Abstract
This study characterized the prevalence, sociodemographic characteristics, and behavioral health of U.S. adult subpopulations with distinct drug use trajectories during the first year of the COVID-19 pandemic. Adult respondents (n = 8306) in a nationally-representative longitudinal study completed 13 monthly web surveys (March 2020–March 2021). Frequency of past-week drug use, cannabis use, and alcohol use (range:0–7), as well as anxiety and depressive symptoms, were assessed at each survey. Growth mixture models were used to parse out distinct subpopulations with homogenous drug use trajectories based on mean drug use days over time. Four drug use trajectories were identified: Stable Abstinence (85.7% [95%CI = 85.0–86.5] of the sample) with <1 mean past-week drug use days; Escalating Infrequent Use (7.1% [95%CI = 6.6–7.7]) with 0.2 March mean past-week drug use days and increases from April to October; Use Cessation (4.3% [95%CI = 3.8–4.7]) with 1.1 March mean past-week drug use days that initially increased, then sharply decreased to near zero; and Stable Frequent Use (2.9% [95%CI = 2.5–3.3]) with between 2.4 and 3.5 past-week drug use days across the study period. Compared to the stable abstinence group, the other subgroups were more likely to be Hispanic or Black, younger in age, unemployed, below the federal poverty line, and less likely to have a college degree or be married. They also reported higher levels of alcohol and cannabis use, as well as higher anxiety and depressive symptoms. These results provide opportunities to optimize the targeted delivery of preventive interventions for substance use during the COVID-19 pandemic and future public health emergencies.
Keywords: Epidemiology, COVID-19 pandemic, Drug use, Substance use
1. Introduction
Patterns of substance use in the U.S. general population appear to be changing over the course of the COVID-19 pandemic. In a nationally-representative cross-sectional survey in June 2020, 13.3% of adults retrospectively reported having started or increased substance use during the pandemic, which increased to 15.1% in a September 2020 follow-up survey (Czeisler et al., 2020, 2021). Slight changes in levels of alcohol and cannabis use in the overall population have been observed during the first several months of pandemic (Brenneke et al., 2022; Nordeck et al., 2022).
While prior studies have examined changes in substance use (without distinguishing between substances) and changes in alcohol and cannabis use, to our knowledge, no studies have investigated changes in use of other drugs. This is despite the fact that rates of drug-related overdoses have increased throughout the first year of the pandemic (Holland et al., 2021), primarily driven by exposure to drugs that cannot be legally used for recreational purposes or non-medical use of prescription drugs (e.g., opioids, stimulates, anxiolytics). Given the sociodemographic disparities in the impact of the pandemic on day-to-day life, with a greater burden of pandemic-related disruptions falling on women, people of color, and lower-income adults (Karpman et al., 2020; Kochhar, 2020), changes in drug use – which may be done as a means of coping with stress, isolation, grief, or job loss (MacMillan et al., 2021) – may also be heterogeneous according to these characteristics. Finally, slight increases in psychological distress, cannabis use, and alcohol use documented in other studies (Brenneke et al., 2022; Nordeck et al., 2022; Riehm et al., 2021) suggest that similar changes may have occurred in drug use, given the interrelatedness of mental health and substance use. Altogether, tracking use of drugs other than cannabis or alcohol constitutes an important surveillance activity that could have implications for targeted prevention efforts during the pandemic and afterwards.
Existing research has not used longitudinal, repeated-measures methods to examine person-centered changes in substance use during the pandemic. Two sizeable groups, for example, younger and older adults, might average out to show only subtle changes if one group experiences a substantial decrease and the other experiences a substantial increase in use. Relatedly, some individuals may have both increased and decreased drug use at different points in time in response to fluctuations in the stringency of pandemic-related restrictions and other risk factors. It is also likely that population-wide trends of slight changes in non-specific “substance use” could be obscuring clinically important, divergent trajectories between the diverse types of drugs being used by Americans. Without longitudinal analyses that disaggregate unique changes in drug use over time, it is impossible to identify such substantively meaningful heterogenous subgroups that may call for different profiles of intervention and policy strategies.
Observing population-level trends in drug use during the pandemic has proven challenging because many ongoing surveys halted recruitment, resulting in a dearth of data (Ignaszewski, 2021). In this context, the Understanding America Study (UAS), an internet-based, nationally-representative survey, represents an important source of data. Since the onset of the COVID-19 pandemic in the U.S., the UAS has administered repeated surveys to a longitudinal sample of U.S. adults. The current study leveraged UAS longitudinal data to (1) identify subpopulations characterized by distinct trajectories of recreational use of illicit drugs or non-medical use of prescription drugs other than alcohol or cannabis (hereafter referred to as “drug use”) and (2) examine how sociodemographic and behavioral characteristics mapped onto membership in each subpopulation.
2. Methods
2.1. Participants and procedures
The UAS is a probability-based online panel of 8547 non-institutionalized adults regularly surveyed on social, economic, and health issues that represents the entire U.S (Alattar et al., 2018). UAS uses address-based random probability sampling and is regularly refreshed with two-stage adaptive sampling to increase national representativeness detailed elsewhere (Alattar et al., 2018). Panel recruitment rates range from 15% to 20% and annual retention rates are approximately 95%. Each survey contains updated sampling weights using a two-step procedure with post-stratification ranking algorithms to increase demographic national representativeness (Alattar et al., 2018). Initial panel recruitment is completed by postal mail. Phone contact follows for identity verification, written informed consent, and demographic information surveys (later updated quarterly).
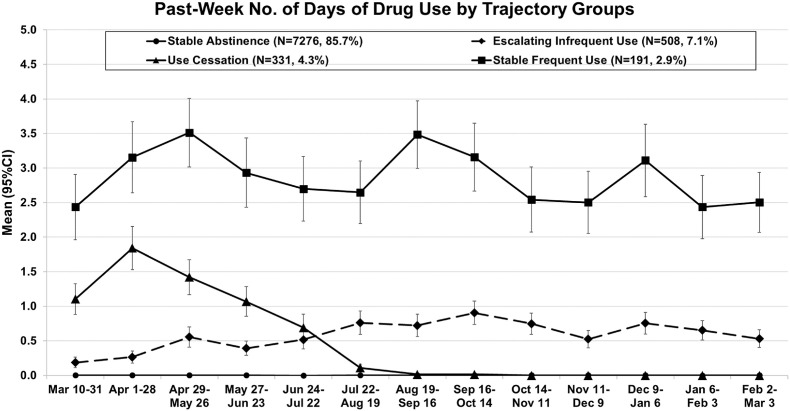
All UAS panel members were invited to the Coronavirus in America longitudinal survey consisting of a March 10, 2020 baseline (wave 1; 1 day before COVID-19 was declared a global pandemic by WHO) (Cucinotta and Vanelli, 2020) and repeated follow-ups at approximately monthly intervals starting April 1, 2020 (Kapteyn et al., 2020). A nested stratified design randomized participants to respond on a pre-assigned day across a 14-day period with 13-day response windows for each respective follow-up. Surveys were self-administered web questionnaires. UAS shipped an Internet-enabled tablet to households without Internet service or devices for at-home use. This study used 13 surveys wave each collected approximately 4 weeks apart (03/10/2020-03/03/2021; see dates in Fig. 1 ). This study period coincided with the declaration of a national emergency on March 13, 2020; surpassing a death toll of 100,000 people on May 28, 2020; the first emergency use authorization for a COVID-19 vaccine on December 11, 2020; and the subsequent revision of mask-wearing recommendations by the CDC in March 2021.
Fig. 1.
Past-week of number of drug use days by trajectory groups.
We included participants who (1) completed at least one survey and (2) provided data for past 7-day drug use during at least one survey. Of the 8547 UAS panel respondents invited for the Coronavirus in America survey, 8425 completed ≥1 surveys, of whom 8306 (97.2% of total sample) provided past 7-day drug use frequency data at ≥1 timepoints, constituting the analytic sample (79,879 observations). There was variability across waves in response rates (Mean = 75.1%[SD = 3.4%]; range = 65.7–82.9%) and in total surveys completed per respondent (mean = 9.62[SD = 4.17], Range = 1–13). Supplemental Table 1 details wave-specific response rates. University of Southern California's Institutional Review Board approved this study.
2.2. Measures
Demographics. Participants self-reported sex (female or male), race/ethnicity (Hispanic, Non-Hispanic Black, Non-Hispanic White, Non-Hispanic Asian, Non-Hispanic Other [American Indian, Alaska Native, Pacific Islander combined due to small frequencies]), age (18–39, 40–50, 51–64, 65+ years), marital status (yes/no), household structure (living alone, living with partner only, living with children only [i.e., single parent/guardian], living with partner and children, and other [multigenerational households, roommates, etc.]), annual household income (above vs. below federal poverty threshold), highest education (college degree: yes/no), and current working status (yes/no).
Substance use. Three items assessing number of days using of three psychoactive drug classes (i.e., cannabis, alcohol, and other drugs, described as ‘recreational drugs other than alcohol or cannabis products’) in the past week were assessed (range: 0–7). The item assessing use of other drugs was used as the primary outcome in the trajectory modeling, whereas cannabis and alcohol use were included as covariates.
Anxiety and depressive symptoms. The Patient Health Questionnaire (PHQ-4) was used to assess anxiety and depressive symptoms. The PHQ-4 is a widely used and well-validated measure comprised of two items from the PHQ-9 depression measure and two items from the Generalized Anxiety Disorder-7 (GAD-7) (Kroenke et al., 2019; Kroenke et al., 2009). The scale assesses the frequency of core symptoms of depressive disorders (e.g., ‘Feeling down, depressed, or hopeless’) and anxiety disorders (e.g., ‘Feeling nervous, anxious or on edge’) over the past two weeks (response options: 0 [not at all], 1 [several days], 2 [more than half the days], 3 [nearly every day]). Based on the prior studies (Manea et al., 2016; Plummer et al., 2016), the depressive symptoms (2-item; Cronbach's α = 0.87) and anxiety disorders (2-item; α = 0.87) scales were separately calculated using sum scores (range = 0–6), and each scale was dichotomized to identify participants scoring above a total score of ≥3 indicating moderate-to-severe anxiety or depressive symptoms.
2.3. Data analysis
A series of growth mixture models (GMMs) (B. Muthén and Muthén, 2000) was conducted to identify homogenous subgroups with distinct trajectories of drug use using mean, variance, and covariance patterns of person-level repeated measurements of estimated latent intercepts, linear slopes, and quadratic slopes. The number of past-week drug use days was treated as a count variable. Selection of the best-fitting class solution was guided by Akaike Information Criterion (AIC), entropy values, and Lo–Mendell–Rubin (LMR) likelihood ratio tests (Nylund et al., 2007). To ensure a global solution, the GMM analysis was replicated using multiple start values and different random starts. As the default model option, GMM random effects (i.e., variation around the mean trajectory within classes) and residual variances (i.e., the variance of the difference between the observed and estimated value for each individual at each time point) were constrained to be equal for each class. Descriptions of each trajectory in final GMMs were based on: (a) tests of whether estimated linear/quadratic slopes significantly differed from zero, and (b) estimated means of past-week drug use day at each timepoint using trajectories variables. The auxiliary BCH/DCAT method in Mplus was performed to examine differences in probability of drug use trajectory group memberships by each demographic, substance use, and psychological distress variable (i.e., continuous variables with the BCH option; categorical variables with the DCAT option) (Asparouhov and Muthén, 2014). Significance of differences was reported based on the overall and pair-wise Chi-square/degree of freedom (χ2/df) values from the auxiliary procedure. Based on each respondent's initial survey assessment (i.e., baseline wave assessments), associations between each demographic, substance use, and psychological distress variable and drug use trajectory memberships were examined. In addition, variables which could have changed during the pandemic (i.e., employment status, marital status, cannabis and alcohol use, anxiety and depressive symptoms) were also examined using the final wave assessments including each respondent's last survey assessment across Dec 9, 2020–Mar 3, 2021 (i.e., last 3 waves). Analyses were conducted using Mplus Version 8 accounting for the nesting and sampling structure, as well as national-representative sampling weights (Muthén, 2015). Missingness was handled using full information maximum likelihood estimation. Benjamini-Hochberg two-tailed p-values were corrected for multiple tests to maintain study-wise false discovery rate of .05 (Benjamini and Hochberg, 1995).
3. Results
3.1. Descriptive results
Study sample.Table 1 displays summary statistics of differences in demographic, substance use, and psychological distress variables across drug use trajectory groups. At baseline, the analytic sample was 52.4% female, 18.3% Hispanic, 12.0% Black, 60.7% White, 5.2% Asian, and 3.8% other race/ethnicity. The weighted past-week number of drug use days in the overall sample collapsing data timepoints across the entire follow-up period were as follows: 0 (96.4%), 1 (0.8%), 2 (0.7%), 3 (0.5%), 4 (0.3%), 5 (0.3%), 6 (0.1%), and 7 (0.9%) days.
Table 1.
Sociodemographic, substance use, and mental distress variables of overall sample and by trajectory group for No. drug use days outcomes.
| Variables | By drug use trajectory group |
|||||
|---|---|---|---|---|---|---|
| Overall (n = 8306)a,b | Stable Abstinence (N = 7276, 85.7%)c | Escalating Infrequent Use (N = 508, 7.1%)c | Use Cessation (N = 331, 4.3%)c | Stable Frequent Use (N = 191, 2.9%)c | P-value for group differenced | |
| Baseline Wave Assessmentse | ||||||
| Female sex (vs. Male), N(%) | 4907 (52.4) | 52.4 (51.2–53.6)1 | 47.7 (44.1–51.3)1 | 53.7 (49.7–57.8)1 | 54.9 (49.3–60.6)1 | .09 |
| Race/ethnicity, N(%) | <.001 | |||||
| Hispanic | 1401 (18.3) | 17.3 (16.4–18.2)2 | 23.3 (20.2–26.3)1 | 20.4 (17.1–23.6)1,2 | 27.1 (21.9–32.2)1 | |
| White | 5342 (60.7) | 63.4 (62.3–64.5)1 | 48.4 (44.8–51.9)2,3 | 53.2 (49.1–57.2)2 | 42.9 (37.2–48.5)3 | |
| Black | 660 (12.0) | 10.4 (9.7–11.1)2 | 17.8 (15.1–20.6)1 | 19.8 (16.5–23.0)1 | 19.1 (14.5–23.6)1 | |
| Asian | 427 (5.2) | 5.4 (4.8–5.9)1 | 5.1 (3.5–6.7)1,2 | 4.0 (2.4–5.6)1,2 | 2.8 (0.9–4.6)2 | |
| Otherf | 465 (3.8) | 3.6 (3.1–4.0)2,3 | 5.5 (3.8–7.1)1,2 | 2.6 (1.3–3.9)3 | 8.3 (5.1–11.4)1 | |
| Age, y, N(%) | <.001 | |||||
| 18-39 | 2691 (43.3) | 41.1 (39.9–42.2)3 | 51.2 (47.7–54.8)2 | 49.8 (45.8–53.9)2 | 65.4 (60.0–70.9)1 | |
| 40-50 | 1659 (17.0) | 17.0 (16.1–17.9)1 | 16.7 (14.1–19.4)1 | 17.6 (14.5–20.7)1 | 18.1 (13.7–22.5)1 | |
| 51-64 | 2227 (22.7) | 23.3 (22.3–24.3)1 | 20.6 (17.7–23.5)1,2 | 20.8 (17.5–24.1)1,2 | 14.4 (10.4–18.4)2 | |
| 65+ | 1720 (17.1) | 18.6 (17.8–19.6)1 | 11.4 (9.2–13.7)2,3 | 11.8 (9.2–14.4)2 | 2.0 (0.04–3.7)3 | |
| Received college degree, N(%) | 4600 (45.0) | 48.1 (46.9–49.3)1 | 31.5 (28.2–34.8)2 | 35.6 (31.7–39.5)2 | 20.9 (16.2–25.6)3 | <.001 |
| Below federal poverty level, N(%) | 1325 (19.8) | 16.1 (15.2–17.0)3 | 35.7 (32.2–39.2)2 | 32.6 (28.7–36.5)2 | 46.2 (40.4–52.0)1 | <.001 |
| Working, N(%) | 5084 (62.1) | 62.9 (61.7–64.0)1 | 60.7 (57.2–64.2)1,2 | 56.3 (52.3–60.4)2 | 52.7 (46.5–58.9)3 | .01 |
| Currently married, N(%) | 4511 (53.4) | 56.7 (55.6–57.9)1 | 37.6 (34.1–41.1)3 | 47.1 (43.0–51.1)2 | 25.9 (20.9–31.0)4 | <.001 |
| Household structure, N (%) | <.001 | |||||
| Living alone | 1174 (13.2) | 12.9 (12.1–13.7)1 | 13.7 (10.9–16.4)1 | 17.5 (13.5–21.3)1 | 13.3 (8.9–17.7)1 | |
| Living with partner only | 2036 (22.6) | 23.8 (22.8–24.8)1 | 13.0 (10.3–15.7)2 | 23.0 (18.8–27.4)1 | 8.6 (5.0–12.3)2 | |
| Living with children only | 309 (3.8) | 3.5 (3.1–3.9)2 | 5.1 (3.4–6.9)1,2 | 6.8 (4.2–9.4)1 | 4.7 (2.0–7.4)1,2 | |
| Living with partner and children | 1641 (20.8) | 21.4 (20.4–22.3)1 | 18.8 (15.6–21.8)1 | 18.6 (14.6–22.6)1,2 | 10.7 (6.8–14.8)2 | |
| Otherg | 2938 (39.7) | 38.4 (37.3–39.5)3 | 49.5 (45.5–53.5)2 | 34.2 (29.2–38.9)3 | 62.7 (56.3–68.8)1 | |
| Cannabis use (1+days), N(%) | 961 (12.5) | 6.9 (6.3–7.5)4 | 29.3 (26.0–32.5)2 | 34.9 (31.0–38.8)2 | 60.0 (54.3–65.6)1 | <.001 |
| Alcohol use (1+days), N(%) | 3531 (40.9) | 37.6 (36.4–38.7)3 | 47.5 (43.9–51.1)2 | 62.0 (58.1–66.0)1 | 62.2 (56.6–67.8)1 | <.001 |
| PHQ-2-Anxiety symptoms, N(%)h | 1428 (16.8) | 15.2 (14.4–16.1)3 | 22.7 (19.7–25.7)2 | 22.7 (19.7–25.7)2 | 32.7 (27.3–38.1)1 | <.001 |
| PHQ-2-Depressive symptoms, N(%)h |
938 (11.6) |
9.9 (9.2–10.6)3 |
18.2 (15.4–20.9)2 |
14.4 (11.6–17.2)2 |
32.4 (27.0–37.8)1 |
<.001 |
| Final Wave Assessmentsi | ||||||
| Working, N(%) | 4077 (58.1) | 59.0 (57.7–60.2)1 | 56.9 (53.2–60.7)1 | 58.2 (52.7–63.8)1 | 41.0 (34.2–47.6)2 | .02 |
| Currently married (vs. other), N(%) | 3962 (54.7) | 57.8 (56.6–59.1)1 | 40.2 (36.5–43.8)3 | 48.4 (44.1–52.7)2 | 29.2 (23.4–35.0)4 | <.001 |
| Cannabis use (1+days), N(%) | 766 (11.5) | 6.1 (5.5–6.7)4 | 31.7 (28.1–35.2)2 | 23.7 (19.9–27.4)3 | 65.5 (59.4–71.7)1 | <.001 |
| Alcohol use (1+days), N(%) | 2744 (37.1) | 34.6 (33.3–35.8)3 | 49.5 (45.7–53.4)1 | 41.6 (38.3–44.9)2 | 59.2 (52.8–65.6)1 | <.001 |
| PHQ-2-Anxiety symptoms, N(%)h | 790 (11.1) | 9.8 (9.0–10.5)3 | 15.1 (12.3–17.8)2 | 13.7 (10.6–16.7)2 | 27.1 (21.3–32.8)1 | <.001 |
| PHQ-2-Depressive symptoms, N(%)h | 743 (10.5) | 8.9 (8.2–9.7)3 | 17.3 (14.4–20.2)2 | 12.6 (9.9–15.3)2 | 29.4 (23.5–35.3)1 | <.001 |
dDifferences were calculated by the χ2/df from the overall test of auxiliary model for each covariate. Groups not sharing superscript numerals are significantly different (p < .05) in post-hoc pairwise contrasts for χ2 tests.
Total analysic sample N = 8306. Available data Ns = 7035–8306.
Unweighted N and weighted % are shown for categorical variables.
Membership probability (%) and 95% confidence interval are shown.
Assessed at each respondent's initial survey assessment.
Native American (American Indian/Alaska Native), Native Hawaiian, or Pacific Islander.
Other household structures included multigenerational households, households with roommates, etc.
Sum score was calculated using 2 items (Range = 0–6). Cutoff score ≥3.
Assessed at each respondent's last survey assessment across Dec 9, 2020–Mar 3, 2021 (i.e., last 3 waves).
3.2. Drug use frequency trajectories
Fit statistics of GMMs on drug use frequency with 1- to 5-class solutions supported a 4-class model (AIC = 37273.71, Entropy = .94, LMR P-Value<.001; see Table 2 ). Depicted in Fig. 1, the final GMM yielded the following four groups: (i) Stable Abstinence (85.7% [95%CI = 85.0–86.5] of the analytic sample; linear slope, p = .77; quadratic slope, p = .84]) with <1 mean past-week drug use days across all timepoints; (ii) Escalating Infrequent Use (7.1% [95%CI = 6.6–7.7]; linear, p < .001; quadratic, p < .001) with a mean of 0.2 past-week drug use days in March, increases across April to October (0.9 days), and reduced rate of increases in last 5 timepoints (November 2020–March 2021 range: 0.5–0.7). (iii) Use Cessation (4.3% [95%CI = 3.8–4.7]; linear, p < .001; quadratic, p < .001) with 1.1 March mean past-week drug use days that increased to 1.9 by April, but sharply decreased to zero or near zero across remaining timepoints (August 2020–March 2021 range: 0.00–0.02), and (iv) Stable Frequent Use (2.9% [95%CI = 2.5–3.3]; linear, p = .08; quadratic, p = .02) with 2.4 March past-week drug use days that increased to 3.5 in May and returned to baseline (May 2020–March 2021 range: 2.5–3.5).
Table 2.
Fit indices for growth mixture model for past-week drug use days outcome.a.
| Class # | AIC | BIC | SSA-BIC | Entropy | LMR-p |
|---|---|---|---|---|---|
| 1 | 74101.450 | 74122.524 | 74112.991 | – | – |
| 2 | 43726.140 | 43775.313 | 43753.068 | 0.963 | <.001 |
| 3 | 38982.475 | 39059.748 | 39024.792 | 0.950 | <.001 |
| 4 | 37273.712 | 37379.083 | 37331.416 | 0.941 | .001 |
| 5 | 36326.847 | 36460.317 | 36399.938 | 0.936 | .31 |
Abbreviations: AIC = Akaike Information Criterion. LMR p = The Lo–Mendell–Rubin (LMR) likelihood ratio test p-value.
Growth mixture modeling was conducted using number of drug use days indicators (N = 8306). Final model in bold font.
The demographic composition of the drug use trajectory groups differed from each other (Table 1). Notable results of pairwise comparisons to the Stable Abstinence trajectory group include higher proportions of 18-39-year olds, those living with children only, and those below the poverty threshold in three other drug use trajectory groups (e.g., the highest proportions in the Stable Frequent Use trajectory and second-highest in the Escalating Infrequent Use and Use Cessation trajectories). In addition, compared to the Stable Abstinence trajectory group, those in three drug use trajectory groups showed lower proportions of those with college degree, working, married at baseline, living with a partner only, and living with a partner and children.
In terms of behavioral health problems, the Stable Frequent Use trajectory showed the highest proportions of cannabis use and anxiety and depressive symptoms, and the Escalating Infrequent Use and Use Cessation trajectories showed higher proportions of those using cannabis and alcohol and reporting moderate-to-severe anxiety and depressive symptoms at baseline, compared to the Stable Abstinence trajectory.
With regards to the covariates assessed at each respondent's last survey assessment across Dec 9, 2020–Mar 3, 2021, the Stable Frequent Use trajectory group, compared to other trajectory groups, consistently included the highest proportion of cannabis and alcohol users and those with anxiety and depressive symptoms at the final timepoint. The Stable Abstinence trajectory group had the lowest proportions of cannabis and alcohol users and those with anxiety and depressive symptoms and the highest proportion of married couples. The Use Cessation trajectory group included significantly lower proportions of cannabis and alcohol users compared to the Escalating Infrequent Use trajectory group.
4. Discussion
Prior research has identified distinct trajectories of substance use in the general population in response to public health crises that occurred prior to the COVID-19 pandemic (Joshi and Cerdá, 2017). In this study, we identified trajectories of drug use over the first year of the COVID-19 pandemic (March 2020–March 2021) using data from a nationally-representative sample of U.S. adults. The results of our study provide some of the first longitudinal evidence pertaining to use of drugs other than alcohol, nicotine, or cannabis during the pandemic, which could be used to inform public health interventions and identify vulnerable subgroups.
We identified four distinct trajectories of drug use based on past-week frequency of use. The vast majority of the sample had very low or no drug use throughout the study period (85.7%), reporting less that one day of use in the past week on average. Two subgroups had fluctuating levels of drug use across the study period. One peaked shortly after the onset of the pandemic at 1.9 days of past-week use and declined thereafter demonstrating a pattern of use cessation 4–5 months into the pandemic (4.3% of the sample). The other group reported steadily increasing drug use frequency that stabilized later in the study period and using at an infrequent, but consistent basis throughout the pandemic. After two months into the pandemic, this group use frequency ranged from approximately once every two weeks (mean weekly use 0.5) to once per week (mean weekly use 0.9 days) throughout the remainder of the study follow-up (7.1% of the sample). Finally, a small subgroup displayed relatively frequent drug use consistently across the study period, ranging from 2.5 to 3.5 days of use in the past week (2.9% of the sample). These trajectories largely affirm prior studies of substance use after public health disasters, which have observed modest, temporally variable increases in substance use for some people (Joshi and Cerdá, 2017; North, 2017).
Mapping of sociodemographic characteristics onto trajectories reflects both the general epidemiology of substance use and the epidemiology of substance use following public health crises (Galea et al., 2004; Merikangas and McClair, 2012; North, 2017). Compared to the stable abstinence group, the other subgroups were more likely to be Hispanic or Black, younger in age, unemployed, living with children only, and living below the federal poverty line, and less likely to have received a college degree, be married, be living with a partner only, or be living with a partner and children. With regards to covariates which could have changed during the pandemic and were assessed by respondent's last survey assessment across Dec 9, 2020–Mar 3, 2021, these groups also tended to have higher levels of alcohol and cannabis use, as well as higher anxiety and depressive symptoms, with the highest levels of these behaviors seen in the stable frequent use group. Individuals affected by stress, isolation, grief, or job loss may have been particularly likely to increase drug use as a means of coping, which is suggested by the self-medication model (MacMillan et al., 2021; Markou et al., 1998). Alternatively, the precipitation model proposes that drug use may trigger the onset of psychopathological symptoms via neurotoxic effects (Brady and Sinha, 2005). The extent to which our pattern of findings supports either model, however, should be interpreted with caution due to the correlational nature of our analyses. Altogether, the sociodemographic and behavioral correlates identified in this study are similar to those identified in studies of mental distress, alcohol, and cannabis use during the pandemic (Brenneke et al., 2022; Nordeck et al., 2022; Riehm et al., 2021) and add urgency to intervene among these vulnerable populations.
Most prior studies have found that changes in substance use in response to public health crises do not tend to translate into new-onset substance use disorders (North, 2017). However, given that the COVID-19 pandemic departs from traditional models of public health crises (Galea et al., 2020) and that protracted drug use may result in adverse health events (Palamar et al., 2019), our results still warrant public health attention, particularly as the COVID-19 pandemic continues. The pattern of use in the use cessation group may reflect an initial response to stress, uncertainty, and/or boredom associated with the onset of the pandemic that dissipates over time (Joshi and Cerdá, 2017). This group may benefit from rapidly disseminated interventions in the initial stages of a crisis, such as positive public health messaging and telephone or web-based services that can deliver social support and crisis intervention services (Arendt et al., 2020; Bäuerle et al., 2020; Zhou et al., 2020). Additionally, from a prevention standpoint, the escalating infrequent use group is of particular interest. Relative to the use cessation group, the escalating infrequent use group tended to report more frequent use of other substances, which may reflect a generalized vulnerability for substance use or poly-substance use. Gradually increasing use in this group may also reflect experimentation during the early months of the pandemic, which translated into more habitual use as the pandemic continued. Screening and Brief Intervention (SBI) is designed to prevent escalation in substance use, and may thus be especially relevant for this group; opportunities to scale up SBI during the COVID-19 pandemic, such as within telehealth frameworks, have been discussed elsewhere (Ghosh and Sharma, 2021). Finally, the patterns of substance use observed in the stable frequent use group may reflect more chronic problems that pre-date the COVID-19 pandemic. This group may be best served by increasing and maintaining access to substance use services, possibly via tele-health, which policy initiatives have sought to increase access to (Lin et al., 2020). Importantly, the three subgroups with any level of drug use were generally characterized by poorer mental health, so interventions that address the mental health implications of the pandemic in the general population are also likely to be valuable for these groups.
This study has limitations. Due to survey limitations, we were only able to examine drug use broadly, rather than individual drugs (i.e., ecstasy, cocaine, non-medical use of prescription drugs, etc.), and at least one study suggests that patterns of use may have differed by each drug (Palamar et al., 2021). We examined frequency of use in the past week, which may not reflect changes in other aspects of use, such as dosage or intensity. The UAS relies on self-report data, which may be affected by recall bias, though this is likely reduced by the relatively frequent, bi-weekly survey schedule. Substance use was not assessed for participants prior to the onset of the pandemic, which limits our understanding of pre-pandemic trends. GMMs prioritize a parsimonious set of trajectories to summarize heterogeneity; not all respondents in our study will have had patterns of drug use that map closely to one of the trajectories identified in our analyses. On the other hand, strengths of this study include repeated monthly assessments from the start of the COVID-19 pandemic for a full year, which is not available from other data sources, and the separation of other drug use from cannabis and alcohol.
In summary, we identified distinct trajectories of drug use during the first year of the COVID-19 pandemic among a nationally-representative sample of adult in the U.S. In aggregate, increases in drug use were modest and returned to baseline by the end of the study period; however, our analyses uncovered subpopulations for whom increases were sharper and sustained, which warrants public health attention. The sociodemographic and behavioral correlates of each subgroup provide opportunities to optimize the targeted delivery of preventive interventions for substance use during the COVID-19 pandemic and future public health emergencies.
Funding
Dr. Riehm was supported by the National Institute of Mental Health (NIMH) Psychiatric Epidemiology Training Program (5T32MH013043-50) at Columbia University. Dr. Smail was supported by National Institute on Aging (NIA) Translational Research on Aging and Mobility (TRAM) program (T32AG062728). Research reported in this publication was supported by National Institute on Drug Abuse (NIDA) Award Number K24048160 (Leventhal). The Understanding America Study was supported by the Bill & Melinda Gates Foundation and a grant from the National Institute on Aging (5U01AG054580). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Understanding America Survey.
Credit statement
Kira E Riehm: Conceptualization, Methodology, Writing - Original Draft, Writing - Review & Editing, Junhan Cho: Conceptualization, Data Curation, Formal Analysis, Writing - Review & Editing, Emily J Smail: Conceptualization, Data Curation, Writing - Review & Editing, Eric Pedersen: Conceptualization, Writing - Review & Editing, Jungeun Olivia Lee: Conceptualization, Writing - Review & Editing, Jordan P Davis: Conceptualization, Writing - Review & Editing, Adam M Leventhal: Conceptualization, Methodology, Writing - Review & Editing, Supervision.
Declaration of competing interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2022.07.055.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Alattar L., Messel M., Rogofsky D. An introduction to the understanding America study Internet panel. Soc. Secur. Bull. 2018;78:13. [Google Scholar]
- Arendt F., Markiewitz A., Mestas M., Scherr S. COVID-19 pandemic, government responses, and public mental health: investigating consequences through crisis hotline calls in two countries. Soc. Sci. Med. 2020;265 doi: 10.1016/j.socscimed.2020.113532. [DOI] [PubMed] [Google Scholar]
- Asparouhov T., Muthén B. Auxiliary variables in mixture modeling: using the BCH method in Mplus to estimate a distal outcome model and an arbitrary secondary model. Mplus Web Notes. 2014;21(2):1–22. [Google Scholar]
- Bäuerle A., Graf J., Jansen C., Dörrie N., Junne F., Teufel M., Skoda E.-M. An e-mental health intervention to support burdened people in times of the COVID-19 pandemic: CoPE it. J. Publ. Health. 2020 doi: 10.1093/pubmed/fdaa058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamini Y., Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. Roy. Stat. Soc. B. 1995;57(1):289–300. [Google Scholar]
- Brady K.T., Sinha R. Co-occurring mental and substance use disorders: the neurobiological effects of chronic stress. Am. J. Psychiatr. 2005;162(8):1483–1493. doi: 10.1176/appi.ajp.162.8.1483. [DOI] [PubMed] [Google Scholar]
- Brenneke S.G., Nordeck C.D., Riehm K.E., Schmid I., Tormohlen K.N., Smail E.J.…Thrul J. Trends in cannabis use among U.S. adults amid the COVID-19 pandemic. Int. J. Drug Pol. 2022;100 doi: 10.1016/j.drugpo.2021.103517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed.: Atenei Parmensis. 2020;91(1):157. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M.É., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R.…Barger L.K. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. MMWR (Morb. Mortal. Wkly. Rep.) 2020;69(32):1049. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M.É., Lane R.I., Wiley J.F., Czeisler C.A., Howard M.E., Rajaratnam S.M.W. Follow-up survey of US adult reports of mental health, substance use, and suicidal ideation during the COVID-19 pandemic, September 2020. JAMA Netw. Open. 2021;4(2) doi: 10.1001/jamanetworkopen.2020.37665. e2037665-e2037665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S., Merchant R.M., Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern. Med. 2020 doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- Galea S., Nandi A., Vlahov D. The social epidemiology of substance use. Epidemiol. Rev. 2004;26(1):36–52. doi: 10.1093/epirev/mxh007. [DOI] [PubMed] [Google Scholar]
- Ghosh A., Sharma K. Screening and brief intervention for substance use disorders in times of COVID-19: potential opportunities, adaptations, and challenges. Am. J. Drug Alcohol Abuse. 2021;47(2):154–159. doi: 10.1080/00952990.2020.1865996. [DOI] [PubMed] [Google Scholar]
- Holland K.M., Jones C., Vivolo-Kantor A.M., Idaikkadar N., Zwald M., Hoots B.…Houry D. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiatr. 2021;78(4):372–379. doi: 10.1001/jamapsychiatry.2020.4402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ignaszewski M.J. The epidemiology of drug Abuse. J. Clin. Pharmacol. 2021;61(S2):S10–S17. doi: 10.1002/jcph.1937. [DOI] [PubMed] [Google Scholar]
- Joshi S., Cerdá M. In: Textbook of Disaster Psychiatry. 2 ed. Raphael B., Fullerton C.S., Weisaeth L., Ursano R.J., editors. Cambridge University Press; Cambridge: 2017. Trajectories of health, resilience, and illness; pp. 76–86. [Google Scholar]
- Kapteyn A., Angrisani M., Bennett D., de Bruin W.B., Darling J., Gutsche T., et al. Tracking the effect of the COVID-19 pandemic on the lives of American households. Surv. Res. Methods. 2020;14(2) doi: 10.18148/srm/2020.v14i2.7737. [DOI] [Google Scholar]
- Karpman M., Zuckerman S., Gonzalez D., Kenney G.M. Urban Institute; 2020. The COVID-19 Pandemic Is Straining Families' Abilities to Afford Basic Needs.https://www.urban.org/sites/default/files/publication/102124/the-covid-19-pandemic-is-straining-families-abilities-to-afford-basic-needs_2.pdf Available at: [Google Scholar]
- Kochhar R. Pew Research Center; 2020. Hispanic Women, Immigrants, Young Adults, Those with Less Education Hit Hardest by COVID-19 Job Losses.https://www.pewresearch.org/fact-tank/2020/06/09/hispanic-women-immigrants-young-adults-those-with-less-education-hit-hardest-by-covid-19-job-losses Available at: [Google Scholar]
- Kroenke K., Baye F., Lourens S.G. Comparative validity and responsiveness of PHQ-ADS and other composite anxiety-depression measures. J. Affect. Disord. 2019;246:437–443. doi: 10.1016/j.jad.2018.12.098. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W., Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ–4. Psychosomatics. 2009;50(6):613–621. doi: 10.1016/S0033-3182(09)70864-3. [DOI] [PubMed] [Google Scholar]
- Lin L., Fernandez A.C., Bonar E.E. Telehealth for substance-using populations in the age of Coronavirus disease 2019: recommendations to enhance adoption. JAMA Psychiatr. 2020;77(12):1209–1210. doi: 10.1001/jamapsychiatry.2020.1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacMillan T., Corrigan M.J., Coffey K., Tronnier C.D., Wang D., Krase K. Exploring factors associated with alcohol and/or substance use during the COVID-19 pandemic. Int. J. Ment. Health Addiction. 2021 doi: 10.1007/s11469-020-00482-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manea L., Gilbody S., Hewitt C., North A., Plummer F., Richardson R.…McMillan D. Identifying depression with the PHQ-2: a diagnostic meta-analysis. J. Affect. Disord. 2016;203:382–395. doi: 10.1016/j.jad.2016.06.003. [DOI] [PubMed] [Google Scholar]
- Markou A., Kosten T.R., Koob G.F. Neurobiological similarities in depression and drug dependence: a self-medication hypothesis. Neuropsychopharmacology. 1998;18(3):135–174. doi: 10.1016/S0893-133X(97)00113-9. [DOI] [PubMed] [Google Scholar]
- Merikangas K.R., McClair V.L. Epidemiology of substance use disorders. Hum. Genet. 2012;131(6):779–789. doi: 10.1007/s00439-012-1168-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B., Muthén L.K. Integrating person‐centered and variable‐centered analyses: growth mixture modeling with latent trajectory classes. Alcohol Clin. Exp. Res. 2000;24(6):882–891. [PubMed] [Google Scholar]
- Muthén L. Muthen & Muthen; Los Angeles: 2015. Mplus User's Guide. BO.(1998-2015) [Google Scholar]
- Nordeck C.D., Riehm K.E., Smail E.J., Holingue C., Kane J.C., Johnson R.M.…Thrul J. Changes in drinking days among United States adults during the COVID-19 pandemic. Addiction. 2022;117(2):331–340. doi: 10.1111/add.15622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- North C.S. In: Textbook of Disaster Psychiatry. 2 ed. Raphael B., Fullerton C.S., Weisaeth L., Ursano R.J., editors. Cambridge University Press; Cambridge: 2017. Epidemiology of disaster mental health: the foundation for disaster mental health response; pp. 27–43. [Google Scholar]
- Nylund K.L., Asparouhov T., Muthén B.O. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct. Equ. Model.: A Multidiscip. J. 2007;14(4):535–569. [Google Scholar]
- Palamar J.J., Acosta P., Le A., Cleland C.M., Nelson L.S. Adverse drug-related effects among electronic dance music party attendees. Int. J. Drug Pol. 2019;73:81–87. doi: 10.1016/j.drugpo.2019.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar J.J., Le A., Acosta P. Shifts in drug use behavior among electronic dance music partygoers in New York during COVID-19 social distancing. Subst. Use Misuse. 2021;56(2):238–244. doi: 10.1080/10826084.2020.1857408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plummer F., Manea L., Trepel D., McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen. Hosp. Psychiatr. 2016;39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005. [DOI] [PubMed] [Google Scholar]
- Riehm K.E., Holingue C., Smail E.J., Kapteyn A., Bennett D., Thrul J.…Stuart E.A. Trajectories of mental distress among U.S. Adults during the COVID-19 pandemic. Ann. Behav. Med. 2021;55(2):93–102. doi: 10.1093/abm/kaaa126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou X., Snoswell C.L., Harding L.E., Bambling M., Edirippulige S., Bai X., Smith A.C. The role of telehealth in reducing the mental health burden from COVID-19. Telemedicine e-Health. 2020;26(4):377–379. doi: 10.1089/tmj.2020.0068. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.