Abstract
The prognosis of root‐filled teeth depends not only on a successful root canal treatment but also on the restorative prognosis. This critical review discusses the advantages and limitations of various methodologies used to assess the load capacity or clinical survivability of root‐filled teeth and restorations. These methods include static loading, cyclic loading, finite element analysis and randomized clinical trials. In vitro research is valuable for preclinical screening of new dental materials or restorative modalities. It also can assist investigators or industry to decide whether further clinical trials are justified. It is important that these models present high precision and accuracy, be reproducible, and present adequate outcomes. Although in vitro models can reduce confounding by controlling important variables, the lack of clinical validation (accuracy) is a downside that has not been properly addressed. Most importantly, many in vitro studies did not explore the mechanisms of failure and their results are limited to rank different materials or treatment modalities according to the maximum load capacity. An extensive number of randomized clinical trials have also been published in the last years. These trials have provided valuable insight on the survivability of the root‐filled tooth answering numerous clinical questions. However, trials can also be affected by the selected outcome and by intrinsic and extrinsic biases. For example, selection bias, loss to follow‐up and confounding. In the clinical scenario, hypothesis‐based studies are preferred over observational and retrospective studies. It is recommended that hypothesis‐based studies minimize error and bias during the design phase.
Keywords: clinical trials, cyclic loading, finite element analysis, load capacity
INTRODUCTION
The long‐term prognosis of the root‐filled tooth relies not only on successful diagnosis, treatment planning, microbial control and symptoms management but also on the restorative treatment plan. An effective restoration of the root‐filled tooth can prevent recontamination by coronal leakage, strengthen the remaining tooth structure, protect the tooth in normal function, maintain healthy periodontal tissues among others. Failure to protect the root‐filled tooth is linked to structural and biological failures that involve the development of secondary caries, discolouration, cuspal fractures and vertical root fractures (Rivera & Walton, 2007). Cracks are always colonized by bacterial biofilms and have the potential to produce deleterious effects on the periodontal tissues (Ricucci et al., 2015). The outcome is catastrophic and irreversible if the crack extends or develops below the crestal bone leading to the inevitable loss of the root‐filled tooth (PradeepKumar et al., 2016).
Different methodologies have been used during the last decades to assess the load capacity and predict the clinical behaviour of teeth and restorations including static loading, cyclic fatigue, finite element analysis (FEA) and clinical trials. Methods to analyse the load capacity of root‐filled teeth and associated materials are not free of bias. It is essential that the reader understands the advantages and limitations of each analytical approach used to predict the biomechanical behaviour of the root‐filled teeth. In many cases, the aim of the model is not to reproduce the clinical behaviour of the restoration but to find the mechanisms that leads to the restoration's failure. In contrast, clinical trials can reveal the effect of a specific restorative procedure on the survival rate of the root‐filled tooth. However, the results may be influenced by the selected endpoint (catastrophic failure versus restoration failure) and by intrinsic biases such as loss to follow‐up, sample size, confounding variables among others. Either methodology, laboratory or clinical, presents its own limitations and biases. This critical review will discuss the advantages and limitations of the most common methodologies used to test the load capacity and survival rates of teeth and restorations including static, cyclic loading, FEA and clinical trials.
STATIC AND CYCLIC LOADING
Load capacity refers to the maximum stress or load that may be assigned on a root‐filled tooth under experimental conditions for a given time period (Ordinola Zapata & Fok, 2021). In other words, it refers to the capacity of a root‐filled tooth to perform its intended function when supporting a physiological amount of force. As previously reported (Ordinola Zapata & Fok, 2021), the term ‘fracture resistance’ is a common expression used in endodontic research, however, root‐filled teeth are complex structures of multiple irregular components such as: enamel, dentine, post (or dowel), luting agent, build‐up material, coronal bonding agent, ceramics, among others. Thus, in reality researchers report the ‘load capacity’ of the restored tooth (Figure 1).
FIGURE 1.
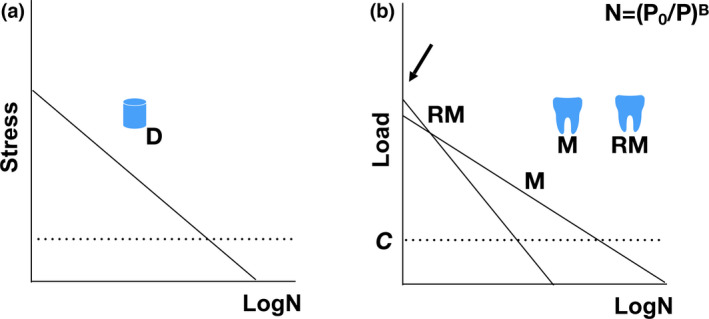
Differences between fracture resistance and load capacity. Fracture resistance is a mechanical property of a material in relation to the propagation of a pre‐existing crack. Different from fracture resistance, the load capacity is the maximum static load that a structure can sustain; it is affected by geometry and constituent materials. The testing of materials is different from the testing of structures composed of different elements. The former uses specimens of simple shapes under simple stress states. The use of cyclic fatigue data (a, D = dentine), stress versus life (N), can allow the investigator to make predictions for structures using stress analysis based on the physiological chewing force values (C). The use of static loading alone is not predictive; knowing the load capacity is not enough to predict the service life (number of cycles) of a structure because two structures can have the same load capacity but different service lives under simulated clinical conditions (b; M = molar, RM = restored molar). See how static loading (arrow) give information of only one cycle
A methodology to test the load capacity of structures is the static loading test or monotonically increasing stress test. In this cross‐sectional scenario, a single cycle is used with an increasing load until the catastrophic failure of the root‐filled tooth occurs. This type of ‘destructive’ test is able to provide the maximum load capacity (Naumann et al., 2009). A variety of studies have tried to demonstrate the effect of irrigants, intracanal dressings, different access cavities or posts designs on the load capacity of root‐filled teeth (Andreasen et al., 2002; Dotto et al., 2020; Naumann et al., 2009; Rover et al., 2017, 2020; Sabeti et al., 2018).
In the last years static loading has been used extensively to assess the load capacity of teeth that received different pulp chamber access designs. The methodological characteristics can be found in Table 1. The data revealed that the crosshead speed during the static load application had a range of 0.5–2 mm min−1 and the median speed value was 1 mm min−1. The load angulation varied between 15 and 30 degrees for molars and between 30 and 135 degrees for anterior teeth and premolars. The median number of samples per group used in these studies was 10. In all cases, teeth fractured above the maximum physiological bite force. Several controlled and uncontrolled factors can affect static load experiments including the loading position, the load angulation, presence or not of a full‐coverage restoration, presence of old or young dentine, amount of loss hard tissue, collagen degradation among others (Mireku et al., 2010).
TABLE 1.
Characteristics of included studies testing the load capacity of root‐filled teeth
| Author | Type of access cavities | Tooth type | N | Static/cyclic loading | Load direction | Crosshead speed | Parameters of cyclic loading | Results | |
|---|---|---|---|---|---|---|---|---|---|
| 2021 | Santosh et al. (2021) | Conservative & traditional & truss | Mandibular molar | 10 | Thermomechanical cycling before static loading test | 30° to the long axis of the tooth | 1 mm/min | 5 ~ 50 N, 15 Hz, 125 000 cycles | Mandibular molars with conservative and truss access cavities exhibited superior load capacity compared with traditional ones. |
| 2021 | Silva et al. (2021) | Ultraconservative & conventional | Mandibular first molar | 30 | Static | 30° to the long axis of the tooth | 1 mm/min | — | A minimally invasive access cavity did not increase the load capacity of mandibular first molars. |
| 2021 | Lima et al. (2021) | Ultraconservative & traditional | Mandibular molar | 10 | Thermomechanical cycling before static loading test | 30° to the long axis of the tooth | 1 mm/min | 86 N, 2 Hz, 300 000 cycles | No differences were observed in the load capacity between different access cavities. |
| 2021 | Maske et al. (2021) | Minimally invasive & conventional | Mandibular molar | 10 | Thermocycling before static loading test | Vertical | 0.5 mm/min | — | The type of access cavity preparation did not increase the load capacity of endodontically treated teeth. |
| 2020 | Saberi et al. (2020) | Traditional & truss | Mandibular molar | 10 | Thermocycling before static loading test | 15° to the long axis of the tooth | 1 mm/min | — | The truss access cavity enhances the load capacity of endodontically treated teeth under thermal stresses. |
| 2020 | Xia et al. (2020) | Contracted & traditional | First premolar | 10 | Thermomechanical cycling before static loading test | 135° to the long axis of the tooth | 1 mm/min | 5 ~ 50 N, 15 Hz, 500 000 cycles | Contracted access cavity could not improve the load capacity of the endodontically treated premolars. |
| 2020 | Augusto et al. (2020) | Ultraconservative & traditional | Mandibular molar | 8 | Static | 30° to the long axis of the tooth | Continuous | — | Ultraconservative access cavities did not offer any advantages in comparison with traditional cavities on the load capacity of mandibular molars. |
| 2020 | Rover et al. (2020) | Minimally invasive & traditional | Mandibular incisor | 10 | Static | 135° to the long axis of the tooth | 1 mm/min | — | The design of access cavity did not impact on the load capacity of mandibular incisors. |
| 2020 | Barbosa et al. (2020) | Conservative & traditional & truss | Mandibular molar | 10 | Static | 30° to the long axis of the tooth | Continuous | — | Conservative access cavities did not show advantage in load capacity of mandibular molars compared with traditional ones. |
| 2020 | Silva et al. (2020) | Ultraconservative & traditional | 2‐rooted maxillary premolar | 10 | Static | 30° to the long axis of the tooth | 1 mm/min | — | Ultraconservative access cavities were not associated with an increase in load capacity of 2‐rooted maxillary premolars. |
| 2020 | Sarvaiya et al. (2020) | Lingual cingulum access & lingual conventional access & Lingual incisal straight‐line access | Maxillary central incisors | 10 | Static | 130° to the long axis of the tooth | 1 mm/min | — | The load capacity was highest in the lingual conventional access group, followed by the lingual cingulum access group, and lingual incisal straight‐line access group. |
| 2019 | Abou‐Elnaga et al. (2019) | Truss & traditional | Mandibular first molar | 12 | Static | Vertical | 1 mm/min | — | The truss access cavity preparation improved the load capacity of endodontically treated teeth with mesio‐occluso‐distal cavities. |
| 2018 | Sabeti et al. (2018) | Conservative & traditional | Maxillary molar | 10 | Static | Not mentioned | Not mentioned | — | Conservative access cavity in comparison with traditional cavity had no significant impact on the load capacity of maxillary molars. |
| 2018 | Corsentino et al. (2018) | Conservative & traditional & truss | Mandibular molar | 10 | Static | 30° to the long axis of the tooth | 0.5 mm/min | — | Truss access cavity did not increase the load capacity of endodontically treated teeth in comparison with conservative and traditional ones. |
| 2018 | Özyürek et al. (2018) | Conservative & traditional | Mandibular first molar | 20 | Static | 15° to the long axis of the tooth | 1 mm/min | — | Conservative preparation did not increase the load capacity of teeth with class II cavities compared with traditional preparation. |
| 2018 | Makati et al. (2018) | Conservative & conventional | Mandibular molar | 30 | Thermocycling before static loading test | Not mentioned | 1 mm/min | — | Conservative access cavity increased load capacity of mandibular molars compared to conventional one. |
| 2017 | Rover et al. (2017) | Contracted & traditional | Maxillary first molar | 15 | Static | 30° to the long axis of the tooth | 1 mm/min | — | Contracted access cavity did not increase load capacity of maxillary first molars compared with traditional cavity. |
| 2017 | Plotino et al. (2017) | Conservative & ultraconservative & traditional | Maxillary and mandibular molars and premolars | 10 | Static | 30° to the long axis of the tooth | 0.5 mm/min | — | Teeth with traditional access showed lower load capacity than the ones prepared with conservative or ultraconservative ones. |
| 2017 | Chlup et al. (2017) | Conservative & traditional | Maxillary and mandibular premolars | 10 | Static | 30° to the long axis of the tooth | 0.5 mm/min | — | There was no statistically significant difference between conservative and traditional access cavities in maxillary and mandibular premolars. |
| 2016 | Moore et al. (2016) | Contracted & traditional | Maxillary molar | 9 | Thermomechanical cycling before static loading test | 30° to the long axis of the tooth | 1 mm/min | 5 ~ 50 N, 15 Hz, 1 000 000 cycles | Contracted access cavities did not impact biomechanical responses compared with traditional ones. |
| 2014 | Krishan et al. (2014) | Conservative & traditional | Maxillary incisors, mandibular premolars, and molars | 10/teeth type | Static | 30‐135° to the long axis of the tooth | 1 mm/min | — | Conservative access cavities conveyed a benefit of increased load capacity in mandibular molars and premolars. |
| 2011 | Taha et al. (2011) | Access cavity with no axial wall & extensive & traditional | Maxillary premolars | 10 | Static | 45° to the long axis of the tooth | 0.5 mm/min | — | Loss of axial walls of access cavities weakened teeth considerably. |
| 2007 | Nissan et al. (2007) | Labial & palatal access | Central and lateral maxillary incisors | 20/central incisors;10/lateral incisor | Static | 130° to the long axis of the tooth | 2 mm/min | — | Different endodontic accesses‐labial or palatal‐did not affect the load capacity of maxillary incisors. |
It is important to note that the static‐loading test produces failure values that are above the physiological range and is more relevant to failures caused by accidentally high forces (the average chewing motion force is 20–120 N; Yilmaz & Sadeler, 2021). The fact that biofilm colonization of dentinal cracks is commonly observed in vertical root fractures and cracked teeth cases (Ricucci et al., 2015; Rivera & Walton, 2007) suggests that crack propagation in restorative failures is a slow and gradual process. Another limitation is that stable crack growth like those observed in cracked teeth cannot occur under static loading because of the large amount of energy released in a very short time (Lin et al., 2021, 2022a).
A second technique for appraising the fatigue behaviour of a root‐filled tooth is to use the correlation between the cyclic stress amplitude and the number of cycles to failure or cyclic fatigue test (Figure 2). Fatigue failure appears due to the application of a fluctuating stress that is much lower than that required to cause a catastrophic failure during a static test with a monotonically increasing force (Arola, 2017; Campbell, 2008; Drummond, 2008; Taha et al., 2011). Nearly 90% of failures in engineering are initiated by cyclic fatigue (Campbell, 2008). In dentistry, except for traumatic dental fractures, teeth are subjected to a relatively lower but frequent mastication force every day. The cyclic nature of mastication and the deferred failure of dental hard tissues and restorations occurs after a phase of oral function indicating that an understanding of fatigue is necessary to estimate the durability of the root‐filled tooth (Arola, 2017; Mireku et al., 2010; Naumann et al., 2005). Three key elements are present in this model, the simulated mastication process (Hz), the load amplitude (N) and the number of cycles to fracture (time), being the load and the number of cycles equally important in this type of experimental model. All these factors (force, frequency and time) are considered clinically important and are useful to understand the aetiology of catastrophic failures. According to Basquin's equation (1910), the time taken or the number of cycles () required to cause failure reduces exponentially with the stress amplitude (), that is, , where is the static fracture strength and α is the fatigue life reduction factor, both of which depend on material property of the tested material (Basquin, 1910). There have been several studies on the fatigue behaviours of dentine and dental materials, for example, fibre posts and ceramics. However, very few studies have utilized this approach to analyse a root‐filled tooth restored with multiple materials (Lin et al., 2021; Mireku et al., 2010; Naumann et al., 2005). This analysis is important because some components may fail earlier than the others, and failure of the overall structure would be initiated by the component with the shortest life expectancy (i.e. dentine–composite interface), which may not necessarily be the one with the highest stress. It is important to mention that significant differences in load capacities of root–filled teeth occurred between the dynamic method and static loading (Naumann et al., 2005). For example, results based on static loading tests revealed that glass fibre is a weaker post material than titanium. A different conclusion could be obtained if dynamic loading is performed (Naumann et al., 2005).
FIGURE 2.
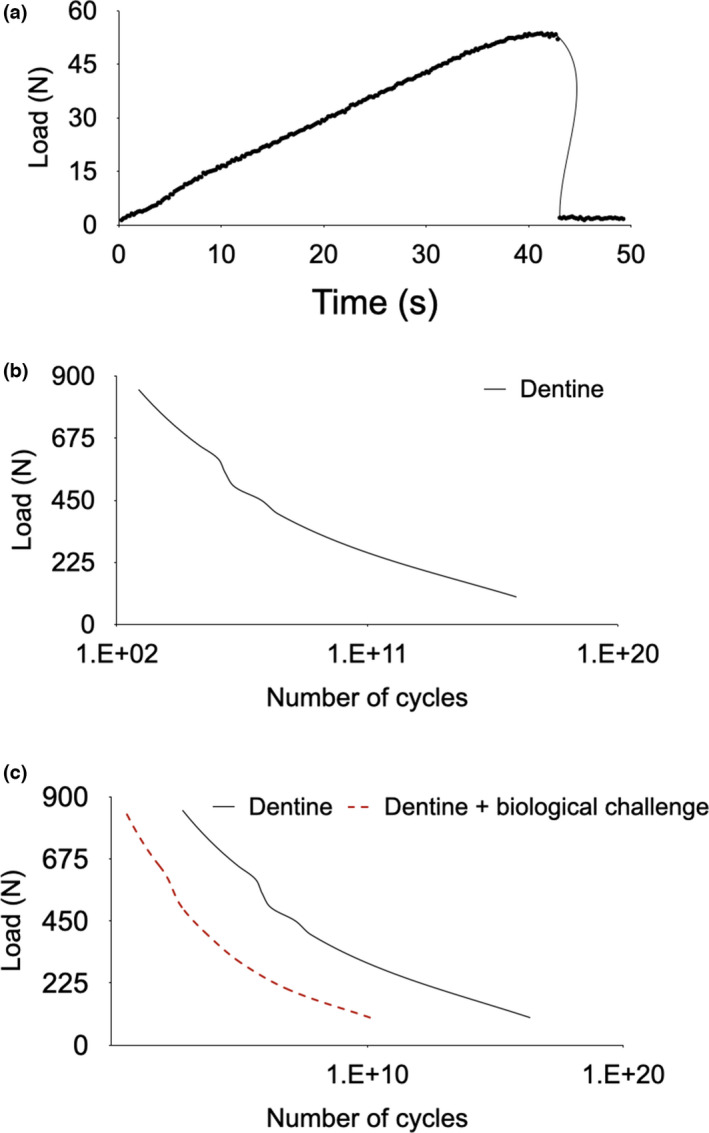
Load against time for a dentinal section using static loading (a), load against number of cycles (b) and hypothetical degradation of a material under the combined action of cyclic loading and a harmful environment (c). (Frequency: 1 Hz)
Although cyclic loading has been used to approximate the mastication process to laboratory conditions, it is rarely used in endodontic experiments because of its long duration. Accelerated cyclic fatigue models have been suggested to reduce test duration (Lin et al., 2021). However, the limitation is that the clinical stress that a tooth is receiving can be lower than those produced by the model parameters. Therefore, the number of cycles required to initiate and propagate the cracks would be much higher in the clinical scenario (Lin et al., 2022a). There are also differences in the mode of failure between cyclic and static load modalities. Fracture of restored teeth caused by static loading initiates from the locations of stress concentration near the loading point (Lin et al., 2021) while cyclic fatigue can induce longitudinal cracks below the restorative material (Lin et al., 2021, 2022a).
Recently, some studies used a combination of cyclic fatigue with static loading to fracture the samples (Lima et al., 2021; Santosh et al., 2021; Xia et al., 2020). Teeth are subjected to cyclic loading with relatively low loading amplitude (5 ~ 50 N) and higher number of cycles (100 000 ~ 500 000) to simulate oral chewing function before the static loading test (Table 1). Thermocycling was also combined with mechanical loading in some studies to better mimic thermal changes in the oral cavity (Lima et al., 2021; Santosh et al., 2021). The advantage of this method is that the aging process could also be considered when studying the load capacity of restored teeth (Lima et al., 2021).
LIMITATIONS OF STATIC AND CYCLIC LOADING
Mechanical loading can only produce restoration's fracture or interfacial degradation led by mechanical factors. It is important to notice that both static and cyclic loading use an axial load that lacks the tridimensional movement of mastication (Figure 2). Moreover, the environmental effects during testing of tooth and restorations have hardly been measured in previous laboratory studies. There are many other factors besides mechanical loading that affect the behaviour of restored teeth, like chemical and biological interactions among materials, fluids and microbial cells (Zhang et al., 2020, 2021).
To assess the reliability of in‐vitro models the differences between precision and accuracy need to be explained. In this context, precision measures how repeatable and reproducible are the results obtained by a certain test. Accuracy represents how close the measurements are to the clinical truth. In some scenarios, the role of a preclinical study is to deliver reliable and reproducible data (high precision). In this way, the investigator can be able to rank different materials and techniques in an affordable manner. However, an important step that still needs to be improved in the endodontic field is the accuracy of laboratory models. In this context, accuracy means that the laboratory model can predict the clinical performance or reproduces the results of a gold standard. It is important to recognize the differences between these concepts because a test can be precise and not accurate at the same time (Figure 3).
FIGURE 3.
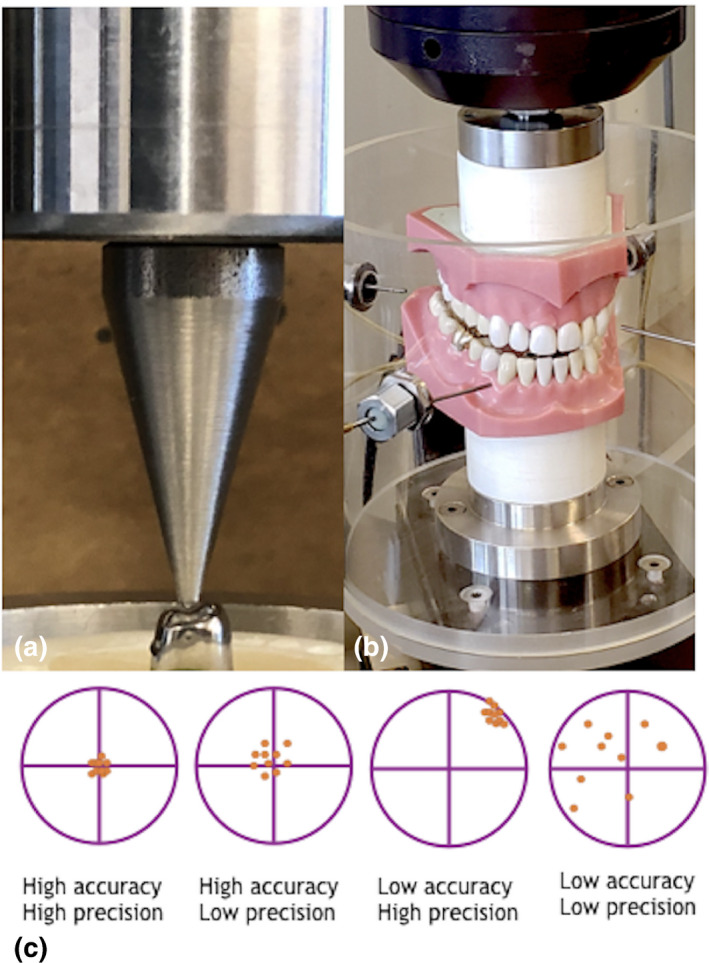
Static and dynamic loading use axial loads (a). The tridimensional movement can be obtained using an artificial mouth, observe the excursive movement produced in this model designed by Delong and Douglas (1983). This artificial oral environment has demonstrated a greater correlation with clinical wear studies; 250 000 cycles simulates 1 year of clinical wear with normal intraoral conditions (DeLong et al., 1992; Sakaguchi et al., 1986). (b) Differences between precision and accuracy (c), the best scenario is obtained when measurements provided by a test are precise and accurate (left), a model can be precise and not accurate at the same time (low accuracy, high precision). Photograph of the artificial mouth is courtesy of Minnesota Dental Research Center for Biomaterials and Biomechanics (MDRCBB)
One of the first attempts to produce an artificial mouth or ‘gold standard test’ was reported by Delong and Douglas (1983). According to these authors, the development of an oral environment requires the coordination of three areas: 1. Artificial saliva reacting with the restoration like the way natural saliva react with the same material. 2. The mastication forces must be duplicated, including excursive movements, 3. The temperature fluctuations, aeration and humidity control must mimic the conditions found in the natural environment. One additional requirement to improve accuracy is that the artificial oral conditions should stress the tested material in a mechano‐biochemical environment also known as multicomponent model (Carrera et al., 2017; Zhang et al., 2020, 2021). In the clinical scenario, dental materials and their respective bonding interfaces can worsen through polymerization shrinkage of resin composites, pH variation, biofilm colonization, wear and hydrolysis (Zhang et al., 2020, 2021). Biofilm challenge has been considered by previous authors (Carrera et al., 2017) because produces degradative products that interact accelerating the interface degradation. For example, a bonded interface in a root‐filled tooth subjected to low pH can fail faster compared to the same tooth stressed in an inert environment such as air (Orrego et al., 2017). This is relevant for direct restorations because debonding of the dentine–composite interface happens prior to longitudinal cracking or cuspal flexure in root‐filled teeth under mechanical loading (Lin et al., 2022b). While these relevant variables that contribute to the degradation of the restorative material interface or the substratum have been evaluated separately, they need to be considered concomitantly to account for synergistic effects in future studies (Orrego et al., 2017; Zhang et al., 2021). To develop a gold standard to test different restorative modalities an accelerated multicomponent model needs to predict accurately the mode and the speed of the restoration failure. This can only be accomplished if the individual components are synchronized and calibrated with clinical data (Zhang et al., 2021). The future development of new laboratory models will bring not only precise but also highly accurate results (Figure 4).
FIGURE 4.
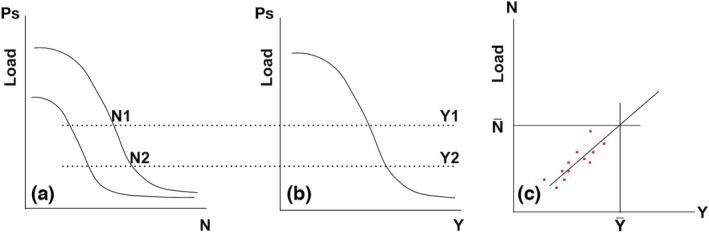
Theoretical conversion factor for laboratory time against clinical time. (a) In vitro data are obtained for a structure from accelerated cyclic loading test to obtain the number of cycles to failure. In‐vitro data N1, N2, … is compared with (b) clinical data Y1, Y2, … (i.e. number of years of service) for the same values of survival probability. (c) clinical life is plotted against the in vitro number of cycles to obtain conversion factor, allowing a prediction of the clinical life of the structure to be made. Adapted from Zhang et al. (2021)
PROBABILISTIC AND DETERMINISTIC APPROACHES
A probabilistic model includes elements of randomness. In assessing dental restorations, the investigator is unlikely to get the same exact result every time the experiment is replicated. Mineralized dental tissues and many restorative materials are relatively brittle in nature, which means that they are stronger in compression than in tension, and they may express a large deviation in their fracture strength (Kinney et al., 2003; Park et al., 2008). The materials principle states that brittle materials fail because of the unstable extension of pre‐existing flaws which are distributed at random. These pre‐existing flaws (i.e. internal cracks) can present a range of different sizes and orientations within different samples. Even highly homogeneous samples in terms of composition and dimensions (such as CAD/CAM restorations) do not all fail at the same load or at the same time when exposed to the same mechanical test. Crack size and orientation can occur randomly, which is why results from predictions for dental materials or restored teeth need to be expressed in terms of failure probability (Lin et al., 2022a). Interestingly, according to the weakest link theory the specimen with the largest flaw is not necessarily the weakest if that flaw is in a region or oriented in a direction that is not highly stressed (Fok & Chew, 2020). For example, cracks in the buccal area of root‐filled molars are not linked to catastrophic outcomes compared to cracks in the distal marginal ridge (Krell & Caplan, 2018). Thus, instead of simply designing a restoration that can last for a certain period, its probability of failure as a function of time must be specified, which is the most clinically significant variable.
FINITE ELEMENT ANALYSIS IN ENDODONTICS, DETERMINISTIC APPROACH
A deterministic model does not include elements of randomness. The same results are obtained every time the investigator runs the model with the same initial conditions. Deterministic models generate the exact same outcomes under a given set of pre‐established conditions. Thus, no statistical comparisons can be obtained. One example of this approach is the finite element analysis (FEA). This is a numerical methodology for modelling complex structures and analysing their mechanical behaviours (Trivedi, 2014). This method subdivides a physical model into small elements of finite dimensions, each of which possesses a specific geometry, structural and material properties (Choi et al., 2014). By combining this information, equilibrium relationships between the applied load and induced displacement are established by means of computer algorithms (Choi et al., 2014). In dentistry, FEA has been widely used in the fields of implantology, prosthodontics and orthodontics (van Staden et al., 2006; Sun et al., 2008). Over the recent years, increasing FEA studies have also been carried out for evaluating the stress distribution of teeth, instruments or structures in endodontics. With the development of digital imaging systems such as cone beam computed tomography and microcomputed tomography, accurate three‐dimensional anatomical models of teeth and bone could be acquired at the micrometre level (Gao et al., 2006). This provides reliable three‐dimensional models for FEA to better simulate the actual conditions of different clinical scenarios.
ADVANTAGES OF FEA
As a powerful methodology for studying the mechanical behaviour of a structure or material, FEA exhibits notable advantages. First, it helps researchers to acquire stress distributions of a complex structure under different scenarios, which is difficult to get from laboratory experiments (Jiang et al., 2018; Trivedi, 2014). Teeth subjected to endodontic treatments or restorative procedures are usually complex structures containing different components with irregular geometries; thus, the stress amplitude of each component under cyclic loading is difficult to determine. Despite micro‐computed tomography (micro‐CT) or post‐failure analysis (fractography) using scanning electron microscopy can identify the failure initiation sites, laboratory tests are incapable to record the actual stress inside the tested object, not to mention the failure sites or mechanisms (Figures 5 and 6). Thus, FEA is a valid method to address the mechanical performance as well as to interpret the mechanisms of experimental results (Lin et al., 2022a, 2022b).
FIGURE 5.
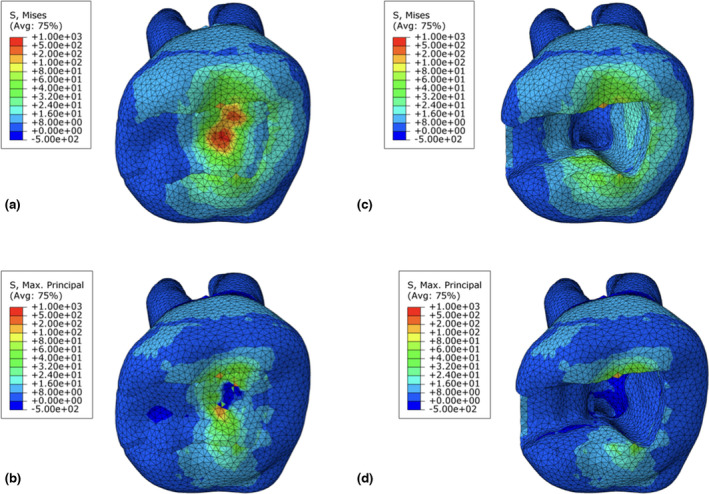
Stress distributions of restored (a, b) and unrestored (c, d) maxillary molars under 800 N compressive load. (a, c) are showing Von Mises distributions; (b, d) are showing maximum principal stress distributions. (a) indicates von Mises stress concentrations at the central fossa around the loading point. (b) shows compressive stress at the loading point and tensile stress around the loading point at the occlusal surface. There is ~8 MPa tensile stress concentration at the buccal surface. Under the same load, the distributions of von Mises and maximum principal stress are different. Maximum principal stress indicates stress normal to the plane with no shear stress on it. Positive values show tensile stress while negative show compressive. Figures (b, d) shows most tooth structures are subjecting to tensile stress under a compressive load. The pulp chamber floor is the only site that showing compressive stress. Von Mises indicates the equivalent stress based on the von Mises criterion. It has only positive values. More stress concentration area could be seen in the teeth involving the buccal cusps, which was not shown in the maximum principal stress. It indicated that the buccal cusps might not be subjected to normal tensile stress but being possibly subjected to other stresses
FIGURE 6.
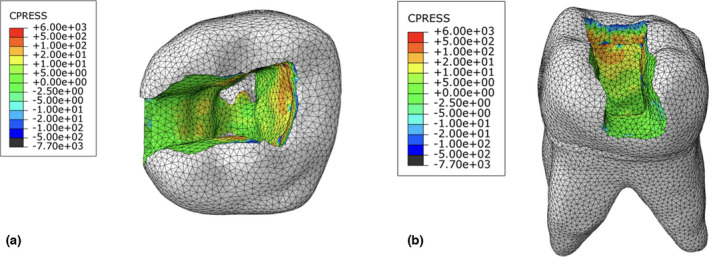
Stress distributions at dentine–composite interface from occlusal (a) and distal (b) surfaces. Both tensile and compressive stresses (MPa) concentrations are shown at the dentine–enamel junction. CPRESS (contact pressure) indicates interfacial stress, positive values indicate interfacial compressive stress while negative indicate interfacial tensile stress. The interfacial tensile stress contributes most to debonding
Finite element analysis can also focus on a particular factor, which eliminates other confounding issues that may occur in clinical practice or in the laboratory (Trivedi, 2014). Clinical or experimental studies could be challenged by many confounding factors, for example, bias from the operators or observers, variations of tooth anatomies, flaws induced during the operation, equipment calibration, among others (Brankovic et al., 2019; Leloup et al., 2001). It is difficult to precisely control every issue during the in vivo/vitro study. FEA can focus on the specific factor needed to be studied with other parameters fixed. With a precise model, right parameters and fine mesh partition, the result of FEA can replicate clinical situations or experiments (Choi et al., 2014).
Finite element analysis is also less costly and time consuming. FEA has the ability to obtain the stress magnitude and direction of the interior of an object without destroying the sample (Richert et al., 2020). A task running on a three‐dimensional model under a particular load usually takes no longer than 1 h. Though FEA often requires numerous job running and modifications of the models to get reliable results, it still consumes less time and cost compared with experimental research (Chien et al., 2021).
In FEA, stress, strain, force and displacement could be evaluated through the analysis. The most widely used parameter in dental FEA is stress. Maximum principal stress and von Mises values are most commonly reported (Table 2). Determining which parameter to use depends on the mechanical property of the material as well as the strength theory representing its damage mechanism (Trivedi, 2014). The maximum principal stress is the stress normal to the plane with no shear stress on it, with positive values representing tensile stress while negative representing compressive stress (Santos‐Filho et al., 2014). This parameter should be evaluated when the maximum principal stress criterion, that is, failure of an object, occurs at the point where its tensile maximum principal stress exceeds the limit strength of the material, is considered as failure mechanisms, which applies for most brittle materials (Wang et al., 2016a, 2016b). Tensile stress is the main cause of fractures of brittle materials. On the other hand, von Mises is a kind of equivalent stress based on the von Mises criterion that failure occurs at the point where its shear strain energy per unit volume exceeds the limit strain energy density of the material (Barsanescu & Comanici, 2017). This parameter applies mainly to the failure of ductile materials such as metals or alloys (Barsanescu & Comanici, 2017). Hence, maximum principal stress values should be evaluated in brittle structures that are more sensitive to failure by tensile stress, such as enamel or ceramics. Dentine behaves like a brittle solid under bending, whereas it also exhibits plastic behaviour under compression (Zaytsev et al., 2014). From the microscale, crack growth in the microstructured dentine is accompanied by ductile fracture of intertubular dentine and brittle cracking of the peritubular dentine (Ivancik & Arola, 2013). For this reason, both maximum principal stress and von Mises have been used in dental FEA to analyse the stress distribution in dentine.
TABLE 2.
Characteristics of included studies assessing the load capacity of root‐filled teeth using finite element analysis
| Year | Author | Type of access cavities | Tooth type | Single/Multiple loading points | Load magnitude in total | Load direction | Stress parameters | With experiments | Results |
|---|---|---|---|---|---|---|---|---|---|
| 2020 | Wang et al. (2020) | Conservative & traditional | Maxillary first molar | Multiple, four | 800 N | Vertical | Maximum principal stress | No | Conservative endodontic cavity significantly reduced the concentration of tensile stress of dentine. |
| 2020 | Saber et al. (2020) | Conservative & traditional & truss | Mandibular first molar | Multiple | 250 N | Vertical/oblique | Von Mises | No |
Conservative and truss endodontic cavity designs had higher stress concentrated at the cervical line under oblique loading. The highest VM stress was recorded for the conservative access design. |
| 2020 | Franco et al. (2020) | Conservative & conventional | Maxillary first premolar | Multiple, two | 100 N | Vertical/oblique | Displacement tensile stress | No | Conventional cavities presented higher displacement tensile stress. |
| 2020 | Guler (2020) | Ultraconservative & traditional | Maxillary first molar | Single | 480 N, 240 N | Vertical/oblique | Von Mises | No | Ultraconservative cavities had higher maximum von Mises stresses than conventional ones. |
| 2019 | Zhang et al. (2019) | Conservative & modified & traditional | Maxillary first molar | Multiple (four points) | 800 N | Vertical | Von Mises & maximum principal stress | No | The fracture resistance of an endodontically treated tooth was increased by preparing the conservative endodontic cavity. |
| 2019 | Roperto et al. (2019) | Conservative & traditional | Maxillary first premolar | Single | 100 N | Oblique | Von Mises | With fracture test | No significant differences in the fracture resistance among different endodontic cavity designs. |
| 2018 | Jiang et al. (2018) | Conservative & traditional & extended | Maxillary first molar | Single & Multiple (four points) | 800 N, 225 N | Vertical/oblique | Von Mises | No | Conservative access cavity reduced stress concentration on pericervical dentine. |
| 2018 | Allen et al. (2018) | Minimally invasive & straight‐line | Mandibular first molar | Multiple | 100 N | Vertical/oblique | Von Mises | No | A traditional endodontic access cavity may render a tooth more susceptible to fracture compared with an minimally invasive access design. |
| 2016 | Yuan et al. (2016) | Minimally invasive & straight‐line | Mandibular first molar | Single | 250 N | Vertical/oblique | Von Mises | No | Minimally invasive access preparation reduced the stress distribution in crown and cervical regions. |
Current FEA studies in endodontics have included the following categories: the influences of different access cavities, root canal enlargement and restorative procedures. Most of these studies were carried out with linear static models. Most of the FEA studies are mainly focused on the biomechanical influence of minimally invasive endodontic cavities (Table 2). Of these studies, conservative access cavities were compared with the traditional ones (Franco et al., 2020; Jiang et al., 2018; Roperto et al., 2019; Saber et al., 2020; Wang et al., 2020; Yuan et al., 2016; Zhang et al., 2019) or with truss ones (Saber et al., 2020). Most studies used the maxillary/mandibular first molar for the comparison (Jiang et al., 2018; Saber et al., 2020; Wang et al., 2020; Yuan et al., 2016; Zhang et al., 2019) while some others used premolars (Franco et al., 2020; Roperto et al., 2019). Regarding the load applied, vertical (Franco et al., 2020; Jiang et al., 2018; Saber et al., 2020; Wang et al., 2020; Yuan et al., 2016; Zhang et al., 2019) or oblique load (Franco et al., 2020; Jiang et al., 2018; Roperto et al., 2019; Saber et al., 2020; Yuan et al., 2016) with magnitudes of 80 ~ 800 N were often included in these studies. One of the studies included the extended FEA for simulating the initiation and propagation of cracks in dental hard tissues (Zhang et al., 2019). Failure probability was also evaluated in some of the FEA studies through Weibull analysis (Wang et al., 2020). Of the results analyses, only von Mises stress was evaluated in most studies (Jiang et al., 2018; Roperto et al., 2019; Saber et al., 2020; Yuan et al., 2016). Other studies analysed only maximum principal stress (Wang et al., 2020). One study included both maximum principal stress and von Mises (Zhang et al., 2019). The general conclusions of these FEA studies support the idea that conservative endodontic access cavities resulted in reduced stress concentration in dentine, especially at the cervical region (Franco et al., 2020; Jiang et al., 2018; Roperto et al., 2019; Saber et al., 2020; Wang et al., 2020; Yuan et al., 2016; Zhang et al., 2019).
Another important process of endodontic treatment is dentine removal by root canal preparation (Saber et al., 2020; Smoljan et al., 2021; Wang et al., 2020). Some other studies also investigated the susceptibility of vertical root fractures with these factors (Cheng et al., 2007; Lertchirakarn et al., 2003a, 2003b; Sathorn et al., 2005a, 2005b; Yuan et al., 2018). Basically, two kinds of loading force were considered: the vertical/oblique occlusal loads to mimic the mastication process of the tooth (Palareti et al., 2016; Saber et al., 2020; Smoljan et al., 2021; Wang et al., 2020) or the compaction force/pressure applied to the inner wall of the root canals to mimic the compaction or condensation of gutta percha during the obturation (Chai & Tamse, 2018; Palareti et al., 2016). The effects of irrigants on the stress concentrations of roots were also focused in one study (Belli et al., 2014). Another two studies built a simplified model to study the fracture resistance of radicular dentine by using transverse root sections through analytical solution, FEA and laboratory experiments (Munari et al., 2019; Xu et al., 2021).
The mostly extensive category of FEA studies in endodontics is associated with restorative procedures with direct resin composite restoration, full‐coverage crown, fibre/metal post, inlay/onlay/endocrown in root‐filled teeth with different coronal defects (Aslan et al., 2019; Ausiello et al.; 2017; Chang et al., 2015, 2018; Helal & Wang, 2019; Lin et al., 2020; Liu et al., 2014; Pinto et al., 2019; Rodrigues et al., 2020; Santos‐Filho et al., 2014; Wang et al., 2016; Wayne et al., 2014; Xiong et al., 2015; Yoon et al., 2018; Zelic et al., 2015). Similarly to FEA studies on access cavities, the FEA of restorations mostly used single‐point loading force to the modelled tooth (Liu et al., 2014; Aslan et al., 2019; Ausiello et al., 2017; Chang et al., 2018; Lin et al., 2020; Pinto et al., 2019; Santos‐Filho et al., 2014; Wang et al., 2016; Xiong et al., 2015; Yoon et al., 2018). Both axial (Aslan et al., 2019; Chang et al., 2015; Helal & Wang, 2019; Lin et al., 2020; Yoon et al., 2018) and oblique (Ausiello et al., 2017; Chang et al., 2018; Liu et al., 2014; Pinto et al., 2019; Santos‐Filho et al., 2014; Wang et al., 2016; Xiong et al., 2015; Zelic et al., 2015) loads were applied in these studies. Molars (Helal & Wang, 2019; Lin et al., 2020; Rodrigues et al., 2020; Wayne et al., 2014; Yoon et al., 2018; Yuan et al., 2016) and premolars were the most frequently used teeth for the analyses (Aslan et al., 2019; Chang et al., 2015, 2018; Liu et al., 2014; Wang et al., 2016; Xiong et al., 2015; Zelic et al., 2015).
DISADVANTAGES OF FEA
The most apparent drawback of FEA is that it greatly relies on the model and assumptions performed during the analysis (Choi et al., 2014). Hence, the model must be as precise as possible, and the parameters used should reflect the conditions of clinical practice or experiments. The type, arrangement and total number of elements also impact the reliability of FEA (Trivedi, 2014). The finer the mesh, the more accurate the result is, but the longer the analysis time. Hence, appropriate mesh size should be utilized to achieve a balance between time and accuracy. During the analysis, mesh size should be reduced for the same model until acquiring same results of the stress analysis (Choi et al., 2014). This is how convergence is achieved for the finite element model as to eliminate errors induced by the mesh size.
Whenever possible, experimental validation should be performed to verify the accuracy of FEA (Trivedi, 2014), which is not a common practice in endodontic research. Most FEA studies performed only numerical analysis, while only few also performed laboratory experiments to validate the results (Lin et al., 2022a; Roperto et al., 2019). The other limitation is that most FEA studies in dentistry are used with numerous assumptions, regarding the structure geometry, material properties, loading force, quality of bonding and boundary conditions (Trivedi, 2014). For example, dentine and enamel are anisotropic, inhomogeneous biomaterials with microstructures inside them (Thompson, 2020). However, in order to simplify the analysis, most FEA studies in dentistry assumed that those materials are isotropic, linearly elastic and homogeneous (Richert et al., 2020). FEA models also assumed a well‐bonded interface. However, it is known that perfect bonding is difficult to achieve in the endodontic scenario because of the irregular geometry, residual sodium hypochlorite contamination, shrinkage of build‐up materials, among others. Furthermore, the periodontal ligament (PDL) has a distinct stress–strain mechanical property compared to its adjacent dental hard tissues, which makes the simulation quite hard in FEA as it would easily cause convergent problems (Fill et al., 2012). Thus, PDL has been usually considered as a linearly or non‐linearly elastic material, or being ignored as it is softer than other adjacent materials (Fill et al., 2012). The boundary conditions of some models found in the literature were not clinically representative. For instance, Allen et al., (2018) fixed all the nodes of the outer surface of the roots in all directions. However, the root of a tooth should be surrounded by PDL, cortical and trabecular bone rather than fully fixed. Hence, the model could be over‐constrained by using inappropriate boundary conditions, which may result in inaccurate results of FEA.
The third limitation of traditional FEA in dentistry is that it usually assumes that every material is intact with no intrinsic defect into it (Zhang et al., 2019). Nevertheless, every object has numerous defects or porosities at the micro level, for example, voids in the composite material, preoperative cracks in the dentinal structure (Chen et al., 2008). Consequently, failure may not necessarily develop in the positions of highest stress, but in those with high stress intensity factors or low fracture toughness. As a result, some advanced finite element methods, for example, extended finite element method (XFEM), have been introduced and applied in dental research (Zhang et al., 2019). XFEM was developed to allow failure processes such as crack propagation to be modelled explicitly.
It should be noted that the maximum principal stress was evaluated in numerous studies in endodontics (Aslan et al., 2019; Ausiello et al., 2017; Chang et al., 2015, 2018; Lin et al., 2020; Liu et al., 2014; Santos‐Filho et al., 2014; Xiong et al., 2015; Yoon et al., 2018; Zelic et al., 2015), others used von Mises (Helal & Wang, 2019; Liu et al., 2014; Pinto et al., 2019; Rodrigues et al., 2020; Santos‐Filho et al., 2014; Wang et al., 2016; Wayne et al., 2014). In overall, most studies used only von Mises to evaluate the load capacity of teeth (Allen et al., 2018; Guler, 2020; Jiang et al., 2018; Roperto et al., 2019; Saber et al., 2020; Yuan et al., 2016). Though dentine also has plastic behaviours, the most common way of failure in dentine is fracture rather than plastic deformation (Ivancik & Arola, 2013). Hence, the tensile stress should be the leading/main stress causing failure under static loading based on the maximum principal stress criterion (Wang et al., 2016). As a result, FEA studies regarding load capacity of teeth, for example, designs of access cavities, should more focus on maximum principal stress, or both maximum principal stress and von Mises when also considering the plastic behaviour of dentine.
In addition, some studies have compared peak values of stresses to investigate the load capacity of different groups/designs (Franco et al., 2020; Jiang et al., 2018; Saber et al., 2020). However, the high stress might be caused by structure features of the model, for example, sharp angles, unsmooth edge/margin, among others, but not by different designs. It is biased to evaluate or compare only peak stresses. For this reason, stress distributions of different areas and median stress values should also be considered and analysed. Overall, FEA studies in endodontics has displayed a great significance in evaluating the biomechanical performance of teeth and instruments regarding the variations in structures, treatments, and materials. As a powerful tool, this method should be conducted along with laboratory experiments in the future to increase validity and reliability. Differences between both methods can be found in Table 3.
TABLE 3.
Differences between finite element analysis (FEA), static‐loading and cyclic‐loading tests
| FEA | Static‐loading tests | Cyclic‐loading tests | |
|---|---|---|---|
| Destructive | No | Most are destructive. The fracture loads are usually high, resulting in non‐restorable fractures for the tested samples. |
|
| Results acquired |
Stress, strain, load (both magnitude and direction) |
Load capacity | Load amplitude, number of cycles to failure, and time. |
| Influencing factors | Influenced by model, mesh and setting | Consistency of the operator, sample variability | Consistency of the operator, sample variability. |
| Duration of testing | Short | Short | Long, could range from several hours to several months, depending on the type of samples and aim of the study. |
| Cost | Low | Low | High |
| Advantages |
|
|
|
| Disadvantage |
|
|
|
CLINICAL STUDIES
Although mechanistic laboratory studies can allow researchers to understand complex biological or physical behaviours, laboratory results should be validated by clinical observation. It is important to acknowledge that the Oxford Centre for Evidence Based Medicine includes bench tests at the same level of evidence as expert opinion (level 5). Even though it is debatable whether laboratory data can predict clinical behaviour or not, it is important to highlight that laboratory data must be cited as basic research and not as evidence‐based medicine. In other words, clinical decisions cannot be solely made only using laboratory data even if they are aggregated into systematic reviews and meta‐analyses. Evidence‐based medicine not only considers the best available evidence but also considers patients' preferences and individual clinical experience in order to guide clinical decisions (Sackett, 1997).
THE PRIMARY OUTCOME
The final test of any new technique or material is a carefully controlled clinical trial (DeLong & Douglas, 1983). The outcome of an experimental study or clinical trial often returns a collection of endpoints rather than a single event. For example, a clinical trial comparing the efficacy of a new restorative modality to improve the survival of a root‐filled tooth against standard of care can present different outcomes. Various endpoints that could appear over the course of years are secondary caries, marginal failures, marginal discoloration, loss of anatomical form, debonding of the restoration, changes in surrounding tissues, crack development, cuspal fractures, change in the time to survival and in some cases tooth loss. The presence of multiple outcomes generates some difficulty in the analysis of the failure frequency, or the efficacy of the restorative intervention assessed. The primary endpoint is usually the most important outcome and the basis for establishing the required number of patients to be enrolled in a clinical study. Historically, catastrophic failures or unrestorable fractures of the root‐filled tooth have been used as the primary outcome in laboratory or clinical studies. Secondary outcomes are also reported and are used to evaluate additional effects of the intervention under investigation and include tooth discoloration, debonding, presence of restorable fractures, among others.
Overall, clinical studies assessing the prognosis of root‐filled teeth have utilized two main outcomes.
a. Survival: absence of catastrophic failure (failure leading to loss of the restoration or tooth); and b. Success: absence of both catastrophic failure (restoration or tooth loss) and non‐catastrophic failures.
It is also important to mention that catastrophic failures may take months or years to appear. In restorative dentistry there is a lag between the completion of the root canal treatment and the restoration placement or between the restoration completion and the occurrence of failure. This time‐lag influences the primary and secondary outcome. A restorative treatment outcome that is deemed successful at the 1‐year recall visit can be catalogued as a failure if the patient is followed‐up for a longer time such as for 3 or 5 years. For example, according to Pradeepkumar et al. (2016) vertical root fractures are detected between 2 and 5 years after root canal completion. Clinical trials assessing the prognosis of root‐filled teeth reviewed in this report have mostly utilized short to medium‐term follow‐up periods. Gbadebo et al. (2014) used the shortest follow‐up period (0.5 years), another studies used between 2 and 6 years of follow‐up (Bitter et al., 2009; Cloet et al., 2017; Ferrari et al., 2000, 2007, 2012; Karteva et al., 2018; Mannocci et al., 2002, 2005; Sarkis‐Onofre et al., 2014; Schmitter et al., 2011; Skupien et al., 2016). To date, the limited long‐term follow‐up evidence (>10 years) was derived from two randomized clinical trial (Ellner et al., 2003; Naumann et al., 2017), and three non‐randomized trials (Fokkinga et al., 2007, 2008) (Table 4) Thus, readers need to consider that short‐term outcomes may not reflect the clinical reality.
TABLE 4.
Characteristics of reviewed randomized controlled trials
| Author (Year) | Follow‐up (years) | Teeth (n) Lost to follow‐up (%) | Residual coronal structure Pre‐stratification (Y/N) | Interventions tested | Outcomes |
|---|---|---|---|---|---|
| Direct versus Indirect restorations | |||||
| Skupien et al. (2016) | 5 years |
Ant, PM, M (57); (<20%) |
At least 1‐wall present; N |
Fib‐P/Composite versus Fib‐P/Crown |
Fib‐P/Composite: Success (92%); Survival (96%) Fib‐P/Crown: Success (98%); Survival (100%) |
| Mannocci et al. (2002) | 3 years |
PM (117); (<20%) |
>2 walls; N |
Fib‐P/Composite versus Fib‐P/Crown |
Fib‐P/Composite: Success (92%) Fib‐P/Crown: Success (94%) |
| Posts versus No posts | |||||
| Karteva et al. (2018) | 1 year |
PM (35); (<20%) |
Absence of 1–2 walls; N |
Metal‐P versus Fib‐P versus No post Final restoration: Composite |
Success and survival: Rates not specified |
|
Cloet et al. (2017) |
5 years |
Ant, posterior (24‐181); (<20%) |
>2‐walls; <2‐walls; ferrule present,Y |
Cast‐PC No post Fib‐P (prefabricated) Fib‐P (custom) Final restoration: Crown |
Cast‐PC: Survival (91.2%) No post: Survival (91.7%) Fib‐P (prefabricated): Survival (91.4%) Fib‐P (custom): Survival (92.1%) |
| Ferrari et al. (2012) | 6 years |
PM (360); (<20%) |
Pre‐stratification groups: No wall; no‐ferrule No wall; ferrule present 1‐wall 2‐walls 3‐walls 4‐walls |
Fib‐P (prefabricated) versus Fib‐P (custom) versus No post Final restoration: Crown |
Fib‐P (prefab): Success (76.6%); Survival (99.1%) Fib‐P (custom): Success (61.3%); Survival (97.2%) No post: Success (42.1%); Survival (85.9%) |
| Bitter et al. (2009) | 2.5 years |
Ant, PM, M (120); (<20%) |
Pre‐stratification groups: No wall 1‐wall >2‐walls |
Fib‐P versus No post Final restoration: Composite; partial crowns for >2‐walls |
Fib‐P: Success (93%) No post: Success (90%) For No‐wall group: Fib‐P (93%); No post (69%) |
| Ferrari et al. (2007) | 2 years |
PM (240); (<20%) |
Pre‐stratification groups: No wall; no‐ferrule No wall; ferrule present 1‐wall 2‐walls 3‐walls 4‐walls |
Fib‐P versus No post Final restoration: Crown |
Fib‐P: Survival (92.5%) No post: Survival (70%) |
| Mannocci et al. (2005) | 5 years |
PM (219); (<20%) |
>2‐walls; N |
Fib‐P/composite versus no post/amalgam |
Fib‐P/Composite: Success (89%); Survival (100%) No post/Amalgam: Success (91%); Survival (94%) |
| Prefabricated versus custom cast‐PC | |||||
| Sarkis‐Onofre et al. (2014) | 3 years |
Ant, posterior (72); (20%, balanced across groups) |
No coronal wall; ferrule up to 0.5 mm; N |
Fib‐P versus Cast‐PC Final restoration: Crown |
Fib‐P: Survival (91.9%) Cast‐PC: Survival (97.1%) |
| Ellner et al. (2003) | 10 years |
Ant, PM (50); (<20%) |
At least 2 mm ferrule present; N |
Metal‐P (threaded) versus Cast‐PC (different types) Final restoration: Crown |
Metal‐P: Survival ( 80%) Cast‐PC: Survival (97%) |
| Rigid versus non‐rigid posts | |||||
| Naumann et al. (2017) | 11 years |
Ant, PM, M (91); (>20%) |
<2‐walls; ferrule present; N |
Fib‐P versus Metal‐P Final restoration: Crown |
Fib‐P: Survival (58.7%) Metal‐P: Survival (74.2%) |
| Gbadebo et al. (2014) | 0.5 years |
Ant, PM, M (40); (<20%) |
At least 2 mm ferrule present; N |
Fib‐P versus Metal‐P Final restoration: Crown |
Fib‐P: Survival (100%) Metal‐P: Survival (97.5%) |
| Schmitter et al. (2011) | 5 years |
Not specified (100); (<20%) |
At least 40% coronal loss; N |
Fib‐P versus Metal‐P Final restoration: Crown |
Fib‐P: Survival (71.8%) Metal‐P: Survival (50%) |
Abbreviations: Ant, anterior; Cast‐PC, custom cast post and core; Fib‐P, fibre post; M, molar; Metal‐P, prefabricated metal post; PM, premolar.
COHORT VERSUS RANDOMIZED CLINICAL TRIALS
A cohort study is an observational study design in which the researcher observes subjects over a period of time based on the presence or absence of an exposure, for example, presence of a crown versus a filling. The exposure has already occurred but the endpoint (secondary caries, cuspal fracture, vertical root fracture or extraction) is yet to happen. On the other hand, a randomized clinical trial is an experimental study design wherein patients are assigned randomly by a researcher to the intervention (e.g. crown) or the control group (e.g. filling) and compared overtime for differences in outcomes. Control groups can also include the standard of care. Cohort studies are intrinsically rated lower than randomized trials in the hierarchy of evidence due to higher risk of different biases (Higgins et al., 2021).
There are at least three broad types of biases encountered in clinical studies, these are bias in the selection of study participants, for example enrolling patients with favourable preoperative prognosis; information bias or bias due to differences in the way information is obtained (lack of precision); and confounding or presence of prognostic factors (e.g. age, unrecorded amount of ferrule, parafunction, among others) associated with both the exposure and the outcome and directly involved in the causal pathway. Confounders can bias the effect of the intervention or exposure on the final outcome. Other types of biases are related to missing outcome data (attrition or loss to follow‐up) and bias in selection of the reported result (Higgins et al., 2021).
One way to reduce the effect of confounders is to use stratification. Stratification is a procedure in which both treatment and control groups are matched based on suspected confounders either a priori, that is, during the design phase of the clinical trial or during statistical analysis (Kernan et al., 1999). When stratification is done a priori or during the randomization process, it is termed as pre‐stratification. The goal of pre‐stratification is to prevent disproportion of known confounding factors (Kernan et al., 1999) such as number of residual walls, presence of ferrule, type of tooth, age, etc. For example, having more anterior teeth in one group compared to the other, or significant inter‐group differences between the age of participants can affect the results. Among 13 randomized clinical trials in the subject (Table 4), only four studies pre‐stratified the amount of residual tooth structure (Bitter et al., 2009; Cloet et al., 2017; Ferrari et al., 2007, 2012) (Table 4)
Though randomized clinical trials are rated higher than cohort studies, they still are at risk of biases. Risk of bias in randomized trials are broadly grouped according to issues arising in five different domains – issues with the randomization process, deviations from intended interventions, missing outcome data, errors in measurement, and selective reporting of results (Higgins et al., 2021).
An important factor that can affect the power of a clinical trial is missing outcome data or losses to follow‐up. Traditionally, the internal validity of study findings most likely will be affected if the loss to follow‐up proportion is above 20%. The hierarchy of evidence for making treatment guidelines (Oxford Centre for Evidence‐Based Medicine, 2009) includes systematic review of well‐designed large randomized clinical trials (with homogeneity), and randomized clinical trials with narrow confidence interval. Among the clinical studies included in this review, all the non‐randomized trials (observational studies) had substantial loss to follow‐up (>50%) (Table 5). On the other hand, only one randomized trial had a 20% loss to follow‐up. Although formal risk of bias calculation of individual studies was not conducted in this review, most of the included randomized clinical trials in the topic were judged to be high or unclear risk of bias according to numerous systematic reviews that combined findings from these studies (Batista et al., 2019; Bolla et al., 2007; Marchionatti et al., 2017; Naumann et al., 2018; Sarkis‐Onofre et al., 2017; Schwendicke and Stolpe, 2017, 2018; Sequeira‐Byron et al., 2015; Zhu et al. 2015). Some limitations were observed among these systematic reviews or meta‐analysis as well, for example, non‐randomized clinical trials were included in the analysis (Naumann et al., 2018; Sarkis‐Onofre et al., 2017; Shu et al., 2018), overlapping information is also common, the findings of Mannocci et al. (2002), Fokkinga et al. (2007), Bitter et al. (2009) and Gbadebo et al. (2014) have been reproduced in at least two systematic reviews or meta‐analysis.
TABLE 5.
Characteristics of reviewed non‐randomized controlled trials
| Author (Year) | Follow‐up (years) |
Teeth (n) Lost to follow‐up (%) |
Residual coronal structure Pre‐stratification (Y/N) |
Interventions tested | Outcomes |
|---|---|---|---|---|---|
| Fokkinga et al. (2008) | 17 years |
Ant, PM, M (98); (>50%) |
Presence of >75% tooth structure (at least 1 mm thickness and height); 1–2 mm ferrule present; N |
Metal‐P versus No post Final restoration: Composite |
Metal‐P: Tooth survival (75%); Restoration survival (57%) No post: Tooth survival (82%); Restoration survival (49%) |
|
Fokkinga et al. (2007) (Substantial dentinal height) |
17 years |
Ant, PM, M (196); (>50%) |
Presence of >75% tooth structure (at least 1 mm thickness and height); 1–2 mm ferrule present; N |
Metal‐P versus Cast‐PC versus No post Final restoration: Crown |
Metal‐P: Tooth survival (92%); Restoration survival (84%) Cast‐PC: Tooth survival (92%); Restoration Survival (85%) No post: Tooth survival (83%); Restoration survival (88%) |
|
Fokkinga et al. (2007) (Minimal dentinal height) |
17 years |
Ant, PM, M (111); (>50%) |
<75% tooth structure (at least 1 mm height); or 1–2 mm ferrule absent; N |
Metal‐P versus Cast‐PC Final restoration: Crown |
Metal‐P: Tooth survival (83%); Restoration survival (71%) Cast‐PC: Tooth survival (92%); Restoration survival (84%) |
Abbreviations: Ant: anterior; Cast‐PC: custom cast post and core; M: molar; Metal‐P: prefabricated metal post; PM: premolar.
LIMITATIONS OF THE CLINICAL EVIDENCE
Numerous inconsistencies of effect estimates have been reported across different prospective studies which made summarizing the conclusions of clinical trials difficult. Overall, studies are heterogeneous regarding important baseline factors such as different types of anatomy (e.g. anterior, bicuspid and molar) or different amounts of residual tooth structure (e.g. presence/absence of ferrule or number of dentinal walls). Additional heterogeneity was observed due to the presence of different post systems/materials or differences in clinical procedures and luting cements. Furthermore, clinical studies have assessed outcomes using different definitions (restoration success versus restoration survival versus tooth survival). This highlights the need for more well‐designed randomized clinical trials with consistent protocols and longer follow‐up periods to increase our confidence in the findings.
CONCLUDING REMARKS
Laboratory models to test the load capacity and durability of root‐filled teeth are necessary for the development and test of new restorative modalities. Ideally, laboratory data should be able to predict the clinical behaviour and life expectancy of the root‐filled tooth. However, to date in vitro models present questionable accuracy and the results depend on the model's assumptions. Most importantly, many in vitro studies do not explore the mechanisms of failure and their results are limited to rank different materials or treatment modalities according to the maximum load capacity. In many cases, the load capacity does not represent physiological values and the results are more relevant to failures caused by accidentally high forces. Among different methods, cyclic fatigue and FEA are powerful tools that need to be used in conjunction to understand the mechanisms of failure of restorative procedures. Although, the majority of deterministic models can give insights about the failure process, these models also present limitations and are based on assumptions that require experimental validation. In the clinical scenario, mechanistic and hypothesis‐based prospective studies are preferred over observational studies. These clinical studies should minimize error and bias during the design phase.
ACKNOWLEDGEMENTS
The authors deny any conflicts of interest related to this study. Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health Award Number UL1‐TR002494. This manuscript is based on a previous editorial letter “Research that matters: debunking the myth of the fracture resistance of root filled teeth” (2021) International Endodontic Journal 54, 297‐300. Authors would like to thank Alex Fok PhD for his helpful advice and feedback.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare that are relevant to the content of this article.
ETHICS STATEMENT
The article is a review and did not involve human participants.
AUTHOR CONTRIBUTION
Ronald Ordinola‐Zapata: Conceptualization, writing, editing. Fei Lin: Conceptualization, writing, editing. Sanket Nagarkar: Writing, editing. Jorge Perdigão: Writing, editing.
Ordinola‐Zapata, R. , Lin, F. , Nagarkar, S. & Perdigão, J. (2022) A critical analysis of research methods and experimental models to study the load capacity and clinical behaviour of the root filled teeth. International Endodontic Journal, 55(Suppl. 2), 471–494. Available from: 10.1111/iej.13722
REFERENCES
- Abou‐Elnaga, M.Y. , Alkhawas, M.B.A.M. , Kim, H.C. & Refai, A.S. (2019) Effect of truss access and artificial truss restoration on the fracture resistance of endodontically treated mandibular first molars. Journal of Endodontics, 45, 813–817. [DOI] [PubMed] [Google Scholar]
- Allen, C. , Meyer, C. , Yoo, E. , Vargas, J. , Liu, Y. & Jalali, P. (2018) Stress distribution in a tooth treated through minimally invasive access compared to one treated through traditional access: a finite element analysis study. Journal of Conservative Dentistry, 21, 505–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreasen, J.O. , Farik, B. & Munksgaard, E.C. (2002) Long‐term calcium hydroxide as a root canal dressing may increase risk of root fracture. Dental Traumatology, 18, 134–137. [DOI] [PubMed] [Google Scholar]
- Arola, D. (2017) Fatigue testing of biomaterials and their interfaces. Dental Materials, 33, 367–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aslan, T. , Üstün, Y. & Esim, E. (2019) Stress distributions in internal resorption cavities restored with different materials at different root levels: a finite element analysis study. Australian Endodontic Journal, 45, 64–71. [DOI] [PubMed] [Google Scholar]
- Augusto, C.M. , Barbosa, A.F.A. , Guimaraes, C.C. , Lima, C.O. , Ferreira, C.M.A. , Sassone, L.M. et al. (2020) A laboratory study of the impact of ultraconservative access cavities and minimal root canal tapers on the ability to shape canals in extracted mandibular molars and their fracture resistance. International Endodontic Journal, 53, 1516–1529. [DOI] [PubMed] [Google Scholar]
- Ausiello, P. , Ciaramella, S. , Martorelli, M. , Lanzotti, A. , Zarone, F. , Watts, D.C. et al. (2017) Mechanical behavior of endodontically restored canine teeth: effects of ferrule, post material and shape. Dental Materials, 33, 1466–1472. [DOI] [PubMed] [Google Scholar]
- Barbosa, A.F.A. , Silva, E.J.N.L. , Coelho, B.P. , Ferreira, C.M.A. , Lima, C.O. & Sassone, L.M. (2020) The influence of endodontic access cavity design on the efficacy of canal instrumentation, microbial reduction, root canal filling and fracture resistance in mandibular molars. International Endodontic Journal, 53, 1666–1679. [DOI] [PubMed] [Google Scholar]
- Barsanescu, P.D. & Comanici, A.M. (2017) von Mises hypothesis revised. Acta Mechanica, 228, 433–446. [Google Scholar]
- Basquin, O.H. (1910) The exponential law of endurance tests. Proceedings of the American Society for Testing and Materials, 10, 625–630. [Google Scholar]
- Batista, V.E.S. , Bitencourt, S.B. , Bastos, N.A. , Pellizzer, E.P. , Goiato, M.C. & Dos Santos, D.M. (2019) Influence of the ferrule effect on the failure of fiber‐reinforced composite post‐and‐core restorations: a systematic review and meta‐analysis. Journal of Prosthetic Dentistry, 123, 239–245. [DOI] [PubMed] [Google Scholar]
- Belli, S. , Eraslan, O. , Eraslan, O. , Eskitascioglu, M. & Eskitascioglu, G. (2014) Effects of NaOCl, EDTA and MTAD when applied to dentine on stress distribution in post‐restored roots with flared canals. International Endodontic Journal, 47, 1123–1132. [DOI] [PubMed] [Google Scholar]
- Bitter, K. , Noetzel, J. , Stamm, O. , Vaudt, J. , Meyer‐Lueckel, H. , Neumann, K. et al. (2009) Randomized clinical trial comparing the effects of post placement on failure rate of postendodontic restorations: preliminary results of a mean period of 32 months. Journal of Endodontics, 35, 1477–1482. [DOI] [PubMed] [Google Scholar]
- Bolla, M. , Muller‐Bolla, M. , Borg, C. , Lupi‐Pegurier, L. , Laplanche, O. & Leforestier, E. (2007) Root canal posts for the restoration of root filled teeth. Cochrane Database of Systematic Reviews, 24, CD004623. [DOI] [PubMed] [Google Scholar]
- Brankovic, M. , Kardys, I. , Steyerberg, E.W. , Lemeshow, S. , Markovic, M. , Rizopoulos, D. et al. (2019) Understanding of interaction (subgroup) analysis in clinical trials. European Journal of Clinical Investigation, 49, 1–9. [DOI] [PubMed] [Google Scholar]
- Campbell, F.C. (2008) Fatigue. In: Campbell, F.C. (Ed.) Elements of metallurgy and engineering alloys. Cleveland, Ohio: ASM International, pp. 243–264. [Google Scholar]
- Carrera, C.A. , Li, Y. , Chen, R. , Aparicio, C. , Fok, A. & Rudney, J. (2017) Interfacial degradation of adhesive composite restorations mediated by oral biofilms and mechanical challenge in an extracted tooth model of secondary caries. Journal of Dentistry, 66, 62–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chai, H. & Tamse, A. (2018) Vertical root fracture in buccal roots of bifurcated maxillary premolars from condensation of Gutta‐percha. Journal of Endodontics, 44, 1159–1163. [DOI] [PubMed] [Google Scholar]
- Chang, Y.H. , Lee, H. & Lin, C.L. (2015) Early resin luting material damage around a circular fiber post in a root canal treated premolar by using micro‐computerized tomographic and finite element sub‐modeling analyses. Journal of the Mechanical Behavior of Biomedical Materials, 51, 184–193. [DOI] [PubMed] [Google Scholar]
- Chang, Y.H. , Wang, H.W. , Lin, P.H. & Lin, C.L. (2018) Evaluation of early resin luting cement damage induced by voids around a circular fiber post in a root canal treated premolar by integrating micro‐CT, finite element analysis and fatigue testing. Dental Materials, 34, 1082–1088. [DOI] [PubMed] [Google Scholar]
- Chen, P.Y. , Lin, A.Y.M. , Lin, Y.S. , Seki, Y. , Stokes, A.G. , Peyras, J. et al. (2008) Structure and mechanical properties of selected biological materials. Journal of the Mechanical Behavior of Biomedical Materials, 1, 208–226. [DOI] [PubMed] [Google Scholar]
- Cheng, R. , Zhou, X.D. , Liu, Z. & Hu, T. (2007) Development of a finite element analysis model with curved canal and stress analysis. Journal of Endodontics, 33, 727–731. [DOI] [PubMed] [Google Scholar]
- Chien, P.Y.H. , Walsh, L.J. & Peters, O.A. (2021) Finite element analysis of rotary nickel‐titanium endodontic instruments: a critical review of the methodology. European Journal of Oral Sciences, 129, e12802. [DOI] [PubMed] [Google Scholar]
- Chlup, Z. , Žižka, R. , Kania, J. & Přibyl, M. (2017) Fracture behaviour of teeth with conventional and mini‐invasive access cavity designs. Journal of the European Ceramic Society, 37, 4423–4429. [Google Scholar]
- Choi, A.H. , Conway, R.C. & Ben‐Nissan, B. (2014) Finite‐element modeling and analysis in nanomedicine and dentistry. Nanomedicine, 9, 1681–1695. [DOI] [PubMed] [Google Scholar]
- Cloet, E. , Debels, E. & Naert, I. (2017) Controlled clinical trial on the outcome of glass fiber composite cores versus wrought posts and cast cores for the restoration of endodontically treated teeth: a 5‐year follow‐up study. International Journal of Prosthodontics, 30, 71–79. [DOI] [PubMed] [Google Scholar]
- Corsentino, G. , Pedullà, E. , Castelli, L. , Liguori, M. , Spicciarelli, V. , Martignoni, M. et al. (2018) Influence of access cavity preparation and remaining tooth substance on fracture strength of endodontically treated teeth. Journal of Endodontics, 44, 1416–1421. [DOI] [PubMed] [Google Scholar]
- DeLong, R. & Douglas, W.H. (1983) Development of an artificial oral environment for the testing of dental restoratives: bi‐axial force and movement control. Journal of Dental Research, 62, 32–36. [DOI] [PubMed] [Google Scholar]
- DeLong, R. , Pintado, M.R. & Douglas, W.H. (1992) The wear of enamel opposing shaded ceramic restorative materials: an in vitro study. The Journal of Prosthetic Dentistry, 68, 42–48. [DOI] [PubMed] [Google Scholar]
- Dotto, L. , Sarkis Onofre, R. , Bacchi, A. & Rocha Pereira, G.K. (2020) Effect of root canal irrigants on the mechanical properties of endodontically treated teeth: a scoping review. Journal of Endodontics, 46, 596–604. [DOI] [PubMed] [Google Scholar]
- Drummond, J.L. (2008) Degradation, fatigue, and failure of resin dental composite materials. Journal of Dental Research, 87, 710–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellner, S. , Bergendal, T. & Bergman, B. (2003) Four post‐and‐core combinations as abutments for fixed single crowns: a prospective up to 10‐year study. International Journal of Prosthodontics, 16, 249–254. [PubMed] [Google Scholar]
- Ferrari, M. , Cagidiaco, M.C. , Grandini, S. , De Sanctis, M. & Goracci, C. (2007) Post placement affects survival of endodontically treated premolars. Journal of Dental Research, 86, 729–734. [DOI] [PubMed] [Google Scholar]
- Ferrari, M. , Vichi, A. & Garcia‐Godoy, F. (2000) Clinical evaluation of fiber‐reinforced epoxy resin posts and cast post and cores. American Journal of Dentistry, 13, 15b–18b. [PubMed] [Google Scholar]
- Ferrari, M. , Vichi, A. , Fadda, G.M. , Cagidiaco, M.C. , Tay, F.R. , Breschi, L. et al. (2012) A randomized controlled trial of endodontically treated and restored premolars. Journal of Dental Research, 91, S72–S78. [DOI] [PubMed] [Google Scholar]
- Fill, T.S. , Toogood, R.W. , Major, P.W. & Carey, J.P. (2012) Analytically determined mechanical properties of, and models for the periodontal ligament: critical review of literature. Journal of Biomechanics, 45, 9–16. [DOI] [PubMed] [Google Scholar]
- Fok, A. & Chew, H. (2020) Mechanical failure of dental restorations: The weakest‐link theory. In: Fok, A. & Chew, H. (Eds.) Mathematical Models for Dental Materials Research, 1st edition. Springer Nature: Cham, pp. 47–53. [Google Scholar]
- Fokkinga, W.A. , Kreulen, C.M. , Bronkhorst, E.M. & Creugers, N.H. (2007) Up to 17‐year controlled clinical study on post‐and‐cores and covering crowns. Journal of Dentistry, 35, 778–786. [DOI] [PubMed] [Google Scholar]
- Fokkinga, W.A. , Kreulen, C.M. , Bronkhorst, E.M. & Creugers, N.H. (2008) Composite resin core‐crown reconstructions: an up to 17‐year follow‐up of a controlled clinical trial. International Journal of Prosthodontics, 21, 109–1915. [PubMed] [Google Scholar]
- Franco, A.B.G. , Franco, A.G. , de Carvalho, G.A.P. , Ramos, E.V. , Amorim, J.C.F. & de Martim, A.S. (2020) Influence of conservative endodontic access and the osteoporotic bone on the restoration material adhesive behavior through finite element analysis. Journal of Materials Science: Materials in Medicine, 31, 2–7. [DOI] [PubMed] [Google Scholar]
- Gao, J. , Xu, W. & Ding, Z. (2006) 3D finite element mesh generation of complicated tooth model based on CT slices. Computer Methods and Programs in Biomedicine, 82, 97–105. [DOI] [PubMed] [Google Scholar]
- Gbadebo, O.S. , Ajayi, D.M. , Oyekunle, O.O. & Shaba, P.O. (2014) Randomized clinical study comparing metallic and glass fiber post in restoration of endodontically treated teeth. Indian Journal of Dental Research, 25, 58–63. [DOI] [PubMed] [Google Scholar]
- Guler, M.S. (2020) Effect of access cavity designs on stress distribution. Emerging Materials Research, 9, 1–6. [Google Scholar]
- Helal, M.A. & Wang, Z. (2019) Biomechanical assessment of restored mandibular molar by endocrown in comparison to a glass fiber post‐retained conventional crown: 3D finite element analysis. Journal of Prosthodontics, 28, 988–996. [DOI] [PubMed] [Google Scholar]
- Higgins, J.P.T. , Savović, J. , Page, M.J. , Elbers, R.G. & Sterne, J.A.C. (2021) Chapter 8: assessing risk of bias in a randomized trial. In: Higgins, J.P.T. , Thomas, J. , Chandler, J. , Cumpston, M. , Li, T. , Page, M.J. & Welch, V.A. (Eds.) Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021). Cochrane. Available from: www.training.cochrane.org/handbook [Google Scholar]
- Ivancik, J. & Arola, D.D. (2013) The importance of microstructural variations on the fracture toughness of human dentin. Biomaterials, 34, 864–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang, Q. , Huang, Y. , Tu, X.R. , Li, Z. , He, Y. & Yang, X. (2018) Biomechanical properties of first maxillary molars with different endodontic cavities: a finite element analysis. Journal of Endodontics, 44, 1283–1288. [DOI] [PubMed] [Google Scholar]
- Karteva, E.G. , Manchorova, N.A. , Vladimirov, S.B. & Keskinova, D.A. (2018) Clinical assessment of endodontically treated teeth, restored with or without radicular posts. Folia Medica, 60, 291–299. [DOI] [PubMed] [Google Scholar]
- Kernan, W.N. , Viscoli, C.M. , Makuch, R.W. , Brass, L.M. & Horwitz, M.I. (1999) Stratified randomized for clinical trials. Journal of Clinical Epidemiology, 52, 19–26. [DOI] [PubMed] [Google Scholar]
- Kinney, J.H. , Marshall, S.J. & Marshall, G.W. (2003) The mechanical properties of human dentin: a critical review and re‐evaluation of the dental literature. Critical Reviews in Oral Biology & Medicine, 14, 13–29. [DOI] [PubMed] [Google Scholar]
- Krell, K.V. & Caplan, D. (2018) 12‐month succes of cracked teeth treated with orthograde root canal treatment. Journal of Endodontics, 44, 543–548. [DOI] [PubMed] [Google Scholar]
- Krishan, R. , Paqué, F. , Ossareh, A. , Kishen, A. , Dao, T. & Friedman, S. (2014) Impacts of conservative endodontic cavity on root canal instrumentation efficacy and resistance to fracture assessed in incisors, premolars, and molars. Journal of Endodontics, 40, 1160–1166. [DOI] [PubMed] [Google Scholar]
- Leloup, G. , D'Hoore, W. , Bouter, D. , Degrange, M. & Vreven, J. (2001) Meta‐analytical review of factors involved in dentin adherence. Journal of Dental Research, 80, 1605–1614. [DOI] [PubMed] [Google Scholar]
- Lertchirakarn, V. , Palamara, J.E.A. & Messer, H.H. (2003a) Finite element analysis and strain‐gauge studies of vertical root fracture. Journal of Endodontics, 29, 529–534. [DOI] [PubMed] [Google Scholar]
- Lertchirakarn, V. , Palamara, J.E.A. & Messer, H.H. (2003b) Patterns of vertical root fracture: factors affecting stress distribution in the root canal. Journal of Endodontics, 29, 523–528. [DOI] [PubMed] [Google Scholar]
- Lima, C.O. , Barbosa, A.F.A. , Ferreira, C.M. , Ferretti, M.A. , Aguiar, F.H.B. , Lopes, R.T. et al. (2021) Influence of ultraconservative access cavities on instrumentation efficacy with XP‐endo Shaper and Reciproc, filling ability and load capacity of mandibular molars subjected to thermomechanical cycling. International Endodontic Journal, 54, 1383–1393. [DOI] [PubMed] [Google Scholar]
- Lin, F. , Ordinola‐Zapata, R. , Xu, H. , Heo, Y.C. & Fok, A. (2021) Laboratory simulation of longitudinally cracked teeth using the step‐stress cyclic loading method. International Endodontic Journal, 54, 1638–1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, F. , Ordinola‐Zapata, R. , Ye, N. , Xu, H. & Fok, A. (2022a) Fatigue analysis of restored teeth longitudinally cracked under cyclic loading. Dental Materials, 38, 204–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, F. , Ordinola‐Zapata, R. , Fok, A. & Lee, R. (2022b) Influence of minimally invasive endodontic access cavities and bonding status of resin composites on the mechanical property of endodontically treated teeth: a finite element study. Dental Materials, 38, 242–250. [DOI] [PubMed] [Google Scholar]
- Lin, J. , Lin, Z. & Zheng, Z. (2020) Effect of different restorative crown design and materials on stress distribution in endodontically treated molars: a finite element analysis study. BMC Oral Health, 20, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, S. , Liu, Y. , Xu, J. , Rong, Q. & Pan, S. (2014) Influence of occlusal contact and cusp inclination on the biomechanical character of a maxillary premolar: a finite element analysis. Journal of Prosthetic Dentistry, 112, 1238–1245. [DOI] [PubMed] [Google Scholar]
- Makati, D. , Shah, N.C. , Brave, D. , Rathore, V.P.S. , Bhadra, D. & Dedania, M.S. (2018) Evaluation of remaining dentin thickness and fracture resistance of conventional and conservative access and biomechanical preparation in molars using cone‐beam computed tomography: an in vitro study. Journal of Conservative Dentistry, 21, 324–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannocci, F. , Bertelli, E. , Sherriff, M. , Watson, T.F. & Ford, T.R. (2002) Three‐year clinical comparison of survival of endodontically treated teeth restored with either full cast coverage or with direct composite restoration. Journal of Prosthetic Dentistry, 88, 297–301. [DOI] [PubMed] [Google Scholar]
- Mannocci, F. , Qualtrough, A.J. , Worthington, H.V. , Watson, T.F. & Pitt Ford, T.R. (2005) Randomized clinical comparison of endodontically treated teeth restored with amalgam or with fiber posts and resin composite: five‐year results. Operative Dentistry, 30, 9–15. [PubMed] [Google Scholar]
- Marchionatti, A.M.E. , Wandscher, V.F. , Rippe, M.P. , Kaizer, O.B. & Valandro, L.F. (2017) Clinical performance and failure modes of pulpless teeth restored with posts: a systematic review. Brazilian Oral Research, 31, e64. [DOI] [PubMed] [Google Scholar]
- Maske, A. , Weschenfelder, V.M. , Soares Grecca Vilella, F. , Burnett Junior, L.H. & de Melo, T.A.F. (2021) Influence of access cavity design on fracture strength of endodontically treated lower molars. Australian Endodontic Journal, 47, 5–10. [DOI] [PubMed] [Google Scholar]
- Mireku, A.S. , Romberg, E. , Fouad, A.F. & Arola, D. (2010) Vertical fracture of root filled teeth restored with posts: the effect of patient age and dentine thickness. International Endodontic Journal, 43, 218–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore, B. , Verdelis, K. , Kishen, A. , Dao, T. & Friedman, S. (2016) Impacts of contracted endodontic cavities on instrumentation efficacy and biomechanical responses in maxillary molars. Journal of Endodontics, 42, 1779–1783. [DOI] [PubMed] [Google Scholar]
- Munari, L.S. , Bowles, W.R. & Fok, A.S.L. (2019) Relationship between canal enlargement and fracture load of root dentin sections. Dental Materials, 35, 818–824. [DOI] [PubMed] [Google Scholar]
- Naumann, M. , Metzdorf, G. , Fokkinga, W. , Watzke, R. , Sterzenbach, G. , Bayne, S. et al. (2009) Influence of test parameters on in vitro fracture resistance of post‐endodontic restorations: a structured review. Journal of Oral Rehabilitation, 36, 299–312. [DOI] [PubMed] [Google Scholar]
- Naumann, M. , Schmitter, M. , Frankenberger, R. & Krastl, G. (2018) "Ferrule comes first. Post is second!" Fake news and alternative facts? A systematic review. Journal of Endodontics, 44, 212–219. [DOI] [PubMed] [Google Scholar]
- Naumann, M. , Sterzenbach, G. & Proschel, P. (2005) Evaluation of load testing of postendodontic restorations in vitro: linear compressive loading, gradual cyclic loading and chewing simulation. Journal of Biomedical Material Research Part B applied Biomaterials, 74B, 829–834. [DOI] [PubMed] [Google Scholar]
- Naumann, M. , Sterzenbach, G. , Dietrich, T. , Bitter, K. , Frankenberger, R. & von Stein‐Lausnitz, M. (2017) Dentin‐like versus rigid endodontic post: 11‐year randomized controlled pilot trial on no‐wall to 2‐wall defects. Journal of Endodontics, 43, 1770–1775. [DOI] [PubMed] [Google Scholar]
- Nissan, J. , Zukerman, O. , Rosenfelder, S. , Barnea, E. & Shifman, A. (2007) Effect of endodontic access type on the resistance to fracture of maxillary incisors. Quintessence International, 38, e364–e367. [PubMed] [Google Scholar]
- Ordinola‐Zapata, R. & Fok, A.S.L. (2021) Research that matters: debunking the myth of the “fracture resistance” of root filled teeth. International Endodontic Journal, 54, 297–300. [DOI] [PubMed] [Google Scholar]
- Orrego, S. , Melo, M.A. , Lee, S.H. , Xu, H.H.K. & Arola, D.D. (2017) Fatigue of human dentin by cyclic loading and during oral biofilm challenge. Journal of Biomedical Material Research Part B Applied Biomaterials, 105, 1978–1985. [DOI] [PubMed] [Google Scholar]
- Oxford Centre for Evidence‐Based Medicine. Available at: https://www.cebm.ox.ac.uk/resources/levels‐of‐evidence/oxford‐centre‐for‐evidence‐based‐medicine‐levels‐of‐evidence‐march‐2009. Accessed March 2022.
- Özyürek, T. , Ülker, Ö. , Demiryürek, E.Ö. & Yılmaz, F. (2018) The effects of endodontic access cavity preparation design on the fracture strength of endodontically treated teeth: traditional versus conservative preparation. Journal of Endodontics, 44, 800–805. [DOI] [PubMed] [Google Scholar]
- Palareti, G. , Legnani, C. , Cosmi, B. , Antonucci, E. , Erba, N. , Poli, D. et al. (2016) Comparison between different D‐Dimer cutoff values to assess the individual risk of recurrent venous thromboembolism: analysis of results obtained in the DULCIS study. International Journal of Laboratory Hematology, 38, 42–49. [DOI] [PubMed] [Google Scholar]
- Park, S. , Quinn, J.B. , Romberg, E. & Arola, D. (2008) On the brittleness of enamel and selected dental materials. Dental Materials, 24, 1477–1485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto, C.L. , Bhering, C.L.B. , de Oliveira, G.R. , Maroli, A. , Reginato, V.F. , Caldas, R.A. et al. (2019) The influence of post system design and material on the biomechanical behavior of teeth with little remaining coronal structure. Journal of Prosthodontics, 28, e350–e356. [DOI] [PubMed] [Google Scholar]
- Plotino, G. , Grande, N.M. , Isufi, A. , Ioppolo, P. , Pedullà, E. , Bedini, R. et al. (2017) Fracture strength of endodontically treated teeth with different access cavity designs. Journal of Endodontics, 43, 995–1000. [DOI] [PubMed] [Google Scholar]
- PradeepKumar, A.R. , Shemesh, H. , Jothilatha, S. , Vijayabharathi, R. , Jayalakshmi, S. & Kishen, A. (2016) Diagnosis of vertical root fractures in restored endodontically treated teeth: a time‐dependent retrospective cohort study. Journal of Endodontics, 42, 1175–11380. [DOI] [PubMed] [Google Scholar]
- Richert, R. , Farges, J.‐C. , Tamimi, F. , Naouar, N. , Boisse, P. & Ducret, M. (2020) Validated finite element models of premolars: a scoping review. Materials, 13, 3280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ricucci, D. , Siqueira, J.F. , Loghin, S. & Berman, L.H. (2015) The cracked tooth: histopathologic and histobacteriologic aspects. Journal of Endodontics, 41, 343–352. [DOI] [PubMed] [Google Scholar]
- Rivera, E.M. & Walton, R. (2007) Longitudinal tooth fractures: findings that contribute to complex endodontic diagnoses. Endodontic Topics, 16, 82–111. [Google Scholar]
- de Rodrigues, M.P. , Soares, P.B.F. , Gomes, M.A.B. , Pereira, R.A. , Tantbirojn, D. , Versluis, A. & Soares, C.J. (2020) Direct resin composite restoration of endodontically‐treated permanent molars in adolescents: bite force and patient‐specific finite element analysis. Journal of Applied Oral Science, 28, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roperto, R. , Sousa, Y.T. , Dias, T. , Machado, R. , Perreira, R.D. , Leoni, G.B. et al. (2019) Biomechanical behavior of maxillary premolars with conservative and traditional endodontic cavities. Quintessence International, 50, 350–356. [DOI] [PubMed] [Google Scholar]
- Rover, G. , Belladonna, F.G. , Bortoluzzi, E.A. , De‐Deus, G. , Silva, E.J.N.L. & Teixeira, C.S. (2017) Influence of access cavity design on root canal detection, instrumentation efficacy, and fracture resistance assessed in maxillary molars. Journal of Endodontics, 43, 1657–1662. [DOI] [PubMed] [Google Scholar]
- Rover, G. , de Lima, C.O. , Belladonna, F.G. , Garcia, L.F.R. , Bortoluzzi, E.A. , Silva, E.J.N.L. et al. (2020) Influence of minimally invasive endodontic access cavities on root canal shaping and filling ability, pulp chamber cleaning and fracture resistance of extracted human mandibular incisors. International Endodontic Journal, 53, 1530–1539. [DOI] [PubMed] [Google Scholar]
- Saber, S.M. , Hayaty, D.M. , Nawar, N.N. & Kim, H.C. (2020) The effect of access cavity designs and sizes of root canal preparations on the biomechanical behavior of an endodontically treated mandibular first molar: a finite element analysis. Journal of Endodontics, 46, 1675–1681. [DOI] [PubMed] [Google Scholar]
- Saberi, E.A. , Pirhaji, A. & Zabetiyan, F. (2020) Effects of endodontic access cavity design and thermocycling on fracture strength of endodontically treated teeth. Clinical Cosmetic and Investigational Dentistry, 12, 149–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabeti, M. , Kazem, M. , Dianat, O. , Bahrololumi, N. , Beglou, A. , Rahimipour, K. et al. (2018) Impact of access cavity design and root canal taper on fracture resistance of endodontically treated teeth: an ex vivo investigation. Journal of Endodontics, 44, 1402–1406. [DOI] [PubMed] [Google Scholar]
- Sackett, D.L. (1997) Evidence based medicine. Seminars in Perinatology, 21, 3–5. [DOI] [PubMed] [Google Scholar]
- Sakaguchi, R.L. , Douglas, W.H. , Delong, R. & Pintado, M.R. (1986) The wear of posterior composite in an artificial mouth: a clinical correlation. Dental Materials, 2, 235–240. [DOI] [PubMed] [Google Scholar]
- Santos‐Filho, P.C.F. , Veríssimo, C. , Raposo, L.H.A. , Noritomi Meceng, P.Y. & Marcondes Martins, L.R. (2014) Influence of ferrule, post system, and length on stress distribution of weakened root‐filled teeth. Journal of Endodontics, 40, 1874–1878. [DOI] [PubMed] [Google Scholar]
- Santosh, S.S. , Ballal, S. & Natanasabapathy, V. (2021) Influence of minimally invasive access cavity designs on the fracture resistance of endodontically treated mandibular molars subjected to thermocycling and dynamic loading. Journal of Endodontics, 47, 1496–1500. [DOI] [PubMed] [Google Scholar]
- Sarkis‐Onofre, R. , Fergusson, D. , Cenci, M.S. , Moher, D. & Pereira‐Cenci, T. (2017) Performance of post‐retained single crowns: a systematic review of related risk factors. Journal of Endodontics, 43, 175–183. [DOI] [PubMed] [Google Scholar]
- Sarkis‐Onofre, R. , Jacinto, R.C. , Boscato, N. , Cenci, M.S. & Pereira‐Cenci, T. (2014) Cast metal vs. glass fibre posts: a randomized controlled trial with up to 3 years of follow up. Journal of Dentistry, 42, 582–587. [DOI] [PubMed] [Google Scholar]
- Sarvaiya, U. , Rudagi, K. & Joseph, J. (2020) A comparative evaluation of the effect of different access cavity designs on root canal instrumentation efficacy and resistance to fracture assessed on maxillary central incisors: an in vitro study. Journal of Conservative Dentistry, 23, 609–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sathorn, C. , Palamara, J.E.A. & Messer, H.H. (2005) A comparison of the effects of two canal preparation techniques on root fracture susceptibility and fracture pattern. Journal of Endodontics, 31, 283–287. [DOI] [PubMed] [Google Scholar]
- Sathorn, C. , Palamara, J.E.A. , Palamara, D. & Messer, H.H. (2005) Effect of root canal size and external root surface morphology on fracture susceptibility and pattern: a finite element analysis. Journal of Endodontics, 31, 288–292. [DOI] [PubMed] [Google Scholar]
- Schmitter, M. , Hamadi, K. & Rammelsberg, P. (2011) Survival of two post systems–five‐year results of a randomized clinical trial. Quintessence International, 42, 843–850. [PubMed] [Google Scholar]
- Schwendicke, F. & Stolpe, M. (2017) Cost‐effectiveness of different post‐retained restorations. Journal of Endodontics, 43, 709–714. [DOI] [PubMed] [Google Scholar]
- Schwendicke, F. & Stolpe, M. (2018) Restoring root‐canal treated molars: cost‐effectiveness‐analysis of direct versus indirect restorations. Journal of Dentistry, 77, 37–42. [DOI] [PubMed] [Google Scholar]
- Sequeira‐Byron, P. , Fedorowicz, Z. , Carter, B. , Nasser, M. & Alrowaili, E.F. (2015) Single crowns versus conventional fillings for the restoration of root‐filled teeth. Cochrane Database of Systematic Reviews, 9, CD009109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shu, X. , Mai, Q.Q. , Blatz, M. , Price, R. , Wang, X.D. & Zhao, K. (2018) Direct and indirect restorations for endodontically treated teeth: a systematic review and meta‐analysis, IAAD 2017 Consensus Conference Paper. Journal of Adhesive Dentistry, 20, 183–194. [DOI] [PubMed] [Google Scholar]
- Silva, A.A. , Belladonna, F.G. , Rover, G. , Lopes, R.T. , Moreira, E.J.L. , De‐Deus, G. et al. (2020) Does ultraconservative access affect the efficacy of root canal treatment and the fracture resistance of two‐rooted maxillary premolars? International Endodontic Journal, 53, 265–275. [DOI] [PubMed] [Google Scholar]
- Silva, E.J.N.L. , Lima, C.O. , Barbosa, A.F.A. , Augusto, C.M. , Souza, E.M. , Lopes, R.T. et al. (2021) Preserving dentine in minimally invasive access cavities does not strength fracture resistance of restored mandibular molars. International Endodontic Journal, 54, 966–974. [DOI] [PubMed] [Google Scholar]
- Skupien, J.A. , Cenci, M.S. , Opdam, N.J. , Kreulen, C.M. , Huysmans, M.C. & Pereira‐Cenci, T. (2016) Crown vs. composite for post‐retained restorations: a randomized clinical trial. Journal of Dentistry, 48, 34–39. [DOI] [PubMed] [Google Scholar]
- Smoljan, M. , Hussein, M.O. , Guentsch, A. & Ibrahim, M. (2021) Influence of progressive versus minimal canal preparations on the fracture resistance of mandibular molars: a 3‐dimensional finite element analysis. Journal of Endodontics, 47, 932–938. [DOI] [PubMed] [Google Scholar]
- van Staden, R.C. , Guan, H. & Loo, Y.C. (2006) Application of the finite element method in dental implant research. Computer Methods in Biomechanics and Biomedical Engineering, 9, 257–270. [DOI] [PubMed] [Google Scholar]
- Sun, J. , Jiao, T. , Tie, Y. & Wang, D. (2008) Three‐dimensional finite element analysis of the application of attachment for obturator framework in unilateral maxillary defect. Journal of Oral Rehabilitation, 35, 695–699. [DOI] [PubMed] [Google Scholar]
- Taha, N.A. , Palamara, J.E. & Messer, H.H. (2011) Fracture strength and fracture patterns of root filled teeth restored with direct resin restorations. Journal of Dentistry, 39, 527–535. [DOI] [PubMed] [Google Scholar]
- Thompson, V.P. (2020) The tooth: an analogue for biomimetic materials design and processing. Dental Materials, 36, 25–42. [DOI] [PubMed] [Google Scholar]
- Trivedi, S. (2014) Finite element analysis: a boon to dentistry. Journal of Oral Biology and Craniofacial Research, 4, 200–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, C.H. , Du, J.K. , Li, H.Y. , Chang, H.C. & Chen, K.K. (2016a) Factorial analysis of variables influencing mechanical characteristics of a post used to restore a root filled premolar using the finite element stress analysis combined with the Taguchi method. International Endodontic Journal, 49, 690–699. [DOI] [PubMed] [Google Scholar]
- Wang, J. , Ren, L. , Xie, L.Z. , Xie, H.P. & Ai, T. (2016b) Maximum mean principal stress criterion for three‐dimensional brittle fracture. International Journal of Solids and Structures, 102–103, 142–154. [Google Scholar]
- Wang, Q. , Liu, Y. , Wang, Z. , Yang, T. , Liang, Y. , Gao, Z. et al. (2020) Effect of access cavities and canal enlargement on biomechanics of endodontically treated teeth: a finite element analysis. Journal of Endodontics, 46, 1501–1507. [DOI] [PubMed] [Google Scholar]
- Wayne, J.S. , Chande, R. , Porter, H.C. & Janus, C. (2014) Effect of restoration volume on stresses in a mandibular molar: a finite element study. Journal of Prosthetic Dentistry, 112, 925–931. [DOI] [PubMed] [Google Scholar]
- Xia, J. , Wang, W. , Li, Z. et al. (2020) Impacts of contracted endodontic cavities compared to traditional endodontic cavities in premolars. BMC Oral Health, 20, 250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong, Y. , Huang, S.H. , Shinno, Y. , Furuya, Y. , Imazato, S. , Fok, A. et al. (2015) The use of a fiber sleeve to improve fracture strength of pulpless teeth with flared root canals. Dental Materials, 31, 1427–1434. [DOI] [PubMed] [Google Scholar]
- Xu, H. , Ye, N. , Lin, F. , Heo, Y.C. & Fok, A.S.L. (2021) A new method to test the fracture strength of endodontically‐treated root dentin. Dental Materials, 37, 796–804. [DOI] [PubMed] [Google Scholar]
- Yilmaz, E.Ç. & Sadeler, R. (2021) A literature review on chewing simulation and wear mechanisms of dental biomaterials. Journal of Bio‐and Tribo‐Corrosion, 7, 91. [Google Scholar]
- Yoon, H.G. , Oh, H.K. , Lee, D.Y. & Shin, J.H. (2018) 3‐D finite element analysis of the effects of post location and loading location on stress distribution in root canals of the mandibular 1st molar. Journal of Applied Oral Science, 26, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan, K. , Niu, C. , Xie, Q. , Jiang, W. , Gao, L. , Huang, Z. et al. (2016) Comparative evaluation of the impact of minimally invasive preparation vs. conventional straight‐line preparation on tooth biomechanics: a finite element analysis. European Journal of Oral Sciences, 124, 591–596. [DOI] [PubMed] [Google Scholar]
- Yuan, K. , Niu, C. , Xie, Q. , Jiang, W. , Gao, L. , Ma, R. et al. (2018) Apical stress distribution under vertical compaction of gutta‐percha and occlusal loads in canals with varying apical sizes: a three‐dimensional finite element analysis. International Endodontic Journal, 51, 233–239. [DOI] [PubMed] [Google Scholar]
- Zaytsev, D. , Ivashov, A. , Mandra, J. & Panfilov, P. (2014) On the deformation behavior of human dentin under compression and bending. Materials Science and Engineering C, 41, 83–90. [DOI] [PubMed] [Google Scholar]
- Zelic, K. , Vukicevic, A. , Jovicic, G. , Aleksandrovic, S. , Filipovic, N. & Djuric, M. (2015) Mechanical weakening of devitalized teeth: three‐dimensional finite element analysis and prediction of tooth fracture. International Endodontic Journal, 48, 850–863. [DOI] [PubMed] [Google Scholar]
- Zhang, A. , Chen, R. , Aregawi, W. et al. (2020) Development and calibration of biochemical models for testing dental restorations. Acta Biomaterials, 109, 132–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, A. , Ye, N. , Aregawi, W. , Zhang, M. , VanHeel, B. , Chew, H.P. et al. (2021) A review of mechano‐biochemical models for testing composite restorations. Journal of Dental Research, 100, 1030–1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, Y. , Liu, Y. , She, Y. , Liang, Y. , Xu, F. & Fang, C. (2019) The effect of endodontic access cavities on fracture resistance of first maxillary molar using the extended finite element method. Journal of Endodontics, 45, 316–321. [DOI] [PubMed] [Google Scholar]
- Zhu, Z. , Dong, X.Y. , He, S. , Pan, X. & Tang, L. (2015) Effect of post placement on the restoration of endodontically treated teeth: a systematic review. International Journal of Prosthodontics, 28, 475–483. [DOI] [PubMed] [Google Scholar]


