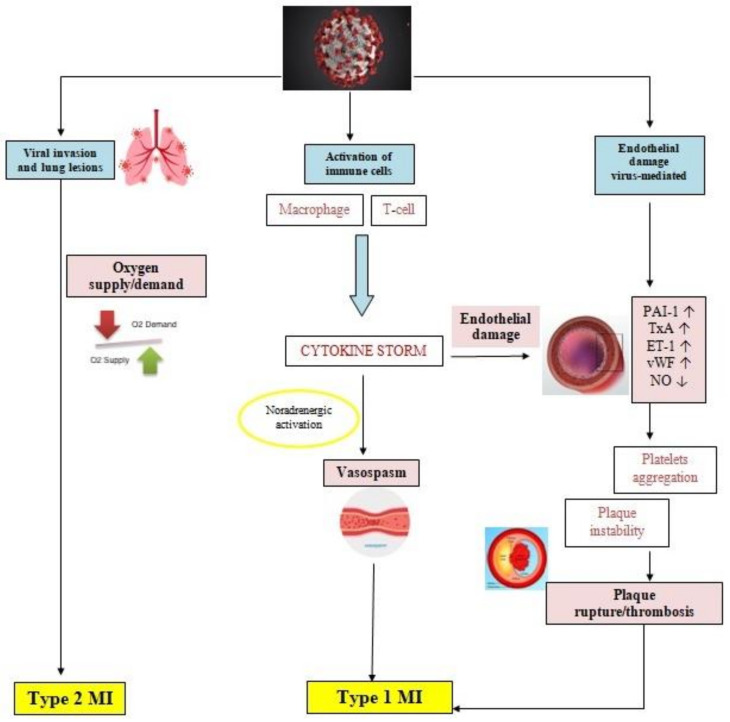
Figure 1.
Pathophysiology of myocardial ischemia in COVID-19 patients. COVID-19 infection acts by biding to the ACE2 receptors present on the surface of the host cell, which may be pneumocytes, macrophages, or endothelial cells. Pulmonary infection may range from mild disease to pneumonia and ARDS in severe forms, which in cases of severe respiratory impairment causes hypoxia and due to an oxygen supply/demand mismatch, a type 2 MI. An aberrant inflammatory response is typically described in COVID-19 infection, with the release of cytokines and molecules involved in inflammation, such as IL-1, IL-6, IL-7, TNFα, and IFNγ. The negative effects of cytokines manifest by increasing the production of oxidative stress agents and prothrombotic factors, which damage the endothelial function. Furthermore, SARS-CoV-2 may interact directly with the molecules expressed on the surface of the endothelial cells. The inflammatory environment promotes platelets activation and aggregation, upregulates the sympathetic nervous system, increasing the risk of instability of preexisting atheromatous plaques and coronary spasm. All these mechanisms predispose to plaque rupture and thrombosis, leading to type 1 MI. ACS: acute coronary syndrome; ACE2: angiotensin-converting enzyme 2; COVID-19: coronavirus disease 2019; IFNγ: interferon γ; IL-1: interleukin 1; IL-6: interleukin 6; IL-7: interleukin 7; MI: myocardial infarction; SARS-CoV-2: severe acute respiratory syndrome coronavirus 2; TNFα: tumor necrosis factor α.