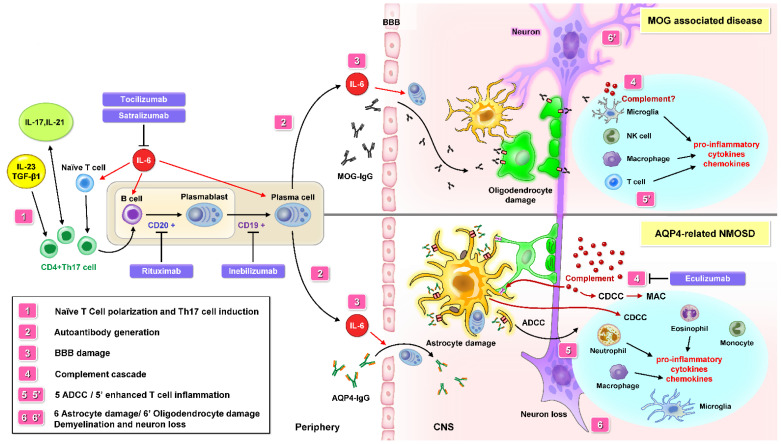
Figure 1.
The pathological mechanism of NMOSD may involve peripheral autoimmune dysregulation. Interleukin 6 (IL-6) is a key factor in AQP4-related NMOSD pathophysiology. A similar role of IL-6 is also reported in MOG-associated disease (MOGAD). Besides IL-6, Th17 cells differentiation may be induced by IL-17, IL-21, IL-23, and TGF-β1. It is thought that an impaired innate immune system may promote naive T cell transformation into Th 17 cell and stimulate B cell differentiation to plasmablasts, then to plasma cells producing AQP4-IgG or MOG-IgG autoantibody. A leaky BBB contributes to the migration of AQP4-IgG from the periphery into the CNS. AQP4-IgG bind to AQP4 and activate the complement cascade (CDC and CDCC) and ADCC. Cytokine and chemokine production leads to the recruitment of macrophages, eosinophils, neutrophils, and monocytes to the inflammation site. After microglia and macrophage infiltration, astrocytes and oligodendrocyte are damaged, which leads to advanced axonal degeneration and neuronal death. AQP4-IgG-seropositivity in NMOSD indicates the entity of astrocytopathy, and MOG-IgG results in oligodendropathy, named MOGAD. Current maintenance therapies include interfering with complement activation (Eculizumab), IL-6 R signaling (Tocilizumab and Satralizumab), and plasma cells producing AQP-4 and MOG IgG Abs (Rituximab and Inebilizumab). Abbreviations: NMOSD = neuromyelitis optica spectrum disorders; BBB = blood–brain barrier; CDC = complement-dependent cytotoxicity; CDCC = complement-dependent cellular cytotoxicity; ADCC = antibody-dependent cellular cytotoxicity; MOG = myelin oligodendrocyte glycoprotein; AQP-4 = aquaporin-4; IL-6 = interleukin 6; IL-17 = interleukin 17; Th17 cell = T helper 17 cell; TGF-β1 = transforming growth factor beta 1; IL-6 R = IL-6 receptor.