Abstract
Arndt‐Gottron (S‐AG) syndrome or scleromyxedema is a scarce disease characterized by a generalized papular and sclerodermoid eruption and systemic manifestations that can lead to significant morbid‐mortality. Interesting, S‐AG can be associated with a paraprotein. We report an exceptional scleromyxedema case associated with a benign monoclonal gammapathy in an old woman.
Keywords: Arndt‐Gottron syndrome, monoclonal gammapathy, scleromyxedema, treatment

1. INTRODUCTION
Arndt‐Gottron (S‐AG) syndrome or scleromyxedema, also referred to the systemic form of Lichen myxedematosus, is a scarce disease of not well‐known etiology. 1 It is characterized by a generalized papular and sclerodermoid eruption due to mucin accumulation in the dermis, increased fibroblast proliferation, and fibrosis. 1 S‐AG, affecting mostly middle‐aged adults of 30–50 years, may be a life‐threatening syndrome due to systemic involvement of other organs. 2 Interestingly, S‐AG can be associated with a paraprotein. Herein, we report an exceptional scleromyxedema case associated with a benign monoclonal gammapathy in an old Tunisian woman.
2. OBSERVATION
A 85‐year‐old Tunisian woman, with a history of osteoporosis, was admitted in our department because of swelling reddened and indurated skin on the face, ears, neck, upper limbs, and back. These skin abnormalities started 2 months before and were progressively worsening. No improvement was noted under antihistamine therapy (Desloratadine 5 mg daily). On examination, we found a generalized eruption of 2–3 mm lichenoid papules. Lesions were most common on upper trunk, neck, and face with leonine facies (Figures 1, 2). These lichenoid lesions coalesced, leading to the induration of the underlying tissue. There is no Raynaud phenomenon or dysphagia. The remainder of the physical examination was normal; notably, no tumoral syndrome was found. Complementary tests revealed a microcytic hypochromic anemia to 11.1 g/dl due to iron deficiency and an inflammatory biologic syndrome. Calcemia, renal, and liver functions were all normal. Serum protein electrophoresis showed a narrow spike in the gamma region suggesting monoclonal gammapathy. Immunoelectrophoresis revealed monoclonal spikes IgG Lambda (λ) in both blood and urine samples. The bone marrow examination did not find any abnormalities especially plasma cells of aberrant morphology. Thus, the diagnosis of monoclonal gammapathy of the IgG λ was made. All other tests, including antinuclear antibodies, rheumatoid factors, anti‐DNA antibodies, anti‐neutrophil cytoplasmic antibodies, and cryoglobulin results, were normal or negative. Serology tests for hepatitis B and C virus and human immunodeficiency virus were negative. Upper and lower gastrointestinal endoscopy were normal. A computed axial tomography of the chest, abdomen, and pelvis did not furnish any significant data. A skin biopsy showed a thinned epidermis with irregularly arranged fibroblasts, fibrosis and diffuses mucin deposition within the upper and mid reticular dermis. A perivascular, lymphocytic, and plasmacytic infiltrate was also present. Hair follicles were atrophic. No signs of malignancy were detected. On that account, the diagnosis of Arndt‐Gottron scleromyxedema was retained. The patient was treated with double antihistamine therapy (Hydroxyzine hydrochloride 25 mg was associated with Desloratadine because of severe pruritus with sleep disturbance), prednisone (orally, 1 mg/Kg/day the first month and then gradually tapered), and 9 courses of polyvalent immunoglobulins (intravenously, 2 g/kg for 4 days monthly). Within the next three months, the lesions had almost completely disappeared and antihistamine therapy was stopped. During 9‐year follow‐up period, the patient remained stable. She did not present any systemic manifestation of (S‐AG).
FIGURE 1.

Reddened and indurated skin on the neck and on the upper trunk with eruption of lichenoid papules
FIGURE 2.
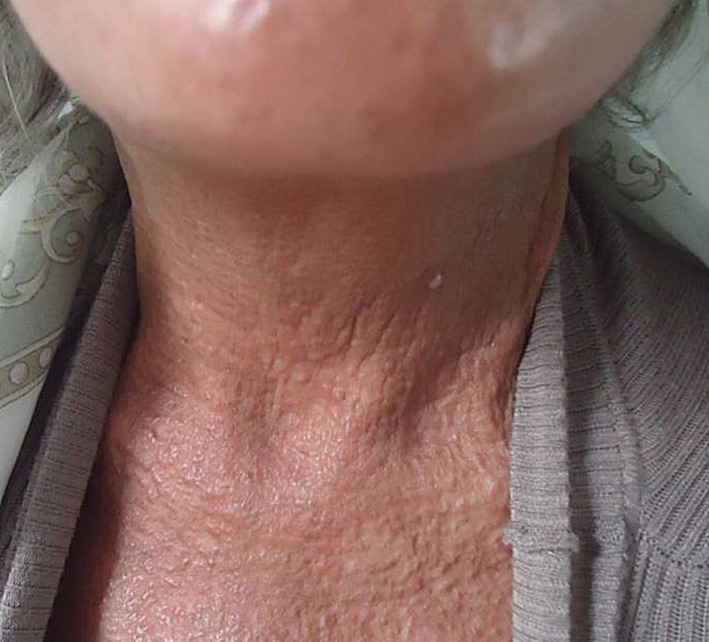
Reddened and indurated skin on the neck with eruption of lichenoid papules
3. DISCUSSION
Herein, we report an exceptional case of scleromyxedema in Tunisia. First of all, Arndt‐Gottron (S‐AG) syndrome is a very rare condition occurring usually in middle‐aged adults. 1 , 2 In our patient, the onset of S‐AG symptoms began at about 85 years old (elderly onset), which is not frequently described. Moreover, the etiopathogenesis of S‐AG still enigmatic to date and its optimal therapeutic strategy remains challenging. 1 , 2 Actually, as noted in our patient, there is hyperproliferation of dermal fibroblasts, with dermal mucin deposition and increased collagen deposition on histology. 3 Clinically, S‐AG is a condition revealed, like our patient's case, by diffused and symmetric lichenoid papules often arranged linearly and causing extensive thickening of the skin. These features usually involve the face, neck, distal forearms, and hands, and set the palms and mucous membranes apart. Even if extracutaneous manifestations of S‐AG were absent in our case, it is crucial to constantly seek them out as they can be life‐threatening in some cases by involving cardiovascular, gastrointestinal, pulmonary, and central nervous systems. Rheumatologic manifestations can on the one hand lead to significant disability and on the other hand be confused with other connective disease especially systemic scleroderma and dermatomyositis. Pathological features are the most important pillars of S‐AG diagnosis especially in these cases. Systemic manifestations may result from mucin deposition in various organs since mucin has been identified in adventitia around vessels in many organs, including the heart and lungs. 1 Interestingly, authors highlighted an association of S‐AG with paraproteinemia (up to 83% of cases) especially immunoglobulin G (IgG) lambda subtype, as described in our patient, with rare cases developing plasma cell dyscrasia or multiple myeloma (10%). 1 , 4 Therefore, we should seek for gammapathy in any patient presenting a S‐AG. To date, there is no completely satisfactory therapeutic approach to S‐AG. The rarity of this condition, and the lack of well‐designed clinical trials for it, explain mainly that therapeutic approach still not well codified. 4 , 5 , 6 , 7 , 8 , 9 In addition to antihistamine therapy, several agents have been tried: corticosteroids, melphalan, polyvalent immunoglobulins, and even autologous stem cell transplantation. 6 , 7 , 8 , 9 , 10 S‐AG has often a chronic progressive evolution with prognosis depending on among others systemic manifestations of this scarce condition.
4. CONCLUSION
Scleromyxedema is characterized by a generalized papular sclerodermoid eruption and systemic manifestations that can lead to significant morbid‐mortality. More work still needed to understand its etiopathogenesis and to establish a clear and well‐defined therapeutic approach. Immunoglobulins is a well‐tolerated treatment that can modify the disease course in some patients.
AUTHOR CONTRIBUTIONS
Asma Kefi and Fatima Jaziri involved in data collection and writing. Khaoula Ben Abdelghani involved in editing. Sami Turki involved in validation.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
ETHICAL APPROVAL
The work meets ethical and legal guidelines.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
ACKNOWLEDGMENTS
None.
Kefi A, Jaziri F, Ben Abdelghani K, Turki S. Early onset of scleromyxedema Arndt‐Gottron associated with a monoclonal gammapathy: Successful treatment with intravenous immunoglobulins. Clin Case Rep. 2022;10:e06122. doi: 10.1002/ccr3.6122
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- 1. Cokonis Georgakis CD, Falasca G, Georgakis A, Heymann WR. Scleromyxedema. Clin Dermatol. 2006;24(6):493‐497. [DOI] [PubMed] [Google Scholar]
- 2. Mehta V, Balachandran C, Rao R. Arndt Gottron scleromyxedema: successful response to treatment with steroid minipulse and methotrexate. Indian J Dermatol. 2009;54(2):193‐195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Saniee S, Davarnia G. Scleromyxedema without paraproteinemia: treatment with thalidomide and prednisolone. Case Rep Dermatol. 2016;8(3):327‐332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rongioletti F. Lichen myxedematosus (papular mucinosis): new concepts and perspectives for an old disease. Semin Cutan Med Surg. 2006;25(2):100‐104. [DOI] [PubMed] [Google Scholar]
- 5. Heymann WR. Scleromyxedema. J Am Acad Dermatol. 2007;57(5):890‐891. [DOI] [PubMed] [Google Scholar]
- 6. Harper RA, Rispler J. Lichen myxedematosus serum stimulates human skin fibroblast proliferation. Science. 1978;199(4328):545‐547. [DOI] [PubMed] [Google Scholar]
- 7. Guarenti I, Sebastiani V, Pinto G, de Souza PR, de Almeida H Jr. Successful treatment of scleromyxedema with oral thalidomide. Int J Dermatol. 2013;52(5):631‐632. [DOI] [PubMed] [Google Scholar]
- 8. Yeung CK, Loong F, Kwong YL. Scleromyxoedema due to a plasma cell neoplasm: rapid remission with bortezomib, thalidomide and dexamethasone. Br J Haematol. 2012;157(4):411. [DOI] [PubMed] [Google Scholar]
- 9. Bielsa I, Benvenutti F, Guinovart RM, Ferrándiz C. Escleromixedema y síndrome dermato‐neuro: buena respuesta al tratamiento con glucocorticoides e inmunoglobulinas endovenosas [good response of scleromyxedema and dermato‐neuro syndrome to treatment with intravenous immunoglobulins]. Actas Dermosifiliogr. 2012;103(4):317‐320. (in Spanish). [DOI] [PubMed] [Google Scholar]
- 10. Brunet‐Possenti F, Hermine O, Marinho E, Crickx B, Descamps V. Combination of intravenous immunoglobulins and lenalidomide in the treatment of scleromyxedema. J Am Acad Dermatol. 2013;69(2):319‐320. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


