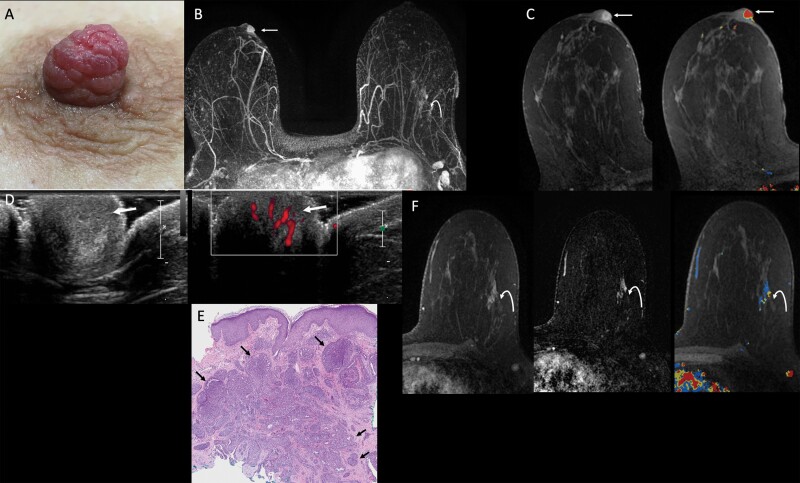
Figure 1.
Images of a 54-year-old female with a six-month history of spontaneous bloody right nipple discharge following poor healing of a nipple laceration. After initial mammographic and sonographic evaluation failed to show an etiology for the bloody discharge, she was referred for MRI. A: Clinical photograph demonstrates a prominent right nipple with hyperemic “raspberry-like” distortion of the nipple. B: Axial maximum intensity projection (MIP) image of first post-contrast MRI subtraction shows asymmetric strong enhancement of the right nipple (arrow) and non-mass enhancement in the outer left breast (curved arrow). C: Axial T1-weighted, fat-suppressed first post-contrast breast MRI shows a rim-enhancing 10-mm oval mass in the right nipple (left, arrow) with washout kinetics (right, arrow). D: MRI-directed transverse US of the right nipple (left) demonstrates a subtle, slightly hypoechoic, heterogeneous, 1-cm, ovoid mass within the right nipple (arrow), with internal vascularity on power Doppler (right, arrow). E: Histopathology (hematoxylin and eosin, 4x) from punch biopsy shows proliferating ductal structures with usual ductal hyperplasia consistent with nipple adenoma (arrows). Myoepithelial cell nuclei (which can be highlighted with immunohistochemical stain for p63) surround each individual ductal structure. F: Axial T1-weighted, fat-suppressed contrast-enhanced breast MRI with kinetic overlay better demonstrates a 3.3-cm linear non-mass enhancement in the outer left breast (curved arrow). The patient underwent MRI-guided biopsy, followed by breast-conserving surgery, with final pathology demonstrating two foci of invasive lobular carcinoma, measuring 1.6 cm and 0.8 cm, on a background of lobular carcinoma in situ. Two left axillary lymph nodes were negative for carcinoma. Surgical pathology from the right nipple confirmed nipple adenoma.