Abstract
Objective
This study aims to establish the effectiveness and active ingredients of UK-based social prescribing interventions targeting mental health and well-being outcomes.
Design
Systematic review adhering to Preferred Reporting Items for Systematic Reviews and Meta-Analysies guidelines and a published protocol.
Data sources
Nine databases were systematically searched up to March 2022.
Eligibility criteria
Social prescribing interventions in the UK involving adults aged ≥18 years, which reported on mental health outcomes.
Data extraction and synthesis
Two reviewers extracted data on study characteristics; outcomes; referral pathways; treatment fidelity strategies; person-centredness; intervention development processes and theory-linked behaviour change techniques (BCTs). Data were narratively synthesised.
Results
52 074 records were retrieved by the search, 13 interventions reported across 17 studies were included in this review (N=5036 participants at post-intervention). Fifteen studies were uncontrolled before-and-after designs, one a randomised controlled trial and one a matched groups design. The most frequently reported referral pathway was the link worker model (n=12), followed by direct referrals from community services (n=3). Participants were predominantly working age adults, and were referred for anxiety, depression, social isolation and loneliness. 16 out of 17 studies reported statistically significant improvements in outcomes (mental health, mental well-being, general health, or quality of life). Strategies to enhance treatment fidelity were suboptimal across studies. Only two studies used a specific theoretical framework. A few studies reported engaging service users in codesign (n=2) or usability and/or feasibility testing (n=4). Overall, 22 BCTs were coded across 13 interventions. The most frequently coded BCTs were social support-unspecified (n=11), credible source (n=7) and social support-practical (n=6).
Conclusions
Robust conclusions on the effectiveness of social prescribing for mental health-related outcomes cannot be made. Future research would benefit from comprehensive intervention developmental processes, with reference to appropriate theory, alongside long-term follow-up outcome assessment, using treatment fidelity strategies and a focus on principle of person-centred care.
PROSPERO registration number
CRD42020167887.
Keywords: MENTAL HEALTH, PUBLIC HEALTH, PRIMARY CARE
Strengths and limitations of this study.
The methodological approach undertaken identified active ingredients within effective social prescribing interventions as well as the overall impact of the interventions on mental health and well-being outcomes.
Heterogeneity of study designs, populations, interventions and outcome measures prevented the conduct of a meta-analysis.
Robust conclusions on the effectiveness of social prescribing for mental health-related outcomes cannot be established due to issues with methodological quality.
Introduction
Social prescribing is a complex intervention that aims to provide holistic support and care to people living with a range of long-term health problems.1 It is defined by the Social Prescribing Network as ‘a means of enabling general practitioners and other frontline healthcare professionals to refer patients to a link worker’ from which a link worker will coproduce an action plan to address what matters to the individual.2
National Health Service England included social prescribing as one of the six pillars of a Universal Personalised Care Strategy,3 and have a target to recruit additional link workers to help reach 900 000 individuals by 2023.3 This is despite several systematic reviews reporting that the evidence for the (cost-) effectiveness of social prescribing is mixed, with most studies having important methodological limitations, including absence of comparison groups,4 disparity in follow-up periods,4 absence of clear and focused objectives5 and no statement of underpinning model or theory informing intervention content or components.6
To determine what works (or does not work) within social prescribing interventions, there is a pressing need to identify ‘active ingredients’ of social prescribing interventions such as mode of delivery, duration, intensity, underpinning theory/model of behavioural change and theory-linked behaviour change techniques (BCTs). Identification of these active ingredients will help to inform the design and evaluation of future social prescribing interventions, including optimisation of existing interventions. Kimberlee7 and Husk et al,8 describe four models of social prescribing (referral pathways): signposting service users to appropriate services or groups; direct referral from primary care to an activity or service; a link worker (based within or externally to primary care) who receives referrals and in turn conducts a needs assessment and refers the service user onto an activity or service; and the latter model with the addition of feedback and a support loop between the link worker and the service user. This has been supported by purposive action, particularly influenced by the language of prescribing in primary care, to enhance the implementation of social prescribing in primary care.9
Approximately one in six adults in the UK are living with mental health conditions10 and social prescribing has the potential to improve outcomes for this population. Mental health has a devasting impact on individuals, their families and society, with depression and anxiety disorders affecting 16% of the UK population at any one time.10 A conservative estimate of the total costs of mental health in the UK in 2019 was £117.9 billion (approximately 5% of GDP), with 56% and 27% for people aged 15–49 and 50–69, respectively.11
Previous systematic reviews have evaluated the impact of social prescribing on people living with a range of health needs and long-term conditions, but without specific focus on elucidating the evidence of social prescribing interventions for people living with mental health conditions.4 8 12 We conducted a systematic review to establish the effectiveness, and active ingredients of UK-based social prescribing interventions targeting mental health.
Methods
Study design
This systematic review followed a published protocol (CRD42020167887)13 and adhered to the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines.14 A PRISMA checklist for this review is presented in online supplemental material 1.
bmjopen-2021-060214supp001.pdf (52.1KB, pdf)
Review criteria
Included studies were social prescribing interventions (any referral pathway, with or without a link worker based in any setting) involving adults aged ≥18 years that reported on mental health or well-being outcomes. Studies involving adults with physical health comorbidities were included if the study reported on mental health-related or well-being outcomes primarily. Only studies with a primary quantitative study design, published in English and conducted in the UK were eligible for inclusion in the review. The decision to restrict the review to UK-based studies was made to ensure relevance and transferability of the findings to the health and social care setting in the UK. Studies were excluded if there was no referral or signposting to either a link worker or group/service and/or did not report any empirical data.
Search strategy
The following nine databases were searched from inception to 21 March 2022: Cochrane Databases of Systematic Reviews (CDSR), The Cochrane Central Register of Controlled Trials (CENTRAL), CINAHL (Cumulative Index of Nursing and Allied Health Literature), Cochrane Protocols, Embase, Medline, PsycINFO, Scopus, and Web of Science. Prior to searching, reviewers carried out an extensive exercise to identify and collate potentially relevant terms to cover the concepts of social prescribing and mental health. The search strategy was then developed by an expert information scientist (LE) and adapted as necessary to consider differing indexing terms and other search functionality available in each of the additional databases.
The search strategy developed for each database is provided in online supplemental material 2. Reference lists of included studies were searched to identify any further studies to be considered for eligibility of inclusion.
bmjopen-2021-060214supp002.pdf (80.2KB, pdf)
Study selection
All results from electronic database searches were uploaded to EndNote V.X9 and underwent a process of deduplication. One reviewer (MC) screened all titles and abstracts and a second reviewer (CJ) independently screened 20% of all titles and abstracts. All studies retained following screening of titles and abstracts were reassessed in full text by the same two reviewers who worked independently using a study selection form. At stage 1 and 2 of study selection, any disagreements between the two reviewers that could not be resolved via discussion were referred to a third reviewer for adjudication (KA or DF). Subsequently, handsearches of reference lists and citation searching of included studies (using Google Scholar) were conducted to identify any potentially relevant literature not captured by the electronic search.
Data extraction
A structured data extraction form was used to capture information on study characteristics (country of origin, aims, design, outcomes targeted, inclusion/exclusion criteria, sampling method, sample size, follow-up period, lost to follow-up), components of social prescribing interventions, methodological quality, extent that interventions were person-centred, treatment fidelity strategies, comprehensiveness of intervention development processes and outcome measures. Data were extracted on three stages of social prescribing (where applicable): initial assessment, use of a facilitator or link worker and delivery of socially prescribed activity at a specific service. Components of the Template for Intervention Description and Replication15 checklist were applied to describe key features of social prescribing interventions. One reviewer (MC) extracted data on all included studies and a second reviewer (KA) checked data extracted from 50% of included studies. Any discrepancies between the two reviewers were resolved by discussion and by checking the primary study data.
Three reviewers (MC, KA and LA) independently coded the presence of theory-linked BCTs within included interventions using the BCT Taxonomy V.1.16 The extent that included interventions adhered to core principles of person-centred care was independently assessed by two reviewers (MC and KA). A four-item checklist was designed specifically for this review, with reference to relevant literature17–19 in order to record whether: a needs assessment was conducted with the study participants (i.e., a tailored conversation to discuss their needs and goals); a choice of social prescribing activity was offered to participants; participants were actively involving in discussion to elicit their preferences for type of social prescribing activity and the participants received a social prescription consistent with their preferred choice of social prescribing activity.
The comprehensiveness of developmental processes for social prescribing interventions were assessed using a checklist developed in a previous systematic review20 to record: use of a framework, theory or model to guide design and evaluation, use of best available evidence from research (eg, systematic review), conducting a needs assessment with service users, evidence of coproduction or design with service users and evidence of piloting or feasibility testing in the target population.
Methodological strategies used by included studies to monitor and enhance the reliability and validity of behavioural interventions (ie, treatment fidelity strategies) were assessed independently by three reviewers (MC, KA, and DF) using a framework published by Bellg et al.21 This framework describes treatment fidelity across five domains: design of the study; monitoring and improving provider training; monitoring and improving delivery of interventions; monitoring and improving receipt of interventions; and monitoring and improving enactment of intervention skills.
Any additional articles, grey literature or media sources that were referenced by included studies were consulted for the purpose of coding intervention development processes, person-centredness, fidelity and BCTs. Where appropriate, data were coded across multiple studies reporting on the same intervention.
Methodological quality assessment
Methodological quality was assessed independently by two reviewers (MC and KA) using the Critical Appraisal Skills Programme Randomised Control Trial Checklist,22 National Heart, Lung and Blood Institute Quality Assessment Tool for Before-and-After Studies,23 and ROBINS-I: tool for assessing risk of bias in non-randomised studies of interventions.24
Data synthesis
Data were synthesised narratively due to the heterogeneity of study designs, populations, interventions (referral pathways, form and content) and outcome measures (i.e., assessment methods to assess mental health and well-being). The ‘promise’ of active ingredients and other intervention features for positively changing outcomes was assessed by calculating promise ratios.25
Patient and public involvement
There was no patient or public involvement in this study.
Results
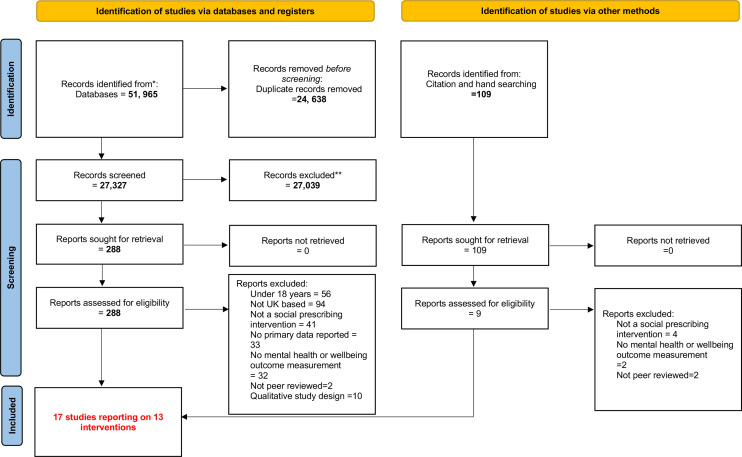
In total 52 074 (database searching n=51 965, reference lists and citation/hand searching n=109) potentially relevant studies were identified from the electronic search (figure 1). A total of 297 full-text articles (database search=288 and citation/handsearching=9) were assessed for inclusion. Seventeen studies reporting on 13 interventions met the inclusion criteria.26–42 An additional 15 sources of grey literature were consulted for details on the intervention development, person-centredness, fidelity and BCTs.43–57
Figure 1.
PRISMA diagram. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses. *Databases searched. **At title and abstract level. CDSR, cochrane databases of systematic reviews; CENTRAL, the cochrane central register of controlled trials; CINAHL, cumulative index of nursing and allied health literature; Cochrane Protocols, Embase, Medline, PsycInfo, Scopus and Web of Science.
Findings of the Art Lift intervention were reported across four studies.26–29 The Art Shine intervention was reported in one study.30 The Social Cure and social prescribing intervention was reported across two studies.38 39 The British Red Cross Connecting Communities,31 The Cadwun Mon,32 The Cares of Life Project,33 The Fife Social Prescribing: Mood Café,34 GROW: Art, Park and Well-being,35 Luton Social Prescribing Programme,36 Museums on Prescription,37 The Southwest Well-being Programme,40 and Wetlands for Well-being42 all were reported within one study. One included study41 did not provide a specific name for the intervention.
Study characteristics
A summary of the 13 interventions reported across the 17 included studies is presented in table 1. Fifteen studies were conducted in England,26–31 33 35–42 one in Wales32 and one in Scotland.34 Seventeen studies had a combined post-intervention sample size of 5036 participants. Fifteen studies were uncontrolled before-and-after designs,26–32 34–40 42 one a randomised controlled trial33 and one a matched groups design.41
Table 1.
Summary of study characteristics
| Author(s) of Corresponding Study(s) | Intervention/programme name | Research design | Population sample sizes (pre–post assessment data and mean age and sex) |
Participant ethnicity* (postassessment data) | Employment status (postassessment data) | Reason for referral | Duration of Follow-up | Referral pathway (Husk et al)8 |
| Crone et al26 | Art Lift | Uncontrolled Before/after study | Preassessment n=157 Postassessment n=84 (mean age=57, SD=15), male n=22, female n=62 |
NR | NR | Anxiety and depression | 2.5 months | Direct Referral from Link Worker in Primary Care |
| Crone et al27 | Uncontrolled Before/after study | Preassessment n=818 Postassessment n=651 (mean age=51.9, SD=15.9), male n=142†, female n=509 |
NR | NR | Anxiety and depression | 2.5 months | Direct Referral from Link Worker in Primary Care | |
| Sumner et al28 | Uncontrolled Before/after study | Preassessment n=547 Postassessment n=418 (mean age=49.7, SD=15.5), male n=83†, female n=335 |
NR | In‡ n=76 Out§ n=176 Retired n=103 |
Anxiety and depression | 2.5 months | Direct Referral from Link Worker in Primary Care | |
| Sumner et al29 | Uncontrolled Before/after study | Preassessment n=245 Postassessment n=110 (mean age=51.3, SD=15.9), male n=16†, female n=94 |
NR | In‡ n=22 Out§ n=86 Retired n=NR Unknown n=2 |
Anxiety and depression | 2 months | Direct Referral from Link Worker in Primary Care | |
| van de Venter et al30 | Art Shine | Uncontrolled Before/after study | Preassessment n=NR Postassessment n=44 (mean age=43, SD=NR), male n=7, female n=36, other n=1 |
‘White British’ n=29 (66%) ‘Black and minority ethnic’ n=9 (21%) Unknown n=6 |
NR | Depression and social isolation | 5 months | Direct Referral from Primary Care |
| Foster et al31 | British Red Cross: Connecting Communities | Uncontrolled Before/after study | Preassessment n=NR Postassessment n=2250 (mean age=65.6, SD=18.8), male n=702, female n=1426, other n=122 |
‘White British’ n=1,313 (58%) ‘Not White British’ n=499 (22%) Unknown n=438 |
NR | Loneliness | 3 months | Link Worker Model |
| Roberts and Windl32 | Cadwyn Mon | Uncontrolled Before/after study | Preassessment n=182 Postassessment n=120 (mean age=76.7, SD=NR), male n=22, female n=98, other n=1 |
NR | NR | Loneliness and social isolation | 3.75 months | Link Worker Model |
| Afuwape et al33 | Cares of Life Project | Randomised controlled trial | n=16 Intervention group Preassessment n=20 Postassessment n=16 (mean age=43.6, SD=7.7) male n=NR, female n=NR n=16 Comparison group Preassessment n=20 Postassessment n=16 (mean age=32.6, SD=11.0) male n=NR, female n=NR |
‘All participants were of Black African Origin or Black Caribbean Origin’ n=32 | NR | Anxiety and depression | 3 months | Direct referral from multiple Sectors¶ |
| Morton et al34 | Fife Social Prescribing (Mood Café) | Uncontrolled Before/after study | Preassessment n=174 Postassessment n=136 (mean age=52, SD=11), male n=37, female n=99† |
NR | NR | Anxiety and depression | NR | Link Worker Model |
| Thomson et al35 | GROW: Art, Park and Well-being | Uncontrolled Before/after study | Preassessment n=20 Postassessment n=20 (mean age=NR), male n=11, female n=9† |
NR | NR | Mental well-being | 2.5 months | Direct referral from Community and Local Mental Health Services |
| Pescheny et al36 | Luton Social Prescribing Programme | Uncontrolled Before/after study | Preassessment n=162 Postassessment n=63 (mean age=NR), male n=23, female n=40 |
NR | In‡ n=22 Out§ n=41 |
Mild to moderate mental health issues | Dependant on Needs Assessment | Link Worker Model |
| Thomson et al37 | Museums on Prescription | Uncontrolled Before/after study | Preassessment n=NR Postassessment n=115 (mean age=NR), male n=42†, female n=73 |
‘White-British’ n=94 (82%) Other=NR |
NR | Social isolation | 2.5 months | Direct Referral from Community Care |
| Kellezi et al38 | Social Cure and Social Prescribing | Uncontrolled Before/after study | Preassessment n=630 Postassessment n=178 (mean age=55.8, SD=13.8), male=86, female=91, other n=1 |
NR | NR | Loneliness | 4 months | Link Worker Model |
| Wakefield et al39 | Uncontrolled Before/after study | Preassessment n=630 Postassessment n=63 (mean age=57.1, SD=15.7), male=32, female=31 |
NR | NR | Social isolation and loneliness | 9 months | Link Worker Model | |
| Jones et al40 | Southwest Well-being Programme | Uncontrolled Before/after study | Preassessment n=841 Postassessment n=687 (mean age=NR), male n=179, female n=357, other n=151 |
‘White’ n=623 (91%) ‘Black or Minority Ethnic Group’ n=38 (6%) Unknown n=26 |
In‡ n=259 Out§ n=198 Retired n=209 Other n=21 |
Anxiety and depression | 3 months | Direct Referral from Community Care |
| Carnes et al41 | Unnamed Intervention | Matched groups design | Survey Study Intervention Group Preassessment, n=184 Postassessment, n=65 (mean age=NR) male=NR, female=NR Comparison group (matched based on age, GP attendance and diagnosis) Preassessment, n=302 Postassessment, n=127 Mean age=NR mMale=NR, female=NR Analysis of healthcare Resource use Intervention group, n=377 (Mean age=NR) male=NR, female=NR Comparison group (matched based on age, sex, ethnicity and comorbidities), n=7540 Mean age=NR male=NR, female=NR |
Survey Study Intervention Group Post-assessment=NR Comparison group Preassessment: White n=170 Non-white n=123 Post-assessment=NR Analysis of Healthcare Resource use=NR |
NR | Anxiety and depression | 8 months | Link Worker Model |
| Maund et al42 | Wetlands for Well-being | Uncontrolled Before/after Sstudy | Preassessment n=16 Postassessment n=16 (mean age=NR), male=8, female=8 |
‘White-British’ n=13 (82%) ‘White-Other’ n=3 (19%) |
In‡ n=1 Out§ n=10 Retired n=5 |
Anxiety and depression | 1.5 months | Link worker model from community referral |
*Terminology used by authors.
†Not explicitly reported, calculated by authors.
‡In=in work, education or position of responsibility.
§Out=out of work, education or position of responsibility.
¶Multiple sector—referral from a combination of the following: general practitioner, healthcare professional, community, self-referral, secondary care or social care.
NR, not reported.
The referral pathways were mapped against those described by Husk et al.8 The most common referral pathway reported within studies was the link worker model (n=12 studies),26–29 31 32 34 36 38 39 41 42 followed by referrals direct from community services (n=3 studies),35 37 40 primary care30 or from multiple services.33
The mean age of participants who received social prescribing interventions ranged from 43 to 77 years across 11 studies.26–34 38 39 Six studies did not report on the age of participants.35–37 40–42 Two studies did not report data on the sex of participants.33 41 Out of 15 studies that reported on participant sex, 12 studies reported a higher proportion of female participants.26–32 34 36–38 40
Data on ethnicity of participants were reported in seven studies,30 31 33 37 40–42 but most did not report data using census categories; for example, only reporting numbers of participants who were White British or from Black, Asian and Minority Ethnic (BAME) groups. Only one study specifically targeted people from BAME groups.33 One study did not report on participant ethnicity at the post-assessment period.41 Proportions of White or White British participants at post-assessment based on data from five studies was 58%,31 66%,30 82%37 42 and 91%.40
Employment status was reported by five studies28–30 36 42 and was summarised into four categories: participants who were in work (either full time or part time), education (full time or part time education or described as a student) or position of responsibility (such as full time carers) (ranged from 1 to 259 participants); those who were not unemployed or incapacitated from work (ranged from 10 to 198 participants based on data from 5 studies); participants who were retired (ranged from 5 to 209 participants based on data from 2 studies); and participants described as ‘other’(ranged from 2 to 21 participants based on data from 2 studies). Employment status was not reported by the remaining 12 studies.26 27 30–35 37–39 41
The most commonly reported reasons for referral to a social prescribing service were anxiety or depression, (or combined anxiety and depression), n=9 studies.26–29 33 35 40–42 Depression and social isolation was the primary reason for referral in one study.30 Loneliness was the primary reason for referral in one study,31 and social isolation in another.37 Social isolation and loneliness was reported as the primary reasons for referral by three studies.32 38 39 The two remaining studies reporting mild to moderate mental health issues36 and mental well-being35 as primary reasons for referral.
The period between baseline assessment and follow-up was reported by 15 studies and ranged between 1.5 months40 and 9 months.39 One study did not report a follow-up period.34 One study reported a follow-up period that was based on individual need.36 Fourteen studies reported sample sizes at preassessment, which ranged from n=1642 to n=841.40 All 17 included studies reported the total number of individuals who took part in a follow-up assessment, ranging from 1642 to 2250.31 Based on data from 14 studies,26–29 32–36 38–42 the average lost to follow-up (attrition rate) was 38% (SD=27), which ranged from 90%39 to 0%.35 42
Study outcomes
Outcomes are grouped into between-group and within-group differences (table 2). Of the 17 included studies, 16 reported statistically significant improvements in mental health, mental well-being, general health or quality-of-life outcomes from baseline to follow-up26–32 34–40 42 or between the intervention group and matched controls.33 Only one intervention (unnamed intervention)41 did not report any statistically significant improvement in outcomes.
Table 2.
Between and within group changes in outcomes
| Intervention/programme Name | Study | Outcome measure | Statistically significant improvement (p value) | 95% CIs |
| Between Group Changes (compared with comparison groups) | ||||
| Cares Of Life Project | Afuwape et al33 | GHQ-28 | Yes (0.03) | 0.86 to 14.65 |
| GAF | No (0.87) | −10.40 to 8.84 | ||
| SF-36 Mental Health Score | Yes (0.02) | −21.99 to −1.88 | ||
| Unnamed Intervention | Carnes et al41 | General Health Score | No | −0.31 to 0.25 |
| HADS Score | No | −2.11 to 2.58 | ||
| Well-being | No | −0.57 to 0.39 | ||
| Within Group Changes | ||||
| Art Lift | Crone et al26 | WEMWBS-7 | Yes (<0.001) | Not reported |
| WEMWBS −14 | Yes (<0.001) | Not reported | ||
| Crone et al27 | WEMWBS-14 | Yes (<0.001) | Not reported | |
| Sumner et al28 | WEMWBS-14 | Yes (<0.001) | 0.93 to 0.98 | |
| Sumner et al29 | GAD-7 | Yes (<0.001) | Not reported | |
| PHQ-8 | Yes (<0.001) | Not reported | ||
| WEMWEBS-14 | Yes (<0.001) | Not reported | ||
| Art Shine | van de Venter et al30 | WEMWBS-14 | Yes (<0.001) | 4.80 to 11.20 |
| BRC Connecting Communities | Foster et al31 | ULS-3 | Yes (<0.001) | −1.91 to −1.77 |
| Cadwyn Mon | Roberts et al32 | De Jong Gierveld Loneliness Scale | Yes (<0.001) | Not reported |
| Lubben Social Network Scale | Yes (<0.004) | Not reported | ||
| Satisfaction with Life Scale | Yes (<0.001) | Not reported | ||
| Fife Social Prescribing (Mood Café) | Morton et al34 | HADS – Anxiety | Yes (p<0.001) | 2.20 to 3.30 |
| HADS – Depression | Yes (<0.001) | 1.90 to 3.20 | ||
| WEMWBS-14 | Yes (<0.001) | −8.10 to −5.10 | ||
| GROW: Art, Park and Well-being | Thomson et al35 | UCL Museum Well-being Measure | Yes (<0.001) | Not reported |
| Luton Social Prescribing Programme | Pescheny et al36 | WEMWBS-7 | Yes (<0.0001) | 1.68 to 3.88 |
| Museums On Prescription | Thomson et al37 | MWM-OA Main Effect | Yes (<0.001) | Not reported |
| Social Cure and Social Prescribing | Kellezi et al38 | ULS-8 | Yes (<0.0001) | Not reported |
| Wakefield et al39 | ULS-8 | Yes (<0.001) | Not reported | |
| EQ5D | Yes (<0.04) | Not reported | ||
| Southwest Well-being Programme | Jones et al40 | General Health Scale* | Yes (<0.001) | Not reported |
| Social Well-being: SWB-6* | Yes (<0.001) | Not reported | ||
| WEMWBS-7* | Yes (<0.001) | Not reported | ||
| CES-D-7** | Yes (<0.001) | Not reported | ||
| Wetlands For Well-being | Maund et al42 | WEMWBS-14 | Yes (0.009) | Not reported |
| GAD-7 | Yes (0.002) | Not reported | ||
| PSS | Yes (0.041) | Not reported | ||
| PANAS (Positive) | Yes (0.012) | Not reported | ||
| PANAS (Negative) | Yes (p=0.025) | Not reported | ||
*Components of the Southwest Well Being Questionnaire.
CES-D-7, Centre for Epidemiology Depression Scale; EQ5D, EuroQol Quality of Life Measure; GAD-7, Generalised Anxiety Disorder; GAF, Global Assessment of Functioning; GHQ-28, General Health Questionnaire-28; GHS, General Health Score; HADS, Hospital Anxiety and Depression Scale; MWM-OA, Museum Well-Being Measure for Older Adults; PANAS, Positive and Negative Affect Schedule; PHQ-8, Patient Health Questionnaire; PSS, Perceived Stress Scale; SF-36, Short Form-36; SWWBQ, Southwest Well-Being Questionnaire; ULS-3 or 8, University College London Loneliness Scale; WEMWBS, Warwick-Edinburgh Mental Well-Being Scale.
The 7-item or 14-item Warwick- Edinburgh Mental Well-being Scale (WEMWBS)58 was the most frequently used outcome measure.26–30 34 36 40 42 Seven studies used the 14-item26–30 34 42 and three used the 7-item short-form version.26 36 40 All studies reported a statistically significant improvement in mental well-being assessed with the WEMWBS.
Three studies used other measures of mental well-being: Social Well-being Questionnaire-640; Museum Well-being Measure for Older Adults37 and University College London Museum Well-being Measure.35 All three studies reported a statistically significant improvement in mental well-being.
Three studies31 38 39 assessed loneliness using the University College London Loneliness Scale-3 or 859 and one32 used the De Jon Gierveld Loneliness Scale.60 All three studies reported a statistically significant reduction in loneliness. One study32 reported a statistically significant reduction in social isolation assessed with the Lubben Social Network Scale.61
Five studies29 34 40–42 used mental health symptom-based outcome measures such as: Hospital Anxiety and Depression Scale,62 Generalised Anxiety Disorder Assessment-7,63 Patient Health Questionnaire-864 or the Centre for Epidemiological Studies Depression Scale-7.65 Four studies reported a statistically significant improvement in symptom-based outcomes.29 34 40 42
General health measures were reported by three studies33 40 41: General Health Questionnaire-2866 or Global Assessment of Functioning.67 In addition, quality-of life-measures were used by three studies32 33 39 using the Satisfaction with Life Scale,68 EuroQol Quality of Life Measure69 and the Short-Form-36.70
Other outcomes assessed by one study42 were stress using the Perceived Stress Scale71 and mood using the Positive and Negative Affect Schedule72 and reported statistically significant improvements in these outcomes following social prescribing.
Two studies38 41 reported on health service utilisation using patient reported data on group memberships and primary care health service use38 and health records to extract data on consultation rates and medication prescribed.41 Both studies reported a statistically significant reduction in use of primary healthcare.
Methodological quality assessment
The methodological quality assessment of for each individual study can be found in online supplemental material 3.
bmjopen-2021-060214supp003.pdf (145.4KB, pdf)
With reference to the 15 uncontrolled before-and-after studies, the scores (out of 22) ranged from 926 39 to 14.30 36 37 42 All before-and-after studies clearly stated the study question or objective and included participants that were representative of those who would be eligible in the clinical population of interest. Seven studies clearly described the eligibility criteria or described the intervention in sufficient enough detail to ensure the consistent delivery across the included population.28 30 32 36 37 40 42 Only one study detailed sufficient information to conclude that all eligible participants were enrolled26 and one study used a sample size that was adequate to provide confidence in the findings (evidence that the sample size achieved was consistent with a statistical power analysis.38 None of the studies measured outcomes at specified intervals across the study. All but two studies26 38 used outcome measures that had been assessed for reliability and validity. All but two studies26 27 used inferential statistical methods to examine changes in outcomes. There were substantial lost to follow-up of greater than 20% reported in 11 studies.26–29 31 32 34 36 38–40 For four studies, there was insufficient data to calculate a percentage lost to follow-up.30 35 37 42
The randomised controlled trial33 scored 20 out of a maximum of 22 points. A potential source for bias was performance and ascertainment as the allocation to groups was not concealed from the interventionists, although in the context of social prescribing interventions this is difficult to achieve.
The matched groups design study41 was found overall to have a moderate level of bias. The bias due to confounding preintervention and selection of participants into the study was judged as being moderate and low, respectively. Bias in classification of interventions was also judged to be low. Bias due to missing, measurement of outcomes and selection of the report results were all judged to be moderate.
Fidelity assessment
A summary table presenting the treatment fidelity assessment of the included interventions and sources of information used is presented in online supplemental material 4.
bmjopen-2021-060214supp004.pdf (75.1KB, pdf)
Design of the study
All 13 intervention’s provided sufficient information to establish use of treatment fidelity strategies for intervention design to ensure the same dose of the intervention had been delivered within conditions.26–42 None of the intervention’s reported any explicit evidence that they had planned for implementation setbacks (eg, sufficient numbers of link workers being recruited to meet future demand).
Monitoring and improving provider training
Seven interventions (Art Shine,30 Cadwyn Mon,31 Cares of Life Project,33 Fife Social Prescribing Mood Café,34 Southwest Well-being Programme,40unnamed intervention41 and Wetlands for Well-being42) provided evidence that they provided standardised training for providers (ie, training was developed specifically for the purpose of intervention delivery). Two interventions (Art Shine30 and Southwest Well-being Programme)40 accommodated and tailored training to address provider differences in delivery (ie, rotations or specific role placement) and targeted acquisition of skills by providers (eg, follow-up sessions with service/research leads). One intervention (Art Shine)30 minimised drift in provider skills over time by monitoring and reviewing delivery on a monthly basis.
Monitoring and improving delivery of interventions
Four interventions (Art Lift,26–29 Art Shine,30 Cadwyn Mon,32 GROW: Art. Park and Well-being)35 provided sufficient information to suggest they controlled for provider differences by using strategies such as rotating sessions attended or offering a range of activities. One intervention (GROW: Art. Park and Well-being)35 explicitly reported monitoring adherence to a protocol. One intervention (Art Shine)30 explicitly reported strategies to reduce differences within interventions.
Monitoring and improving receipt of interventions and enactment of intervention skills
All 13 interventions reported information regarding service users’ comprehension of the intervention. Due to the nature of social prescribing interventions being tailored to the individual and their specific needs, the specific skills that would be targeted by the interventions is difficult to assess. Similarly, and further due to the absence of long- term follow-up assessments after the intervention period, this prohibited a robust assessment of enactment of intervention skills after the intervention activity had ended.
Person-centredness
A summary table of the assessment of person-centredness of the 13 interventions is presented in online supplemental material 5.
bmjopen-2021-060214supp005.pdf (75.9KB, pdf)
Eight interventions (BRC Connecting Communities,31 Cadwyn Mon,32 Cares of Life Project,33 GROW: Art, Park and Well-being,35 Luton Social Prescribing Programme,36 Social Cure and Social Prescribing,38 39 Southwest Well-being Programme40 and unnamed intervention)41 provided evidence that a personal needs assessment with service users was undertaken to discuss their needs and goals. Six interventions (Art Lift,26–29 Cadwyn Mon,32 Cares of Life Project,33 Fife Social Prescribing: Mood Café,34 GROW: Art, Park and Well-being,35 Luton Social Prescribing Programme,36 Southwest Well-being Programme)40 explicitly stated that service users were offered a choice of social prescribing interventions. Three interventions (Luton Social Prescribing Programme,36 Southwest Well-being Programme40 and Wetlands for Well-being)42 provided explicit evidence that service users were actively involved in discussions to elicit their preferences/values on the available social prescribing options. None of the included interventions provided any explicit evidence they ensured service users received a social prescription that was consistent with their preferences.
Overall, three interventions (Art Shine,30 Museums on Prescription37 and Wetlands for Well-being)42 did not report any explicit evidence that any core components of person-centred care were adopted. None of the 13 interventions provided any explicit evidence for all four components of person-centred care.
Intervention development processes
A summary table of the intervention development processes is presented in online supplemental material 6.
bmjopen-2021-060214supp006.pdf (77.8KB, pdf)
Eight interventions (Art Lift,26–29 BRC Connecting Communities,31 Cadwyn Mon,32 Cares of Life Project,33 Fife Social Prescribing: Mood Café,34 GROW: Art, Park and Well-being,35 Museums on Prescription,37 and Southwest Well-being Programme)40 provided explicit evidence they had used the best available evidence in the development (eg, systematic reviews, previous research, previous piloting). Eight interventions (Art Lift,26–29 BRC Connecting Communities,31 Cadwyn Mon,32 Cares of Life Project,33 Fife Social Prescribing: Mood Café,34 Luton Social Prescribing Programme,36 Southwest Well-being Programme40 and unnamed intervention)41 explicitly referred to conducting a population needs assessment to inform intervention development. Four interventions (Art Lift,26–29 Art Shine,30 Fife Social Prescribing: Mood Café,34 and Luton Social Prescribing Programme)36 provided explicit evidence of usability testing or feasibility testing/piloting of the intervention; however, one interventions explicitly reported they were in the pilot stage (unnamed intervention).41
Two interventions provided explicit evidence for the use of a framework to underpin development and evaluation. Cares of Life33 used the Medical Research Council Framework for The Development and Evaluation of Complex Interventions.73 The Social Cure and Social Prescribing38 39 used the Social Cure Framework.74 None of the 13 included interventions provided evidence of the use a theory or model of behaviour change to underpin the development of the intervention. Two interventions (Fife Social Prescribing: Mood Café34 and Southwest Well-being Programme)40 provided evidence of the use of a co-design/production process, working with service users in the codesign of interventions.
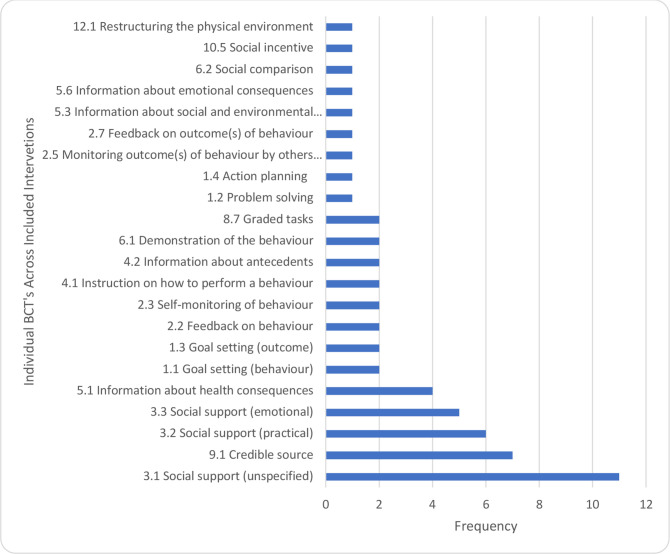
Behaviour change techniques
A total of 22 different BCTs (figure 2) were reported across the 13 interventions. The most frequently coded BCT was social support-unspecified (eg, social support from link workers, friends or relatives)(n=11), followed by credible source (eg, healthcare professional) (n=7), social support-practical (eg, advise on, arrange or provide practical help) (n=6) and social support-emotional (eg, providing support with feelings and emotions) (n=5).
Figure 2.
Frequency of individual BCT’s across included interventions. BCT, behaviour change techniques.
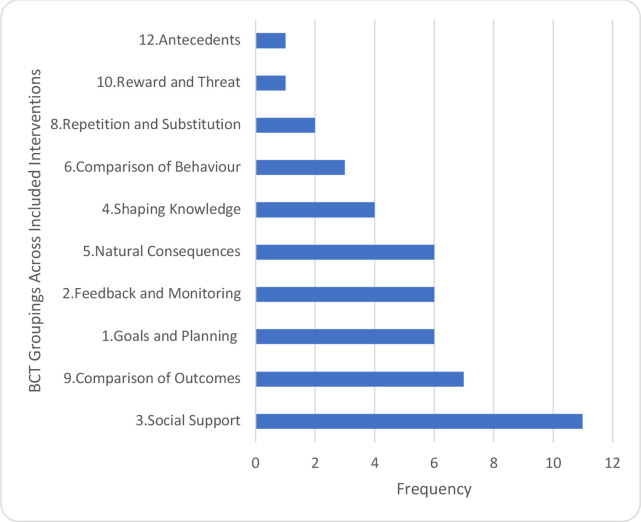
Individual BCTs were categorised into 10 groupings (figure 3) in accordance with the published taxonomy.16 The most common groupings were social support (n=11); comparison of outcomes (n=7), goals and planning; feedback and monitoring; and natural consequences (all n=6).
Figure 3.
Frequency of BCT groupings across the included interventions. BCT, behaviour change technique.
A promise ratio analysis was planned for the coded BCTs and other intervention features; however, this was not feasible due to the preponderance of positive outcomes (17 of the 18 studies all reported statistically significant improvements in outcomes).
Discussion
Summary of findings
This systematic review identified 13 UK-based social prescribing interventions reported across 17 studies, which most-commonly used a link worker model or direct referral from community services, for predominately working-age adults living with common mental health conditions (anxiety and depression). All but one study reported a statistically significant improvement in outcomes (mental well-being, mental health, loneliness and/or general health/ quality of life outcomes). Consistent with previous research,75–77 two studies38 41 in the current review reported reductions in primary healthcare use (consultation rates and medication prescribed). However, these findings should be interpreted with caution. Consistent with previous reviews of social prescribing interventions,4 8 9 75 the majority (15 out of 17) of the included studies were uncontrolled before-and-after studies (with a range of methodological shortcomings). Attrition rates were generally high (mean of 38%) and there was substantial variability in outcome measures. Furthermore, there was a lack of long-term follow-up studies.
Person-centredness is one of the key pillars of social prescribing for empowering the person to improve their own health.78 None of the included interventions in this review reported evidence of adhering to all four core principles of person-centred care.
Ethnicity of participants was under-reported across the studies in the current review. Based on five studies the proportions of White or White British participants ranged from 58%31 to 91%.40 The current Consensus data reports the UK population to be 86% White, 8% Asian, 3% Black and 2% mixed/multiple Ethnic groups.79
Only two interventions reported using a specific framework for design and evaluation of social prescribing interventions—the Medical Research Council Framework For The Development And Evaluation Of Complex Interventions73 and the Social Cure Framework.74 There was a lack of explicit evidence of service user involvement in codesign activity and usability or feasibility testing of interventions. This could lead to suboptimal acceptability and engagement with social prescribing interventions.
Treatment fidelity strategies are critically important for external validity of interventions. Evidence from this review indicated several shortcomings in this regard. However, due to the nature of social prescribing interventions (ie, highly tailored to individuals and their circumstances), the findings of the fidelity assessment should be interpreted with caution. There is no published guidance for assessing fidelity of social prescribing interventions. For example, it is not clear what cognitive and behavioural skills social prescribing interventions are targeting and how these can be assessed in terms of receipt and enactment by participants.
The most common BCT groupings identified were: social support (BCTs—social support-unspecified/ practical/ emotional); comparison of outcomes (BCTs—credible source); goals and planning (BCTs—goal setting (behaviour), problem solving, goal setting (outcome), and action planning); feedback and monitoring (BCTs—feedback on behaviour, self-monitoring of behaviour, monitoring of behaviour by others without feedback, feedback on outcome of behaviour); and natural consequences (BCTs—information about health consequences, information about social and environmental consequences, information about emotional consequences). The importance of identifying and reporting on BCTs used when developing/delivering interventions is important to further understanding and to facilitate replicability.80–82
Given the lack of detail provided by the studies of social prescribing interventions in the review, and that 16 out of 17 studies reported statistically significant improvements in outcomes, we were unable to conduct promise calculations (summing promising interventions (reported positive results) that includes a specific active ingredient of interest, for example different models of social prescribing, and dividing this by the number of non-promising interventions (reporting negative results or no change) featuring the same active ingredient) to explore further the active ingredients of effective social prescribing interventions.
Limitations
Several limitations of this review need to be acknowledged. There continues to be a debate about what constitutes a social prescribing intervention, and this will be reflected in published literature. Therefore, the existence of additional studies that would have met our inclusion criteria cannot be ruled out. Findings of the review are also limited by the descriptions of interventions reported within the included studies (ie, most social prescribing pathways/interventions were not described in detail), which impacts on conclusions about intervention development processes, person-centredness, treatment fidelity and BCTs. Improved quality of reporting on social prescribing models and interventions with reference to a published BCT taxonomy16 would help address this issue.
Future research
It is critical that complex interventions are underpinned by a structured development process involving service users and providers in a codesign activity with reference to appropriate evidence and theory. Future research should prioritise the application of theory to the design and evaluation of interventions to help identify the optimal theoretical approach to underpin social prescribing interventions for specific outcomes.
Future research on social prescribing interventions for mental health (and more broadly) would benefit from systematic evaluation of single and clustered BCTs (alongside improvements in the quality of reporting on intervention descriptions). This would optimise the design and delivery of social prescribing interventions across the entire pathway (eg, from initial contract with a primary care link worker to first appointment with the service providing socially prescribed activities). Interventions could subsequently be tailored for individuals living with mental health conditions to improve person-centred outcomes. Cross-disciplinary reviews have identified the use of BCT clusters including goal planning, feedback and monitoring, social support, and comparison of outcomes, are associated with effectiveness for improving physical activity, mental health seeking behaviour and employee mental health.80–82 In addition, these reviews have highlighted interventions using clusters of BCTs focused on shaping knowledge and comparison of behaviour and have shown improvements in mental health seeking behaviour.81
Despite variable rates of attrition across the studies included in this review, a few studies reported reasons for service users’ disengaging from social prescribing. This warrants attention and further investigation in future research, as well as a more detailed understanding of why a high proportion of those referred to social prescribing interventions fail to engage. Both emphasise the need to engage service users in the design and evaluation of social prescribing interventions with a focus on principles of person-centred care. In addition, this review has further highlighted the lack of long-term follow-up within social prescribing studies. Future research would benefit from evaluations to establish the long-term impact of social prescribing on service users’ mental health, including specific skills targeted by social prescribing interventions to improve fidelity assessment.
The narrative synthesis presented in the review is based on data aggregated across the referral pathways adopted by studies. Therefore, future research should conceptualise social prescribing interventions as complex multifacetted interventions. There are different referral pathways for social prescribing, including outside of primary care settings,83 and the specific contact points (eg, initial assessment, interaction with a facilitator or link worker and receipt/ delivery or socially prescribing activity) need to be considered as sperate, but linked facets of a complex multi-faceted intervention involving interactions between healthcare professionals and service users.
Conclusions
The predominance of before-and-after studies and associated methodological concerns, suboptimal development processes, and limited evidence of treatment fidelity assessments, prevents any robust conclusions on the effectiveness of social prescribing for mental health-related outcomes. Development of future social prescribing interventions would benefit from comprehensive development processes with reference to appropriate frameworks, theories or models (alongside detailed reporting of social prescribing referral pathways), including long-term outcome assessment and adherence to principles of person-centred care.
Supplementary Material
Footnotes
Twitter: @coopermatt7, @healthpsychleah, @drjasonscott
Contributors: MC and DF conceived the review. DF, LA and JS supervised the review. KA, CJ and JS assisted MC with study selection, and methodological quality assessment. MC, KA, DF and LA conducted data extraction. LE designed the search strategy, ran all searches, and collated search results. MC drafted the initial manuscript. All authors revised the manuscript for important intellectual content and approved the final version. DF is the guatantor of this work.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1.Hassan SM, Giebel C, Morasae EK, et al. Social prescribing for people with mental health needs living in disadvantaged communities: the life rooms model. BMC Health Serv Res 2020;20:1–9. 10.1186/s12913-019-4882-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.England N. Social prescribing, 2019. Available: https://www.england.nhs.uk/contact-us/privacy-notice/how-we-use-yourinformation/public-and-partners/social-prescribing/ [Accessed 01 Mar 2020].
- 3.England N. NHS long term plan, 2019. Available: https://www.longtermplan.nhs.uk/ [Accessed 10 Feb 2021].
- 4.Chatterjee HJ, Camic PM, Lockyer B, et al. Non-clinical community interventions: a systematised review of social prescribing schemes. Arts Health 2018;10:97–123. 10.1080/17533015.2017.1334002 [DOI] [Google Scholar]
- 5.Moffatt S, Steer M, Lawson S, et al. Link worker social prescribing to improve health and well-being for people with long-term conditions: qualitative study of service user perceptions. BMJ Open 2017;7:e015203. 10.1136/bmjopen-2016-015203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.White M, Salamon E. An interim evaluation of the ‘Arts For Well-being’social prescribing scheme in County Durham. Centre for Medical Humanities: Durham University, 2010. [Google Scholar]
- 7.Kimberlee R. What is social prescribing? Adv Soc Sci Res J 2015;2. 10.14738/assrj.21.808 [DOI] [Google Scholar]
- 8.Husk K, Blockley K, Lovell R, et al. What approaches to social prescribing work, for whom, and in what circumstances? A realist review. Health Soc Care Community 2020;28:309–24. 10.1111/hsc.12839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bradley G, Scott J, Nomenclature SP. Occupational therapy and the theory of institutional work: creating, maintaining and disrupting medical dominance. Occup Ther Health Care 2021:1–14. 10.1080/07380577.2021.1926046 [DOI] [PubMed] [Google Scholar]
- 10.McManus S, Bebbington P, Jenkins R, et al. Mental health and wellbeing in England: adult psychiatric morbidity survey 2014. NHS Digital: Leeds, 2016. [Google Scholar]
- 11.McDaid D, A-La Park A-L, Davidson G, et al. The economic case for investing in the prevention of mental health conditions in the UK. London School of Economics and Political Science / Mental Health Foundation, 2022. [Google Scholar]
- 12.Bickerdike L, Booth A, Wilson PM, et al. Social prescribing: less rhetoric and more reality. A systematic review of the evidence. BMJ Open 2017;7:e013384. 10.1136/bmjopen-2016-013384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cooper M, Ashley K, Jordan C. Active ingredients in social prescription interventions for adults with mental health issues: a systematic review. In: Protocol. PROSPERO 2020 CRD42020167887 2020, 2020. [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Collaboration C, Training C. Template for intervention description and replication (TIDieR)
- 16.Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (V1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81–95. 10.1007/s12160-013-9486-6 [DOI] [PubMed] [Google Scholar]
- 17.Santana MJ, Manalili K, Jolley RJ, et al. How to practice person-centred care: a conceptual framework. Health Expect 2018;21:429–40. 10.1111/hex.12640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McCormack B, Dewing J, McCance T. Developing person-centred care: addressing contextual challenges through practice development. Online J Issues Nurs 2011;16:3. 10.3912/OJIN.Vol16No02Man03 [DOI] [PubMed] [Google Scholar]
- 19.Moore L, Britten N, Lydahl D, et al. Barriers and facilitators to the implementation of person-centred care in different healthcare contexts. Scand J Caring Sci 2017;31:662–73. 10.1111/scs.12376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Flynn D, Knoedler MA, Hess EP, et al. Engaging patients in health care decisions in the emergency department through shared decision-making: a systematic review. Acad Emerg Med 2012;19:959–67. 10.1111/j.1553-2712.2012.01414.x [DOI] [PubMed] [Google Scholar]
- 21.Bellg AJ, Borrelli B, Resnick B, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH behavior change Consortium. Health Psychol 2004;23:443. 10.1037/0278-6133.23.5.443 [DOI] [PubMed] [Google Scholar]
- 22.Checklist CAS. CASP RCT checklist, 2018. Available: https://casp-uk.net/casp-tools-checklists/ [Accessed 05 Jan 2020].
- 23.NHLBI R. Quality assessment tool for before-after (pre-post) studies. Available: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools [Accessed 05 Jan 2020].
- 24.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355:i4919. 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moore SA, Hrisos N, Flynn D, et al. How should long-term free-living physical activity be targeted after stroke? A systematic review and narrative synthesis. Int J Behav Nutr Phys Act 2018;15:1–19. 10.1186/s12966-018-0730-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Crone DM, O'Connell EE, Tyson PJ, et al. 'Art lift' intervention to improve mental well-being: an observational study from U.K. general practice. Int J Ment Health Nurs 2013;22:279–86. 10.1111/j.1447-0349.2012.00862.x [DOI] [PubMed] [Google Scholar]
- 27.Crone DM, Sumner RC, Baker CM, et al. 'Artlift' arts-on-referral intervention in UK primary care: updated findings from an ongoing observational study. Eur J Public Health 2018;28:404–9. 10.1093/eurpub/cky021 [DOI] [PubMed] [Google Scholar]
- 28.Sumner RC, Crone DM, Baker C, et al. Factors associated with attendance, engagement and wellbeing change in an arts on prescription intervention. J Public Health 2019;130:e88–95. 10.1093/pubmed/fdz032 [DOI] [PubMed] [Google Scholar]
- 29.Sumner RC, Crone DM, Hughes S, et al. Arts on prescription: observed changes in anxiety, depression, and well-being across referral cycles. Public Health 2021;192:49–55. 10.1016/j.puhe.2020.12.008 [DOI] [PubMed] [Google Scholar]
- 30.van de Venter E, Buller A. Arts on referral interventions: a mixed-methods study investigating factors associated with differential changes in mental well-being. J Public Health 2015;37:143–50. 10.1093/pubmed/fdu028 [DOI] [PubMed] [Google Scholar]
- 31.Foster A, Thompson J, Holding E, et al. Impact of social prescribing to address loneliness: a mixed methods evaluation of a national social prescribing programme. Health Soc Care Community 2021;29:1439–49. 10.1111/hsc.13200 [DOI] [PubMed] [Google Scholar]
- 32.Roberts JR, Windle G. Evaluation of an intervention targeting loneliness and isolation for older people in North Wales. Perspect Public Health 2020;140:153–61. 10.1177/1757913919868752 [DOI] [PubMed] [Google Scholar]
- 33.Afuwape SA, Craig TKJ, Harris T, et al. The cares of life project (CoLP): an exploratory randomised controlled trial of a community-based intervention for black people with common mental disorder. J Affect Disord 2010;127:370–4. 10.1016/j.jad.2010.05.017 [DOI] [PubMed] [Google Scholar]
- 34.Morton L, Ferguson M, Baty F. Improving wellbeing and self-efficacy by social prescription. Public Health 2015;129:286–9. 10.1016/j.puhe.2014.12.011 [DOI] [PubMed] [Google Scholar]
- 35.Thomson LJ, Morse N, Elsden E, et al. Art, nature and mental health: assessing the biopsychosocial effects of a 'creative green prescription' museum programme involving horticulture, artmaking and collections. Perspect Public Health 2020;140:277–85. 10.1177/1757913920910443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pescheny JV, Gunn LH, Pappas Y. The impact of the Luton social prescribing programme on mental well-being: a quantitative before-and-after study. J Public Health 2019;27:e69–76. 10.1093/pubmed/fdz155 [DOI] [PubMed] [Google Scholar]
- 37.Thomson LJ, Lockyer B, Camic PM, et al. Effects of a museum-based social prescription intervention on quantitative measures of psychological wellbeing in older adults. Perspect Public Health 2018;138:28–38. 10.1177/1757913917737563 [DOI] [PubMed] [Google Scholar]
- 38.Kellezi B, Wakefield JRH, Stevenson C, et al. The social cure of social prescribing: a mixed-methods study on the benefits of social connectedness on quality and effectiveness of care provision. BMJ Open 2019;9:e033137. 10.1136/bmjopen-2019-033137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wakefield JRH, Kellezi B, Stevenson C, et al. Social prescribing as 'Social Cure': a longitudinal study of the health benefits of social connectedness within a Social Prescribing pathway. J Health Psychol 2022;27:386–96. 10.1177/1359105320944991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jones M, Kimberlee R, Deave T, et al. The role of community centre-based arts, leisure and social activities in promoting adult well-being and healthy lifestyles. Int J Environ Res Public Health 2013;10:1948–62. 10.3390/ijerph10051948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Carnes D, Sohanpal R, Frostick C, et al. The impact of a social prescribing service on patients in primary care: a mixed methods evaluation. BMC Health Serv Res 2017;17:1–9. 10.1186/s12913-017-2778-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Maund PR, Irvine KN, Reeves J, et al. Wetlands for wellbeing: Piloting a nature-based health intervention for the management of anxiety and depression. Int J Environ Res Public Health 2019;16:4413. 10.3390/ijerph16224413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Baker C, Crone D, Clark-Stone F. Art lift (extension), Gloucestershire: evaluation report. UK: University of Gloucestershire; 2013. [Google Scholar]
- 44.Loughren EA, Matthews J, Baker C. Artlift Gloucestershire: update report 2011-2014. UK: University of Gloucestershire; 2014. [Google Scholar]
- 45.Daykin N, McClean S, Pilkington P. Evaluation of Art Lift: A. UK: Partnership Arts and Health Project. University of Glouchestershire, 2008. [Google Scholar]
- 46.van de Venter E, Newman L, NHS Bristol . Arts on referral for inner City Bristol: evaluation report. Bristol, UK: NHS Bristol; 2011. https://www.ahsw.org.uk/wp-content/uploads/2019/07/Artshine_Evaluation.pdf [Accessed 01 May 2022]. [Google Scholar]
- 47.Arts on Referral . Available: http://www.artsonreferral.org [Accessed 01 May 2022].
- 48.Holding E, Thompson J, Foster A, et al. Connecting communities: a qualitative investigation of the challenges in delivering a national social prescribing service to reduce loneliness. Health Soc Care Community 2020;28:1535–43. 10.1111/hsc.12976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Partnership C-op. Available: https://www.redcross.org.uk/get-involved/partner-with-us/co-op [Accessed 01 May 2022].
- 50.Tackling Loneliness Together . British red cross and Co-op end of partnership report. Available: https://www.redcross.org.uk/get-involved/partner-with-us/co-op [Accessed 01 May 2022].
- 51.Café M. Available: https://www.moodcafe.co.uk [Accessed 01 May 2022].
- 52.Not So Grim Up North (GROW) Report . Available: https://www.artshealthresources.org.uk/docs/not-so-grim-up-north/ [Accessed 01 May 2022].
- 53.Pescheny JV, Pappas Y, Randhawa G. Evaluating the implementation and delivery of a social prescribing intervention: a research protocol. Int J Integr Care 2018;18:13. 10.5334/ijic.3087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pescheny JV. An evaluation of the implementation and practice of social prescribing, 2019. [Google Scholar]
- 55.Pescheny JV, Gunn LH, Randhawa G, et al. The impact of the Luton social prescribing programme on energy expenditure: a quantitative before-and-after study. BMJ Open 2019;9:e026862. 10.1136/bmjopen-2018-026862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Halder MM, Wakefield JR, Bowe M, et al. Evaluation and exploration of a social prescribing initiative: study protocol. J Health Psychol 2021;26:345–56. 10.1177/1359105318814160 [DOI] [PubMed] [Google Scholar]
- 57.Westbank HLC . South West healthy living alliance strategy. Devon, UK, 2009. [Google Scholar]
- 58.Tennant R, Hiller L, Fishwick R, et al. The Warwick-Edinburgh mental well-being scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5:1–13. 10.1186/1477-7525-5-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Russell DW. UCLA loneliness scale (version 3): reliability, validity, and factor structure. J Pers Assess 1996;66:20–40. 10.1207/s15327752jpa6601_2 [DOI] [PubMed] [Google Scholar]
- 60.de Jong-Gierveld J, Kamphuls F. The development of a Rasch-type loneliness scale. Appl Psychol Meas 1985;9:289–99. 10.1177/014662168500900307 [DOI] [Google Scholar]
- 61.Lubben J, Blozik E, Gillmann G, et al. Performance of an abbreviated version of the Lubben social network scale among three European community-dwelling older adult populations. Gerontologist 2006;46:503–13. 10.1093/geront/46.4.503 [DOI] [PubMed] [Google Scholar]
- 62.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- 63.Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092–7. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 64.Kroenke K, Strine TW, Spitzer RL, et al. The PHQ-8 as a measure of current depression in the general population. J Affect Disord 2009;114:163–73. 10.1016/j.jad.2008.06.026 [DOI] [PubMed] [Google Scholar]
- 65.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977;1:385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- 66.Goldberg DP, Hillier VF. A scaled version of the general health questionnaire. Psychol Med 1979;9:139–45. 10.1017/s0033291700021644 [DOI] [PubMed] [Google Scholar]
- 67.Hall RC. Global assessment of functioning. A modified scale. Psychosomatics 1995;36:267–75. 10.1016/S0033-3182(95)71666-8 [DOI] [PubMed] [Google Scholar]
- 68.Diener E, Emmons RA, Larsen RJ, et al. The satisfaction with life scale. J Pers Assess 1985;49:71–5. 10.1207/s15327752jpa4901_13 [DOI] [PubMed] [Google Scholar]
- 69.EuroQol Group . EuroQol--a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199–208. 10.1016/0168-8510(90)90421-9 [DOI] [PubMed] [Google Scholar]
- 70.Jenkinson C, Coulter A, Wright L. Short form 36 (SF36) health survey questionnaire: normative data for adults of working age. BMJ 1993;306:1437–40. 10.1136/bmj.306.6890.1437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cohen S, Kamarck T, Mermelstein R. Perceived stress scale. In: Measuring stress: a guide for health and social scientists 10, 1994: 1–2. [Google Scholar]
- 72.Watson D, Clark LA. The PANAS-X: manual for the positive and negative affect schedule-expanded form, 1999. [Google Scholar]
- 73.Council MR . Developing and evaluating complex interventions: new guidance. Medical Research Council, 2008. [Google Scholar]
- 74.Haslam C, Jetten J, Cruwys T. The new pscyhology of health. Unlocking the social cure. London: Routledge, 2018. [Google Scholar]
- 75.Polley M, Pilkington K. A review of the evidence assessing impact of social prescribing on healthcare demand and cost implications, 2017. Available: https://westminsterresearch.westminster.ac.uk/item/q1455/a-review-of-the-evidence-assessing-impact-of-social-prescribing-on-healthcare-demand-and-cost-implications [Accessed 14 Sep 2021].
- 76.Longwill A. Independent evaluation of Hackney WellFamily service. In: Improving health and wellbeing UK, 2014. [Google Scholar]
- 77.Brandling J, House W. Social prescribing in general practice: adding meaning to medicine. Br J Gen Pract 2009;59:454–6. 10.3399/bjgp09X421085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Polley M, Whiteside J, Elnaschie S. What does successful social prescribing look like? In: Mapping meaningful outcomes. London University of Westminster, 2020. [Google Scholar]
- 79. Gov.UK. Population of England and Wales 01/08/2018, 2018. Available: https://www.ethnicity-facts-figures.service.gov.uk/uk-population-by-ethnicity/national-and-regional-populations/population-of-england-and-wales/latest [Accessed 14 Sep 2021].
- 80.French DP, Olander EK, Chisholm A, et al. Which behaviour change techniques are most effective at increasing older adults' self-efficacy and physical activity behaviour? A systematic review. Ann Behav Med 2014;48:225–34. 10.1007/s12160-014-9593-z [DOI] [PubMed] [Google Scholar]
- 81.Sagar-Ouriaghli I, Godfrey E, Bridge L, et al. Improving mental health service utilization among men: a systematic review and synthesis of behavior change techniques within interventions targeting help-seeking. Am J Mens Health 2019;13:1557988319857009. 10.1177/1557988319857009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.de Korte E, Wiezer N, Bakhuys Roozeboom M, Roozeboom MB, et al. Behavior change techniques in mHealth apps for the mental and physical health of employees: systematic assessment. JMIR Mhealth Uhealth 2018;6:e167. 10.2196/mhealth.6363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Scott J, Fidler G, Monk D, et al. Exploring the potential for social prescribing in pre-hospital emergency and urgent care: a qualitative study. Health Soc Care Community 2021;29:654–63. 10.1111/hsc.13337 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-060214supp001.pdf (52.1KB, pdf)
bmjopen-2021-060214supp002.pdf (80.2KB, pdf)
bmjopen-2021-060214supp003.pdf (145.4KB, pdf)
bmjopen-2021-060214supp004.pdf (75.1KB, pdf)
bmjopen-2021-060214supp005.pdf (75.9KB, pdf)
bmjopen-2021-060214supp006.pdf (77.8KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information.