Abstract
Intravenous anesthetic agents such as midazolam, propofol, and ketamine are routinely used to provide anesthesia and sedation. They have been shown to effectively induce and maintain amnesia, sedation, and hypnosis in various patient groups and clinical settings. However, all anesthetic agents have the potential to cause unwanted side effects such as hemodynamic instability, respiratory depression, or slow recovery due to prolonged post-procedural sedation. Remimazolam, a recently approved benzodiazepine for general anesthesia and procedural sedation in Korea, has been successfully used for these purposes. To date, inconclusive knowledge has been obtained regarding the use of remimazolam in different patient populations and under various surgical conditions. With respect to the specific pharmacokinetic and pharmacodynamic characteristics of remimazolam, the use of remimazolam is expected to increase providing safe general anesthesia and sedation. This review aims to provide an overview of the basic and clinical pharmacology of remimazolam and to compare it with midazolam and propofol.
Keywords: Amnesia, Anesthesia, Benzodiazepine, Conscious sedation, Hypnosis, Remimazolam
Introduction
Remimazolam is a rapidly metabolized benzodiazepine (BZD) that has been approved for general anesthesia and procedural sedation in Korea since 2021. It shows the typical pharmacodynamic profile of other BZDs (e.g., midazolam), but has high organ-independent elimination clearance. It is rapidly metabolized by nonspecific esterases [predominantly carboxylesterase 1A (CES 1A)], mainly localized in the human liver, to CNS7054, a so-called inactive metabolite with reduced binding affinity with a 300 to 400 times reduced binding affinity at the γ-aminobutyric acid (GABA) type A receptor. After administration, plasma concentrations of remimazolam predictably and rapidly decrease, and with adequate dosing, there is no prolonged sedative effect. Though it has been approved in Korea for general anesthesia, further clinical experience with remimazolam as well as evidence-based approaches for dosing and drug handling are needed for its safe and efficient use in various patient populations and clinical conditions. Therefore, the aim of this review article is to provide an overview of the specific pharmacodynamic and pharmacokinetic characteristics of remimazolam relevant to its clinical application as a modern intravenous sedative and anesthetic agent.
Basic knowledge on intravenous anesthetic agents
Mechanism of action of intravenous anesthetic agents
While the introduction of general anesthesia was a revolutionary achievement in medical history, the mechanism of action of anesthetic agents is still not fully understood. The concept that anesthetic agents produce neuro-depression in specific areas of the central nervous system by enhancing the effect of inhibitory neurotransmitters (especially GABA), reducing the effect of excitatory neurotransmitters, and suppressing specific neuronal network activity necessary for consciousness and arousal has been generally accepted [1,2]. The GABA receptor system is the main inhibitory receptor population in the human central nervous system and the main target receptor for intravenous anesthetic agents that induce general anesthesia [1]. Most intravenous anesthetic agents, such as barbiturates, BZDs, propofol, and etomidate, bind to GABA type A receptors, except for ketamine, which mainly acts via the N-methyl-D-aspartate (NMDA) receptor along with other receptor types. All intravenous anesthetic agents can induce amnesia, hypnosis, sedation, unconsciousness, and immobility (muscle-suppression), although immobility is achieved to a greater extent with inhalational anesthetic agents. Intravenous anesthetic agents may also induce cardiovascular depression, respiratory depression, or pain during injection.
An ideal intravenous anesthetic agent and soft drug
An ideal intravenous anesthetic agent (Table 1) has not yet been developed. All the available intravenous anesthetic agents can cause undesirable side effects. Therefore, balanced anesthesia using a combination of different anesthetic agents at the lowest possible doses to achieve adequate anesthesia has been used in the past to minimize side effects in daily practice. Modern anesthetic agents must therefore be effective, efficient, and well tolerated. To improve usability, new intravenous anesthetic agents should also offer a drug effect that is predictable, with a rapid onset and offset. Drug development programs are searching for intravenous anesthetic agents that are specifically structured to undergo rapid biotransformation into inactive metabolites. This type of drug is called a “soft drug,” and remifentanil is a well-known prototype. Remimazolam, which is the newest “soft drug," has been developed based on the midazolam molecular structure (Figs. 1 and 2) and is a structural analog with an added ester side chain. After discontinuing the administration of a soft drug, the effects rapidly disappear, as the parent compound is quickly converted to inactive or much less active metabolites [3]. Anesthetic soft drugs can be further characterized by pharmacologic efficiency, which is an easy dosing scheme with a superior care-to-treatment-cost ratio, rapid restoration of protective reflexes, rapid return of spontaneous ventilation, and reduced need for postoperative care monitoring [3].
Table 1.
Ideal Intravenous Anesthetic Agent
| Physical and chemical properties | Pharmacology |
|---|---|
| Chemically stable | Painless injection |
| Water soluble | Low incidence of thrombophlebitis |
| No additives/No reconstitution required | Harmless on extravasation and intraarterial injection |
| Long shelf-life | Low incidence of adverse reactions |
| Compatible with other intravenous fluids or drugs | Smooth onset of anesthesia |
| Bacteriostatic | No associated unwanted movements |
| Anticonvulsant, antiemetic, and analgesic effects | |
| No associated respiratory depression or bronchodilation | |
| No cardiovascular depression or stimulation | |
| Predictable recovery | |
| Rapid conversion to non-active metabolites | |
| No hepatic or renal impairment | |
| No suppression of corticosteroid synthesis | |
| No association with emergence phenomenon | |
| No teratogenic effects | |
| Not much accumulation in body tissues, maintenance of general anesthesia possible |
Fig. 1.
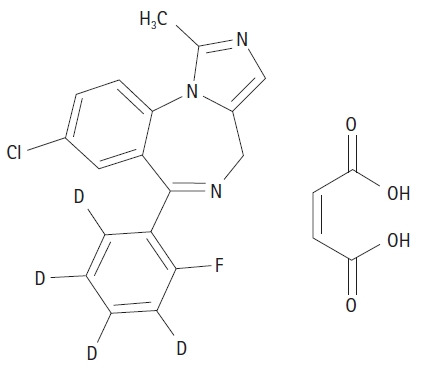
Chemical structure of midazolam.
Fig. 2.
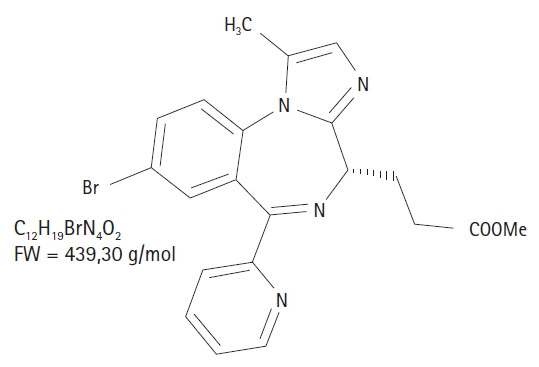
Chemical structure of remimazolam.
Midazolam, a well-known BDZ, is metabolized by hepatic cytochrome P450 enzymes and glucuronide conjugation [4]. However, in contrast to remimazolam, midazolam metabolites are active. The sedative or anesthetic effect of midazolam and its metabolites can be prolonged due to its organ dependency and much lower drug clearance rate, especially after prolonged drug administration or in patients with advanced age or reduced hepatic or renal function. Midazolam, in contrast to remimazolam, cannot be called a soft drug. To date, the use of midazolam for anesthesia and sedation has been limited mainly to postoperative intensive care unit sedation. Midazolam is no longer used for the maintenance of intravenous anesthesia.
Remimazolam
Basic pharmacology of remimazolam
Depending on the plasma and effect site concentrations (biophase) of remimazolam, the following effects can be reliably achieved: amnesia, sedation and hypnosis, unconsciousness, and some degree of immobility. In comparison to midazolam, remimazolam does not cause prolonged sedative effects after discontinuation because it is rapidly metabolized by nonspecific tissue esterases to CNS7054, the only active metabolite with an affinity for the GABA type A receptor that is 300 times lower and with no clinically relevant effect at the receptor site [5]. Remimazolam is a “soft drug” with the pharmacodynamic characteristics of a BZD. Remimazolam shows some characteristics of an ideal intravenous anesthetic agent. It is water-soluble, has a high clearance rate that is organ-independent, and shows more benign hemodynamic and respiratory side effects than propofol.
The pharmacokinetics of remimazolam have been described using non-compartmental and compartmental modeling approaches as well as a recirculatory model [6–8]. In these pharmacokinetic models, total body clearance was found to be independent of body weight, which was remarkable. In a clinical trial, Lu et al. [9] estimated that a body-weight-independent single dose of 11.43 mg of remimazolam achieves a 90% (ED90) probability for adequate sedation during colonoscopy. This study illustrates body-weight-independent and simple dosing concepts for remimazolam. Total body clearance values have been estimated at 70.3 ± 13.9 L/h by Antonik et al. [8] 66.7 ± 2.59 L/h by Wiltshire et al. [7], and 69 ± 7.2 L/h by Schuttler et al. [6]. In contrast, the total body clearance of midazolam has been measured at 22.6 ± 8.36 L/h by Wiltshire et al. [7]. Thus, the clearance of midazolam appears to be nearly one-third the total body clearance of remimazolam. The total body clearance for propofol has been measured at 102 ± 18 L/h by Gepts et al. [10] in a rather historic but still used dataset, incorporated as the “Marsh model” [11] in commercially available target-controlled infusion (TCI) systems for propofol. Therefore, the estimated total body clearance rate of propofol is approximately 25–30% higher than that of remimazolam, but the clearance of propofol is organ-dependent and can be reduced in hepatic disease. In contrast, Stöhr et al. [12] showed that neither hepatic nor renal dysfunction impairs the clearance of remimazolam. A total volume of distribution at steady state (Vdss) of approximately 35 L has been described for remimazolam [6,8], whereas for propofol, the Vdss has been estimated at 400 L [10], which is approximately 10 times the Vdss of remimazolam. A smaller Vdss speeds up drug elimination and patient recovery, as it indicates that less drug has accumulated in the body during administration, and so less has to be cleared after discontinuation. Based on pharmacokinetic simulations, context-sensitive decrement times of a 50% decrease in the plasma and effect site concentrations of remimazolam are very comparable to the simulated times for propofol (Figs. 3 and 4). In these simulations, the pharmacokinetic dataset of Gepts/Marsh et al. [11] for propofol and the pharmacokinetic dataset of Schuttler et al. [6] for remimazolam were used. The decrement time is shorter for remimazolam when we look at the decrease in plasma concentration, but it is approximately 3 to 4 min longer when we look at the decrease in the effect site concentration. This is more consistent with the clinical finding that recovery times after remimazolam anesthesia tend to be approximately 1–5 min longer when directly compared to propofol [13].
Fig. 3.
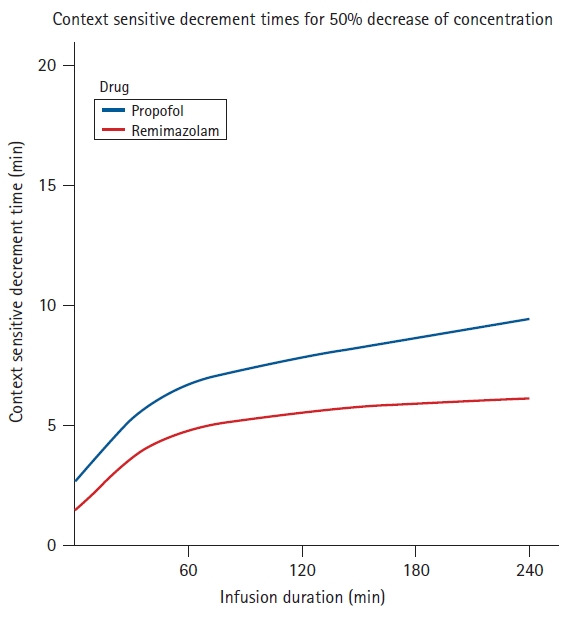
Simulation of context-sensitive decrement times of plasma concentrations for remimazolam and propofol (remimazolam ke0 = 0.25 min-1; propofol ke0 = 0.26 min-1).
Fig. 4.
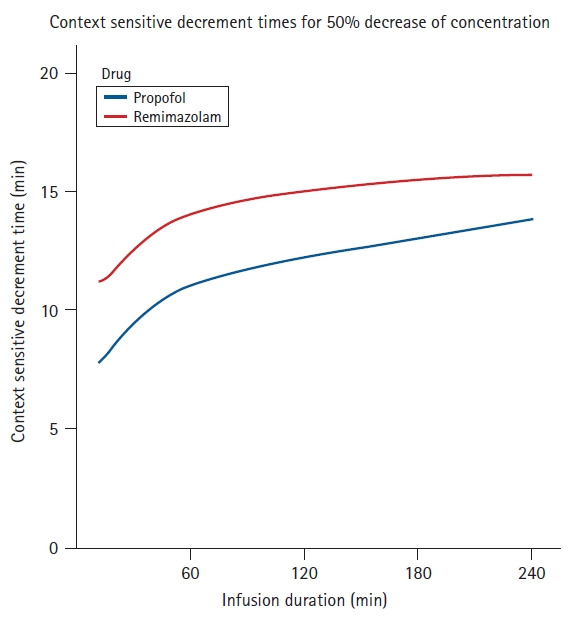
Simulation of the context-sensitive decrement times of effect concentrations for remimazolam and propofol (remimazolam ke0 = 0.25 min-1; propofol ke0 = 0.26 min-1).
The transfer constant ke0 (1/min) describes the speed of drug exchange between the central compartment and the effect compartment or the biophase. A ke0 of approximately 0.25 min-1 has been estimated for remimazolam using the modified observer’s assessment of alertness and sedation (MOAA/S) scale as a parameter of the electroencephalogram (EEG) in volunteers of both sexes by Wiltshire et al. [7]. A ke0 value of 0.33 has been described by Eisenried et al. [14] in young male healthy volunteers using the beta ratio of the EEG as a pharmacodynamic parameter. A larger ke0 value would speed up substance exchange between the effect compartment and central compartment and thus shorten the induction and recovery times. From a scientific point of view, insufficient data have been published to date regarding the exact estimation of the ke0 value of remimazolam for the bispectral index (BIS). This is the most clinically relevant EEG parameter when remimazolam is administered to induce and maintain general anesthesia or sedation.
Interaction modeling between opioids and remimazolam during general anesthesia has only been described for remifentanil in a publication by Zhou et al. [15], in which the BIS was the pharmacodynamic effect parameter. This published interaction model for remimazolam and remifentanil during general anesthesia is inconclusive, as the interaction only shows a relevant effect and a weak interaction up to a remifentanil dosing of 0.5 µg/kg/min, and with higher dosages of remifentanil, the interaction is further reduced. This might be explained by the study designs of the re-evaluated trials, as the whole range of clinically relevant remifentanil and remimazolam concentrations were not studied [15]. Even more relevant for the clinical use of remimazolam is its anesthetic drug potency compared to that of propofol, which is described by the half-maximal effective concentration (EC50). EC50 is the plasma concentration at the time when 50% of the maximal effect for a pharmacodynamic parameter (e.g., the BIS) is achieved. In the study conducted by Wiltshire et al. [7], a decrease in the maximum BIS of 50% was achieved with a remimazolam effect site concentration of 0.259 µg/ml, whereas for propofol, the EC50 value for the BIS was estimated as 1.78 ± 0.67 µg/ml in a publication by Mourisse et al. [16]. Considering these published EC50 values, remimazolam is much more potent than propofol in terms of the effect-site concentrations estimated for the same effect on the BIS. This may explain the slightly prolonged recovery times of remimazolam compared to propofol, as a decrease of the effect site concentration of propofol by 50% reduces the anesthetic effect more than a reduction in the effect site concentration of remimazolam by 50%.
In summary, although the most accurate pharmacokinetic parameters of remimazolam have been described, this is not the case for the pharmacodynamic parameters, such as EC50 and the transfer constant ke0. Further studies are needed to validate these important pharmacological parameters of remimazolam.
Clinical pharmacology of remimazolam
The hemodynamic stability of remimazolam, especially when compared to propofol, is remarkable. Most intravenous anesthetic agents besides ketamine exhibit dose-dependent cardiovascular depressive effects. These cardiovascular effects can be explained by a dose-dependent decrease in systemic vascular resistance as well as a dose-dependent decrease in cardiac contractility. The effects of remimazolam on intracellular calcium homeostasis in endothelial and neuronal cells have not yet been fully elucidated. Urabe et al. [17] studied the effect of remimazolam on the intracellular concentration of calcium. They described how remimazolam can increase the calcium concentration in endothelial and neuronal cells via the G-protein coupled receptors (GPCRs)-inositol 1,4,5-triphosphate (IP3) pathway. They discussed how the effect is reversible, whereas, when propofol is administered, this effect is different and irreversible. This might be the first step to explaining the different hemodynamic effects of remimazolam compared to propofol, possibly modulated by different effects on the intracellular calcium homeostasis of endothelial cells.
Decreased blood pressure with a mean arterial pressure below 65 mmHg for > 1 min is associated with an increased incidence of postoperative myocardial injury or acute kidney injury [18]. As remimazolam is a BZD, better hemodynamic stability than propofol can be expected. Frölich et al. compared the hemodynamic effects of propofol, midazolam, and dexmedetomidine. They found that dexmedetomidine and propofol reduced the arterial blood pressure in a dose-dependent manner. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were maintained in the midazolam group during induction of mild-to-moderate sedation in American Society of Anesthesiologists Physical Status (ASA PS) I human volunteers of both sexes; a significant decrease in the SBP and DBP occurred with the use of propofol [19]. Lim et al. compared the cardiovascular effects of the co-administration of midazolam (0.03 mg/kg) and a reduced dose of propofol (0.8 mg/kg) to a propofol dose of 1.2 mg/kg, each combined with remifentanil for induction of anesthesia in ASA PS I to II patients of both sexes aged > 65 years. The co-administration of midazolam and a lower dose of propofol reduced the time to loss of consciousness, and the decrease in mean arterial blood pressure before, immediately after, and 3 min after intubation was significantly smaller [20]. The hemodynamic effects of remimazolam has the similar characteristics with midazolam. Moreover, remimazolam shows rapid on-set and off-set. Therefore, remimazolam is associated with the better hemodynamic stability than other intravenous anesthetic agents, including propofol.
The concentration of intravenous anesthetic agents and the anesthetic effects over time can be more accurately controlled with the use of a TCI system than with a manually controlled infusion system. Several research groups have investigated and described pharmacokinetic and pharmacodynamic models of remimazolam. Sufficient pharmacokinetic data have been published to further develop and test a TCI system for remimazolam in the near future. Insufficient data have been published describing the concentration-effect relationship of remimazolam on typical EEG parameters such as the BIS during general anesthesia and during co-administration with an opioid in patients [6,14,15]. Further clinical investigations are necessary to clearly define the pharmacodynamic interactions between remimazolam and different opioids in a clinical setting. The parameter “ke0” is important for calculating the speed at which the effect-site concentrations of remimazolam will increase or decrease. This parameter is necessary for a TCI system to directly model and target effect site concentrations and to increase the adjustability of the drug effect over time, especially to shorten recovery times by adequate dosing.
Remimazolam for anesthetic induction and maintenance
For anesthesia induction and maintenance, remimazolam should be compared with propofol. Propofol has the following disadvantages when used for anesthetic induction and maintenance: 1) pain on injection, 2) decrease in blood pressure, 3) decrease in heart rate, 4) respiratory depression, and 5) propofol infusion syndrome (very rare). In the following, we present clinical trial results comparing remimazolam and propofol for the induction and maintenance of general anesthesia.
Dai et al. [21] evaluated the safety and efficacy of remimazolam for anesthetic induction compared with propofol at 2 mg/kg in 190 patients with ASA PS I or II. A bolus dose of sufentanil (0.3 to 0.5 µg/kg) was administered 1 min before anesthetic induction. Anesthesia was successfully induced with remimazolam at 0.2 mg/kg (group R1), 0.3 mg/kg (group R2), and 0.4 mg/kg (group R3) in 89%, 94%, and 100% of patients within 1 min, respectively. Successful induction rates were not significantly different between the R2, R3, and propofol groups. Dai et al. [21] also compared the hypotension rate for the three induction doses of remimazolam (0.2 mg/kg, 0.3 mg/kg, and 0.4 mg/kg) to that for the induction dose of propofol (group P) at 2 mg/kg. Hypotension during induction, defined as a mean arterial blood pressure < 65 mmHg or a systolic blood pressure decrease to < 70% of baseline values, occurred in 13% of patients in group R1 and 24% of patients in group R2. The incidence of hypotension was significantly less in groups R1 and R2 compared to group P (44%). This study has the limitation that the anesthetic drug effect over time was not exactly comparable between the three remimazolam groups and the propofol group. Sufentanil dosing was not standardized. Nevertheless, in this trial, remimazolam showed superior hemodynamic stability during anesthetic induction even though co-administered with sufentanil. Pain on injection was not reported in this trial for all three remimazolam groups; in contrast, it was reported in 27% of patients who had received propofol.
Zhang et al. [22] compared an induction dose of remimazolam (0.2 mg/kg) for anesthesia induction and 1.0 mg/kg/h for anesthesia maintenance to an induction dose of propofol (2 to 2.5 mg/kg) and a propofol maintenance dose of 3–6 mg/kg/h in patients with ASA PS I or II undergoing hysteroscopy. Analgesia was achieved with remifentanil using a TCI with an effect-site target concentration of 1.5 µg/ml in both groups. Remifentanil infusion was initiated after induction with remimazolam or propofol. Based on their definitions of adverse events, the authors reported less significantly low peripheral oxygen saturation values ≤ 95%, lower injection pain (2.4% vs. 80.5%), and less postoperative dizziness (0 vs. 24.4%) when remimazolam was used instead of propofol. They concluded that remimazolam is “a safer alternative to anesthesia during hysteroscopy." However, although awakening times were longer in the remimazolam groups (199 ± 80 s vs. 60 ± 12 s) in this trial, the post-anesthetic care unit length of stay was shorter in the remimazolam group (5.44 ± 1 min vs. 6.3 ± 1.9 min). The depth of anesthesia was monitored using the MOAA/S scale. Furuta et al. [23] presented a case report of successful induction and maintenance of general anesthesia with remimazolam during total mastectomy in a female patient aged 81 years with severe aortic valve stenosis. They concluded that general anesthesia using remimazolam preserved cardiac output in this patient and therefore, remimazolam might be a safe alternative for patients with severe aortic valve stenosis to avoid a further and critical decrease in cardiac contractility.
Liu et al. [24] compared two groups of 30 patients each that were induced with remimazolam 0.3 mg/kg at a constant infusion rate of 1.8 mg/kg/h or propofol as a TCI with a target plasma concentration of 2.5 µg/ml scheduled for valve replacement cardiac surgery. All patients received a sufentanil dose of 1 µg/kg at an infusion rate of 0.1 µg/kg/min. After 7 min, the patients were relaxed, and after 10 min or after the BIS decreased below 60, they were intubated. The primary outcome was the maximum change in heart rate compared to baseline, though the maximum change in mean arterial blood pressure was also evaluated. This study did not find a significant difference of heart rate change between the groups; however, in the remimazolam group, a significantly smaller decrease in mean arterial blood pressure during induction was noted. They concluded that remimazolam may be a safe and effective alternative to propofol for anesthetic induction in patients with cardiac valve disease.
As remimazolam is a BZD, the specific reversal agent flumazenil is available and can be used in clinical practice to further accelerate recovery times or specifically treat prolonged postoperative sedation. This is a valuable advantage compared to propofol because clinicians can easily discriminate between prolonged sedation and other postoperative pathologies, such as postoperative stroke, which would also impact the speed of postoperative recovery to full awareness. However, the routine use of flumazenil for the reversal of remimazolam should be prospectively evaluated for possible side effects and safety in future studies. The main differences between remimazolam and propofol are summarized in Table 2.
Table 2.
Comparison between Remimazolam and Propofol
| Remimazolam | Propofol | ||
|---|---|---|---|
| Anesthetic induction | Speed | Fast | Fast |
| Pain at administration | No | Yes | |
| Anesthetic maintenance | Hypotension | Less frequent, severe | More frequent, severe |
| Emergence from anesthesia | Speed | Fast | Fast |
| Reverse agent | Flumazenil | - |
Precipitation
Sasaki et al. [25] reported the precipitation of remimazolam after a bolus administration of 0.2 mg/kg with Ringer’s acetate solution. Yoshida et al. [26] also reported occlusion of an intravenous line running Ringer’s acetate solution when remimazolam was used at a concentration of 2 mg/ml. The solubility of remimazolam is higher at low pH than at high pH, and its solubility is higher in normal saline than in Ringer’s solution. Therefore, precipitation can occur when it is co-administered with Ringer’s solution. The risk of precipitation increases when a solution with a high remimazolam concentration and a low infusion rate of the maintenance fluid is used. This should be avoided.
Further evaluation of remimazolam
To precisely titrate remimazolam to a chosen pharmacodynamic effect, accurate pharmacokinetic and pharmacodynamic models are essential. To date, interaction modeling between opioids and remimazolam during general anesthesia has only been described for remifentanil in a publication by Zhou et al. [15], for which the BIS was used as a pharmacodynamic effect parameter. Further randomized controlled trials that precisely describe the pharmacodynamic interaction of remimazolam with remifentanil, sufentanil, and fentanyl are necessary for feasible and rational dosing strategies to be developed for various clinical settings and patient populations. The development of a TCI system for remimazolam targeting plasma and effect-site concentrations would further improve exact dosing. The availability of a TCI system could also help reduce recovery times, as the time to reach an estimated awakening concentration of remimazolam can continuously be calculated and displayed on a modern TCI smart pump system. The use of flumazenil to quickly antagonize any residual sedative or anesthetic effects of remimazolam should also be further investigated. Flumazenil will certainly result in shorter recovery times and may also reduce the incidence of postoperative cognitive deficit (POCD) or cognitive decline shortly after surgery. Shi et al. [27] showed that remimazolam had a protective effect in a rat model of cerebral ischemia/reperfusion. Other harmful or protective side effects of general anesthetics, such as recurrence rates of cancer at the site of resection or effects on metastatic disease burden, the incidence of postoperative nausea and vomiting, and the incidence and severity of POCD should be further investigated.
Conclusion
It has previously been shown that remimazolam is non-inferior to midazolam in terms of providing adequate sedation, and when co-administered with opioids, is non-inferior to propofol for induction and maintenance of general anesthesia [8,13]. The hemodynamic and respiratory stability of remimazolam compared to propofol is notable, but further well-designed randomized controlled clinical trials are needed to confirm and support these findings. Awakening times can be slightly prolonged directly compared to propofol; however, current knowledge suggests that the difference is only in the range of 1 to 5 min, which might not be clinically relevant in daily practice [13]. Additionally, a significant advantage of remimazolam is that prolonged recovery can be specifically treated with flumazenil. The risk of precipitation in the infusion line should be recognized, and Ringer’s solution should not be used together with remimazolam as the maintenance fluid. Remimazolam is the first new intravenous anesthetic agent that has been successfully introduced into clinical practice in more than four decades, primarily given its superior hemodynamic safety profile compared to propofol. Remimazolam is a soft drug with a pharmacological profile that should enable it to at least partially replace propofol as a standard intravenous anesthetic agent for general anesthesia in the future.
Acknowledgments
Jörg Fechner dedicates this review in memoriam to Professor Dr. med. Dr. rer. nat. Helmut Schwilden, who died in September of 2015. He would like to thank him for his personal support and for being an outstanding teacher and lecturer in anesthetic pharmacology and pharmacokinetic-pharmacodynamic modeling.
Footnotes
Funding
None.
Conflicts of Interest
Jörg Fechner worked as a medical adviser for PAION in Aachen, Germany and as a consultant for HANAPharm in Seoul, Korea. Seong-Hyop Kim has no competing interests to declare.
Author Contributions
Seong-Hyop Kim (Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing – original draft; Writing – review & editing)
Jörg Fechner (Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing – original draft; Writing – review & editing)
References
- 1.Shin TJ, Kim PJ, Choi B. How general anesthetics work: from the perspective of reorganized connections within the brain. Korean J Anesthesiol. 2022;75:124–38. doi: 10.4097/kja.22078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Son Y. Molecular mechanisms of general anesthesia. Korean J Anesthesiol. 2010;59:3–8. doi: 10.4097/kjae.2010.59.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Birgenheier NM, Stuart AR, Egan TD. Soft drugs in anesthesia: remifentanil as prototype to modern anesthetic drug development. Curr Opin Anaesthesiol. 2020;33:499–505. doi: 10.1097/ACO.0000000000000879. [DOI] [PubMed] [Google Scholar]
- 4.Wandel C, Böcker R, Böhrer H, Browne A, Rügheimer E, Martin E. Midazolam is metabolized by at least three different cytochrome P450 enzymes. Br J Anaesth. 1994;73:658–61. doi: 10.1093/bja/73.5.658. [DOI] [PubMed] [Google Scholar]
- 5.Kilpatrick GJ, McIntyre MS, Cox RF, Stafford JA, Pacofsky GJ, Lovell GG, et al. CNS 7056: a novel ultra-short-acting Benzodiazepine. Anesthesiology. 2007;107:60–6. doi: 10.1097/01.anes.0000267503.85085.c0. [DOI] [PubMed] [Google Scholar]
- 6.Schuttler J, Eisenried A, Lerch M, Fechner J, Jeleazcov C, Ihmsen H. Pharmacokinetics and pharmacodynamics of remimazolam (CNS 7056) after continuous infusion in healthy male volunteers: part I. Pharmacokinetics and clinical pharmacodynamics. Anesthesiology. 2020;132:636–51. doi: 10.1097/ALN.0000000000003103. [DOI] [PubMed] [Google Scholar]
- 7.Wiltshire HR, Kilpatrick GJ, Tilbrook GS, Borkett KM. A placebo- and midazolam-controlled phase I single ascending-dose study evaluating the safety, pharmacokinetics, and pharmacodynamics of remimazolam (CNS 7056): Part II. Population pharmacokinetic and pharmacodynamic modeling and simulation. Anesth Analg. 2012;115:284–96. doi: 10.1213/ANE.0b013e318241f68a. [DOI] [PubMed] [Google Scholar]
- 8.Antonik LJ, Goldwater DR, Kilpatrick GJ, Tilbrook GS, Borkett KM. A placebo- and midazolam-controlled phase I single ascending-dose study evaluating the safety, pharmacokinetics, and pharmacodynamics of remimazolam (CNS 7056): Part I. Safety, efficacy, and basic pharmacokinetics. Anesth Analg. 2012;115:274–83. doi: 10.1213/ANE.0b013e31823f0c28. [DOI] [PubMed] [Google Scholar]
- 9.Lu Z, Zhou N, Li Y, Yang L, Hao W. Up-down determination of the 90% effective dose (ED90) of remimazolam besylate for anesthesia induction. Ann Palliat Med. 2022;11:568–73. doi: 10.21037/apm-22-89. [DOI] [PubMed] [Google Scholar]
- 10.Gepts E, Camu F, Cockshott ID, Douglas EJ. Disposition of propofol administered as constant rate intravenous infusions in humans. Anesth Analg. 1987;66:1256–63. [PubMed] [Google Scholar]
- 11.Marsh B, White M, Morton N, Kenny GN. Pharmacokinetic model driven infusion of propofol in children. Br J Anaesth. 1991;67:41–8. doi: 10.1093/bja/67.1.41. [DOI] [PubMed] [Google Scholar]
- 12.Stöhr T, Colin PJ, Ossig J, Pesic M, Borkett K, Winkle P, et al. Pharmacokinetic properties of remimazolam in subjects with hepatic or renal impairment. Br J Anaesth. 2021;127:415–23. doi: 10.1016/j.bja.2021.05.027. [DOI] [PubMed] [Google Scholar]
- 13.Doi M, Morita K, Takeda J, Sakamoto A, Yamakage M, Suzuki T. Efficacy and safety of remimazolam versus propofol for general anesthesia: a multicenter, single-blind, randomized, parallel-group, phase IIb/III trial. J Anesth. 2020;34:543–53. doi: 10.1007/s00540-020-02788-6. [DOI] [PubMed] [Google Scholar]
- 14.Eisenried A, Schuttler J, Lerch M, Ihmsen H, Jeleazcov C. Pharmacokinetics and pharmacodynamics of remimazolam (CNS 7056) after continuous infusion in healthy male volunteers: Part II. Pharmacodynamics of electroencephalogram effects. Anesthesiology. 2020;132:652–66. doi: 10.1097/ALN.0000000000003102. [DOI] [PubMed] [Google Scholar]
- 15.Zhou J, Leonowens C, Ivaturi VD, Lohmer LL, Curd L, Ossig J, et al. Population pharmacokinetic/pharmacodynamic modeling for remimazolam in the induction and maintenance of general anesthesia in healthy subjects and in surgical subjects. J Clin Anesth. 2020;66:109899. doi: 10.1016/j.jclinane.2020.109899. [DOI] [PubMed] [Google Scholar]
- 16.Mourisse J, Lerou J, Struys M, Zwarts M, Booij L. Multi-level approach to anaesthetic effects produced by sevoflurane or propofol in humans: 1. BIS and blink reflex. Br J Anaesth. 2007;98:737–45. doi: 10.1093/bja/aem104. [DOI] [PubMed] [Google Scholar]
- 17.Urabe T, Miyoshi H, Narasaki S, Yanase Y, Uchida K, Noguchi S, et al. Characterization of intracellular calcium mobilization induced by remimazolam, a newly approved intravenous anesthetic. PLoS One. 2022;17:e0263395. doi: 10.1371/journal.pone.0263395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Salmasi V, Maheshwari K, Yang D, Mascha EJ, Singh A, Sessler DI, et al. Relationship between intraoperative hypotension, defined by either reduction from baseline or absolute thresholds, and acute kidney and myocardial injury after noncardiac surgery: a retrospective cohort analysis. Anesthesiology. 2017;126:47–65. doi: 10.1097/ALN.0000000000001432. [DOI] [PubMed] [Google Scholar]
- 19.Frölich MA, Arabshahi A, Katholi C, Prasain J, Barnes S. Hemodynamic characteristics of midazolam, propofol, and dexmedetomidine in healthy volunteers. J Clin Anesth. 2011;23:218–23. doi: 10.1016/j.jclinane.2010.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lim YS, Kang DH, Kim SH, Jang TH, Kim KH, Ryu SJ, et al. The cardiovascular effects of midazolam co-induction to propofol for induction in aged patients. Korean J Anesthesiol. 2012;62:536–42. doi: 10.4097/kjae.2012.62.6.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dai G, Pei L, Duan F, Liao M, Zhang Y, Zhu M, et al. Safety and efficacy of remimazolam compared with propofol in induction of general anesthesia. Minerva Anestesiol. 2021;87:1073–9. doi: 10.23736/S0375-9393.21.15517-8. [DOI] [PubMed] [Google Scholar]
- 22.Zhang X, Li S, Liu J. Efficacy and safety of remimazolam besylate versus propofol during hysteroscopy: single-centre randomized controlled trial. BMC Anesthesiol. 2021;21:156. doi: 10.1186/s12871-021-01373-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Furuta M, Ito H, Yamazaki M. Anaesthetic management using remimazolam in a patient with severe aortic stenosis: a case report. BMC Anesthesiol. 2021;21:202. doi: 10.1186/s12871-021-01422-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu T, Lai T, Chen J, Lu Y, He F, Chen Y, et al. Effect of remimazolam induction on hemodynamics in patients undergoing valve replacement surgery: a randomized, double-blind, controlled trial. Pharmacol Res Perspect. 2021;9:e00851. doi: 10.1002/prp2.851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sasaki H, Hoshijima H, Mizuta K. Ringer’s acetate solution-induced precipitation of remimazolam. Br J Anaesth. 2021;126:e87–9. doi: 10.1016/j.bja.2020.11.021. [DOI] [PubMed] [Google Scholar]
- 26.Yoshida K, Tanaka S, Watanabe K. A case of intravenous line occlusion when using Acetated Ringer’s solution and remimazolam. J Clin Anesth. 2021;70:110190. doi: 10.1016/j.jclinane.2021.110190. [DOI] [PubMed] [Google Scholar]
- 27.Shi M, Chen J, Liu T, Dai W, Zhou Z, Chen L, et al. Protective effects of remimazolam on cerebral ischemia/reperfusion injury in rats by inhibiting of NLRP3 inflammasome-dependent pyroptosis. Drug Des Devel Ther. 2022;16:413–23. doi: 10.2147/DDDT.S344240. [DOI] [PMC free article] [PubMed] [Google Scholar]


