Figure 1.
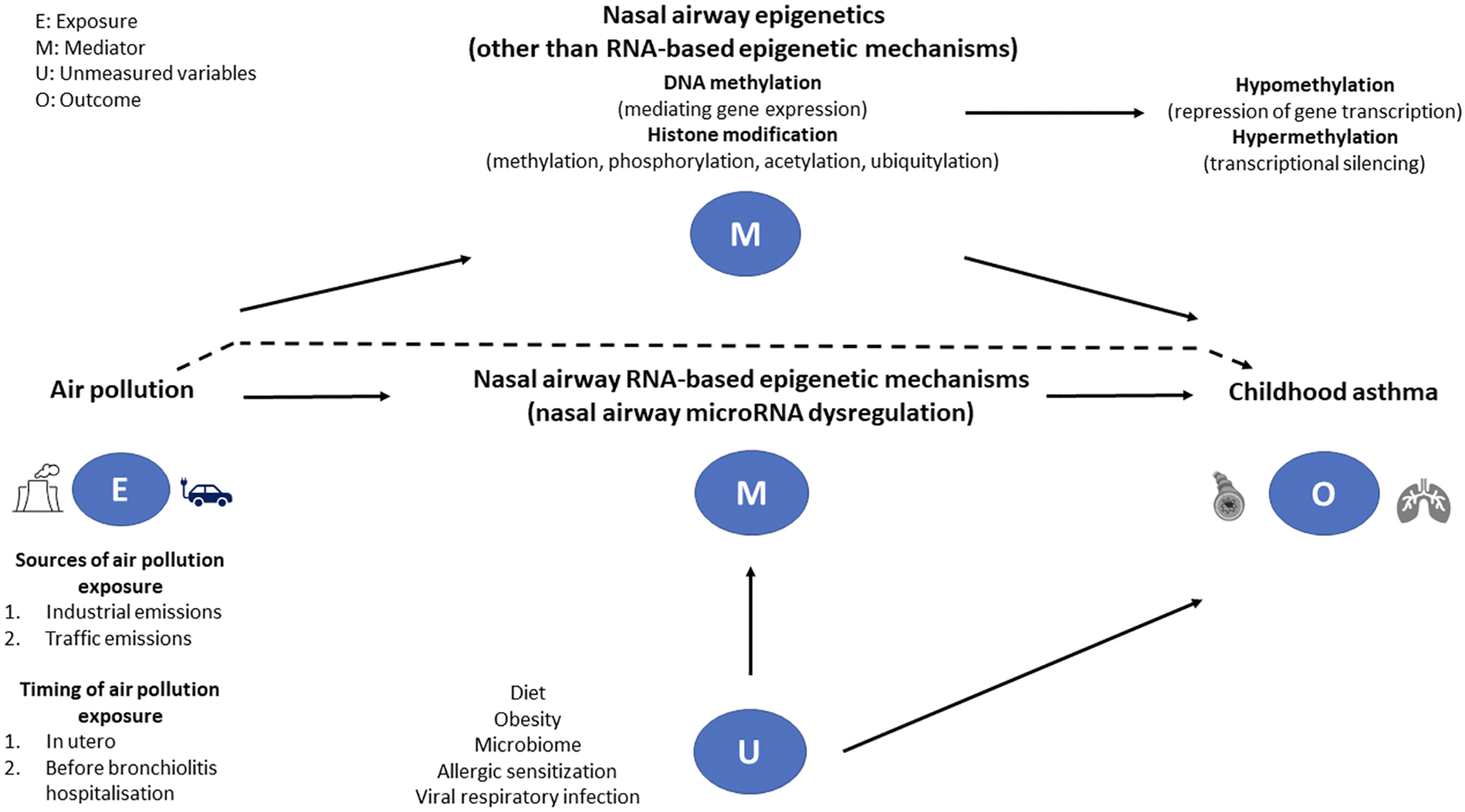
A directed graph describing a proposed causal relationship between the exposure (air pollution), mediators (nasal airway RNA- and non-RNA-based mechanisms), and outcome (childhood asthma) among infants with severe bronchiolitis. The dotted line represents the direct effect of air pollution on the development of asthma. We suggest that nasal microRNA post-transcriptional regulation is a major epigenetic mechanism underlying the regulation of multiple biological pathways within the innate and adaptive immune systems and potentially mediates the exposure-outcome relationship. Several studies describe, in response to air pollution exposure, up- or down-regulation of specific microRNAs in nasal airway samples. However, it is unclear whether, in infants with severe bronchiolitis, a specific nasal airway microRNA signature mediates the pathogenesis of childhood asthma. Other epigenetic mechanisms (e.g., DNA methylation and histone modification) may also act as mediators in the causal pathway. Other factors—such as diet, obesity, microbial exposures (microbiome), allergic sensitization, and viral respiratory infections—are associated with both nasal airway microRNA regulation and asthma development, thereby serving as potential confounders.
