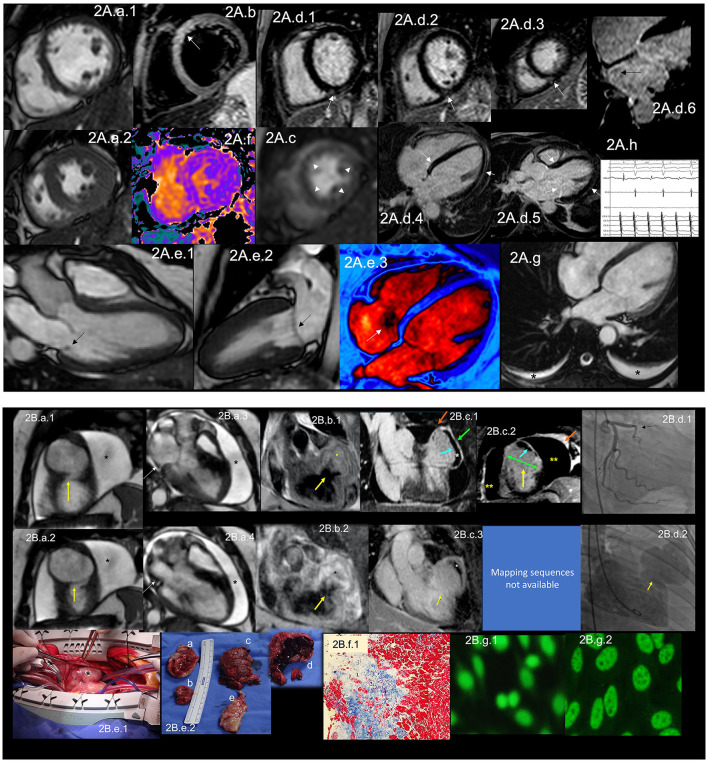
Figure 2.
(A) CMR findings in SLE—(A) from an arrhythmic perspective. A panel figure demonstrates the array of findings from a comprehensive CMR study in SLE from an arrhythmia perspective. (A.a) Shows normal global and regional right and left ventricular functions in SSFP sequence still cine images in short-axis views at the mid-ventricular level in end-diastole (A.a.1) and end-systole (A.a.2) LVEF 66% and RVEF 63%. (A.b) T2-W STIR sequence in short-axis view projection at a mid-ventricular level demonstrating mildly increased signal intensity in the anterior, anteroseptal, and inferoseptal segments (arrow) with a myocardial/skeletal muscle ratio of 2.8 and (A.f) a color-coded T2 mapping (native T2 value of 48 ms) consistent with myocardial edema. (A.c) Stress CMR with FPP T1-W sequence with adenosine infusion at 140 mcg/kg/min over 6 minutes shows a subendocardial ring perfusion defect (arrowheads) consistent with subendocardial ischemia due to endothelial dysfunction and probably microvascular disease (no obstructive coronary artery disease in CCTA). (A.d.1) LGE PSIR sequence. (A.d.1–3) short-axis views at basal (A.d.1), mid (A.d.2) and apical (A.d.3) levels, and long-axis views in 4-chambers (A.d.4,6) and 3-chambers (A.d.5) projections. The arrows in these images show areas of focal fibrosis in the subepicardium in the inferior segments in (A.d.1–3) from the base to the apex. (A.d.4,5) shows areas of midventricular LGE in basal anteroseptal and inferoseptal segments (arrows) and subepicardial enhancement in mid and apical inferolateral segments (arrow). (A.d.6) A zoomed image of the 4-chambers view showing LGE suggestive of LA fibrosis (arrow). (A.h) A polygraphic trace of an EP study showing atrial fibrillation successfully ablated. (A.e.1–3) SSFP sequence still cine images in long-axis views, showing in a 3-chambers view an isointense, small nodule, in the ventricular side of the mitral valve suggestive of Libman-Sacks endocarditis (arrow) (confirmed by echo) (A.e.1), in a 2-chambers view, a mildly thickened mitral valve (A.e.2) and in a color-coded 4-chambers (A.e.3) the presence of tricuspid regurgitation (arrow). (A.g) An SSFP sequence still cine images in true axial view showing bilateral pleural effusion (asterisks). SLE, systemic lupus erythematosus; CMR, cardiovascular magnetic resonance; SSFP, steady-state free precession; LVEF%, left ventricular ejection fraction; RVEF%, right ventricular ejection fraction; T2-W STIR, T2-weighted short-tau inversion recovery; FPP, first-pass perfusion; T1-W, T1-weighted; CCTA, invasive coronary angiography; LGE, late gadolinium enhancement; PSIR, phase-sensitive inversion recovery; LA, contrast enhancement magnetic resonance angiography; EP, electrophysiology. (B) CMR findings in SLE—(B), from a thrombotic perspective. A panel figure demonstrates the array of findings from a comprehensive CMR study in a 1.5 T scanner of SLE from a coronary thrombosis perspective. (B.a.1–4) SSFP sequence still cine images in short-axis views at mid to apical ventricular level in end-diastole (A.a.1) and end-systole (A.a.2) and long-axis 3-chambers view, in end-diastole (B.a.3) and end-systole (B.a.4) that shows in (A.a.1) the loss of continuity of the LV anterior segment (yellow arrow), with normal thickening of the remaining segments (B.a.2) surrounded by a large pericardial effusion (black asterixis), that exhibits hemodynamic compromise as the diastolic collapse of the LA [yellow arrow in (B.a.3,4)]. LVEF 42% and RVEF 65%. (B.b,c) Show the tissue characterization findings. (B.b.1) T1-W sequence in long-axis view demonstrating a wide-necked outpouching of the LV anterior wall with the apparent loss of myocardial continuity with a thinned out, fibrosed muscle surrounding the cavity consistent with true aneurysm (yellow arrow) with tissue within the aneurysmal cavity of two different intensities (yellow asterisks) suggestive of thrombus. (B.b.2) T2-W STIR sequence in long-axis view confirming the findings of T1-W sequences (yellow arrow) with the evident different signal intensity of the tissue components inside the aneurysmal cavity (black asterixis) suggestive of two varying ages of the thrombus, recent and old, and slow-flowing blood. (B.c) LGE PSIR sequence. (B.d.1) Long-axis 3-chambers view showing loss of myocardial continuity, a large cavity surrounded by scarred myocardium (green arrow) with a large thrombus on its endocardial aspect (white asterisks), pericardial enhancement (orange arrow), and a large pericardial effusion (yellow double asterisks) that are confirmed on the corresponding short-axis view (B.c.2). (B.c.3) A long TI LGE-PSIR long-axis 3-chambers view confirming previous data and showing the new thrombus component (yellow asterisks). (B.d.1) An invasive angiography demonstrating a total occlusion of the proximal LAD (arrow) and the invasive ventriculography (B.d.2) Showing a large leak of contrast media at an anterior mid-ventricular level impossible to differentiate aneurysm from pseudoaneurysm. (B.e.1) Open heart surgery showing the intact LV wall covered by the pericardium consistent with a true aneurysm (arrow) which was successfully resected (B.e.2), and surgery confirmed CMR findings, a ventricular aneurysm (B.e.2.a,b), a transmural scar (B.e.2.e) and a large thrombus (B.e.2.c) composed of two different aged thrombi (B.e.2.d). H.E. stain histology confirmed the presence of a large scar with no evidence of atherosclerosis (B.f.1). Based on the inflammatory component of the pericardium, suspicion of autoimmune instead of atherosclerotic etiology was suspected and confirmed by the finding of ANA with a homogeneous pattern in the pericardial effusion (B.g.1) and peripheral blood of a fine speckled pattern (B.g.2). SLE, systemic lupus erythematosus; CMR, cardiovascular magnetic resonance; SSFP, steady-state free precession; LVEF%, left ventricular ejection fraction; RVEF%, right ventricular ejection fraction; LV, left ventricle; LA, left atrium; T2-W STIR, T2-weighted short-tau inversion recovery; FPP, first-pass perfusion; T1-W, T1-weighted; ICA, invasive coronary angiography; LGE, late gadolinium enhancement; PSIR, phase-sensitive inversion recovery; TI, time to inversion; LAD, left anterior descending artery; H.E., hematoxylin and eosin.