A haploinsufficiency causes a new recognizable syndrome with microcephaly, intellectual disability, speech impairment, and distinct facies. Eur J Hum Genet. 2015;23:1473–1481. doi: 10.1038/ejhg.2015.71. [DOI] [PMC free article] [PubMed] [Google Scholar]


