Figure 2: Neuropathology after traumatic brain injury.
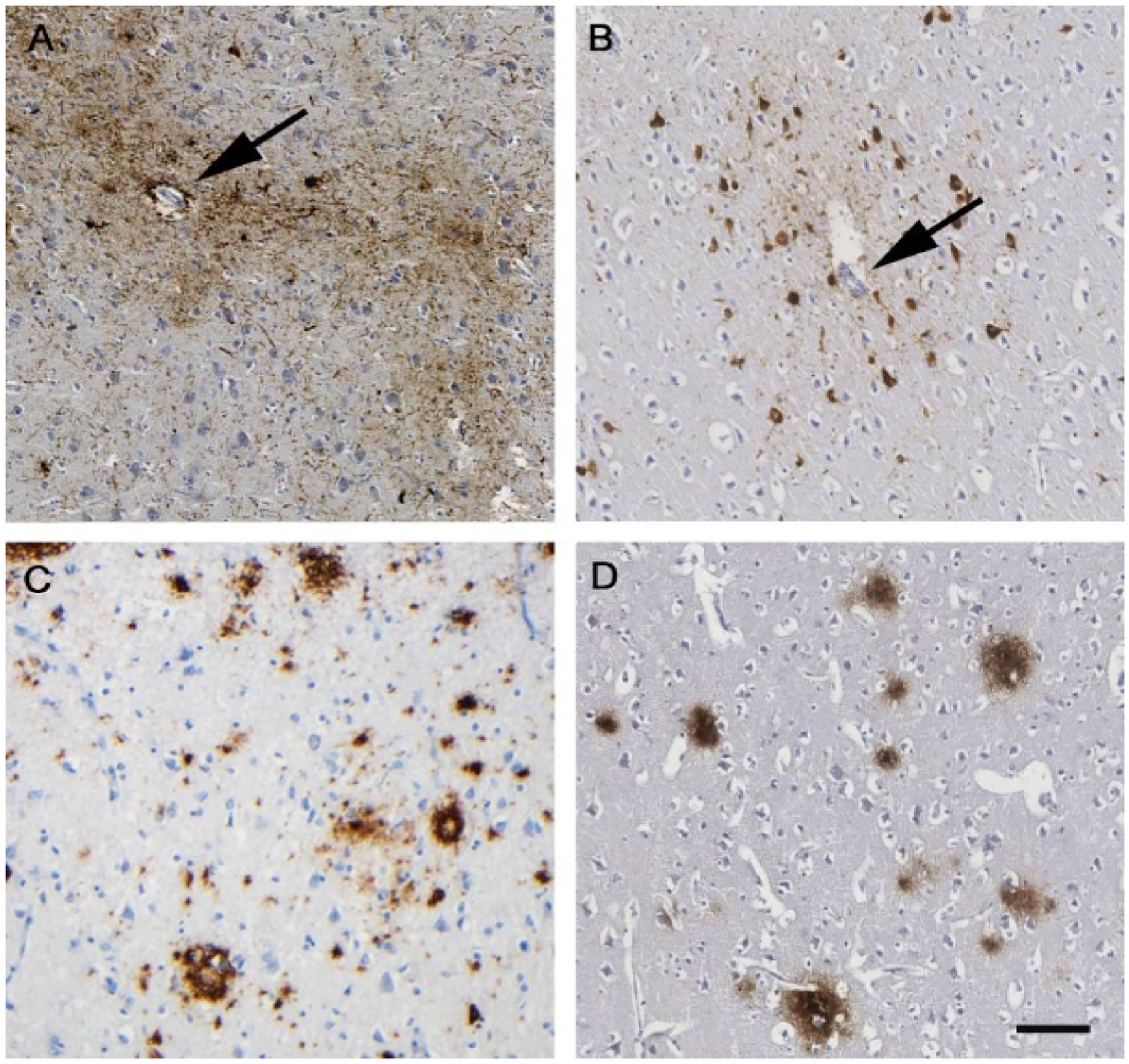
Appearance of hyperphosphorylated tau aggregates within neurons and astrocytes (brown staining in panels A and B) clustered around small cortical vessels (arrows), characteristically in a patchy distribution towards the depths of cortical sulci, is emerging as the distinctive pathology of chronic traumatic encephalopathy. This pathology appears to be virtually exclusive to circumstances in which there has been exposure to brain injury in life, whether as repetitive mild TBI as shown in a 61-year-old male former boxer (A) or single moderate or severe TBI as shown in a 48-year-old man with 3 years of survival after single severe TBI (B). In addition to this distinctive tau pathology, neurodegeneration after TBI is increasingly recognised as a complex pathology, including abnormal amyloid plaque deposition (brown staining in panels C and D). As with tau, aspects of these pathologies can be recognised in case material from patients exposed to either repetitive mild TBI as shown in a 59-year-old male former soccer player (C) or single moderate or severe TBI (D; same patient as in panel B). Phosphorylated tau using antibody CP13 (A) or PHF-1 (B). Amyloid β was stained with antibody 6F3D (C and D). TBI= traumatic brain injury. Scale bar 100 microns for all images.
