Abstract
This study aimed to compare sedentary time (SED) and intensity‐specific physical activity (PA) estimates and the associations of SED and PA with body mass index (BMI) and waist circumference (WC) using three different sets of cut‐points in preschool‐aged children. A total of 751 children (4.7 ± 0.9 years, boys 52.7%) wore an ActiGraph GT3X+BT accelerometer on their hip for 7 days (24 h). Euclidean norm −1 G with negative values rounded to zero (ENMO) and activity counts from vertical axis (VACounts) and vector magnitude (VMCounts) were derived. Estimates of SED and light, moderate, vigorous, and moderate‐to‐vigorous PA (MVPA) were calculated for commonly used cut‐points by Hildebrand et al., Butte et al., and Evenson et al. Furthermore, the prevalence of meeting the PA recommendation, 180 min/day of which at least 60 min/day being MVPA, were assessed for the cut‐points. Multilevel mixed analysis was used to examine associations of SED and PA with BMI and WC. In accordance with the results, SED and PA intensity estimates differed largely across cut‐points (i.e., SED = 22–341 min/day; light PA = 52–257 min/day; moderate PA = 5–18 min/day; vigorous PA = 7–17 min/day; MVPA = 13–35 min/day), and the prevalence of children meeting the PA recommendation varied from 4% to 70%. Associations of SED and PA with BMI or WC varied between the cut‐points. Our results indicate that SED and PA estimates in preschool‐aged children between studies using these cut‐points are poorly comparable. Methods facilitating accelerometer‐derived PA estimate comparison between studies are highly warranted.
Keywords: acceleration metrics, adiposity, exercise, sedentary behavior, youth
1. INTRODUCTION
Engaging in sufficient levels of physical activity (PA) has been connected to numerous health benefits, including lower adiposity in preschool‐aged children (3–5 years). 1 In accordance with the World Health Organization (WHO) PA recommendations, preschool‐aged children should spend at least 180 min a day engaging in PA at any intensity, with the inclusion of at least 60 min of moderate‐to‐vigorous intensity PA (MVPA). 2 Conflictingly, the proportion of preschoolers complying with the recommendation has been reported to vary between 11%–93% when assessed with accelerometers. 3 , 4 , 5 In addition to actual variation in children's habitual PA, accelerometer‐defined PA metrics 6 and cut‐points 7 used have been found to influence the proportions.
Accelerometers are the most widely used objective method of assessing PA in research currently. 8 There are several types of accelerometers and data processing methods available to assess SED and PA, but the estimates of these different methods have been found inconsistent. 9 Usually, accelerometers collect a raw acceleration signal at a pre‐specified frequency and they are cleaned (i.e., gravitational acceleration and noise are removed from the signal) and aggregated over a time period (i.e., epoch). The data processing to clean the signal has traditionally been performed directly by the manufacturers, with the activity counts by ActiGraph being the most frequent acceleration metrics used in previous literature. Activity counts are usually calculated as the vector magnitude of the three axes (VMCounts) or as the one‐dimensional vertical axis (VACounts). Thereafter, age‐appropriate cut‐points are defined to distinguish intensity‐specific PA. 10 , 11 However, activity counts are not comparable between accelerometers from different manufacturers, or even between different generations of accelerometers from the same manufacturer. 9 , 12 Cut‐points are usually calibrated in small studies with limited sample sizes and underrepresented activities of daily life. 10 , 11 , 13 , 14 Therefore, it is typical to observe large discrepancies in the estimation of PA intensities from various cut‐points when they are extrapolated to different settings and/or participants. 15 The development of open‐source algorithms to clean the raw signal is now an alternative to activity counts. 16 , 17 The Euclidean Norm of the raw acceleration in the three axes Minus One G (ENMO, 1 G ~ 9.8 m/s2) with negative values rounded to zero has become widely used and has shown a high agreement between brands, 18 facilitating data harmonization across studies. Although, open‐source raw accelerometer data processing has been warranted in order to increase equivalency of data outputs and improved comparability between studies using different devices, 19 using activity counts provides better comparability with the majority of previous literature. Yet the comparability across commonly used cut‐points based on activity counts and open‐source methods has only been studied in school‐aged children thus far warranting the need to confirm the findings in preschool‐aged children.
Several cut‐points have been used to classify PA intensity from hip‐worn accelerometers in preschoolers. VACounts have been frequently used to assess PA in children 20 and the commonly used cut‐points by Evenson et al. 11 have been cross‐validated among 5 to 15‐year‐old children. 21 The cut‐points by Butte et al. 10 provide PA intensities based on the VMCounts measurements in preschool‐aged children. The more recently developed ENMO measurements offer an open‐source method increasing comparability between studies, and the cut‐points by Hildebrand et al. 13 , 14 have been previously used in children and provide the most reference data. 6 , 19 , 22 A previous study in preschoolers 7 reported that cut‐points by Butte et al. 10 led to less sedentary time (SED) and more light PA and MVPA compared to estimates using cut‐points by Janssen et al. 23 based on VACounts. In school‐aged children, 6 , 22 Hildebrand et al. 13 , 14 has been shown to provide less moderate and vigorous PA compared to estimates using Evenson et al. 11 and Romanzini et al. 24 who used VMCounts. However, it has also been found that Hildebrand et al. 13 , 14 provided more moderate PA and less vigorous PA compared to estimates using Evenson et al. 11 in another study in school‐aged children. 19 The proportions of school‐aged children meeting the PA recommendation (i.e., at least 60 min of MVPA per day) have been reported to vary considerably between different cut‐points. 6 , 19 Yet, there is a lack of previous studies comparing acceleration estimates based on both traditional activity counts and open‐source metrics and cut‐points in preschool‐aged children, even though such knowledge would be essential for comparing SED and PA estimates between studies.
To date, information on comparability between estimates of SED and PA in preschool‐aged children based on different cut‐points is scarce, especially using open‐source metrics. Furthermore, there is a lack of studies examining whether associations of SED and PA with the most frequently used health indicators vary when using different SED and PA cut‐points based on the commonly used metrics. Overweight and obesity are closely connected to health. 25 Their associations with SED and PA have been widely investigated, although with inconsistent findings. 26 Associations of SED and PA with overweight and obesity have been studied in children also compositionally taking the relative changes in the daily activities into account. 27 However, due to the differences in the study designs and methods assessing SED, PA and weight status, conclusions about the associations should still be drawn with caution. 26 Since body mass index (BMI) is the most common method to assess obesity and waist circumference (WC) is an important marker of central obesity, they have been recommended to be used as a routine measurement in clinical practice. 28 Therefore, it is of high importance to further examine how their associations with SED and PA are dependent on the cut‐points used based on data from the same study. Therefore, the aims of this study were to compare (1) SED and intensity‐specific PA estimates and (2) the associations of SED and PA with anthropometrics (BMI and WC) when using three different cut‐points (VACountsEvenson, VMCountsButte, and ENMOHildebrand) in preschool‐aged children.
2. MATERIALS AND METHODS
2.1. Study design and participants
The present study utilizes cross‐sectional data from the Increased Health and Wellbeing in Preschools (DAGIS) study. 29 The study was conducted in early childhood education and care (ECEC) centers in southern and western Finland in 2015–2016. The eligibility criteria for the ECEC centers in the study were: (1) having at least one group consisting of 3–6‐year‐old children, (2) providing early education only during the daytime, (3) being Finnish or Swedish speaking (official languages of Finland), and (4) charging income‐dependent fees. In total, 864 children (25% of the invited children, boys 52%) and their families, from 66 ECEC centers (43% of the invited ECEC centers) in 8 municipalities participated in the study. Guardians gave their written informed consent. The study was approved by the University of Helsinki Ethical Review Board in the Humanities and Social and Behavioral Sciences in February 2015 (#6/2015).
2.2. Assessment of sedentary time and physical activity
SED and PA were measured using a hip‐worn triaxial ActiGraph wGT3X‐BT accelerometer (Pensacola, FL, USA) for 7 days, 24 h per day. The raw accelerations that were collected using 30 Hz were processed using ActiLife v.6.13.3 (ActiGraph, Pensacola, FL, USA) to obtain VMCounts and VACounts using the normal filter developed by ActiGraph. Additionally, we exported the raw accelerations in “.csv” files to process them in the GGIR R package v. 1–5.12 30 to obtain ENMO.
For VMCounts and VACounts, we used ActiLife to obtain the SED and PA intensity metrics. For such purpose, periods of ≥10 min of consecutive zeros were regarded as non‐wear time and removed from the further analyses. 31 In addition, the times between parent‐reported sleep onset and wake‐up were excluded. A valid day was defined as ≥600 min of wearing time during waking hours, and children with valid data on at least 3 weekdays and 1 weekend day were included in the analyses. A 15‐s epoch length was used for VACounts and the Evenson et al. cut‐points were applied (VACountsEvenson). 11 VMCounts were aggregated in 60‐s epochs and the Butte et al. cut‐points were used (VMCountsButte) 10 (Table 1). The epoch and cut‐points decisions were based on the practical considerations reported in a previous systematic review. 20
TABLE 1.
Children's age‐appropriate cut‐points for the estimation of sedentary time (SED) and physical activity (PA) intensities (N = 751)
| References | Acceleration metric | Epoch length | SED/Light PA | Light PA/Moderate PA | Moderate PA/Vigorous PA |
|---|---|---|---|---|---|
| Hildebrand et al. 13 , 14 | ENMO | 5 s | 40 mg | 140 mg | 465 mg |
| Butte et al. 10 | VMCounts | 60 s | 820 c | 3908 c | 6112 c |
| Evenson et al. 11 | VACounts | 15 s | 26 c | 574 c | 1003 c |
Abbreviations: c, Activity counts; ENMO, Euclidean norm −1 g; VACounts, Vertical axis counts; VMCounts, Vector magnitude counts.
The GGIR R package was used to obtain the SED and PA intensity metrics based on ENMO. 30 The processing methods involved the following: (1) Auto‐calibration of the data according to the local gravity. 32 (2) Detection of the non‐wear time based on the raw acceleration of the three axes. 17 In brief, each 15‐min block was classified as non‐wear time if the standard deviation of 2 out of the 3 axes was lower than 13 mg during the surrounding 60‐min moving window, or if the value range for 2 out of the 3 axes was lower than 50 mg. (3) Detection of sustained abnormal high accelerations higher than 5.5 g. (4) Calculation of the ENMO as (~9.8 m/s2) with negative values rounded to zero. (5) Imputation of detected non‐wear time and abnormal high accelerations by means of the acceleration for the rest of the recording period during the same time interval as the affected periods. (6) Identification of waking and sleeping hours using an automatized algorithm guided by parent‐reported sleep times. 33 Finally, estimation of SED and PA intensities were calculated using the Hildebrand et al. 13 , 14 cut‐points for ENMO (ENMOHildebrand) (Table 1). Mean daily SED and PA intensity levels were then calculated as: (mean of available weekdays*5 + mean of available weekend days*2)/7. Furthermore, meeting the WHO recommendation for PA (i.e., 180 min/day at any PA intensity including at least 60 min MVPA) 34 was assessed for VACountsEvenson, VMCountsButte, and ENMOHildebrand.
2.3. Assessment of anthropometrics
Weight and height were measured by trained researchers, and thereafter, BMI was calculated as body weight (kg) / height2 (m). The threshold for being overweight/obese was defined using the age‐ and sex‐specific BMI cut‐offs of the International Obesity Task Force criteria. 35 WC was measured over one layer of clothing twice to the nearest 0.1 cm with measuring tapes (SECA 201) and the mean of these values was calculated. Waist was defined as the midpoint between the top of the iliac crest and the lower margin of the last palpable rib.
2.4. Covariates
Children's age and sex were reported by the parents. Families participated in the study during different seasons and, therefore, the research time was divided into three categories: fall (September‐October), winter (November‐December) and spring (January‐April). The educational level of both parents was inquired by a questionnaire and further categorized as low educational level (i.e., comprehensive, vocation, or high school), middle educational level (i.e., bachelor's degree or college), or high educational level (i.e., master's degree or licentiate/doctor).
2.5. Statistical analysis
Descriptive statistics were calculated as means, standard deviations (SD), and percentages (%). Comparing the time estimates of SED, light PA, moderate PA, vigorous PA, and MVPA between each pair of VACountsEvenson, VMCountsButte, and ENMOHildebrand estimations were conducted using paired‐samples t‐test, Bland‐Altman plots with their limits of agreement (LOA), mean absolute percent error (MAPE), and Lin's concordance correlation coefficient (LCCC). Since VACountsEvenson is the most traditional acceleration metric and cut‐points from these three, it was used as a reference against VMCountsButte and ENMOHildebrand in the analyses regarding MAPE. As no criterion measure exists, VMCountsButte was randomly selected as the reference cut‐points between VMCountsButte and ENMOHildebrand. Multilevel mixed model at the ECEC centers level was used to assess the associations of SED and PA based on VACountsEvenson, VMCountsButte, and ENMOHildebrand with BMI and WC. All models were adjusted for child's age and sex, research season, parental educational level, and accelerometer wear time. Assumptions were visually checked and they were not violated. In this study, the interest was which one of the multilevel mixed models, or both, in each pairwise comparisons contained the correct set of regressors and were more suitable to model BMI or WC. Therefore, we used the J test 36 to examine whether the associations of SED and PA with BMI and WC differed statistically between each pair of the cut‐points used in estimating SED and PA. To control for differences in wear time, paired‐samples t‐test, MAPE, and LCCC as sensitivity analysis were performed by standardizing SED estimates for wear time previously proposed. 37 The analyses were performed in SPSS statistical software (version 26.0) and in R software. Statistical significance was considered when p < 0.05.
3. RESULTS
Valid accelerometer data were obtained for 751 children with 4 (0.7%), 5 (3.7%), 6 (19.0%), and 7 (76.6%) days, and on average the children wore the accelerometer for 6.7 days (SD 0.57). Background characteristics as well as the time spent in SED and various PA intensities based on the different cut‐points are reported in Table 2. The differences between SED and PA intensities estimated from the different cut‐points expressed in min/day are graphically presented in Figure 1. Moreover, the proportion of children meeting the PA recommendations varied from ENMOHildebrand 3.6% to VMCountsButte 46.1% and VACountsEvenson 69.5% (Figure 2). The prevalence was higher for boys than for girls, regardless of the used cut‐points.
TABLE 2.
Descriptive characteristics of participating children
| All | Boys | Girls | p e | ||||
|---|---|---|---|---|---|---|---|
| N | Mean ± SD | N | Mean ± SD | N | Mean ± SD | ||
| Age (years) | 751 | 4.7 ± 0.9 | 396 | 4.8 ± 0.9 | 355 | 4.7 ± 0.9 | 0.24 |
| Height (cm) | 720 | 109.5 ± 7.8 | 372 | 110.5 ± 7.9 | 348 | 108.6 ± 7.7 | 0.001 |
| Weight (kg) | 719 | 19.2 ± 3.5 | 372 | 19.6 ± 3.5 | 347 | 18.8 ± 3.4 | 0.003 |
| BMI (kg/m2) | 719 | 15.9 ± 1.4 | 372 | 15.9 ± 1.3 | 347 | 15.8 ± 1.4 | 0.43 |
| Overweight or obese a (N, %) | 719 | 83 (11.5) | 372 | 40 (10.8) | 347 | 43 (12.4) | 0.50 |
| Waist circumference (cm) | 719 | 53.7 ± 4.0 | 372 | 54.0 ± 3.8 | 347 | 53.5 ± 4.2 | 0.076 |
| Parental education level b (N, %) | 747 | 396 | 351 | 0.11 | |||
| Low | 161 (21.6) | 89 (22.5) | 72 (20.5) | ||||
| Middle | 320 (42.8) | 156 (39.4) | 164 (46.7) | ||||
| High | 266 (35.6) | 151 (38.1) | 115 (32.8) | ||||
| Research season c (N, %) | 751 | 396 | 354 | 0.79 | |||
| Fall | 306 (40.7) | 163 (41.2) | 143 (40.3) | ||||
| Winter | 285 (37.9) | 153 (38.6) | 132 (37.2) | ||||
| Spring | 160 (21.3) | 80 (20.2) | 80 (22.5) | ||||
| PA and SED (min/day) d | |||||||
| SED | |||||||
| ENMOHildebrand | 751 | 711.1 ± 50.3 | 396 | 709.6 ± 50.0 | 355 | 712.8 ± 50.6 | 0.39 |
| VMCountsButte | 751 | 370.2 ± 54.7 | 396 | 366.5 ± 54.7 | 355 | 374.2 ± 54.5 | 0.055 |
| VACountsEvenson | 751 | 392.4 ± 46.6 | 396 | 385.2 ± 46.7 | 355 | 400.4 ± 45.2 | <0.001 |
| Light PA | |||||||
| ENMOHildebrand | 751 | 122.8 ± 23.4 | 396 | 126.9 ± 23.4 | 355 | 118.3 ± 22.7 | <0.001 |
| VMCountsButte | 751 | 379.6 ± 41.6 | 396 | 378.3 ± 41.1 | 355 | 381.1 ± 42.3 | 0.36 |
| VACountsEvenson | 751 | 327.5 ± 34.7 | 396 | 330.2 ± 34.3 | 355 | 324.6 ± 34.9 | 0.029 |
| Moderate PA | |||||||
| ENMOHildebrand | 751 | 33.7 ± 10.6 | 396 | 34.9 ± 11.0 | 355 | 32.3 ± 10.1 | 0.001 |
| VMCountsButte | 751 | 46.4 ± 18.6 | 396 | 51.3 ± 18.6 | 355 | 40.9 ± 17.0 | <0.001 |
| VACountsEvenson | 751 | 51.9 ± 14.6 | 396 | 56.1 ± 14.7 | 355 | 47.1 ± 13.0 | <0.001 |
| Vigorous PA | |||||||
| ENMOHildebrand | 751 | 3.4 ± 2.5 | 396 | 3.4 ± 2.6 | 355 | 3.4 ± 2.3 | 0.97 |
| VMCountsButte | 751 | 12.6 ± 8.6 | 396 | 13.4 ± 9.1 | 355 | 11.7 ± 7.8 | 0.006 |
| VACountsEvenson | 751 | 19.9 ± 9.4 | 396 | 21.2 ± 9.9 | 355 | 18.6 ± 8.8 | <0.001 |
| MVPA | |||||||
| ENMOHildebrand | 751 | 37.1 ± 12.4 | 396 | 38.3 ± 12.8 | 355 | 35.8 ± 11.9 | 0.006 |
| VMCountsButte | 751 | 59.0 ± 24.5 | 396 | 64.8 ± 24.9 | 355 | 52.6 ± 22.5 | <0.001 |
| VACountsEvenson | 751 | 71.8 ± 22.2 | 396 | 77.3 ± 22.6 | 355 | 65.7 ± 20.1 | <0.001 |
| Wearing time during waking hours | |||||||
| ENMOHildebrand | 751 | 862.8 ± 41.8 | 396 | 865.7 ± 40.7 | 355 | 859.5 ± 42.9 | 0.040 |
| VMCountsButte | 751 | 808.8 ± 34.4 | 396 | 809.6 ± 34.2 | 355 | 807.9 ± 34.6 | 0.51 |
| VACountsEvenson | 751 | 791.7 ± 36.0 | 396 | 792.5 ± 36.3 | 355 | 790.8 ± 35.6 | 0.50 |
Abbreviations: ENMO, Euclidean norm −1 g; MVPA, Moderate‐to‐vigorous physical activity; PA, physical activity; SED, sedentary time; VACounts, Vertical axis counts; VMCounts, Vector magnitude counts.
According to Cole and Lobstein 35 .
Low educational level included comprehensive, vocation, or high school; middle educational level included bachelor's degree or college; and high educational level included master's degree or licentiate/doctorate.
Fall was defined as September–October, winter was defined as November–December, and spring was defined as January–April.
Cut‐points by Hildebrand et al. 13 , 14 for ENMOHildebrand, Butte et al. 10 for VMCountsButte, and Evenson et al. 11 for VACountsEvenson.
T‐test for continuous variables and chi‐square test for categorized variables. Significant values are bolded.
FIGURE 1.
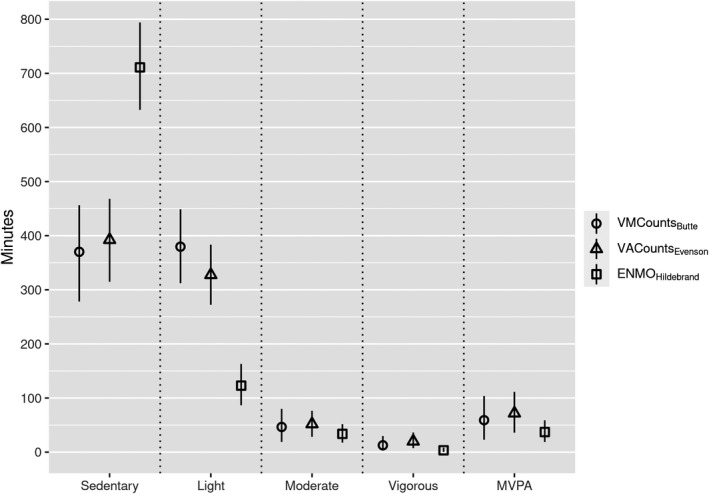
Mean daily time spent (min) and standard deviations (error bars) in sedentary time and physical activity intensitites considering different cut‐points (N = 751). Cut‐points expressed in the legend with the acceleration metric used and the first author of the validation study in subscripts, that is, Butte et al. 10 , Hildebrand et al. 13 , 14 , and Evenson et al. 11 VMCounts: Vector magnitude counts; VACounts: Vertical axis counts; ENMO: Euclidean norm −1 g
FIGURE 2.
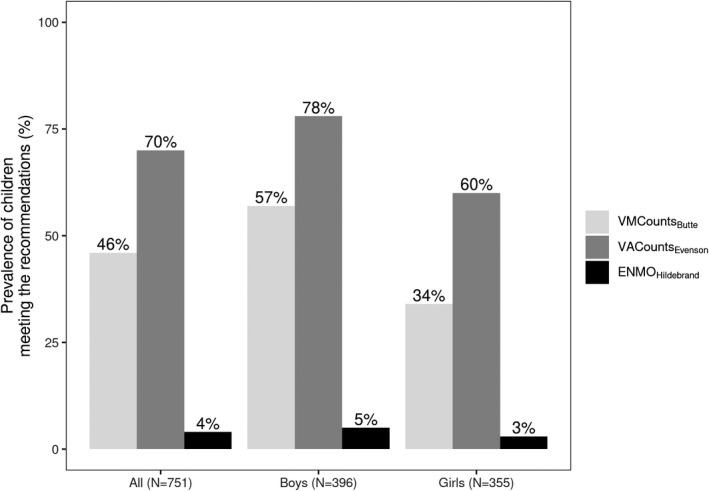
Proportion of children meeting the physical activity recommendation (at least 180 min a day engaging in physical activity at any intensity, with the inclusion of at least 60 min of moderate‐to‐vigorous PA considering different cut‐points (Hildebrand et al. 13 , 14 for ENMOHildebrand, Butte et al. 10 for VMCountsButte, and Evenson et al. 11 for VACountsEvenson). VMCounts: Vector magnitude counts; ENMO: Euclidean norm −1 g; VACounts: Vertical axis counts
Further comparisons between SED and PA intensities estimates are shown in Table 3. All pairwise comparisons were significantly different (p < 0.05). The various mean daily estimations differed between 22–341 min/day for SED, 52–257 min/day for light PA, 5–18 min/day for moderate PA, 7–17 min/day for vigorous PA, and 13–35 min/day for MVPA, respectively. The lowest MAPE was between VACountsEvenson and VMCountsButte in SED (8.7), while the highest MAPE was between VACountsEvenson and ENMOHildebrand in vigorous PA (785.9). Furthermore, the strongest LCCC was between VACountsEvenson and VMCountsButte in moderate PA (0.82), while the weakest LCCC was between VMCountsButte and ENMOHildebrand in light PA (0.01).
TABLE 3.
Comparison between sedentary time (SED) and physical activity (PA) calculated from different cut‐points (N = 751)
|
Difference (min/d) |
LOA |
MAPE (%) |
LCCC | ||
|---|---|---|---|---|---|
| Mean a (95% CI) | SD | ||||
| SED | |||||
| VACountsEvenson vs. ENMOHildebrand | −319 (−322 to −315) | 45.6 | −408 to −229 | 44.8 | 0.02 |
| VACountsEvenson vs. VMCountsButte | 22 (20 to 24) | 29.5 | −36 to 80 | 8.7 | 0.76 |
| VMCountsButte vs. ENMOHildebrand | −341 (−344 to −338) | 46.2 | −431 to −250 | 48.0 | 0.03 |
| Light PA | |||||
| VACountsEvenson vs. ENMOHildebrand | 205 (203 to 207) | 30.2 | 145 to 264 | 173.9 | 0.02 |
| VACountsEvenson vs. VMCountsButte | −52 (−54 to −50) | 22.7 | −97 to −8 | 13.6 | 0.43 |
| VMCountsButte vs. ENMOHildebrand | 257 (254 to 259) | 36.1 | 186 to 327 | 217.3 | 0.01 |
| Moderate PA | |||||
| VACountsEvenson vs. ENMOHildebrand | 18 (17 to 19) | 12.0 | −5 to 42 | 62.9 | 0.28 |
| VACountsEvenson vs. VMCountsButte | 5 (5 to 6) | 8.8 | −12 to 23 | 24.5 | 0.82 |
| VMCountsButte vs. ENMOHildebrand | 13 (12 to 14) | 14.5 | −16 to 41 | 47.8 | 0.40 |
| Vigorous PA | |||||
| VACountsEvenson vs. ENMOHildebrand | 17 (16 to 17) | 8.1 | 1 to 32 | 786.3 | 0.08 |
| VACountsEvenson vs. VMCountsButte | 7 (7 to 8) | 3.9 | −0 to 15 | 413.3 | 0.68 |
| VMCountsButte vs. ENMOHildebrand | 9 (9 to 10) | 7.4 | −5 to 24 | 89.3 | 0.15 |
| MVPA | |||||
| VACountsEvenson vs. ENMOHildebrand | 35 (34 to 36) | 16.3 | 3 to 67 | 102.3 | 0.21 |
| VACountsEvenson vs. VMCountsButte | 13 (12 to 13) | 9.8 | −6 to 32 | 64.0 | 0.79 |
| VMCountsButte vs. ENMOHildebrand | 22 (21 to 23) | 18.0 | −13 to 57 | 31.1 | 0.35 |
Data are presented as mean differences, 95% confident interval (CI), and standard deviation (SD) as well as limits of agreement (LOA), mean absolute percent error (MAPE), and Lin's concordance correlation coefficient (LCCC). Cut‐points expressed with the acceleration metric used; Evenson et al. 11 , Hildebrand et al. 13 , 14 , and Butte et al. 10 .
Abbreviations: ENMO, Euclidean norm −1 g; MVPA, Moderate‐to‐vigorous physical activity; VACounts, Vertical axis counts; VMCounts, Vector magnitude counts.
Based on paired‐samples t‐test, all mean differences were p ≤ 0.001.
Bland‐Altman plots displayed in Figure 3 illustrate the differences in SED and PA estimates between each pair of the cut‐points. The mean bias for SED and all PA intensities were large when comparing the cut‐points. At the individual level, LOA were the widest for SED and light PA between VACountsEvenson and VMCountsButte with ENMOHildebrand, while LOA was the smallest for vigorous PA between VMCountsButte and VACountsEvenson. Moreover, regarding vigorous PA there was a trend between VACountsEvenson and VMCountsButte with ENMOHildebrand showing a greater difference in estimates when the mean increased.
FIGURE 3.
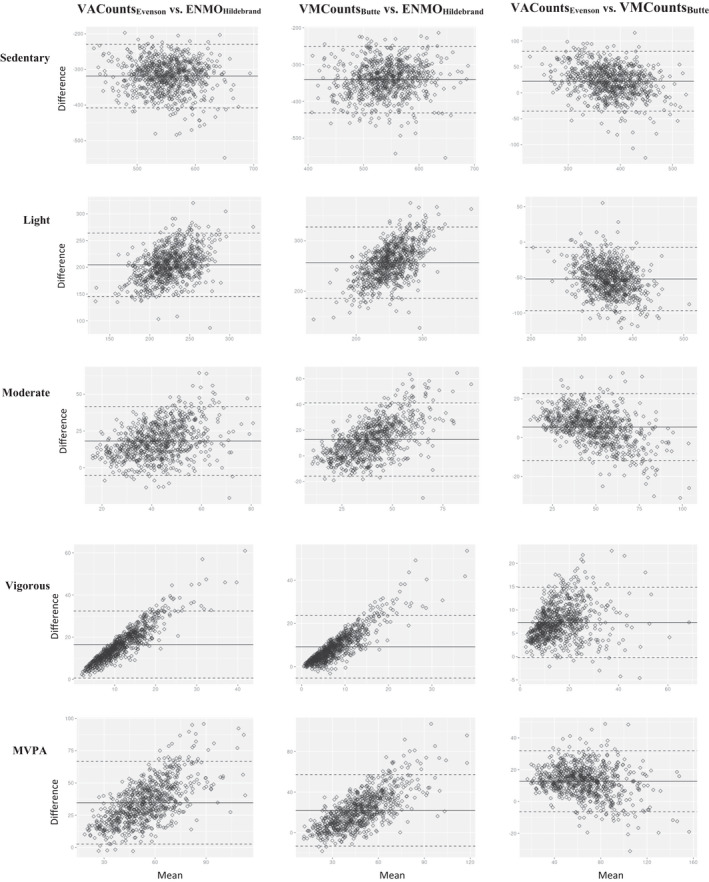
Bland‐Altman plots with their limits of agreements using three different cut‐points (Hildebrand et al. 13 , 14 for ENMOHildebrand, Butte et al. 10 for VMCountsButte, and Evenson et al. 11 for VACountsEvenson), N = 751
Table 4 shows associations of SED and PA intensities with BMI and WC. Using ENMOHildebrand, SED was inversely and light PA directly associated with BMI (both p < 0.05). Using VACountsEvenson or VMCountsButte, all associations with BMI were non‐significant. Using ENMOHildebrand, vigorous PA and MVPA were inversely associated with WC (both p < 0.05). Similarly, using VMCountsButte, moderate PA and MVPA were inversely associated with WC. Using VACountsEvenson, light PA was directly associated with WC (p = 0.010), respectively.
TABLE 4.
Multilevel mixed modelling showing the associations of sedentary time (SED) and physical activity (PA) with body mass index and waist circumference using three different cut‐points (N = 712–713)
| Body mass index | Waist circumference | |||
|---|---|---|---|---|
| β | p‐value | β | p‐value | |
| ENMOHildebrand | ||||
| SED | −0.09 | 0.043 | −0.03 | 0.40 |
| Light PA | 0.09 | 0.028 | 0.03 | 0.35 |
| Moderate PA | 0.00 | 0.91 | −0.06 | 0.078 |
| Vigorous PA | 0.01 | 0.90 | −0.10 | 0.004 |
| MVPA | 0.00 | 0.91 | −0.07 | 0.038 |
| VMCountsButte | ||||
| SED | 0.02 | 0.64 | 0.05 | 0.16 |
| Light PA | −0.03 | 0.41 | −0.01 | 0.70 |
| Moderate PA | 0.00 | 0.97 | −0.08 | 0.012 |
| Vigorous PA | 0.04 | 0.28 | −0.04 | 0.16 |
| MVPA | 0.02 | 0.67 | −0.08 | 0.017 |
| VACountsEvenson | ||||
| SED | −0.06 | 0.14 | −0.04 | 0.21 |
| Light PA | 0.06 | 0.13 | 0.08 | 0.010 |
| Moderate PA | 0.01 | 0.85 | −0.04 | 0.19 |
| Vigorous PA | 0.05 | 0.17 | −0.04 | 0.26 |
| MVPA | 0.03 | 0.46 | −0.04 | 0.18 |
Values are standardized coefficiens (β) with their p‐values based on multilevel mixed modelling. Statistically significant values are bolded.
Adjusted for the child's sex and age, accelerometer wear time, research time, and parental educational level. The analyses regarding waist circumference were additionally adjusted for child's height.
Abbreviations: ENMO, Euclidean norm −1 g; MVPA, Moderate‐to‐vigorous physical activity; VACounts, Vertical axis counts; VMCounts, Vector magnitude counts.
Table S1 presents which multilevel mixed models contained the correct set of regressors in accordance with the J test. Regarding associations with BMI, ENMOHildebrand was more suitable compared to VMCountsButte or VACountsEvenson in SED and light PA, while all three cut‐points were equally suitable in moderate PA, vigorous PA, and MVPA. Regarding associations with WC, ENMOHildebrand was more suitable compared to VMCountsButte or VACountsEvenson in SED and light PA, except VACountsEvenson was equally suitable in SED. ENMOHildebrand and VACountsEvenson were generally more suitable in models regarding moderate PA, vigorous PA, and MVPA.
In accordance with the main findings, sensitivity analyses found SED estimates differing between the cut‐points after standardizing for wear time (all p ≤ 0.001). In addition, MAPE was the lowest between VACountsEvenson and VMCountsButte (9.7) and the highest between VMCountsButte and ENMOHildebrand (44.6). LCCC was the strongest between VACountsEvenson and VMCountsButte (0.71) and the weakest between ENMOHildebrand against VMCountsButte and VACountsEvenson (both 0.02).
4. DISCUSSION
This study aimed to compare (1) SED and intensity‐specific PA estimates and (2) the associations of SED and PA with anthropometrics (BMI and WC) when using three different sets of cut‐points, VACountsEvenson, VMCountsButte, and ENMOHildebrand, in preschool‐aged children. All SED and PA estimates varied largely between the cut‐points, although VACountsEvenson and VMCountsButte were more consistent compared to ENMOHildebrand. Furthermore, the proportion of children meeting the PA recommendations as well as the associations of SED and PA intensities with BMI and WC were highly discrepant across the different cut‐points.
The SED and PA estimates differed between the three cut‐points used in the current study. Especially there was a lack of equivalence and poor agreement between ENMOHildebrand with VACountsEvenson and VMCountsButte. The poor agreement was interpreted, among other things, as large bias in the LOA analyses, which has also been seen in 10‐year‐old children comparing moderate PA, vigorous PA, and MVPA estimates between ENMOHildebrand and Romanzini et al. 22 , 24 We found that VMCountsButte provided the lowest SED estimates followed by VACountsEvenson and ENMOHildebrand. The finding regarding VMCountsButte and VACountsEvenson is similar to what has been previously shown in another study in preschoolers, 7 who reported that SED estimates were lower using VMCountsButte compare to VACountsJanssen. In school‐aged children, 6 it was shown that ENMOHildebrand provided higher SED estimates compared to VACountsEvenson, and the current study indicates that the trend is also present in younger children. Moreover, we observed that the estimates of light PA were opposite to SED; ENMOHildebrand provided the lowest estimates, followed by VACountsEvenson and VMCountsButte. This suggests a possible misclassification of light PA as SED when using the ENMOHildebrand compared to the other cut‐points included in this study. It is likely that the different metrics and cut‐points for SED and light PA may have led to these somewhat differing estimates. VACountsEvenson has been indicated to provide more accurate estimates of SED and light PA compared to other cut‐points using VACounts for ActiGraph when assessed by room calorimetry measurements in preschool‐aged children. 23 Thus, it is possible that ENMOHildebrand may detect some light PA as SED, whereas VMCountsButte may detect some SED as light PA. However, none of these can be used as a criterion. In future studies, the use of machine learning 38 or cut‐point free 39 alternatives should be considered in order to improve classification of PA. Nevertheless, the findings of the current study should be acknowledged when comparing SED and light PA estimates using ENMOHildebrand, VMCountsButte, or VACountsEvenson measurements in young children.
The estimates of MVPA were the lowest using ENMOHildebrand followed by VMCountsButte and VACountsEvenson. The observation regarding VMCounts and VACounts is similar to results previously reported in preschoolers, 7 though the opposite has been observed in school‐aged children. 6 In addition to different cut‐points, the epoch length (VACounts −15s versus VMCounts ‐ 60s) might have influenced estimates, as shorter epoch length may capture more MVPA. The activity pattern of young children is intermittent and includes very short bouts of movement, which is why shorter epoch lengths might be more suitable in capturing higher PA intensities. 20 We also found that ENMOHildebrand provided lower MVPA estimates compared to VMCountsButte and VACountsEvenson, which is supported by the previous studies in school‐aged children, 6 , 22 although opposite results have also been reported. 19 It is notable that the MVPA estimates based on ENMOHildebrand are equivalent with the studies 6 , 22 observing lower estimates using ENMOHildebrand compared to Hänggi et al. 40 and VMCountsRomanzini using VMCounts as well as to VACountsEvenson. The relatively small differences regarding ENMOHildebrand are promising in terms of comparing PA outputs between studies.
In the current study, we observed that the proportion of children meeting the PA recommendation varied from 4% (ENMOHildebrand) to 46% (VMCountsButte) and 70% (VACountsEvenson). VACountsEvenson leading to higher rates compared to VMCountsButte is in line with the study in preschoolers reporting that cut‐points by VACountsEvenson led to higher rates compared to Janssen et al. 23 using VMCounts. 7 Moreover, ENMOHildebrand leading to lower rates compared to VACountsEvenson as well as VMCountsHänggi and VMCountsRomanzini is similar to what has been reported in school‐aged children. 6 , 19 The differences in time spent in MVPA are largely explaining these differences, since all preschool‐aged children have been reported to fulfill the PA recommendation of 180 min of any PA intensity when leaving the stricter MVPA requirement out based on VACountsEvenson and VMCountsJanssen. 7 Since the PA recommendation has been used to describe sufficient levels of PA in young children, it is important to be aware of the differences in the rates of complying with the PA recommendations. However, it is worth noting that the development of the PA recommendations have been based mainly on self‐reported PA data 1 and, thus, these rates should be observed with caution. Nevertheless, more research is needed to provide information on health‐related PA based on objective methods between studies.
To the best of our knowledge, this is the first study investigating associations of SED and PA estimates with anthropometry using ENMOHildebrand measurements. We found that lower SED and higher light PA were associated with a higher BMI using ENMOHildebrand, but no associations were found when using VMCountsButte or VACountsEvenson. One reason for the associations with BMI is that the threshold for light PA in ENMOHildebrand detects light PA differently compared to counts and, therefore, some of the light PA may have been detected as SED. It is worth noting that previous studies in preschool‐aged children have reported mainly null results between SED and BMI 41 and inconsistent results between PA and BMI 1 when SED and PA have been based on cut‐points using VMCounts or VACounts. Furthermore, MVPA and vigorous PA have been observed to positively associate with fat‐free mass, but not with fat mass. 42 Since BMI is an indicator of both, the associations may be difficult to detect. Thus, BMI may not be an accurate assessment to identify children with a high body fatness at preschool age, 43 which may explain the lack of significant associations. Nevertheless, the associations of SED and PA based on ENMOHildebrand measurements with BMI should be cross‐validated using a different study population and to confirm or contravene our findings.
Vigorous PA and MVPA using ENMOHildebrand and moderate PA and MVPA using VMCountsButte were inversely associated with WC and the magnitudes of the associations were consistent. Moreover, the findings regarding MVPA was supported by the J test. Interestingly, light PA using VACountsEvenson was directly associated with WC, which is in line with the previously mentioned association between light PA using ENMOHildebrand and BMI. This may indicate that light PA using VACountsEvenson and ENMOHildebrand detect children with unfavourable anthropometrics in a similar manner.
The wear times also varied between the cut‐points as the data processing methods and algorithms differed, especially between ENMO and VMCounts/VACounts. Since we wanted to compare the actual values of the SED and PA estimates, we did not adjust the values for wear times. However, the associations of SED and PA estimates with anthropometry were adjusted for wear times in order to be comparable with the previous findings regarding associations of SED and PA with BMI and WC. However, since wear time may influence SED estimates, we ran sensitivity analyses by standardizing the SED estimates for wear times. In accordance with the findings, the differences remained similar between the cut‐points when accounting for wear time.
The strengths of the present study include a relatively large sample of children and the assessment of SED and PA in free‐living conditions with the high compliance rate. In addition, the accelerometer processing allowed us to use three different metrics and cut‐points, VACounts, VMCounts, and ENMO, based on the measurements from the same children during the same days. Yet, the similar protocols have been previously conducted in school‐aged children. 6 We are not aware of the previous studies investigating associations of SED and PA estimates using ENMOHildebrand with health outcomes in preschoolers. We included BMI and WC as outcomes, since they have both been recommended to be used as a routine measurement in clinical practice. 44 Increasing knowledge of the comparability of the associations based on different metrics and cut‐points with the commonly used measurements is not only highly valuable for PA researchers, but also for clinicians in promoting health of young children and their families.
The study also has some limitations that need to be considered. Firstly, the cut‐points we used were based on different studies including different samples and protocols, which may have produced different estimates. Secondly, the VACountsEvenson and ENMOHildebrand have been validated in slightly older children (5–8 years and 7–11 years, respectively) compared to VMCountsButte, which may have led to somewhat different SED and PA estimates. We also considered cut‐points by Crotti et al. 45 for ENMO metrics that has been developed for 5–7‐year‐old children. However, we chose to use the cut‐points by Hildebrand et al. 13 , 14 and Evenson et al., 11 since they are more commonly used cut‐points for ENMO and VACounts currently providing the largest body of reference data. 6 , 19 , 20 , 22 Furthermore, using similar protocols in processing the accelerometer data with a previous study 6 provides possibility to confirm findings in another population and age group. Future studies should clarify how PA and SED estimates on children based on the cut‐points by Crotti et al. 45 relates to the others (e.g., VACountsEvenson, VMCountsButte, and ENMOHildebrand). Some standing behaviour might have been misclassified as SED in this study. Although, a hip‐worn ActiGraph accelerometer has been found to accurately classify SED when comparing to ActivePAL, 46 it is worth noting that the authors offer a cut‐point of <22 counts per minute for an optimal for hip vertical axis, which is substantially lower than the commonly used <100 counts per minute. However, since the study was conducted in older adults (>70 years old), there is no information how such cut‐points perform in young children. Therefore, the cut‐point <100 counts per minute was used in the current study. In addition, there is probably little time per day in which a preschool child is standing still for a sustained period of time and consequently, the misclassification of standing versus SED time might be less of a problem in preschoolers than in other populations. Finally, the cross‐sectional study design rejects any conclusion about causality to be drawn from the association of SED and PA with BMI and WC. However, the aim of the study was to compare the associations between the three cut‐points with anthropometry, and not focus on investigating the associations themselves.
In conclusion, our study showed large discrepancies in the SED and PA estimates between the three cut‐points studied in preschool‐aged children, which is in line with previous findings among school‐aged children. 6 We also presented a great variety in the associations of SED and PA with BMI and WC depending on the different cut‐points. Such knowledge is essential when comparing health outcomes between studies using different methods. Furthermore, the proportions of children meeting the PA recommendations varied largely between the cut‐points used, which should be acknowledged in health promotion. In future studies, more attention should be paid to improve the comparability of SED and PA estimates in young children by, for instance, harmonizing accelerometer raw data processing methods.
5. PERSPECTIVES
In the current study, we provide an overview on the comparability of three different cut‐points based on both traditional activity counts and open‐source metrics in classifying SED and intensity‐specific PA in preschool‐aged children. Our study shows that there is great variety in the SED and PA estimates, which precludes comparisons across studies using different methods. This variety also leads to significant differences in the proportions of children meeting the PA recommendations, which makes it nearly impossible to determine the accurate rates. In addition to incongruences in the SED and PA estimates, our study also shows that the associations with health outcomes, such as BMI or WC, might be affected by the selection of cut‐points. Thus, our results not only confirm findings from previous studies, but also extend the current literature to compare three cut‐points from different metrics for young children. In future studies, there is a great need for data pooling and harmonization in order to improve comparability between studies.
CONFLICT OF INTEREST
None of the authors had a conflict of interest.
Supporting information
Table S1
ACKNOWLEDGEMENTS
The authors thank the participating families, the early childhood education and care centers, and members of the DAGIS research group for their help regarding recruitment and data collection.
Leppänen MH, Migueles JH, Abdollahi AM, Engberg E, Ortega FB, Roos E. Comparing estimates of physical activity in children across different cut‐points and the associations with weight status. Scand J Med Sci Sports. 2022;32:971–983. doi: 10.1111/sms.14147
Funding information
This research was funded by the Folkhälsan Research Center, University of Helsinki, Ministry of Education and Culture in Finland, Ministry of Social Affairs and Health, Academy of Finland (Grants: 285439, 287288, 288038), Juho Vainio Foundation, Signe and Ane Gyllenberg Foundation, Finnish Cultural Foundation/South Ostrobothnia Regional Fund, Päivikki and Sakari Sohlberg Foundation, Medicinska Föreningen Liv och Hälsa, Finnish Foundation for Nutrition Research, and Finnish Food Research Foundation
DATA AVAILABILITY STATEMENT
The data are not publicly available due to research ethical reasons and because the owner of the data is the Folkhälsan Research Center and not the research group. However, researchers interested in the data and materials from the DAGIS study may contact principal investigator Eva Roos, eva.roos@folkhalsan.fi.
REFERENCES
- 1. Carson V, Lee E, Hewitt L, et al. Systematic review of the relationships between physical activity and health indicators in the early years (0–4 years). BMC Public Health. 2017;17(Suppl 5):854‐863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Guidelines on physical activity, sedentary behaviour and sleep for children under 5 years of age. Geneva: World Health Organization; 2019. https://apps.who.int/iris/handle/10665/311664 Accessed: February 27, 2021. [PubMed]
- 3. De Craemer M, McGregor D, Androutsos O, Manios Y, Cardon G. Compliance with 24‐h movement behaviour guidelines among Belgian pre‐school children: the ToyBox‐study. Int J Environ Res Public Health. 2018;15(10):2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chaput J, Colley RC, Aubert S, et al. Proportion of preschool‐aged children meeting the Canadian 24‐hour movement guidelines and associations with adiposity: results from the Canadian Health Measures Survey. BMC Public Health. 2017;17(Suppl 5):829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cliff DP, McNeill J, Vella SA, et al. Adherence to 24‐hour movement guidelines for the early years and associations with social‐cognitive development among Australian preschool children. BMC Public Health. 2017;17(Suppl 5):857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Migueles JH, Cadenas‐Sanchez C, Tudor‐Locke C, et al. Comparability of published cut‐points for the assessment of physical activity: implications for data harmonization. Scand J Med Sci Sports. 2019;29(4):566‐574. [DOI] [PubMed] [Google Scholar]
- 7. Leeger‐Aschmann CS, Schmutz EA, Zysset AE, et al. Accelerometer‐derived physical activity estimation in preschoolers – comparison of cut‐point sets incorporating the vector magnitude vs the vertical axis. BMC Public Health. 2019;19(1):513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Strath S, Kaminsky L, Ainsworth B, et al. Guide to the assessment of physical activity: clinical and research applications: a scientific statement from the American heart association. Circulation. 2013;128(20):2259‐2279. [DOI] [PubMed] [Google Scholar]
- 9. Welk GJ, Mcclain J, Ainsworth BE. Protocols for evaluating equivalency of accelerometry‐based activity monitors. Med Sci Sports Exerc. 2012;44(1 Suppl 1):S39‐S49. [DOI] [PubMed] [Google Scholar]
- 10. Butte NF, Wong WW, Lee JS, Adolph AL, Puyau MR, Zakeri IF. Prediction of energy expenditure and physical activity in preschoolers. Med Sci Sports Exerc. 2014;46(6):1216‐1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci. 2008;26(14):1557‐1565. [DOI] [PubMed] [Google Scholar]
- 12. Grydeland M, Hansen BH, Ried‐Larsen M, Kolle E, Anderssen SA. Comparison of three generations of ActiGraph activity monitors under free‐living conditions: do they provide comparable assessments of overall physical activity in 9‐year old children? BMC Sports Sci Med Rehabil. 2014;6(1):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hildebrand M, Van hees VT, Hansen BH, Ekelund U. Age group comparability of raw accelerometer output from wrist‐ and hip‐worn monitors. Med Sci Sports Exerc. 2014;46(9):1816‐1824. [DOI] [PubMed] [Google Scholar]
- 14. Hildebrand M, Hansen BH, van Hees VT, Ekelund U. Evaluation of raw acceleration sedentary thresholds in children and adults. Scand J Med Sci Sports. 2017;27(12):1814‐1823. [DOI] [PubMed] [Google Scholar]
- 15. Rowlands AV, Rennie K, Kozarski R, et al. Children's physical activity assessed with wrist‐ and hip‐worn accelerometers. Med Sci Sports Exerc. 2014;46(12):2308. [DOI] [PubMed] [Google Scholar]
- 16. Vähä‐Ypyä H, Vasankari T, Husu P, et al. Validation of cut‐points for evaluating the intensity of physical activity with accelerometry‐based mean amplitude deviation (MAD). PLoS One. 2015;10(8):e0134813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. van Hees VT, Gorzelniak L, Dean León EC, et al. Separating movement and gravity components in an acceleration signal and implications for the assessment of human daily physical activity. PLoS One. 2013;8(4):e61691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rowlands AV, Mirkes EM, Yates T, et al. Accelerometer‐assessed physical activity in epidemiology: are monitors equivalent? Med Sci Sports Exerc. 2018;50(2):257‐265. [DOI] [PubMed] [Google Scholar]
- 19. Fairclough SJ, Noonan R, Rowlands AV, Van hees V, Knowles Z, Boddy LM. Wear compliance and activity in children wearing wrist and hip mounted accelerometers. Med Sci Sports Exerc. 2016;48(2):245‐253. [DOI] [PubMed] [Google Scholar]
- 20. Migueles J, Cadenas‐Sanchez C, Ekelund U, et al. Accelerometer data collection and processing criteria to assess physical activity and other outcomes: a systematic review and practical considerations. Sports Med. 2017;47(9):1821‐1845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Trost SG, Loprinzi PD, Moore R, Pfeiffer KA. Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc. 2011;43(7):1360‐1368. [DOI] [PubMed] [Google Scholar]
- 22. Buchan DS, McLellan G. Comparing physical activity estimates in children from hip‐worn actigraph GT3X+ accelerometers using raw and counts based processing methods. J Sports Sci. 2019;37(7):779‐787. [DOI] [PubMed] [Google Scholar]
- 23. Janssen X, Cliff DP, Reilly JJ, et al. Predictive validity and classification accuracy of ActiGraph energy expenditure equations and cut‐points in young children. PLoS One. 2013;8(11):e79124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Romanzini M, Petroski EL, Ohara D, Dourado AC, Reichert FF. Calibration of ActiGraph GT3X, actical and RT3 accelerometers in adolescents. Eur J Sport Sci. 2014;14(1):91‐99. [DOI] [PubMed] [Google Scholar]
- 25. Ortega FB, Cadenas‐Sanchez C, Lee D, Ruiz JR, Blair SN, Sui X. Fitness and fatness as health markers through the lifespan: an overview of current knowledge. Prog Prev Med (NY). 2018;3(2):e0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Veldman SLC, Paw CA, Mai JM, Altenburg TM. Physical activity and prospective associations with indicators of and development in children aged <5 years: a systematic review. Int J Behav Nutr Phys Act. 2021;18(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dumuid D, Stanford TE, Martin‐Fernández J, et al. Compositional data analysis for physical activity, sedentary time and sleep research. Stat Methods Med Res. 2018;27(12):3726‐3738. [DOI] [PubMed] [Google Scholar]
- 28. Ross R, Neeland IJ, Yamashita S, et al. Waist circumference as a vital sign in clinical practice: a consensus statement from the IAS and ICCR working group on visceral obesity. Nat Rev Endocrinol. 2020;16(3):177‐189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lehto E, Ray C, Vepsäläinen H, et al. Increased health and wellbeing in preschools (DAGIS) Study—Differences in children’s energy balance‐related behaviors (EBRBs) and in long‐term stress by parental educational level. Int J Environ Res Public Health. 2018;15(10):2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Migueles JH, Rowlands AV, Huber F, Sabia S, van Hees VT. GGIR: a research Community‐Driven open source R package for generating physical activity and sleep outcomes from multi‐day raw accelerometer data. J Meas Phys Behav. 2019;2(3):188‐196. [Google Scholar]
- 31. Cliff DP, Reilly JJ, Okely AD. Methodological considerations in using accelerometers to assess habitual physical activity in children aged 0–5 years. J Sci Med Sport. 2008;12(5):557‐567. [DOI] [PubMed] [Google Scholar]
- 32. van Hees VT, Fang Z, Langford J, et al. Autocalibration of accelerometer data for free‐living physical activity assessment using local gravity and temperature: an evaluation on four continents. J Appl Physiol (Bethesda, Md.: 1985). 2014;117(7):738‐744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. van Hees VT, Sabia S, Anderson KN, et al. A novel, open access method to assess sleep duration using a wrist‐worn accelerometer. PLoS One. 2015;10(11):e0142533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. WHO guidelines on physical activity and sedentary behaviour. Geneva: World Health Organization; 2020. Licence: CC BY‐NC‐SA 3.0 IGO.
- 35. Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut‐offs for thinness, overweight and obesity. Pediatr Obes. 2012;7(4):284‐294. doi: 10.1111/j.2047-6310.2012.00064.x [DOI] [PubMed] [Google Scholar]
- 36. Davidson R, MacKinnon J. Several tests for model specification in the presence of alternative hypotheses. Econometrica. 1981;49(3):781‐793. [Google Scholar]
- 37. Katapally TR, Muhajarine N. Towards uniform accelerometry analysis: a standardization methodology to minimize measurement bias due to systematic accelerometer wear‐time variation. J Sports Sci Med. 2014;13(2):379‐386. [PMC free article] [PubMed] [Google Scholar]
- 38. Ahmadi MN, Pavey TG, Trost SG. Machine learning models for classifying physical activity in free‐living preschool children. Sensors (Basel, Switzerland). 2020;20(16):4364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rowlands A, Edwardson C, Davies M, Khunti K, Harrington D, Yates T. Beyond cut points: accelerometer metrics that capture the physical activity profile. Med Sci Sports Exerc. 2018;50(6):1323‐1332. [DOI] [PubMed] [Google Scholar]
- 40. Hänggi JM, Phillips LRS, Rowlands AV. Validation of the GT3X ActiGraph in children and comparison with the GT1M ActiGraph. J Sci Med Sport. 2013;16(1):40‐44. [DOI] [PubMed] [Google Scholar]
- 41. Poitras VJ, Gray CE, Janssen X, et al. Systematic review of the relationships between sedentary behaviour and health indicators in the early years (0–4 years). BMC Public Health. 2017;17(Suppl 5):868‐889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Leppänen MH, Nyström CD, Henriksson P, et al. Physical activity intensity, sedentary behavior, body composition and physical fitness in 4‐year‐old children: results from the ministop trial. Int J Obes (Lond). 2016;40(7):1126‐1133. [DOI] [PubMed] [Google Scholar]
- 43. Forsum E, Flinke Carlsson E, Henriksson H, Henriksson P, Löf M. Total body fat content versus BMI in 4‐year‐old healthy Swedish children. J Obes. 2013;2013:1‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Ross R, Blair S, Arena R, et al. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation. 2016;134:e653‐e699. [DOI] [PubMed] [Google Scholar]
- 45. Crotti M, Foweather L, Rudd JR, Hurter L, Schwarz S, Boddy LM. Development of raw acceleration cut‐points for wrist and hip accelerometers to assess sedentary behaviour and physical activity in 5‐7‐year‐old children. J Sports Sci. 2020;38(9):1036‐1045. [DOI] [PubMed] [Google Scholar]
- 46. Koster A, Shiroma EJ, Caserotti P, et al. Comparison of sedentary estimates between activPAL and hip‐ and wrist‐worn ActiGraph. Med Sci Sports Exerc. 2016;48(8):1514‐1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1
Data Availability Statement
The data are not publicly available due to research ethical reasons and because the owner of the data is the Folkhälsan Research Center and not the research group. However, researchers interested in the data and materials from the DAGIS study may contact principal investigator Eva Roos, eva.roos@folkhalsan.fi.


