Abstract
The coronavirus disease 2019 (COVID-19) pandemic has a disproportionate impact on vulnerable subpopulations, including those with severe mental illness (SMI). This study examined the one-year prevalence of suicidal ideation (SI), suicide plans (SP), and suicide attempts (SA) in bipolar disorder (BD) and schizophrenia (SCZ) patients during the pandemic. Prevalence rates were compared between the two disorders and associated factors were examined. A survey was conducted in six tertiary psychiatric hospitals and psychiatric units. People with a diagnosis of BD or SCZ were invited to participate. SI, SP, and SA (suicidality for short) were assessed and associated factors were examined using binary logistical regression. The 1-year prevalence of SI, SP and SA in BD patients were 58.3%, (95% CI: 54.1–62.6%), 38.4% (95% CI: 34.3–42.6%) and 38.6% (95% CI: 34.5–42.8%), respectively, which were higher than the corresponding figures in SCZ patients (SI: 33.2%, 95% CI: 28.6–37.8%; SP: 16.8%, 95% CI: 13.2–20.5%; SA: 19.4%, 95% CI: 15.5–23.3%). Patients with younger age, experience of cyberbullying, a history of SA among family or friends, a higher fatigue and physical pain score, inpatient status, and severe depressive symptoms were more likely to have suicidality. The COVID-19 pandemic was associated with increased risk of suicidality, particularly in BD patients. It is of importance to regularly screen suicidality in BD and SCZ patients during the pandemic even if they are clinically stable.
Subject terms: Schizophrenia, Bipolar disorder
Introduction
Suicide is a serious public health concern, and about 703,000 people worldwide died by suicide in 2019 [1]. It is one of the leading causes of death globally, with more than one in every 100 deaths (1.3%) caused by suicide [1]. Although China is one of the countries with the lowest suicide rates, China accounts for about one-sixth of suicide deaths worldwide [1]. Suicidality can be conceptualized as a continuum of thoughts and actions, from mild to severe, including suicidal ideation (SI), suicide planning (SP), suicide attempts (SA), and suicide deaths [2]. Non-fatal suicidality (i.e., SI, SP, and SA) is a strong predictor of subsequent suicide death [3]. A previous meta-analysis reported that the lifetime prevalence (95% CI) of SI and SA in China’s general population were 3.9% (2.5–6.0%) and 0.8% (0.7–0.9%), respectively [4]. Several factors are known to increase suicide risk including a previous SA, a family history of suicide and maltreatment, alcohol or drug abuse, and mental disorders [5–9].
Compared to those with no psychiatric disorders, individuals with severe mental illness (SMI) are more likely to commit suicide [10, 11]. In particular, both bipolar disorder (BD) and schizophrenia (SCZ) patients have higher rates of suicidality [11, 12]. Previous meta-analyses showed that the pooled lifetime and 1-year prevalence of SA in BD were 33.9% (95% CI: 31.3–36.6%), and 15.0% (95% CI: 8.2–21.8%), respectively [13]. In SCZ, the pooled lifetime prevalence of SI and SA were 34.5% (95% CI: 28.2−40.9%) and 26.8% (95% CI: 22.1–31.9%), respectively [14, 15]. Recent studies have suggested that the ongoing (COVID-19) pandemic might have increased suicidality in these susceptible populations [16, 17]. Measures intended to limit the spread of COVID-19, such as social distancing and lockdowns, may also decrease social support and increase loneliness [18], and increase maladaptive ways of coping [19]. Increased screen time, a higher consumption of junk food and alcohol, and tobacco smoking, may worsen the course of BD and SCZ [19, 20].
People with mental disorders have experienced disruptions in clinical care and medications as a result of travel restrictions and quarantine [21]. Moreover, the COVID-19 pandemic dramatically changed the landscape of care for patients with SMI. For instance, a survey involving seventeen regions of the world cautioned that the rise of telepsychiatry may limit psychiatric care opportunities for people without the technological means or aptitude [22]. COVID-19 has also led to overburdened healthcare professionals, compromising their mental health, which in turn results in suboptimal care for patients with mental disorders [23]. These factors may increase the risk of recurring affective episodes and/or suicidality in patients with BD or SCZ.
Financial challenges faced by patients brought about by COVID-19 may contribute to higher suicidality in BD and SCZ patients [24]. Recent studies found that a pre-existing SMI may increase the risk, severity, and mortality of COVID-19 infection [25]. Greater susceptibility to COVID-19 may worsen the stigma and isolation faced by BD and SCZ patients [26]—perhaps increasing suicidality. To the best of our knowledge, no study has examined suicidality in clinically stable BD and SCZ patients during the pandemic, although they account for majority of patients with these disorders.
Here, we examined and compared the 1-year prevalence of SI, SP, and SA in clinically stable BD and SCZ during the COVID-19 pandemic and identified factors associated with suicidality.
Methods
Participants and study site
This was a multicenter, cross-sectional study conducted in six tertiary psychiatric hospitals and psychiatric units in China between September 21, 2020 and October 8, 2021. In keeping with safety guidelines and following previous studies [27, 28], participants were assessed using the QuestionnaireStar program in the WeChat application. WeChat is a widely used social communication application in China and it was used for health monitoring during the pandemic. People entering hospitals are required to report their health status using a WeChat-generated code. We invited people visiting psychiatric units or admitted to psychiatric hospitals to participate in this study. Prospective participants scanned a Quick Response code (QR Code) that led to a study description and invitation. After providing electronic written informed consent, eligible patients were asked to complete a questionnaire. Participants were included if they were: (1) 18 years or above; (2) diagnosed with either BD or SCZ according to the International Classification of Diseases, Tenth Revision (ICD-10) [29]; (3) clinically stable as judged by their psychiatrists. Based on previous studies [30, 31], clinically stable patients were defined as those who had a less than 50% dose change in any main psychotropic medication in the last three months. These medications included antidepressants, mood stabilizers and antipsychotic medications. (4) able to read Chinese and understand the assessment questions. The study protocol received approval from the ethics committees of Beijing Anding Hospital and other participating hospitals.
Measurements
Socio-demographic data, including age, gender, urban or rural residence, marital status, education, living arrangement (with family members/others or alone), employment status, health insurance status, self-reported health and economic status, family history of psychiatric disorders, cyberbullying, suicide attempts or death among family members or friends (henceforth, family-or-friend SA), were collected with a pre-designed data collection form. Clinical characteristics, such as inpatient or outpatient status, age of illness onset, fatigue, physical pain, depressive symptoms, quality of life and suicidality, were also collected.
Fatigue severity was measured with a numeric rating scale [32] with an answer ranging from “0” (no fatigue) to ‘10’ (extreme fatigue). Physical pain was assessed with a Visual Analogue Scale for Pain (VAS) [33] with anchors at “0” (no pain at all) and “10” (worst pain imaginable). The validated Chinese version of the Patient Health Questionnaire-2 (PHQ-2) [34, 35] was used to measure the severity of residual depressive symptoms, with a total score ranging from 0 to 6 and a higher score indicating more severity. Global quality of life (QOL) was measured with the first 2 items of the World Health Organization Quality of Life Scale Brief version (WHOQOL-BREF) [36, 37]. Higher scores reflect higher QOL.
Participants were asked about suicidality with standard questions adapted from the National Comorbidity Survey [38]. These questions were answerable with yes or no: (1) SI: “Over the past year, have you thought that you would be better off dead?” (2) SP: “Over the past year, have you made a plan for suicide?” (3) SA: “Over the past year, have you made an attempt for suicide?” These questions on suicidality have been widely used in other studies [39, 40]
Statistical analysis
All analyses were performed using the R program [41]. Descriptive statistics (i.e., mean ± standard deviation (SD) for continuous variables and frequency counts (%) for categorical variables) summarized the participants’ socio-demographic and clinical characteristics. Continuous variables were examined for normality with the one-sample Kolmogorov-Smirnov test. Afterwards, univariate analyses (i.e., independent t tests, Mann–Whitney U tests, or Chi-square tests) were used to compare socio-demographic and disease-related variables between patients with and without suicidality within each diagnosis (i.e., BD/SCZ). We then examined if QOL differed between patients with and without suicidality by performing an analysis of covariance (ANCOVA), adjusting for variables in which the groups differed significantly in the univariate analyses. Within each diagnosis, binary logistic regression analysis was conducted to identify correlates of suicidality (SI, SP, and SA in separate models), adjusting for confounders. P < 0.05 (two-tailed) was set as the significance level.
Results
Out of 949 patients invited, 905 (95.3%) satisfied the study criteria and completed the assessment. 513 patients had BD (mean age: 29.64 ± 11.58 years; male proportion: 20.5%) and 392 had SCZ (mean age: 32.42 ± 11.34 years; male proportion: 41.8%). The complete socio-demographic and clinical characteristics of the sample are summarized in Table 1.
Table 1.
Socio-demographic and clinical characteristics of participants.
| Variables | Bipolar disorder (N = 513) | Schizophrenia (N = 392) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | SI | SP | SA | Total | SI | SP | SA | |||||||
| No (N = 214) | Yes (N = 299) | No (N = 316) | Yes (N = 197) | No (N = 315) | Yes (N = 198) | No (N = 262) | Yes (N = 130) | No (N = 326) | Yes (N = 66) | No (N = 316) | Yes (N = 76) | |||
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Male gender | 105 (20.5) | 46 (21.5) | 59 (19.7) | 73 (23.1) | 32 (16.2) | 71 (22.5) | 34 (17.2) | 164 (41.8) | 117 (44.7) | 47 (36.2) | 133 (40.8) | 31 (47.0) | 134 (42.4) | 30 (39.5) |
| Urban residents | 404 (78.8) | 167 (78.0) | 237 (79.3) | 251 (79.4) | 153 (77.7) | 250 (79.4) | 154 (77.8) | 225 (57.4) | 157 (59.9) | 68 (52.3) | 191 (58.6) | 34 (51.5) | 180 (57.0) | 45 (59.2) |
| Married | 172 (33.5) | 97 (45.3) | 75 (25.1)*** | 126 (39.9) | 46 (23.4)*** | 123 (39.0) | 49 (24.7)*** | 137 (34.9) | 98 (37.4) | 39 (30.0) | 123 (37.7) | 14 (21.2)* | 118 (37.3) | 19 (25.0)* |
| College and above | 323 (63.0) | 134 (62.6) | 189 (63.2) | 203 (64.2) | 120 (60.9) | 199 (63.2) | 124 (62.6) | 151 (38.5) | 106 (40.5) | 45 (34.6) | 129 (39.6) | 22 (33.3) | 126 (39.9) | 25 (32.9) |
| Living with family members | 417 (81.3) | 185 (86.4) | 232 (77.6)* | 263 (83.2) | 154 (78.2) | 264 (83.8) | 153 (77.3) | 353 (90.1) | 241 (92.0) | 112 (86.2) | 300 (92.0) | 53 (80.3)** | 287 (90.8) | 66 (86.8) |
| Unemployed | 311 (60.6) | 114 (53.3) | 197 (65.9)** | 176 (55.7) | 135 (68.5)** | 173 (54.9) | 138 (69.7)*** | 234 (59.7) | 154 (58.8) | 80 (61.5) | 193 (59.2) | 41 (62.1) | 187 (59.2) | 47 (61.8) |
| Health insurance | 413 (80.5) | 184 (86.0) | 229 (76.6)** | 262 (82.9) | 151 (76.6) | 262 (83.2) | 151 (76.3) | 321 (81.9) | 215 (82.1) | 106 (81.5) | 273 (83.7) | 48 (72.7)* | 261 (82.6) | 60 (78.9) |
| Inpatients | 126 (24.6) | 55 (25.7) | 71 (23.7) | 78 (24.7) | 48 (24.4) | 82 (26.0) | 44 (22.2) | 73 (18.6) | 50 (19.1) | 23 (17.7) | 54 (16.6) | 19 (28.8)* | 58 (18.4) | 15 (19.7) |
| Family history of psychiatric disorders | 96 (18.7) | 39 (18.2) | 57 (19.1) | 55 (17.4) | 41 (20.8) | 55 (17.5) | 41 (20.7) | 50 (12.8) | 30 (11.5) | 20 (15.4) | 40 (12.3) | 10 (15.2) | 28 (12.0) | 12 (15.8) |
| Cyberbullying | 103 (20.1) | 32 (15.0) | 71 (23.7)* | 43 (13.6) | 60 (30.5)*** | 48 (15.2) | 55 (27.8)*** | 95 (24.2) | 50 (19.1) | 45 (34.6)*** | 70 (21.5) | 25 (37.9)** | 79 (25.0) | 16 (21.1) |
| Family members or friends’ SA | 141 (27.5) | 23 (10.7) | 118 (39.5)*** | 48 (15.2) | 93 (47.2)*** | 47 (14.9) | 94 (47.5)*** | 51 (13.0) | 21 (8.0) | 30 (23.1)*** | 28 (8.6) | 23 (34.8)*** | 28 (8.9) | 23 (30.3)*** |
| Family members or friends’ suicide | 70 (13.6) | 24 (11.2) | 46 (15.4) | 33 (10.4) | 37 (18.8)** | 37 (11.7) | 33 (16.7) | 32 (8.2) | 16 (6.1) | 16 (12.3) * | 22 (6.7) | 10 (15.2)* | 22 (7.0) | 10 (13.2) |
| Perceived health status | ||||||||||||||
| Poor/Fair | 375 (73.1) | 138 (64.5) | 237 (79.3) | 216 (68.4) | 159 (80.7) | 214 (67.9) | 161 (81.3) | 286 (73.0) | 181 (69.1) | 105 (80.8) | 233 (71.5) | 53 (80.3) | 224 (70.9) | 62 (81.6) |
| Good | 138 (26.9) | 76 (35.5) | 62 (20.7)*** | 100 (31.6) | 38 (19.3)*** | 101 (32.1) | 37 (18.7)*** | 106 (27.0) | 81 (30.9) | 25 (19.2)*** | 93 (28.5) | 13 (19.7)*** | 92 (29.1) | 14 (18.4)*** |
| Perceived economic status | ||||||||||||||
| Poor/Fair | 455 (88.7) | 185 (86.4) | 270 (90.3) | 275 (87.0) | 180 (91.4) | 275 (87.3) | 180 (90.9) | 371 (94.6) | 248 (94.7) | 123 (94.6) | 309 (94.8) | 62 (93.9) | 300 (94.9) | 71 (93.4) |
| Good | 58 (11.3) | 29 (13.6) | 29 (9.7) | 41 (13.0) | 17 (8.6) | 40 (12.7) | 18 (9.1)* | 21 (5.4) | 14 (5.3) | 7 (5.4) | 17 (5.2) | 4 (6.1)* | 16 (5.1) | 5 (6.6) |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |
| Age (years)# | 29.64 (11.58) | 33.49 (11.77) | 26.89 (10.64)*** | 32.02 (11.81) | 25.83 (10.13)*** | 32.06 (11.73) | 25.79 (10.24)*** | 32.42 (11.34) | 33.65 (11.41) | 29.93 (10.82)*** | 33.41 (11.59) | 27.52 (8.48)*** | 33.31 (11.48) | 28.70 (9.99)*** |
| Age of onset (years)# | 24.79 (10.16) | 26.81 (25.00) | 23.27 (9.14)*** | 26.60 (10.81) | 21.89 (8.25)*** | 26.37 (10.91) | 22.28 (8.26)*** | 25.66 (9.41) | 26.29 (9.63) | 24.37 (8.86)* | 26.13 (9.55) | 23.32 (8.42)* | 26.31 (9.38) | 22.93 (9.11)*** |
| Fatigue# | 4.78 (2.89) | 3.50 (2.66) | 5.69 (2.71)*** | 3.96 (2.71) | 6.10 (2.69)*** | 3.88 (2.66) | 6.21 (2.66)*** | 3.69 (2.55) | 3.11 (2.32) | 4.87 (2.61)*** | 3.39 (2.42) | 5.18 (2.68)*** | 3.34 (2.40) | 5.14 (2.67)*** |
| Physical pain# | 2.73 (2.61) | 2.03 (2.39) | 3.23 (2.66)*** | 2.21 (2.35) | 3.57 (2.79)*** | 2.09 (2.25) | 3.76 (2.82)*** | 2.10 (2.31) | 1.64 (2.01) | 3.02 (2.62)*** | 1.79 (2.11) | 3.61 (2.72)*** | 1.81 (2.12) | 3.29 (2.74)*** |
| PHQ-2 total# | 2.38 (2.06) | 1.35 (1.70) | 3.12 (1.97)*** | 1.64 (1.79) | 3.56 (1.90)*** | 1.68 (1.81) | 3.48 (1.93)*** | 1.74 (1.77) | 1.26 (1.56) | 2.71 (1.78)*** | 1.49 (1.63) | 2.97 (1.92)*** | 1.47 (1.64) | 2.87 (1.86)*** |
| Global QOL# | 5.50 (1.88) | 6.26 (1.86) | 4.95 (1.69)*** | 5.92 (1.84) | 4.81 (1.74)*** | 5.90 (1.80) | 4.86 (1.82)*** | 5.75 (1.75) | 6.11 (1.71) | 5.02 (1.61)*** | 5.93 (1.71) | 4.86 (1.71)*** | 5.93 (1.71) | 4.97 (1.74)*** |
SI suicidal ideation, SP suicide plan, SA suicide attempt, M mean, SD standard deviation, PHQ-2 2-item Patient Health Questionnaire, QOL quality of life.
Note: #Mann–Whitney U test; *P < 0.05; **P < 0.01; ***P < 0.001.
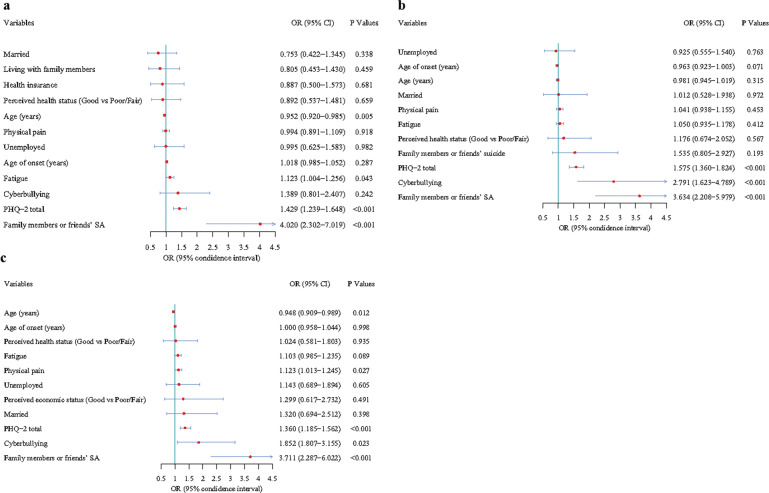
Patients with bipolar disorder
Among BD patients, the 1-year prevalence (95% CI) of SI, SP and SA were: 58.3% (54.1%-62.6%), 38.4% (34.3%-42.6%), and 38.6% (34.5%-42.8%), respectively (Table 1). Univariate analyses revealed that BD patients having any form of suicidality were more likely to be unmarried, unemployed, report cyberbullying, have family-or-friend SA, report poor/fair health status, have younger age and age of onset, higher fatigue, higher physical pain, higher PHQ-2 and lower QOL scores (Table 1). Furthermore, patients without health insurance and those with family-or-friend SA were more likely to have SI or SP. Patients living with family members were less likely to have SI. BD patients with SI (compared to without) were more likely to have SP (χ2 = 176.579, P < 0.001) and SA (χ2 = 188.247, P < 0.001) (Fig. 1a).
Fig. 1. Distribution of suicide plan and suicide attempt in patients with and without suicidal ideation.
Note: Numbers in bar graphs indicate patient counts. a shows counts of suicide plans (SP) and suicide attempts (SA) in BD patients by presence of SI. b shows SP and SA in SCZ by presence of SI. SI increases the risk for SP and SA in both disorders (p < 0.001).
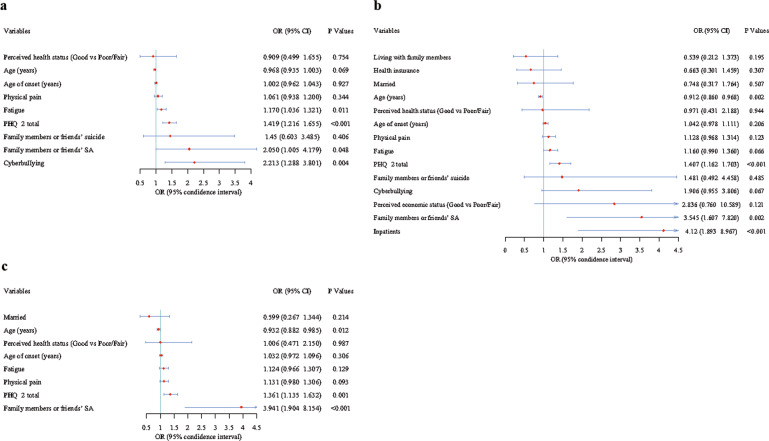
Three logistic regression models (one each for SI, SP, and SA) adjusted for confounders revealed that PHQ-2 total score and family-or-friend SA were positively associated with SI, SP and SA. Higher fatigue was associated with a higher risk of SI (OR = 1.123, 95%CI: 1.004–1.256, P = 0.043), while older age was inversely related to SI (OR = 0.952, 95%CI: 0.920–0.985, P = 0.005) and SA (OR = 0.948, 95%CI: 0.909–0.989, P = 0.012). Patients reporting cyberbullying had a higher risk of SP (OR = 2.791, 95%CI: 1.623–4.789, P < 0.001) and SA (OR = 1.852, 95%CI: 1.807–3.155, P = 0.023). Patients with higher physical pain score had a higher risk of SA (OR = 1.123, 95%CI: 1.013–1.245, P = 0.027). Please refer to Fig. 2a–c for multiple logistic regression models adjusted for various confounders.
Fig. 2. Independent correlates of suicidal ideation, suicide plan and suicide attempt in patients with bipolar disorder by multiple logistic regression analyses.
Note: a, suicidal ideation; b, suicide plan; c, suicide attempt.
ANCOVA revealed that BD patients with SI (compared to without) had lower QOL after controlling for confounders, (F (1,513) = 8.179, P = 0.004).
Patients with schizophrenia
In SCZ patients, the 1-year prevalence (95% CI) of SI, SP and SA were 33.2% (28.6–37.8%), 16.8% (13.2–20.5%), and 19.4% (15.5–23.3%), respectively (Table 1). Univariate analyses revealed that SCZ patients who were older, had a younger age of onset, had family-or-friend SA, reported poor/fair health status, had higher fatigue, higher physical pain, higher PHQ-2 total and lower QOL score were more likely to have SI, SP, and SA. Between SCZ patients with or without suicidality (i.e., any type of suicidality), there were significant differences in marital status, living status, health insurance status, patients' type, cyberbullying, family-or-friend suicide and self-reported economic status. SCZ patients with SI (compared to without) were more likely to have SP (χ2 = 119.394, P < 0.001) and SA (χ2 = 128.641, P < 0.001) (Fig. 1b).
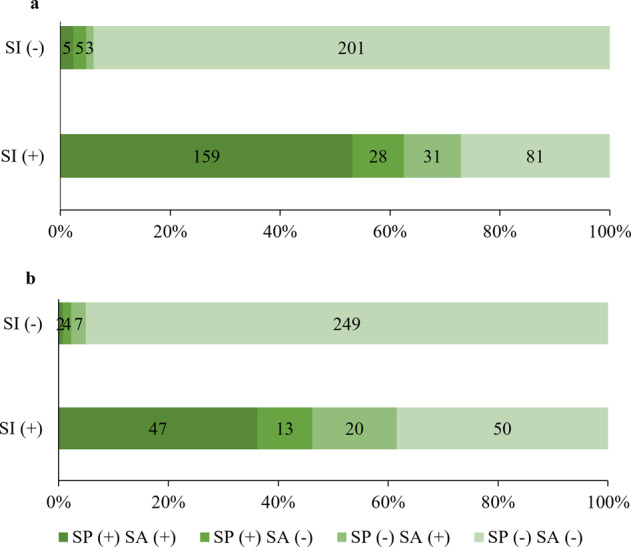
Binary logistic regression analyses revealed that SCZ patients who had severe depressive symptoms and family-or-friend SA had a higher risk of SI, SP and SA. Older age was inversely associated with SP (OR = 0.912, 95%CI: 0.860-0.968, P = 0.002) and SA (OR = 0.932, 95%CI: 0.882–0.985, P = 0.012). A higher fatigue score (OR = 1.170, 95%CI: 1.036–1.321, P = 0.011) and cyberbullying (OR = 2.213, 95%CI: 1.288–3.801, P = 0.004) were associated with higher risk of SI. Inpatients had higher SP risk (OR = 4.12, 95%CI: 1.893–8.967, P < 0.001) compared to outpatients (Fig. 3).
Fig. 3. Independent correlates of suicidal ideation, suicide plan and suicide attempt in patients with schizophrenia by multiple logistic regression analyses.
Note: a, suicidal ideation; b, suicide plan; c, suicide attempt.
Unlike BD, SCZ patients with SI, SP, and SA did not have significantly lower QOL when the ANCOVA controlled for confounding variables.
Discussion
In this study, we examined the 1-year prevalence of SI, SP, and SA in BD and SCZ patients during the COVID-19 pandemic. The main findings are that (1) the prevalence of any type of suicidality in BD patients was significantly higher than that in SCZ patients, and (2) suicidality rates in these disorders were higher compared to pre-pandemic rates. The first finding was similar to the results reached by previous meta-analyses conducted before the COVID-19 pandemic [13, 15]. In these two studies [13, 15], patients with SCZ) had a lower one-year risk of SA (3.0%) compared to those with BD (15.0%). Moreover, we found that BD/SCZ patients with SI had a higher risk of SP and SA than those without SI, which is consistent with previous findings in BD/SCZ patients [42, 43].
Compared to previous meta-analyses, the one-year suicidality rates (SA: 38.6%, 95% CI: 34.5–42.8% in BD; SA SCZ: 19.4%, 95% CI: 15.5–23.3% in SCZ) in this study were higher than non-pandemic rates in BD (one-year SA: 15%, 95% CI: 8–22%) [13] and SCZ (one-year SA: 3.0%, 95% CI: 2.3–3.7%) [15]. Increased suicidality in these two disorders could be byproducts of regulations to curb the transmission of COVID-19. First, social distancing regulations and quarantine [18] had a particularly negative impact on vulnerable populations, who have typically smaller social support networks than the general population [44]. The above measures may have eroded social support resulting in higher suicidality. Second, BD and SCZ patients rely on health professionals for care and prescriptions. COVID-19 regulations may have hindered visits to hospitals and clinics [45] and increased suicidality is an indicator of lost care. Third, the pandemic has both triggered and increased fear of infection, anxiety, and depression in the general population [46] as well as in people with mental disorders [45]. People with mental disorders may be more susceptible to these negative emotions, which may in turn have increased the risk of suicidality. Fourth, stigma and discrimination towards mental illness may have been amplified during the COVID-19 pandemic [19, 47], leading to higher suicidality in the stigmatized group.
The finding that younger age is associated with higher suicidality in both disorders was previously observed in meta-analytic studies of BD and SCZ patients [48, 49]. Online communication became the dominant mode during the pandemic and especially among younger people. Although people with SMI can also benefit from internet communication [50], it brings risks such as hostile, derogatory comments and online harassment [51]. Furthermore, younger people have lower levels of mental resilience, which is crucial for blunting stress and promoting adaptation [52].
We found that cyberbullying increases SA, which is consistent with a previous study that found a positive association between cyberbullying and SI/suicide behaviour [53]. It has been suggested that positive mental health confers resilience to cyberbullying, thereby protecting against suicidality [53]. As opportunities to receive mental health and medications dwindled, younger people and targets of cyberbullying may have become less resilient. Like previous studies [48, 54], we found that a history of SA or deaths in family or friends increases the suicidality of BD and SCZ patients. Having such exposure probably brings trauma, increased rejection, shame, and stigma [55] thereby increasing their own suicidality risk.
The finding that higher fatigue increases risk of suicidality could be part of the higher stress and tension brought about by the pandemic [56]. Living with the pandemic for a year tested everyone’s resolve and many have felt depleted emotionally. Depressive symptoms are common in BD and SCZ patients, which are a well-known risk factor for suicidality in patients with SMI [48, 49]. Compared to non-psychiatric patients, patients with SMI had four times higher risk of reporting high COVID-19-related stress, and were 2–3 times more likely to have COVID-19-related anxiety and depressive symptoms [57]. Physical pain can also be related to depressive symptoms and stress because these conditions enhance pain sensitivity [58–60]. This combination of factors may have contributed to higher suicidality during the pandemic. The discordant findings between SCZ and BD regarding QOL and inpatient status as predictors of suicidality are difficult to explain since some important factors were not measured such as type and doses of psychotropic medications.
The main strength of this study is that we assessed suicidality in participants after one year of living with the pandemic in various areas in China. We also acknowledge several limitations. As a cross-sectional study, a causal effect cannot be inferred between suicidality and various factors. Also, we did not have information regarding patients’ access to medications and telepsychiatry. Differences in these factors may account for differences in suicidality. Finally, the limited range of psychiatric symptoms that we asked about could not be directly attributed to COVID-19 alone. This is in part due to the cross-sectional design of the survey, which was a necessity due to the unanticipated nature of the pandemic.
In conclusion, the pandemic has an outsized impact on SMI patients, resulting in a higher level of suicidality, especially in patients with BD. Several risk factors (e.g., younger age, inpatients, cyberbullying, and depressive symptoms) have been identified, and findings suggest that the importance of suicidality screening in patients with high risk and providing targeted effective interventions.
Acknowledgements
We are grateful to all participants and clinicians involved in this study.
Author contributions
Study design: F-RA, Y-TX. Data collection, analysis and interpretation: Y-CL, WB, HC, YW, LZ, Y-HD, J-JY, XD, Z-TZ, C-ML, K-XF, W-FM, LZ, H-ZL, F-RA. Drafting of the manuscript: WB, ZS, TC, Y-TX. Critical revision of the manuscript: LB. Approval of the final version for publication: all co-authors.
Funding
The study was supported by the Beijing Municipal Science & Technology Commission (Grant No.: Z181100001718124), Beijing Talents Foundation (Grant No.: 2017000021469G222), Xiamen Municipal Health Commission Guidance Project (Grant No.: 3502Z20209249), the University of Macau (MYRG2019-00066-FHS), and the Scientific and Technological Program of Suzhou (SS202069).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Yu-Chen Li, Wei Bai, Hong Cai, Yuxuan Wu, Ling Zhang, Yan-Hong Ding, Juan-Juan Yang.
Contributor Information
Feng-Rong An, Email: afrylm@sina.com.
Yu-Tao Xiang, Email: xyutly@gmail.com.
References
- 1.World Health Organization. Suicide in the world: global health estimates. (World Health Organization, 2019).
- 2.Sveticic J, De Leo D. The hypothesis of a continuum in suicidality: a discussion on its validity and practical implications. Ment Illn. 2012;4:e15–e15. doi: 10.4081/mi.2012.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spittal MJ, Pirkis J, Miller M, Carter G, Studdert DM. The repeated episodes of self-harm (RESH) score: A tool for predicting risk of future episodes of self-harm by hospital patients. J Affect Disord. 2014;161:36–42. doi: 10.1016/j.jad.2014.02.032. [DOI] [PubMed] [Google Scholar]
- 4.Cao XL, Zhong BL, Xiang YT, Ungvari GS, Lai KY, Chiu HF, et al. Prevalence of suicidal ideation and suicide attempts in the general population of China: a meta-analysis. Int J Psychiatry Med. 2015;49:296–308. doi: 10.1177/0091217415589306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brådvik L. Suicide risk and mental disorders. Int J Environ Res Public Health. 2018;15:2028. doi: 10.3390/ijerph15092028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adewuya AO, Oladipo EO. Prevalence and associated factors for suicidal behaviours (ideation, planning, and attempt) among high school adolescents in Lagos, Nigeria. Eur Child Adolesc Psychiatry. 2020;29:1503–12. doi: 10.1007/s00787-019-01462-x. [DOI] [PubMed] [Google Scholar]
- 7.Widom CS, Li X. The role of psychiatric symptoms and environmental vulnerability factors in explaining the relationship between child maltreatment and suicidality: a prospective investigation. J Affect Disord. 2020;276:720–31. doi: 10.1016/j.jad.2020.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ivbijaro G, Kolkiewicz L, Goldberg D, N’Jie INS, Edwards T, Riba MB, et al. Suicide prevention and COVID-19. Asia-Pac Psychiatry. 2021;13:e12482. doi: 10.1111/appy.12482. [DOI] [PubMed] [Google Scholar]
- 9.Wasserman D, Carli V, Iosue M, Javed A, Herrman H. Suicide prevention in psychiatric patients. Asia-Pac Psychiatry. 2021;13:e12450. doi: 10.1111/appy.12450. [DOI] [PubMed] [Google Scholar]
- 10.Das-Munshi J, Chang C-K, Dutta R, Morgan C, Nazroo J, Stewart R, et al. Ethnicity and excess mortality in severe mental illness: a cohort study. Lancet Psychiatry. 2017;4:389–99. doi: 10.1016/S2215-0366(17)30097-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miller JN, Black DW. Bipolar disorder and suicide: a review. Curr Psychiatry Rep. 2020;22:6. doi: 10.1007/s11920-020-1130-0. [DOI] [PubMed] [Google Scholar]
- 12.Simon, RI & Hales, RE The American Psychiatric Publishing textbook of suicide assessment and management. (American Psychiatric Pub, 2012).
- 13.Dong M, Lu L, Zhang L, Zhang Q, Ungvari GS, Ng CH, et al. Prevalence of suicide attempts in bipolar disorder: a systematic review and meta-analysis of observational studies. Epidemiol Psychiatr Sci. 2020;29:e63. doi: 10.1017/S2045796019000593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bai W, Liu ZH, Jiang YY, Zhang QE, Rao WW, Cheung T, et al. Worldwide prevalence of suicidal ideation and suicide plan among people with schizophrenia: a meta-analysis and systematic review of epidemiological surveys. Transl Psychiatry. 2021;11:552. doi: 10.1038/s41398-021-01671-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lu L, Dong M, Zhang L, Zhu X-M, Ungvari GS, Ng CH, et al. Prevalence of suicide attempts in individuals with schizophrenia: a meta-analysis of observational studies. Epidemiol Psychiatr Sci. 2020;29:e39. doi: 10.1017/S2045796019000313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Phiri P, Ramakrishnan R, Rathod S, Elliot K, Thayanandan T, Sandle N, et al. An evaluation of the mental health impact of SARS-CoV-2 on patients, general public and healthcare professionals: a systematic review and meta-analysis. EClinicalMedicine. 2021;34:100806. doi: 10.1016/j.eclinm.2021.100806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Banerjee D, Kosagisharaf JR, Sathyanarayana Rao TS. ‘The dual pandemic’ of suicide and COVID-19: A biopsychosocial narrative of risks and prevention. Psychiatry Res. 2021;295:113577. doi: 10.1016/j.psychres.2020.113577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith K, Lambe S, Freeman D, Cipriani A. COVID-19 vaccines, hesitancy and mental health. Evid Based Ment Health. 2021;24:47. doi: 10.1136/ebmental-2021-300266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fornaro M, De Prisco M, Billeci M, Ermini E, Young AH, Lafer B, et al. Implications of the COVID-19 pandemic for people with bipolar disorders: a scoping review. J Affect Disord. 2021;295:740–751. doi: 10.1016/j.jad.2021.08.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reynolds CM, Purdy J, Rodriguez L, McAvoy H. Factors associated with changes in consumption among smokers and alcohol drinkers during the COVID-19 `lockdown'period. Eur J Public Health. 2021;31:1084–1089. doi: 10.1093/eurpub/ckab050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stefana A, Youngstrom EA, Chen J, Hinshaw S, Maxwell V, Michalak E, et al. The COVID-19 pandemic is a crisis and opportunity for bipolar disorder. Bipolar Disord. 2020;22:641–3. doi: 10.1111/bdi.12949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kinoshita, S, Cortright, K, Crawford, A, Mizuno, Y, Yoshida, K, Hilty, D et al. Changes in telepsychiatry regulations during the COVID-19 pandemic: 17 countries and regions’ approaches to an evolving healthcare landscape. Psychological Med. 1-8, 10.1017/S0033291720004584 (2020). [DOI] [PMC free article] [PubMed]
- 23.Busch IM, Moretti F, Mazzi M, Wu AW, Rimondini M. What we have learned from two decades of epidemics and pandemics: a systematic review and meta-analysis of the psychological burden of frontline healthcare workers. Psychotherapy Psychosomatics. 2021;90:178–190. doi: 10.1159/000513733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fegert JM, Vitiello B, Plener PL, Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc psychiatry Ment Health. 2020;14:1–11. doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Toubasi AA, AbuAnzeh RB, Tawileh HBA, Aldebei RH, Alryalat SAS. A meta-analysis: the mortality and severity of COVID-19 among patients with mental disorders. Psychiatry Res. 2021;299:113856. doi: 10.1016/j.psychres.2021.113856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lohiniva A-L, Dub T, Hagberg L, Nohynek H. Learning about COVID-19-related stigma, quarantine and isolation experiences in Finland. PloS One. 2021;16:e0247962. doi: 10.1371/journal.pone.0247962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bai W, Cai H, Liu S, Liu H, Qi H, Chen X, et al. Attitudes toward COVID-19 vaccines in Chinese college students. Int J Biol Sci. 2021;17:1469–75. doi: 10.7150/ijbs.58835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu S, Xi HT, Zhu QQ, Ji M, Zhang H, Yang BX, et al. The prevalence of fatigue among Chinese nursing students in post-COVID-19 era. PeerJ. 2021;9:e11154. doi: 10.7717/peerj.11154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.World Health Organization. The ICD-10 classification of mental and behavioural disorders: Diagnostic criteria for research. (World Health Organization, 1993).
- 30.Ma YF, Li W, Deng HB, Wang L, Wang Y, Wang PH, et al. Prevalence of depression and its association with quality of life in clinically stable patients with COVID-19. J Affect Disord. 2020;275:145–8. doi: 10.1016/j.jad.2020.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lobana A, Mattoo SK, Basu D, Gupta N. Quality of life in schizophrenia in India: comparison of three approaches. Acta Psychiatr Scand. 2001;104:51–55. doi: 10.1034/j.1600-0447.2001.104001051.x. [DOI] [PubMed] [Google Scholar]
- 32.Berger AM, Abernethy AP, Atkinson A, Barsevick AM, Breitbart WS, Cella D, et al. NCCN Clinical Practice Guidelines Cancer-related fatigue. J Natl Compr Canc Netw. 2010;8:904–31. doi: 10.6004/jnccn.2010.0067. [DOI] [PubMed] [Google Scholar]
- 33.Haefeli M, Elfering A. Pain assessment. Eur Spine J. 2006;15:S17–24. doi: 10.1007/s00586-005-1044-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284–92. doi: 10.1097/01.Mlr.0000093487.78664.3c. [DOI] [PubMed] [Google Scholar]
- 35.Yu X, Stewart SM, Wong PTK, Lam TH. Screening for depression with the Patient Health Questionnaire-2 (PHQ-2) among the general population in Hong Kong. J Affect Disord. 2011;134:444–7. doi: 10.1016/j.jad.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 36.Xia P, Li N, Hau KT, Liu C, Lu Y. Quality of life of Chinese urban community residents: a psychometric study of the mainland Chinese version of the WHOQOL-BREF. BMC Med Res Methodol. 2012;12:37. doi: 10.1186/1471-2288-12-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.The WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL Group. Psychol Med. 1998;28:551–8. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- 38.Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56:617–26. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- 39.Zhong Y, Xia L, Zhao TT, Zhang YL, Zhang YL, Li WZ, et al. The Prevalence of Suicide Attempts and Independent Demographic and Clinical Correlates among Chronic Schizophrenia Patients in Agricultural Areas of China. Psychiatr Q. 2019;90:683–91. doi: 10.1007/s11126-019-09644-1. [DOI] [PubMed] [Google Scholar]
- 40.Gao T, Xiang YT, Zhang H, Gao J, Kong Y, Hu Y, et al. Prevalence and correlates of suicidal behaviors among college students in Northeastern China: a cross-sectional study. Psychiatr Q. 2018;89:359–70. doi: 10.1007/s11126-017-9540-9. [DOI] [PubMed] [Google Scholar]
- 41.R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, Vienna, Austria, 2021).
- 42.Valtonen HM, Suominen K, Mantere O, Leppämäki S, Arvilommi P, Isometsä ET. Prospective study of risk factors for attempted suicide among patients with bipolar disorder. Bipolar Disord. 2006;8:576–85. doi: 10.1111/j.1399-5618.2006.00341.x. [DOI] [PubMed] [Google Scholar]
- 43.Montross LP, Kasckow J, Golshan S, Solorzano E, Lehman D, Zisook S. Suicidal ideation and suicide attempts among middle-aged and older patients with schizophrenia spectrum disorders and concurrent subsyndromal depression. J Nerv Ment Dis. 2008;196:884–90. doi: 10.1097/NMD.0b013e31818ec823. [DOI] [PubMed] [Google Scholar]
- 44.Degnan A, Berry K, Sweet D, Abel K, Crossley N, Edge D. Social networks and symptomatic and functional outcomes in schizophrenia: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. 2018;53:873–88. doi: 10.1007/s00127-018-1552-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yao H, Chen J-H, Xu Y-F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020;7:e21–e21. doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bendau A, Petzold MB, Pyrkosch L, Mascarell Maricic L, Betzler F, Rogoll J, et al. Associations between COVID-19 related media consumption and symptoms of anxiety, depression and COVID-19 related fear in the general population in Germany. Eur Arch Psychiatry Clin Neurosci. 2021;271:283–91. doi: 10.1007/s00406-020-01171-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chaimowitz GA, Upfold C, Géa LP, Qureshi A, Moulden HM, Mamak M, et al. Stigmatization of psychiatric and justice-involved populations during the COVID-19 pandemic. Prog Neuro-Psychopharmacol Biol Psychiatry. 2021;106:110150. doi: 10.1016/j.pnpbp.2020.110150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cassidy RM, Yang F, Kapczinski F, Passos IC. Risk factors for suicidality in patients with schizophrenia: a systematic review, meta-analysis, and meta-regression of 96 studies. Schizophrenia Bull. 2018;44:787–97. doi: 10.1093/schbul/sbx131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.da Silva Costa L, Alencar ÁP, Neto PJN, dos Santos MDSV, da Silva CGL, Pinheiro SDFL, et al. Risk factors for suicide in bipolar disorder: a systematic review. J Affect Disord. 2015;170:237–54. doi: 10.1016/j.jad.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 50.Chung JE. Social interaction in online support groups: Preference for online social interaction over offline social interaction. Computers Hum Behav. 2013;29:1408–14. doi: 10.1016/j.chb.2013.01.019. [DOI] [Google Scholar]
- 51.Naslund JA, Aschbrenner KA, Marsch LA, Bartels SJ. The future of mental health care: peer-to-peer support and social media. Epidemiol Psychiatr Sci. 2016;25:113–22. doi: 10.1017/S2045796015001067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhong X, Wu D, Nie XQ, Xia J, Li ML, Lei F, et al. Parenting style, resilience, and mental health of community-dwelling elderly adults in China. BMC Geriatrics. 2016;16:135. doi: 10.1186/s12877-016-0308-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Brailovskaia J, Teismann T, Margraf J. Cyberbullying, positive mental health and suicide ideation/behavior. Psychiatry Res. 2018;267:240–2. doi: 10.1016/j.psychres.2018.05.074. [DOI] [PubMed] [Google Scholar]
- 54.Carballo JJ, Harkavy-Friedman J, Burke AK, Sher L, Baca-Garcia E, Sullivan GM, et al. Family history of suicidal behavior and early traumatic experiences: Additive effect on suicidality and course of bipolar illness? J Affect Disord. 2008;109:57–63. doi: 10.1016/j.jad.2007.12.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pitman A, Osborn D, King M, Erlangsen A. Effects of suicide bereavement on mental health and suicide risk. Lancet Psychiatry. 2014;1:86–94. doi: 10.1016/S2215-0366(14)70224-X. [DOI] [PubMed] [Google Scholar]
- 56.Chatterjee SS, Barikar C M, Mukherjee A. Impact of COVID-19 pandemic on pre-existing mental health problems. Asian J Psychiatr. 2020;51:102071–102071. doi: 10.1016/j.ajp.2020.102071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Iasevoli F, Fornaro M, D’Urso G, Galletta D, Casella C, Paternoster M, et al. Psychological distress in patients with serious mental illness during the COVID-19 outbreak and one-month mass quarantine in Italy. Psychological Med. 2021;51:1054–6. doi: 10.1017/S0033291720001841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Crettaz B, Marziniak M, Willeke P, Young P, Hellhammer D, Stumpf A, et al. Stress-induced allodynia–evidence of increased pain sensitivity in healthy humans and patients with chronic pain after experimentally induced psychosocial stress. PloS One. 2013;8:e69460. doi: 10.1371/journal.pone.0069460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fischer S, Doerr JM, Strahler J, Mewes R, Thieme K, Nater UM. Stress exacerbates pain in the everyday lives of women with fibromyalgia syndrome—The role of cortisol and alpha-amylase. Psychoneuroendocrinology. 2016;63:68–77. doi: 10.1016/j.psyneuen.2015.09.018. [DOI] [PubMed] [Google Scholar]
- 60.Li D-J, Hsu S-T, Chou FH-C, Chou L-S, Hsieh K-Y, Kao W-T, et al. Predictors for depression, sleep disturbance, and subjective pain among inpatients with depressive disorders during the COVID-19 pandemic: a cross-sectional study. Int J Environ Res Public Health. 2021;18:6523. doi: 10.3390/ijerph18126523. [DOI] [PMC free article] [PubMed] [Google Scholar]