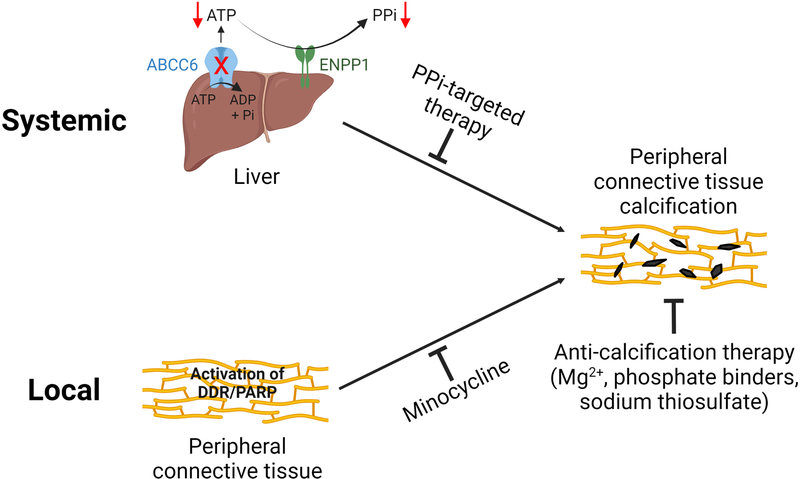
Figure 6. Proposed pathomechanisms of PXE – both systemic and local factors contribute to ectopic calcification in PXE.
The metabolic nature of PXE is supported by the reduced circulating concentrations of PPi, a potent endogenous inhibitor of calcification. Systemic PPi deficiency in PXE is caused by the reduced ABCC6 transport activity in hepatocytes, reducing the extracellular ATP pool which serves as substrate for ENPP1, an ectonucleotidase/pyrophophotase 1, to generate PPi. Targeted therapies to raise plasma PPi levels have been shown to be effective to counteract ectopic calcification in murine models of PXE. On the other hand, local activation of DNA damage response and PAR deposition triggers ectopic calcification in peripheral connective tissues. Minocycline, a potent inhibitor of DDR/PAR, prevents ectopic calcification in PXE. Collectively, both systemic and local factors contribute to the pathogenesis of ectopic calcification in PXE. The potential interaction between these two pathways cannot be excluded. Furthermore, other anti-calcification therapies such as magnesium, phosphate binders, and sodium thiosulfate have therapeutic effects on ectopic calcification independent of the underlying pathomechanisms of PXE.