Abstract
Purpose:
The purpose of the study was to investigate the incidence, cause and probability of re-hospitalization within 30 and 365 days after percutaneous coronary intervention (PCI) in patients with diabetes.
Method:
Between January 2010 and September 2014, 2763 patients with diabetes were treated with PCI at two Hospitals in Western Denmark. Reasons for readmission within 30 and 365 days were identified.
Results:
Readmission risks for patients with diabetes were 58% within 365 days and 18% within 30 days. Reason for readmission was ischemic heart disease (IHD) in 725 patients (27%), and non-IHD-related reasons in 826 patients (31%). IHD-related readmission within 365 days was associated with female gender (OR 1.3, 95% CI: 1.1–1.5), and non-ST-segment elevation myocardial infarction, compared to stable angina at the index hospitalization (OR 1.3, 95% CI: 1.1–1.6). Among patients with diabetes, increased risk of readmission due to other reasons were age (OR 1.3, 95% CI: 1.2–1.5) and higher scores of modified Charlson Comorbidity index (CCI): CCI ≥3 (OR 3.6, 95% CI: 2.8–4.6).
Conclusion:
More than half of the patients with diabetes mellitus undergoing PCI were readmitted within 1 year. Comorbidities were the strongest predictor for non-IHD-related readmission, but did not increase the risk for IHD-related readmissions.
Keywords: Coronary artery disease, percutaneous coronary intervention, diabetes mellitus, re-hospitalization
Introduction
Cardiovascular disease is often more progressive with diffuse and complex atherosclerosis in diabetic patients, resulting in poor clinical outcome. 1 The prevalence of ischemic heart disease (IHD) is high among patients with diabetes, and the diabetic population has both increased comorbidity and mortality compared to patients without diabetes.2,3 Symptomatic IHD is often treated with revascularization by either percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG), where less invasive revascularization with PCI often is preferred in diabetes patients with single vessel disease or non-complex multi-vessel disease. 4 Patients with diabetes undergoing PCI have an increased occurrence of long-term risk of death, myocardial infarctions (MI) and repeat revascularization compared to patients without diabetes. 5
Unplanned readmission followed by PCI is common, and up to 16% of patients undergoing PCI are readmitted within 30-days after the procedure.6–8 Cardiac events and symptoms are the most frequent reasons for readmission among patients undergoing PCI, and comorbidities are known to be predictors of all-cause rehospitalization.6,8
Among patients undergoing revascularization with PCI, up to forty percent have diabetes, and most often coexisting morbidities like chronic lung disease, peripheral artery disease, hypertension, and chronic kidney disease.7,9 Patients with diabetes are more likely to have complex multi-vessel cardiovascular disease compared to patients without diabetes,10,11 and previous work has indicated awareness for diabetic patients with comorbidities to be treated as high-risk groups, hoping to reduce the high readmission rate for diabetic patients with cardiovascular disease.12,13
The aim of this study was to assess the risk of readmission after PCI in patients with diabetes and to evaluate the associated characteristics for readmission related to IHD and all other readmission reasons.
Methods
Setting
The study was conducted using the Western Denmark’s healthcare database. The database covers about 55% of the Danish population. Detailed description of the database had been described in a previous study. 6 To assess all PCI procedures performed from 1 January 2010 to 30 September 2014, at Aarhus University Hospital and Odense University Hospital, the Western Denmark Heart Registry was used.
All Danish citizens are tracked in the healthcare system and national registries. The Danish Civil Registration System has since 1968 kept electronic records on gender, birthdate, residence, and emigration date, and characteristics of all non-psychiatric in-patient admissions since 1977 with daily update. The 10-digit civil registration number assigned at birth and used in all registries allows accurate record linkage. The Danish Civil Registration System provided vital status data for the study population and minimized loss to follow-up. The study was approved by The Danish Data Protection Agency (2012-41-0164).
Data analysis
The data analysis had previously been described. 6 All PCI procedures conducted during January 2010 and September 2014 were cross-referenced to the Danish Civil Registration System using the 10-digit civil registration number, and readmissions within 365 days after index PCI were thereby tracked. The reason for readmission was defined using ICD-10-coding, and only the primary diagnosis registered at discharge was determined to be the reason for readmission. Readmission within 2 days after index procedure was interpreted as transfer between hospitals or departments and was not included as readmission. Patients readmitted several times during the first year after the PCI procedure were only included in the dataset once, and only included with the first given diagnosis.
Comorbidity scores were computed using the Charlson Comorbidity Index (CCI), 14 which contains 19 major disease categories, e.g. diabetes, heart failure and cancer. The CCI estimates the risk of 1-year mortality by a weighted calculation based on the number and seriousness of the comorbidities. In this analysis, we used a modified CCI as diabetes was removed from the index, as the inclusion criteria were patients with diabetes. The indication for PCI was divided into: STEMI, NSTEMI, SAP and “other”, where “other” included: arrhythmia, valve disease, cardiomyopathy and chronic heart failure, evaluation of cardiac risk prior to non-cardiac surgery or cardiac arrest.
Statistical analysis
Contingency tables were created for the main study variables characterizing patients readmitted to hospital and not readmitted after PCI. The readmitted patients with diabetes were divided into patients readmitted due to IHD-related reasons and without diagnoses of IHD. The follow-up period was 365 days after PCI. Distribution of continuous variables for the two readmitted patient groups versus the non-readmitted group were statistically compared using t-tests. Distribution for categorical variables was compared using the χ2-test. For readmitted patients, the most frequent causes of readmission were identified. To estimate the probability of readmission within 365 days after index PCI, Kaplan-Meier curves were constructed and compared across indications for PCI (stable angina pectoris (SAP), ST-segment elevation MI (STEMI) and non-ST-segment elevation MI (NSTEMI), and other), comorbidities (using CCI 10 years prior to PCI), and gender with log-rank tests.
Analysis for potential risk factors for readmission after PCI (comorbidities, age and gender) were conducted using logistic regression. All data analyses were performed using SAS software, version 9.2 (SAS Institue Inc., Cary, NC, USA).
Results
Study population and patient characteristics
Between 1 January 2010 and 30 September 2014, 18,025 patients were treated with PCI. After exclusion due to missing readmission dates (n = 176), death during index hospitalization (n = 566), emigration (n = 14) and foreign citizenship (n = 158), 17,111 patients were left for analysis. Of these patients, 2673 diabetic patients represented the final cohort. Clinical characteristics at baseline are presented in Table 1. Patients with readmission due to IHD did not differ in patient characteristics, compared to patients who were not readmitted. Patients readmitted due to non-IHD-related reasons were older, more often smokers, had higher levels of creatinine and had longer index admissions. Patients with prior acute MI, PCI or previous heart surgery were more often readmitted due to reasons other than angina/MI. Patients with comorbidities were more often readmitted within 1 year, no matter the reason.
Table 1.
Baseline patient characteristics.
| All patients (2673) | IHD readmissions (725) | Other readmissions (826) | Not readmitted (1122) | p-value (IHD vs non-readm.) | p-value (other vs non-readm.) | |
|---|---|---|---|---|---|---|
| Male, no. (%) | 1897 (71.0) | 491 (67.7) | 579 (70.1) | 827 (73.7) | 0.0055 | 0.0788 |
| Age, mean (SD) | 67.2 (10.7) | 65.5 (11.0) | 69.8 (10.6) | 66.3 (10.1) | 0.0875 | <0.0001 |
| Family history, n (%) | 1165 (43.6) | 301 (41.5) | 350 (42.4) | 514 (45.8) | 0.1927 | 0.0052 |
| Smoker, n (%) | 657 (24.6) | 171 (23.6) | 195 (23.6) | 291 (5.9) | 0.4138 | 0.039 |
| BMI, mean (SD) | 29.2 (5.8) | 29.3 (5.8) | 28.8 (5.9) | 29.4 (5.7) | 0.7994 | 0.0605 |
| Hypertension, n (%) | 2105 (78.8) | 563 (77.7) | 667 (80.8) | 875 (78.0) | 0.7526 | 0.3083 |
| Lipid treatment, n (%) | 2143 (80.2) | 561 (77.4) | 678 (82.1) | 904 (80.6) | 0.2461 | 0.5998 |
| Creatinine, mean (SD) | 100.5 (76.2) | 93.8 (67.5) | 120.4 (100.3) | 90.3 (55.6) | 0.2816 | <0.0001 |
| Systolic blood pressure, mmHg, mean (SD) | 137.7 (23.7) | 137.2 (22.7) | 135.7 (24.8) | 139.6 (23.3) | 0.037 | 0.0007 |
| Diastolic blood pressure, mmHg, mean (SD) | 74.0 (13.4) | 74.1 (13.3) | 72.4 (13.8) | 75.2 (13.0) | 0.0941 | <0.0001 |
| Year of intervention | 0.0512 | 0.0305 | ||||
| 2010 | 533 (19.9) | 159 (21.9) | 177 (21.4) | 197 (17.6) | ||
| 2011 | 642 (24.0) | 186 (25.7) | 173 (20.9) | 283 (25.2) | ||
| 2012 | 568 (21.2) | 155 (21.4) | 177 (21.4) | 236 (21.0) | ||
| 2013 | 570 (21.3) | 142 (19.6) | 193 (23.4) | 235 (20.9) | ||
| 2014 | 360 (13.5) | 83 (11.4) | 106 (12.8) | 171 (15.2) | ||
| Prior AMI | 624 (23.3) | 163 (22.5) | 214 (25.9) | 247 (22.0) | 0.3915 | 0.0275 |
| Prior PCI | 688 (25.7) | 196 (27.0) | 209 (25.3) | 283 (25.2) | 0.6863 | 0.2689 |
| Prior heart surgery | 362 (13.5) | 101 (13.9) | 130 (15.7) | 131 (11.7) | 0.1532 | 0.0093 |
| No. diseased vessels | 0.0003 | 0.0663 | ||||
| 0 vessel | 5 (0.2) | 0 (0) | 3 (0.4) | 2 (0.2) | ||
| 1 vessel | 1011 (37.8) | 245 (33.8) | 304 (36.8) | 462 (41.2) | ||
| 2 vessels | 554 (20.7) | 175 (24.1) | 151 (18.3) | 228 (20.3) | ||
| 3 vessels | 378 (14.1) | 126 (17.4) | 123 (14.9) | 129 (11.5) | ||
| Diffuse disease | 8 (0.3) | 1 (0.1) | 2 (0.2) | 5 (0.4) | ||
| Indication for PCI | 0.0008 | 0.0015 | ||||
| STEMI | 422 (15.8) | 127 (17.5) | 121 (14.6) | 174 (15.5) | ||
| NSTEMI | 824 (30.8) | 252 (34.8) | 251 (30.4) | 321 (28.6) | ||
| SAP | 1309 (49.0) | 334 (46.1) | 391 (47.3) | 584 (52.0) | ||
| Other | 118 (4.4) | 12 (1.7) | 63 (7.6) | 43 (3.8) | ||
| 10-year Charlson comorbidity index, n (%) | <0.0001 | <0.0001 | ||||
| 0 | 1064 (39.8) | 298 (41.1) | 212 (25.7) | 554 (49.4) | ||
| 1–2 | 1137 (42.5) | 303 (41.8) | 379 (45.9) | 455 (40.6) | ||
| ≥3 | 472 (17.7) | 124 (17.1) | 235 (28.5) | 113 (10.1) | ||
| Duration of index admission, n (%) | 0.0505 | <0.0001 | ||||
| 0–3 days | 2033 (76.1) | 570 (78.6) | 572 (69.2) | 891 (79.4) | ||
| 4–7 days | 389 (14.6) | 116 (16.0) | 127 (15.4) | 146 (13.0) | ||
| >7 days | 251 (9.4) | 39 (5.4) | 127 (15.4) | 85 (7.6) | ||
| Days from PCI to readmission, n (%) | <0.0001 | <0.0001 | ||||
| 0–30 days | 1599 (59.8) | 247 (34.1) | 230 (27.8) | 1122 (100.0) | ||
| 31–365 days | 1074 (40.2) | 478 (65.9) | 596 (72.2) | — | ||
| Death ≤365 after PCI, n | 166 | 35 | 108 | 23 |
Data presented as mean ± SD, or n (%). AMI: acute myocardial infarction. BMI: body mass index. CABG: coronary artery bypass graft surgery. IHD: Ischemic heart disease. NSTEMI: non-ST-segment elevation myocardial infarction. PCI: percutaneous coronary intervention. SAP: stable angina pectoris. STEMI: ST-segment elevation myocardial infarction.
Causes for readmission
Table 2 represents the reasons for readmission. After 365 days, 725 patients (27.1%) were readmitted due to IHD, and 826 patients (30.9%) were readmitted due to all other reasons. The 30-days readmission rate was 18.3%, 9.5% were readmitted due to IHD-related reasons, whereas 8.8% were readmitted due to reasons other than IHD. Within 365 days, 166 patients died. Of the patients readmitted due to non-IHD-related causes 108 died within 365 days.
Table 2.
Causes of the first readmission within 30 and 365 days after PCI.
| 30-days readmission | One year readmission | |||
|---|---|---|---|---|
| IHD-related readmissions (n = 253) | IHD-related readmissions (n = 725) | |||
| Diagnosis | N (%) | Diagnosis | N (%) | |
| 1 | Angina pectoris/chest pain | 206 (81.4) | Angina pectoris/chest pain | 612 (84.4) |
| 2 | Acute coronary syndrome | 47 (18.6) | Acute coronary syndrome | 113 (15.6) |
| Non-IHD-related readmissions (n = 235) | Non-IHD-related readmissions (n = 826) | |||
| 1 | Heart insufficiency | 20 (7.9) | Abdominal symptoms excl. GI bleeding | 60 (7.3) |
| 2 | Respiratory insufficiency | 17 (6.7) | Heart insufficiency | 60 (7.3) |
| 3 | Atrial fibrillation and atrial flutter | 15 (5.9) | Infection | 58 (7.0) |
| 4 | Pneumonia | 15 (5.9) | Respiratory insufficiency | 57 (6.9) |
| 5 | Anemia | 14 (5.5) | Endocrine conditions | 52 (6.3) |
| 6 | Endocrine conditions | 14 (5.5) | Peripheral vascular disease | 42 (5.1) |
| 7 | Bleeding incl. GI bleeding | 13 (5.1) | Atrial fibrillation and atrial flutter | 39 (4.7) |
| 8 | Arrhythmia | 12 (4.7) | Pneumonia | 39 (4.7) |
| 9 | Peripheral vascular disease | 11 (4.3) | Valve disease | 38 (4.6) |
| 10 | Procedure complications | 11 (4.3) | Bleeding incl. GI bleeding | 34 (4.1) |
| 11 | Abdominal symptoms excl. GI bleeding | 10 (4.0) | Suspicion of condition or disease | 32 (3,9) |
| 12 | Infection | 10 (4.0) | Neurological conditions excl. stroke/TIA | 30 (3.6) |
| 13 | Valve disease | 10 (4.0) | Arrhythmia | 29 (3.5) |
| 14 | Dermatological conditions | 9 (3.6) | Conditions in the musculoskeletal system | 29 (3.5) |
| 15 | Kidney insufficiency | 7 (2.8) | Anemia | 28 (3.4) |
| 16 | Conditions in the musculoskeletal system | 7 (2.8) | Kidney insufficiency | 24 (2.9) |
| 17 | Stroke/TIA | 6 (2.4) | Procedure complications | 24 (2.9) |
| 18 | Syncope | 6 (2.4) | Dermatological conditions | 21 (2.5) |
| 19 | Benign tumors | 3 (1.2) | Cancer | 20 (2.4) |
| 20 | Cancer | 3 (1.2) | Syncope | 20 (2.4) |
| 21 | Urological conditions | 3 (1.2) | Stroke/TIA | 18 (2.2) |
| 22 | Neurological conditions excl. stroke/TIA | 2 (0.8) | Benign tumors | 15 (1.8) |
| 23 | Fractures, contusions and lesions | 14 (1.7) | ||
| 24 | Urological conditions | 13 (1.6) | ||
| Others | 16 (6.3) | Others | 37 (4.5) | |
GI: gastrointestinal, IHD: ischemic heart disease, PCI: percutaneous coronary intervention, TIA: transient ischemic attack.
Of the 725 patients readmitted on suspicion of IHD within 365 days of the initial admission, 113 patients (16%) had acute coronary syndrome, and 612 (84%) were readmitted due to angina pectoris/chest pains. Almost 20% of the patients readmitted within the first 30 days were admitted due to ACS (acute coronary syndrome). Within 365 days, 31% of all patients with diabetes were readmitted due to causes other than IHD. The three most common reasons for non-IHD related readmission within the first year included: Heart failure (7%), abdominal symptoms (7%), and infection (7%). During 30-day readmission, the highest occurrences of non-IHD-related readmission were: Heart failure (8%), respiratory insufficiency (7%) and atrial fibrillation and atrial flutter (6%). Endocrine conditions presented 6% of all non-IHD-related readmission within 365 days and 6% after 30 days, and consisted mostly of complication to diabetes.
Risk of readmission
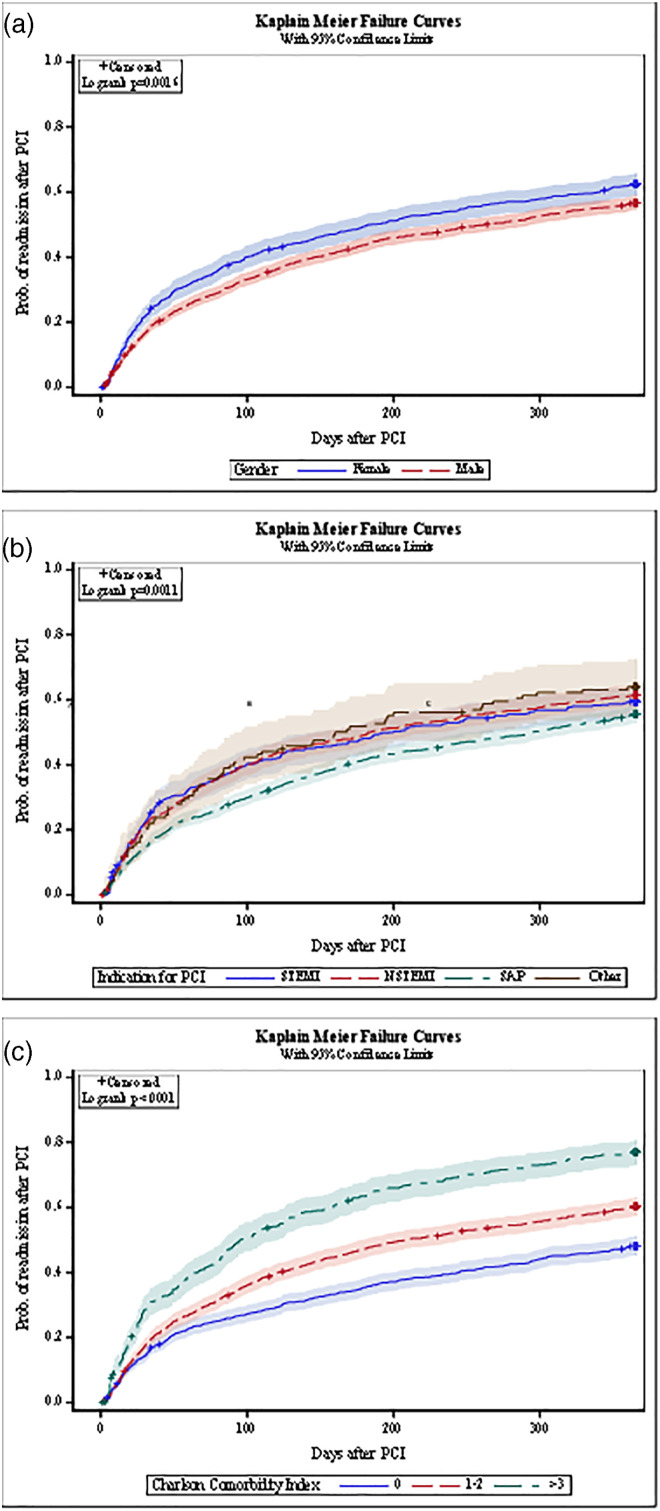
The probability of readmission represented by Kaplan Meier plots is shown in Figure 1. The predictors for diabetic patients readmitted due to angina/MI or other reasons are shown in Table 3. The probability of any readmission within 365 days increased significantly, if patients were female, had higher CCI, or if the initial PCI was performed on the indication “other”, followed by NSTEMI, STEMI and SAP. The modified 10-year CCI was the strongest predictor for non-IHD readmission, followed by indication for PCI and old age. Patients with CCI ≥3 had 3.6 fold higher odds of IHD-related readmission compared to diabetic patients with CCI 0 (OR 3.6, 95% CI 2.8–4.6), and patients with CCI 1-2 had a 1.8 fold higher odds of readmission due to non-IHD related reasons (OR 1.8, 95% CI 1.5–2.2). The modified CCI was not a predictor of readmission due to angina/MI. Patients with diabetes who presented with NSTEMI and STEMI had no increased probability of non-IHD readmission, compared to patients with SAP at index procedure, but "other" indication for PCI had a 2.5 fold higher odds of non-IHD related readmission within 365 days (OR 2.5, 95% CI 1.7–3.7, p < 0.0001). Age was linked to greater risk of non-IHD related readmission (OR 1.3, 95% CI 1.2–1.5, p < 0.0001). For diabetic patients, their risk of IHD-related readmission decreased with age (OR 0.8, 95% CI 0.7–0.9). Also, patients with “other” indication for PCI had a lower risk of IHD-related readmission, compared to SAP patients (OR 0.3, 95% CI 0.2–0.6) whereas patients presenting with NSTEMI had an increased risk of IHD-readmissions (OR 1.3, 95% CI 1.1–1.6). Women had a slightly higher risk of IHD-related readmission, compared to men (OR 1.3, 95% CI 1.1–1.5).
Figure 1.
Kaplan-Meier cumulative event curves with 95% confidence limits for probability of readmission after PCI within a year as per various factors. (a) Gender. (b) modified Charlson comorbidity index. (c) Indication for percutaneous coronary intervention.
Table 3.
Predictors for readmission within one year and 30-days.
| Predictors for readmission within 30 days | Predictors for readmission within 1 year | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Readmission related to IHD | Other readmission | Readmission related to IHD | Other readmission | ||||||
| Characteristic | Comparator | Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value |
| Gender | Female versus male | 1.675 (1.276; 2.199) | 0.0002 | 1.031 (0.764; 1.390) | 0.8428 | 1.274 (1.056; 1.537) | 0.0115 | 0.992 (0.822; 1.199) | 0.9369 |
| Age | Per 10-year increase | 0.847(0.752; 0.954) | 0.0062 | 1.210 (1.057; 1.385) | 0.0057 | 0.810 (0.747; 0.879) | <0.0001 | 1.332 (1.223; 1.450) | <0.0001 |
| CCI 10 | |||||||||
| 1–2 | 1–2 vs. 0 | 0.900 (0.668; 1.213) | 0.4890 | 2.025 (1.415; 2.900) | 0.0001 | 1.022 (0.843; 1.240) | 0.8219 | 1.819 (1.490; 2.222) | <0.0001 |
| ≥3 | ≥3 vs 0 | 1.215 (0.844; 1.749) | 0.2957 | 4.118 (2.802; 6.051) | <0.0001 | 1.016 (0.788; 1.308) | 0.9049 | 3.581 (2.812; 4.561) | <0.0001 |
| Presentation | |||||||||
| Other | Other versus SAP | 0.600 (0.238; 1.510) | 0.2779 | 2.124 (1.220; 3.699) | 0.0078 | 0.342 (0.185; 0.631) | 0.0006 | 2.496 (1.686; 3.697) | <0.0001 |
| NSTEMI | NSTEMI versus SAP | 1.627 (1.207; 2.191) | 0.0014 | 1.281 (0.935; 1.756) | 0.1236 | 1.286 (1.058; 1.563) | 0.0117 | 0.923 (0.758; 1.125) | 0.4277 |
| STEMI | STEMI versus SAP | 1.762(1.232; 2.521) | 0.0019 | 1.628 (1.099; 2.411) | 0.0151 | 1.224 (0.958; 1.565) | 0.1063 | 1.089 (0.846; 1.402) | 0.5073 |
IHD: Ischemic heart disease. NSTEMI: non-ST-segment elevation myocardial infarction. PCI: percutaneous coronary intervention. SAP: stable angina pectoris. STEMI: ST-segment elevation myocardial infarction.
An analysis investigating characteristics associated with readmission within 30-days was also performed. The results revealed the same tendencies in probability as seen above. Only the analysis for indication for PCI differed between the two groups, as patients who underwent PCI due to both STEMI and NSTEMI had increased risk of IHD-related readmission within the first 30 days after index procedure (OR 1.8, 95% CI 1.2–2.5 and OR 1.6, 95% CI 1.2–2.2). Patients with STEMI and “other” also had an increased probability of readmissions due to other reasons than IHD (OR 1.6, 95% CI 1.1–2.4 and OR 2.1, 95% CI 1.2–3.7).
Repeat angiography and revascularization
Of the 2673 enrolled patients with diabetes, 22% had repeat coronary angiography within the first year after index procedure. About 10% of all patients underwent repeat, unplanned PCI within 365 days, and 1% of the patients had revascularization with CABG, with a mean of 133 ± 114.7 and 152 ± 135.7 days after index procedure, respectively. A total of 155 patients received staged revascularization. The staged procedures consisted of 116 staged PCI and 39 staged CABGs. The staged PCI procedures were performed 33 days ±34.0 after PCI (Table 4).
Table 4.
Patients with new coronary angiography and revascularization within 365 days (2673).
| Patients with new revascularization | 578 (21.6%) |
| Patients with PCI | 245 (9.2%) |
| Days since PCI | 133 ± 114.7 |
| Patients with CABG | 37 (1.4%) |
| Days since PCI | 152 ± 135.7 |
| Patients with staged* revascularization | 116 (4.3%) |
| Patients with staged* PCI | 116 (4.3%) |
| Days since PCI | 33 ± 34.0 |
| Patients with staged* CABG | 39 (1.5%) |
| Days since PCI | 120 ± 19.5 |
Data presented as mean ± SD, or n (%). CABG: coronary artery bypass graft surgery. PCI: percutaneous coronary intervention. *New PCI or CABG procedures after index PCI performed without new angiogram were interpreted as stages.
Discussion
The study provided information about re-hospitalization of diabetic patients after PCI. The all-cause 30-day readmission rate was 18% for patients with diabetes. More than half (58%) of the diabetic patients were re-hospitalized within 1 year. The most frequent cause of readmission was suspicion of angina/chest pains followed by MI, and other reasons for readmission were several and various. One of ten received unplanned revascularization with PCI within 1 year. A high number of comorbidities was the strongest predictor for non-IHD-related readmission.
A thorough systematic review and meta-analysis has identified the 30-day risk of readmission and potential associated risk factors for readmission. 8 Thirty days after treatment with PCI, an estimate of 1 in 7 patients were rehospitalized. The readmission rate rises to about 50% after 1 year in an all-comer population, 6 and to 71% after 5 years in an octogenarian population presenting with ACS. 15 The 30-day readmission risks range from 3.3-15.8% in the literature.8,16–19 The high readmission risks in the present study differ from previous studies due to multiple reason. First, the indication for PCI varied from high-risk emergency treatments to low-risk elective patients. Furthermore, a majority of the studies in the review originated in the United States, where insurance and healthcare models differ significantly from the Danish National Health Services, which offer universal tax-supported health care, covering free access to general practitioners and hospitals. Finally, the diabetic population is known to be more vulnerable, and diabetes is an independent predictor for readmission after PCI.2,12,13,17,20 To our knowledge, there has not previously been conducted a study investigating readmission in a population of diabetics undergoing PCI, and the present results are therefore challenging to compare with the existing literature.
The proportion of patients with cardiac readmissions in the meta-analysis varies from 4.6-75.3%. 8 In the present study, non-IHD-related readmission accounted for the majority of the rehospitalizations compared to IHD-related readmissions (31% vs 27%), whereas the IHD-related readmissions were slightly dominating after 30-days (9.4% vs 8.7%). Chest pain is the most common reason for readmission, and ACS was the second most common reason. The proportions are higher than seen in other work. Diabetic patients are known to have higher risk of major adverse cardiac events after PCI compared to non-diabetic patients, and the findings are therefore not surprising.21,22 However, non-IHD related reasons for readmission are most likely not related to the index procedure and possibly not due to PCI complications. In a previous validation study investigating predictors for hospital readmission risk among diabetic patients discharged from the hospital, 1 out of 5 diabetic patients was readmitted within 30-days for any cause. 23 The reason for readmission ranges from heart failure, chest pains or dyspnea, kidney failure, infection or complications of device or implant, and the burden of macrovascular diabetes complications (coronary artery disease, stroke, heart failure and peripheral vascular disease) were strong predictors for readmission. 23 The high incidence of non-IHD related readmission in the current study is possibly due to the burden of comorbidity, and not the PCI itself.
A study by Gyldenkerne et al. 24 concluded that diabetic patients with concomitant diabetes and coronary artery disease had a much higher risk of MI and all-cause death compared to non-diabetic patients with coronary artery disease. Patients with diabetes also have a higher risk of stroke even when coronary artery disease is not present. 25 It is suggested that interaction between cardiovascular disease and diabetes enhances the risk of micro- and macrovascular complications, such as stroke, peripheral artery disease and kidney failure, which could explain the association with worse outcome. Although patients with diabetes with a coronary angiography without coronary artery disease did not have an increased risk of MI compared to non-diabetic patients, 24 they remained at increased risk of stroke and all-cause death.25,26 Our study supported the implication that diabetic patients with comorbidities continuous to be a high-risk patient group with worse outcome and increased risk of readmission and should be treated with caution and awareness.
Patients presenting with ACS (STEMI or NSTEMI) did not have an increased risk of redamission for non-IHD reasons at 12 months, but “other” indication for PCI increased the risk for readmission after both 1-year and 30-days. Patients undergoing revascularization with PCI due to other reasons than STEMI, NSTEMI or SAP consists of a high-risk group of patients. Other reasons included PCI in relation to valve disease, arrhythmia, and congestive heart failure with severe ejection fraction. Even though it is tempting to believe, that urgent emergency treatments of high-risk patients presenting with STEMI result in high readmission risk, the STEMI-patients had an increased risk within the first 30-days for both IHD and non-IHD related readmission compared to SAP, but no increased risk within 365 days after the index procedure. Our previous analysis found unplanned revascularization with PCI in 7.3% of all patients undergoing PCI within 365 days and CABG in 1%. 6 In the present study, diabetic patients showed slightly higher risk of unplanned revascularization, as 9% of the diabetic patients underwent unplanned PCI, and 1% unplanned CABG. Among patients undergoing PCI, diabetes mellitus is associated with increased long-term risk of death, MI and repeat revascularization compared to patients without diabetes when treated with bare-metal-stents. However, the development of the drug-eluting stents (DES) has significantly reduced the risk.5,22,27 Cardiovascular disease in diabetic patients is more likely to consist of complex, multi-vessel lesions, small vessels with diffuse disease and containing more calcification, necrotic core and thin-cap atheroma.11,28 Studies and meta-analyses have concluded that the increased risk of repeated revascularization is associated with the complexity of coronary lesions, as diabetic patients with non-complex lesions have the same revascularization rate as non-diabetic patients treated with DES.29,30
Limitations
There are several limitations to this study. Only the first readmission diagnosis after index PCI was included in the data set, and we did not distinguish between patients who were readmitted several times within 1 year. Also, readmission within 2 days after index PCI was interpreted as transfer between hospitals or department in relation to the index admission, thereby risking exclusion of very early and acute readmission. Furthermore, the ICD-10 codes used for heart failure were not specified into acute or chromic heart failure, and as all patients have IHD we cannot clarify if acute heart failure has been classified as ACS if the cardiac biomarkers have been increased. Among 155 rehospitalizations due do a new PCI or CABG procedures without a new angiogram before the intervention, the intervention were interpreted as staged. From an economic point of view a rehospitalization will count either if it is acute or staged, but the patient experience may differ. Also, the retrospective study design made it difficult to make a statement about causality. Finally, the data from the present study represents a population with free access to healthcare, which may have impacted the readmission rates, and the study is thereby limited in terms of generalizing the data to other healthcare systems and hospitals without these patient advantages.
Conclusion
More than half of patients with diabetes treated with PCI were rehospitalized within 365 days. Comorbidity is a strong predictor for readmission, especially for non-IHD related readmission. Patients with diabetes are a complex patient population, and diabetic patients continue to be a high-risk patient group with increased risk for rehospitalization and repeat revascularization.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Kirstine N Hansen https://orcid.org/0000-0003-4457-1713
Rikke Søgaard https://orcid.org/0000-0003-3557-8550
References
- 1.Orbach A, Halon DA, Jaffe R, et al. Impact of diabetes and early revascularization on the need for late and repeat procedures. Cardiovasc Diabetol 2018; 17: 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ida S, Kaneko R, Imataka K, et al. Relationship between frailty and mortality, hospitalization, and cardiovascular diseases in diabetes: a systematic review and meta-analysis. Cardiovasc Diabetol 2019; 18: 81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Einarson TR, Acs A, Ludwig C, et al. Psrevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007-2017. Cardiovasc Diabetol 2018; 17: 83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Montalescot G, Sechtem U, Achenbach S, et al. ESC guidelines on the management of stable coronary artery disease: the task force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 2013; 34: 2949–3003. [DOI] [PubMed] [Google Scholar]
- 5.Maeng M, Jensen LO, Kaltoft A, et al. Comparison of stent thrombosis, myocardial infarction, and mortality following drug-eluting versus bare-metal stent coronary intervention in patients with diabetes mellitus. Am J Cardiol 2008; 102: 165–172. [DOI] [PubMed] [Google Scholar]
- 6.Hansen KN, Bendix K, Antonsen L, et al. 1-year rehospitalization after percutaneous coronary intervention: a retrospective analysis. EuroIntervention 2018; 14(8): 926–934. [DOI] [PubMed] [Google Scholar]
- 7.Wasfy JH, Strom JB, O’Brien C, et al. Causes of short-term readmission after percutaneous coronary intervention. Circ Cardiovasc Interv 2014; 7: 97–103. [DOI] [PubMed] [Google Scholar]
- 8.Kwok CS, Narain A, Pacha HM, et al. Readmissions to hospital after percutaneous coronary intervention: a systematic review and meta-analysis of factors associated with readmissions. Cardiovasc Revasc Med 2020; 21: 375–391. [DOI] [PubMed] [Google Scholar]
- 9.Lemor A, Hernandez GA, Patel N, et al. Predictors and etiologies of 30-day readmissions in patients with non-ST-elevation acute coronary syndrome. Catheter Cardiovasc Interv 2019; 93: 373–379. [DOI] [PubMed] [Google Scholar]
- 10.Donahoe SM, Stewart GC, McCabe CH, et al. Diabetes and mortality following acute coronary syndromes. J Am Med Assoc 2007; 298: 765–775. [DOI] [PubMed] [Google Scholar]
- 11.Creager MA, Lüscher TF, Cosentino F, et al. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: Part I. Circulation 2003; 108: 1527–1532. [DOI] [PubMed] [Google Scholar]
- 12.Tisminetzky M, Gurwitz JH, Miozzo R, et al. Impact of cardiac- and noncardiac-related conditions on adverse outcomes in patients hospitalized with acute myocardial infarction. J Comorb 2019; 9: 2235042x19852499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nakatani D, Sakata Y, Mizuno H, et al. Impact of diabetes mellitus on rehospitalization for heart failure among survivors of acute myocardial infarction in the percutaneous coronary intervention era. Circ J 2009; 73: 662–666. [DOI] [PubMed] [Google Scholar]
- 14.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373–383. [DOI] [PubMed] [Google Scholar]
- 15.Barywani SB, Petzold M. Octogenarians died mainly of cardiovascular diseases five years after acute coronary syndrome. Scand Cardiovasc J 2016; 50: 300–304. [DOI] [PubMed] [Google Scholar]
- 16.Yost GW, Puher SL, Graham J, et al. Readmission in the 30 days after percutaneous coronary intervention. J Am Coll Cardiol Cardiovasc Interv 2013; 6: 237–244. [DOI] [PubMed] [Google Scholar]
- 17.Ricciardi MJ, Selzer F, Marroquin OC, et al. Incidence and predictors of 30-day hospital readmission rate following percutaneous coronary intervention (from the National Heart, Lung, and Blood Institute Dynamic Registry). Am J Cardiol 2012; 110: 1389–1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moretti C, D’Ascenzo F, Omede P, et al. Thirty-day readmission rates after PCI in a metropolitan center in Europe: incidence and impact on prognosis. J Cardiovasc Med 2015; 16: 238–245. [DOI] [PubMed] [Google Scholar]
- 19.Hannan EL, Zhong Y, Krumholz H, et al. 30-day readmission for patients undergoing percutaneous coronary interventions in New York state. J Am Coll Cardiol Cardiovasc Interv 2011; 4: 1335–1342. [DOI] [PubMed] [Google Scholar]
- 20.Wasfy JH, Rosenfield K, Zelevinsky K, et al. A prediction model to identify patients at high risk for 30-day readmission after percutaneous coronary intervention. Circ Cardiovasc Qual Outcomes 2013; 6: 429–435. [DOI] [PubMed] [Google Scholar]
- 21.Ellert J, Christiansen EH, Maeng M, et al. Impact of diabetes on clinical outcomes after revascularization with sirolimus-eluting and biolimus-eluting stents with biodegradable polymer from the SORT OUT VII trial. Catheter Cardiovasc Interv 2019; 93: 567–573. [DOI] [PubMed] [Google Scholar]
- 22.Iglesias JF, Heg D, Roffi M, et al. Five-year outcomes in patients with diabetes mellitus treated with biodegradable polymer sirolimus-eluting stents versus durable polymer everolimus-eluting stents. J Am Heart Assoc 2019; 8: e013607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rubin DJ, Handorf EA, Golden SH, et al. Development and novel tool to predict hospital readmission risk among patients with diabetes. Endocr Pract 2016; 22: 1204–1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gyldenkerne C, Olesen KK, Thrane PG, et al. Diabetes is not a risk factor for myocardial infarction in patients without coronary artery disease: a study from the Western Denmark Heart Registry. Diab Vasc Dis Res 2020; 17: 1479164120941809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Olesen KKW, Madsen M, Gyldenkerne C, et al. Diabetes mellitus is associated with increased risk of ischemic stroke in patients with and without coronary artery disease. Stroke 2019; 50: 3347–3354. [DOI] [PubMed] [Google Scholar]
- 26.Olesen KKW, Madsen M, Gyldenkerne C, et al. Ten-year cardiovascular risk in diabetes patients without obstructive coronary artery disease: a retrospective Western Denmark cohort study. Cardiovasc Diabetol 2021; 20: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jensen LO, Maeng M, Kaltoft A, et al. Stent thrombosis, myocardial infarction, and death after drug-eluting and bare-metal stent coronary interventions. J Am Coll Cardiol 2007; 50: 463–470. [DOI] [PubMed] [Google Scholar]
- 28.Marso SP, Mercado N, Maehara A, et al. Plaque composition and clinical outcomes in acute coronary syndrome patients with metabolic syndrome or diabetes. J Am Coll Cardiol Cardiovasc Imaging 2012; 5: S42–S52. [DOI] [PubMed] [Google Scholar]
- 29.Farkouh ME, Domanski M, Sleeper LA, et al. Strategies for multivessel revascularization in patients with diabetes. New Engl J Med 2012; 367: 2375–2384. [DOI] [PubMed] [Google Scholar]
- 30.Kedhi E, Généreux P, Palmerini T, et al. Impact of coronary lesion complexity on drug-eluting stent outcomes in patients with and without diabetes mellitus: analysis from 18 pooled randomized trials. J Am Coll Cardiol 2014; 63: 2111–2118. [DOI] [PubMed] [Google Scholar]