Abstract
The aim of the study was to investigate the impact of the COVID‐19 lockdown on children's and adolescents' mental health in Greece during the lockdown of spring 2020. A cross‐sectional survey of 1232 Greek parents was conducted in spring 2020. 35.1% of parents reported that their children's psychological health was significantly affected. Parental unemployment, limited opportunity for tele‐work and deteriorating psychological health, increased family conflicts and children's pre‐existing physical health conditions were all significantly associated with mental health impact. Children and adolescents may experience adverse mental health effects due to the COVID‐19 pandemic.
Keywords: adolescence, children, COVID‐19, lockdown, mental health, pandemic
INTRODUCTION
Children and adolescents around the world are experiencing an unprecedented disruption of their everyday lives and daily routines due to the COVID‐19 pandemic and the subsequent lockdown measures, imposed to mitigate the risk of virus transmission. Concerns about multiple effects of the pandemic on the mental health and well‐being of the paediatric population have been raised (Araújo et al., 2020; Asmundson & Taylor, 2020; Brooks et al., 2020; Liu, Zhang, Wong, Hyun, & Hahm, 2020; Luo et al., 2020; Mactavish et al., 2020; Mazza et al., 2020; Rogers, Chesney, et al., 2020; Wang et al., 2020). Meta‐analytic data suggest that there was an overall increase in mental health symptoms in the general population, which was most pronounced during the early stages of the pandemic (March–April 2020) (Robinson et al., 2022). In the population of children and adolescents rising depression, anxiety and loneliness were reported in China, Canada, Turkey and the United States (Duan et al., 2020; Jiao et al., 2020; Kılınçel et al., 2020; Rogers, Chesney, et al., 2020; Xie et al., 2020; Zhou et al., 2020). Quarantined children and adolescents in India presented significantly higher levels of psychological distress when compared with their non‐quarantined peers (Saurabh & Ranjan, 2020). Similar results were reported by studies in Europe. In Italy and Spain, which were two countries that experienced very high numbers of cases and deaths during the first wave of the pandemic, conduct problems, irritability and loneliness in youth increased during the spring lockdown (Orgilés et al., 2020). A representative nationwide study in Germany showed that two‐thirds of children and adolescents were significantly affected by the pandemic (Ravens‐Sieberer et al., 2022). Studies of parents reporting on their children's psychological health presented similar findings. In a nationwide study in the United States, 14% of the parents reported worsening behavioural health of their children (Ellis et al., 2020). The CoRonavIruS health and Impact Survey (CRISIS) conducted in population samples of parents in the United States and the United Kingdom showed that pre‐existing mood states, perceived COVID risk and lifestyle changes were strongly associated with negative mood states of the offspring during the pandemic (Nikolaidis et al., 2021). The COSPACE study, which was designed during the early lockdown in the United Kingdom as an online survey of parental reports on their children's mental health and reported significant deteriorations in several mental health symptoms among preadolescent children (Waite et al., 2021).
In Greece, as in many other countries, regulatory lockdown measures have been introduced in the spring of 2020. All schools and universities closed for 8–10 weeks. All sport and leisure activities were suspended, while about 80% of private sector services providing psychological treatments for children and adolescents with mental health problems (reimbursed by the National Organization for the Provision of Health Services) closed (Giannopoulou & Tsobanoglou, 2020). During the first wave of the pandemic Greece managed to contain the pandemic and had a relatively low number of confirmed COVID‐19 cases and deaths compared to other countries (Johns Hopkins Center for Systems Science and Engineering, 2020). Data reporting on the mental health effects of the COVID‐19 pandemic on children and adolescents in Greece are limited. An online survey of 442 Greek senior high school students conducted in April 2020 revealed a rise in depression and anxiety levels in the time of home confinement (Giannopoulou et al., 2021). A qualitative study investigating the impact of the pandemic through individual interviews with nine psychiatric inpatient adolescents in a paediatric hospital in Athens reported anxiety about harm to self and beloved ones (Giannakopoulos et al., 2020).
The pandemic has placed enormous pressure on health systems around the globe. The strain was particularly alarming for the Greek health system, which has only recently started recovering from a recent deep fiscal crisis with profound socioeconomic implications. During the last decade, there were significant cuts in hospital budgets, understaffing, occasional shortages of medical supplies and limited access to care and preventive services (Kentikelenis et al., 2011). Child and adolescent mental health services and supportive policies underwent major budget changes. Public funding cuts led to some services not being fully operational, many non‐profit child and adolescent mental health community centres, psychosocial rehabilitation units and highly specialized establishments were suspended, while the number of abused or neglected children admitted for child protection to paediatric hospitals increased dramatically (Kolaitis & Giannakopoulos, 2015).
Socioeconomic inequalities have been shown to significantly affect youth mental health outcomes. Children and adolescents with lower socioeconomic status are at higher risk of developing mental health problems, with the inequalities being stronger for family income than type of parental occupation (Reiss, 2013). Parental job loss and unemployment may stress families and many studies report deteriorating children's mental health during periods of declining family income (Milligan & Stabile, 2011) or parents' sudden job loss (Johnson et al., 2010). While unemployed parents tend to spend more time with their offspring, this may have a negative impact on children, since unemployment correlates with parental stress and mental health problems, which are, in turn, associated with child stress (Lupien et al., 2000). The association between parental and youth mental health has been established by numerous studies showing that parents' mental health problems negatively affect the psychological health of their children (Ramchandani & Stein, 2003; Vostanis et al., 2006).
The aim of the present study was to investigate the impact of the COVID‐19 pandemic and the measure of lockdown in the spring 2020 on the mental health of children and adolescents in Greece. More specifically, the study investigated the type of symptomatology presented by a sample of children and adolescents in Greece during the first wave of the pandemic in spring 2020, as reported by their parents, as well as its association with socioeconomic factors. During the early phase of the pandemic many families experienced unexpected job loss and income insecurity, since many facilities and services closed suddenly in early March 2020. Thus, a further aim of our study was to explore possible socioeconomic associations of children's mental health as reported by their parents.
METHODS
The study was a cross‐sectional online survey of a convenience sample of Greek parents of children aged <18 years. Despite the serious limitations associated with this type of sampling, we chose to use it in order to obtain quickly data from a larger number of parents during the first, acute phase of the pandemic. A questionnaire was designed and uploaded in an online survey tool (www.surveymonkey.com). Initially, participants were presented with an informed consent, consisting of a brief presentation of the research group and the purpose of the study. They were asked to read and provide their consent before proceeding to the questionnaire. If they agreed, they were forwarded to the questions of the survey. Our survey took place between 21 April and 30 May 2020. The study and the survey instrument were advertised in social media, while a press release was distributed to journalists who presented the study inviting participants in internet news‐media. The study was approved by the ethics committee of the University of West Attica in Athens, Greece. Survey participation was anonymous and participants were informed through the consent form that they could exit the questionnaire at any time. The IP addresses were recorded by the online system in order to prevent double entries.
The questionnaire consisted of three sections. The first section included general sociodemographic variables for parents and their offspring (parental sex, age, nationality, geographical area of current address, type of residential area, highest educational level attained and employment status; child's sex and age), as well as information regarding family and/or household characteristics (family annual income, number of bedrooms, number of household members). Information relevant to the pandemic, such as parental tele‐working and employment as a healthcare worker during the lockdown, was also sought. The second section included questions about conditions of the everyday life of the family during the lockdown period. We obtained information about conflicts within the family, the level of contact with friends and relatives and self‐perceived psychological health of parents. The third section included information about the psychological impact of the pandemic on children. We developed the questionnaire for the needs of the current study based on ‘The CoRonavIruS Health Impact Survey’ (CRISIS) (Nikolaidis et al., 2021), which used a questionnaire covering key domains relevant to mental distress and resilience during the pandemic. Specifically, we asked the following question: ‘Do you think that your child's psychological health was affected by the lockdown measures’? The possible answers were 'no', 'yes', ‘I don't know/ I am not sure’. We further asked parents to rate their child's psychological health now and before the lockdown on a 5‐item Likert scale ranging from ‘bad’ to ‘excellent’. We also included Likert‐type questions about current psychological symptoms (sleep, stress, fear of being infected with the coronavirus, negative thoughts, depressive mood). Additionally, we asked about changes in physical activity and nutrition of the child during the lockdown. The specific questions asked were: ‘Do you think that your child's physical activity level/ nutrition changed during the pandemic?’ Possible answers ranged on a 4‐item Likert scale from 'no' to 'a lot'. Finally, we asked about the parent's rating about the most significant difficulties experienced by the child during the lockdown. Possible answers were as follows: 'stress', 'social isolation', ‘increase in screen time’, ‘absence from educational activities’, ‘decrease in physical activity’, ‘change in sleep time’, ‘increased calorie intake’.
The questionnaire is not a validated measure, but a self‐constructed instrument developed for the needs of the present study. To improve the design of the data collection instrument and to avoid potential comprehension issues experienced by the study participants, eight parents, who did not participate in the study, were recruited to pretest the questionnaire using the method of cognitive interviewing (Collins, 2003).
Statistical analysis
The outcome of interest in our study was the impact of the pandemic on the psychological health of children and adolescents as reported by their parents. The impact was defined as present if answering 'yes' to the question: ‘Do you think that your child's psychological health was affected by the lockdown measures’? Only 12 parents (0.97%) in our sample reported that the current psychological health of their children was 'good'/'very good' or 'excellent' and the psychological health before the lockdown 'poor'/'fair'. Thus, it could be assumed that the direction of the overall impact of the lockdown was negative.
Results were reported for the whole sample, with categorical variables presented as number (%) and continuous variables as mean (SD). Chi‐square tests were used for categorical variables in order to compare characteristics between those with and without an impact of the pandemic on children's psychological health. Logistic regression analysis was performed to examine factors associated with an impact of the pandemic on children's psychological health. All analyses were performed using SPSS v.22.
RESULTS
The sample of our study consisted of 1232 parents who completed the online questionnaire. Table 1 shows the basic sociodemographic and socioeconomic characteristics of participants. Most of them were of Greek nationality (98.2%), middle‐aged women (79.6%), highly educated (90.0%) and residing in big cities (81.3%). Approximately half of the unemployed parents (7.0% out of a total unemployment rate of 15.0%) reported that they were employed before the pandemic, but lost their jobs during the lockdown. The majority of participants reported a family annual income of ≥10 000 euros, while more than half of the households (55.9%) had more than two bedrooms in their home. Most of the participants were parents of children younger than 13 years (70.4%), with almost 1 out of 5 (19.5%) reporting their current psychological health as fair or bad. A positive history of mental or developmental disorder was reported for 5.1% of the children, while a history of physical health condition was reported by 5.5%.
TABLE 1.
Basic sociodemographic and socioeconomic characteristics in a sample of 1232 parents in Greece
| Total (N = 1232) | ||
|---|---|---|
| N or mean | % or SD | |
| Parents' age | 43.8 | 7.5 |
| Parents' sex | ||
| Male | 243 | 19.8 |
| Female | 979 | 79.6 |
| Do not want to declare | 8 | 0.7 |
| Parents' educational level | ||
| Primary school/ Secondary school/ Vocational school/ Senior high school | 118 | 9.6 |
| Technical college/ University/ Postgraduate degree | 1109 | 90 |
| Residential area | ||
| Urban | 1001 | 81.3 |
| Non‐urban | 220 | 17.9 |
| Greek citizenship | ||
| Yes | 1210 | 98.2 |
| No | 12 | 1 |
| Parents' employment status | ||
| Public sector employee | 382 | 31 |
| Private sector employee | 339 | 27.5 |
| Self‐employed | 300 | 24.4 |
| Student/Pensioner | 24 | 1.9 |
| Unemployed | 98 | 8 |
| Employed prior to the pandemic, but currently unemployed | 86 | 7 |
| Family annual income | ||
| 0–9999 euro | 93 | 7.5 |
| ≥10 000 euro | 1115 | 90.5 |
| Parent's job with no possibility for tele‐work | 552 | 42.4 |
| Number of people in the household | ||
| ≤4 | 1053 | 85.5 |
| >4 | 178 | 14.4 |
| Number of bed‐rooms in the household | ||
| ≤2 | 553 | .43.6 |
| >2 | 689 | 55.9 |
| Parent's self‐reported psychological health | ||
| Excellent/ Very good/ Good | 991 | 80.4 |
| Fair/ Bad | 240 | 19.5 |
| Increase of family conflicts | ||
| Yes | 290 | 23.5 |
| No | 831 | 67.5 |
| Do not know/ Not sure | 111 | 9 |
| Gender of the child | ||
| Male | 676 | 50 |
| Female | 593 | 48.1 |
| Age of the child | ||
| <13 years | 867 | 70.4 |
| ≥13 years | 365 | 29.6 |
| Positive history of mental or developmental disorders of the child | 63 | 5.1 |
| Positive history of physical disorders of the child | 68 | 5.5 |
Figure 1 shows children's difficulties associated with the lockdown as reported by the parent. The parents in our sample reported that social isolation and the increase in screen time were the most significant difficulties experienced by the child or adolescent during the lockdown, followed by the decrease in physical activity and absence from educational activities.
FIGURE 1.
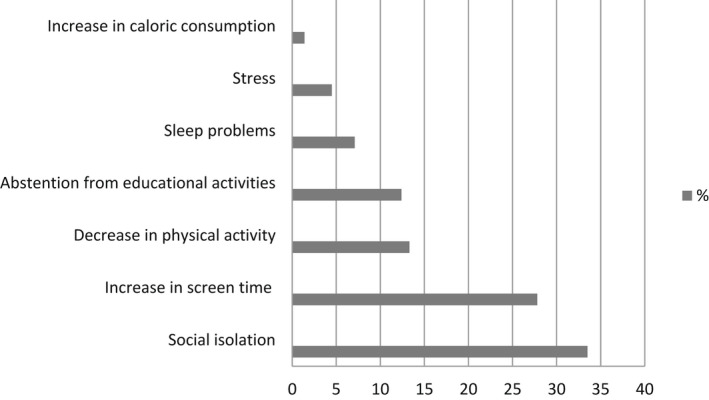
Difficulties experienced by children and adolescents during the lockdown as reported by the parent in a sample of 1232 parents in Greece.
Approximately one‐third of participants reported that the psychological health of their child was affected by the lockdown. Table 2 presents the characteristics of these cases compared to those with no impact of the lockdown on child's psychological health. Statistically significant differences between the two groups were observed in the employment status of the parent, the opportunity for the parent to work from home, the increase in family conflicts, parent's psychological condition and the positive history of mental or developmental and physical health condition of the child.
TABLE 2.
Characteristics of children without and with a negative impact of the pandemic on their psychological health as reported by the parent in a sample of 1232 parents in Greece
| Negative impact on child's psychological health | |||||
|---|---|---|---|---|---|
| Yes | No/Not sure | p value | |||
| n | % | n | % | ||
| Total | 432 | 35.1 | 800 | 64.9 | |
| Parent's educational level | |||||
| Senior high school or less | 36 | 8.3 | 82 | 10.3 | .269 |
| Technical college or University or Postgraduate degree | 395 | 91.4 | 714 | 89.3 | |
| Residential area | |||||
| Urban | 344 | 79.6 | 657 | 82.1 | .184 |
| Non‐urban | 86 | 19.9 | 134 | 16.8 | |
| Greek citizenship | |||||
| Yes | 425 | 98.4 | 785 | 98.1 | .182 |
| No | 2 | 0.5 | 10 | 1.3 | |
| Parent's employment status | |||||
| Public sector employee | 120 | 27.8 | 262 | 32.8 | .002 |
| Private sector employee | 117 | 27.1 | 222 | 27.8 | |
| Self‐employed | 100 | 23.1 | 200 | 25 | |
| Student/ Pensioner | 5 | 1.2 | 19 | 2.4 | |
| Unemployed | 44 | 10.2 | 54 | 6.8 | |
| Employed prior to the pandemic, but currently unemployed | 44 | 10.2 | 42 | 5.3 | |
| Family annual income | |||||
| 0–9999 euro | 40 | 9.3 | 53 | 6.6 | .093 |
| ≥10 000 euro | 383 | 88.7 | 732 | 91.5 | |
| Parent's job with no possibility for tele‐work | 206 | 47.7 | 316 | 39.5 | .005 |
| Number of people in the household | |||||
| ≤4 | 372 | 86.1 | 681 | 85.1 | .675 |
| >4 | 60 | 13.9 | 118 | 14.8 | |
| Number of bed‐rooms in the household | |||||
| ≤2 | 196 | 45.4 | 337 | 42.1 | .308 |
| >2 | 234 | 54.2 | 455 | 56.9 | |
| Parent's self‐reported psychological health | |||||
| Excellent/ Very good/ Good | 295 | 68.3 | 696 | 87 | <.001 |
| Fair/ Bad | 136 | 31.5 | 104 | 13 | |
| Increase of family conflicts | |||||
| Yes | 171 | 39.6 | 119 | 14.9 | <.001 |
| No | 225 | 52.1 | 606 | 75.8 | |
| Do not know/ Not sure | 36 | 8.3 | 75 | 9.4 | |
| Gender of the child | |||||
| Male | 213 | 49.3 | 403 | 50.4 | .856 |
| Female | 208 | 48.1 | 385 | 48.1 | |
| Age of the child | |||||
| <13 years | 318 | 73.6 | 549 | 68.6 | .067 |
| ≥13 years | 114 | 26.4 | 251 | 31.4 | |
| Positive history of mental or developmental disorders of the child | 30 | 6.9 | 33 | 4.1 | .032 |
| Positive history of physical disorders of the child | 40 | 9.3 | 28 | 3.5 | <.001 |
Bold indicates statistical significant value (p < .05).
Table 3 presents the results of logistic regression analysis. Unemployment of the parent, both previously existing and having occurred during the lockdown, parent having no opportunity to work from home, increase in family conflicts, impaired psychological condition of the parent during the lockdown and child's previous history of physical health condition were all significantly associated with a higher risk of a negative impact of the lockdown on the child's psychological health.
TABLE 3.
Logistic regression analysis of factors associated with an impact of the pandemic on children's psychological health in a sample of 1232 parents in Greece
| Negative impact on child's psychological health | |||
|---|---|---|---|
| OR | 95% CI | p value | |
| Parent's educational level | |||
| Primary/Secondary/Vocational/Senior high school | 1 | ||
| Technical college/University/Postgraduate degree | 1.58 | 0.98–2.55 | .062 |
| Residential area | |||
| Non‐urban | 1 | ||
| Urban | 0.85 | 0.60–1.19 | .342 |
| Greek citizenship | |||
| No | 1 | ||
| Yes | 1.22 | 0.25–6.00 | .811 |
| Parent's employment status | |||
| Public sector employee | 1 | ||
| Private sector employee | 1.32 | 0.93–1.88 | .118 |
| Businessman | 1.15 | 0.81–1.65 | .437 |
| Student/Pensioner | 0.66 | 0.22–1.97 | .461 |
| Unemployed | 1.87 | 1.09–3.21 | .023 |
| Employed before the lockdown but currently unemployed | 2.3 | 1.35–3.93 | .002 |
| Family annual income | |||
| ≥10 000 euro | 1 | ||
| 0–9999 euro | 1.02 | 0.60–1.76 | .935 |
| Parent's job with no opportunity for working from home (tele‐work) | |||
| No | |||
| Yes | 1.38 | 1.05–1.80 | .019 |
| Number of people in the household | |||
| ≤3 | 1 | ||
| >3 | 1.19 | 0.89–1.60 | .23 |
| Number of bedrooms in the household | |||
| ≤2 | 1 | ||
| >2 | 0.87 | 0.65–1.15 | 0.331 |
| Parent's self‐assessed psychological health | |||
| Excellent/Very good/Good | 1 | ||
| Fair/Bad | 2.17 | 1.57–2.99 | <.001 |
| Increase in family conflicts during the lock down | |||
| Do not know/Not sure | 1 | ||
| Yes | 3.28 | 1.98–5.44 | <.001 |
| No | 0.94 | 0.58–1.50 | .783 |
| Child's gender | |||
| Female | 1 | ||
| Male | 0.93 | 0.71–1.22 | .6 |
| Child's age | |||
| <13 years | 1 | ||
| ≥13 years | 1.01 | 0.75–1.36 | .958 |
| Positive history of mental or developmental disorder of the child | |||
| No | 1 | ||
| Yes | 1.26 | 0.70–2.26 | .444 |
| Positive history of physical health condition of the child | |||
| No | 1 | ||
| Yes | 2.12 | 1.21–3.72 | .009 |
Abbreviations: CI, Confidence interval; OR, Odds ratio.
Bold indicates statistical significant value (p < .05).
DISCUSSION
Approximately one‐third of the participants in a sample of 1232 parents in Greece reported that the psychological health of their offspring was considerably affected during the lockdown in the spring of 2020. The most significant difficulty experienced by the children and adolescents during the lockdown was social isolation. The unemployment of the parent and their deprivation from opportunities for tele‐work, increased family conflicts and a deteriorating psychological health of the parent was significantly associated with the impact of the lockdown on the mental health of their offspring. Previous history of physical health condition of the child was statistically significantly associated with a higher risk of the measures having an impact on the psychological health of the child. There was a trend for a similar association with previous history of a mental or developmental disorder of the child, which however did not reach the level of statistical significance.
One of the major concerns of the parents in our sample during the lockdown was the social isolation of their children. In many countries around the world, children and adolescents have experienced an unexpected and prolonged period of physical isolation from their friends, peers, teachers, extended family and various community networks. Literature shows that isolation associated with quarantine measures has negative psychological effects in adults, including confusion, anger and post‐traumatic distress (Brooks et al., 2020). Loneliness might be a major issue associated with social isolation. Loneliness is conceptualized as the negative emotion of a discrepancy between the social contact actually experienced by a person and the desire for it (Perlman & Peplau, 1981). Social isolation is not necessarily followed by loneliness. However, early evidence shows that more than one‐third of adolescents report high levels of loneliness (VandePol, 2020), while a rapid systematic review of previous literature reports that social isolation and loneliness increases the risk of depression and possibly anxiety (Loades et al., 2020).
Further concerns of the parents in our sample were the limited physical activity and the increased screen time of children and adolescents during the lockdown. A study conducted in 2426 children and adolescents in Shanghai, China confirmed a substantial decrease in physical activity and a significant increase in screen time during the COVID‐19 pandemic (Xiang et al., 2020). The vicious circle between reduced physical activity and increased sedentary behaviour was one of the major concerns early in the crisis that lead in an urgent call for systematic efforts to mitigate the effects of home confinement of children (Guan et al., 2020; Wang et al., 2020).
Our study presents some interesting findings suggesting socioeconomic inequality in the distribution of the negative effects of the COVID‐19 crisis in the population of children and adolescents. The unemployment of the parent that was either present prior or occurred during the course of the pandemic was significantly associated with a negative impact on children's psychological health. Our findings are in line with previous studies about significant determinants of youth psychological health. Socioeconomic inequalities are among the most common findings in literature investigating the mental health of children and adolescents (Elgar et al., 2015; Magklara et al., 2010). There is evidence that higher income inequality relates not only to more psychological and physical symptoms, but also to fewer days of physical activity and higher Body Mass Index, which is in accordance with the higher concern of reduced physical activity reported in our study (Elgar et al., 2015). Parental unemployment is one of the most significant socioeconomic indicators associated with the psychological health of children and adolescents. In addition to that, family income has been shown to be a stronger socioeconomic indicator than the type of parental occupation (Reiss, 2013). Financial stress is considered to be the most important consequence of unemployment, with regard to the health of the unemployed individual and the family members (Magklara et al., 2010; Whelan, 1992). The significance of the above‐mentioned associations is of particular interest for Greece, since it is a country that was severely affected by a major fiscal crisis during the last decade (Kentikelenis et al., 2011). According to a report conducted on behalf of UNICEF 3 years ago, almost one in two children in Greece (45%) lived in material deprivation and 22% in severe material deprivation (Papatheodorou & Papathanasiou, 2017).
Increased family conflicts and poorer psychological health of the parent have been also associated with higher risk of a negative impact of the crisis on the psychological health of children and adolescents in our study. Family conflict, in the form of either inter‐adult or parent–child conflict, has been linked in various studies to children's behavioural, emotional, social, academic and health problems and identified as important predictor of children's maladjustment (Cummings & Schatz, 2012). Regarding the impact of parental psychological health, most existing findings derive from studies conducted in clinical populations, linking parental psychopathology to a wide range of negative outcomes for their offspring (Zahn‐Waxler et al., 2002). Population studies have shown similar results reporting positive associations between parental psychological distress and psychosocial maladjustment of their offspring (Roustit et al., 2010; Vostanis et al., 2006). Similarly, a UK online study that utilized parental reports about the pandemic impact on their children's mental health showed that children that experienced higher emotional distress during the pandemic were more likely to have a parent with worse psychological health (Raw et al., 2021).
Finally, our study showed a positive association between a history of physical health condition and a negative impact of the lockdown on the psychological health of the child. Similar findings have been shown by a recent meta‐analysis, which reported that change in mental health symptoms tended to be larger among participants with a pre‐existing physical health condition compared to the general population (Robinson et al., 2022). Chronic physical illness is thought to be a risk factor for psychological problems. The presence of physical symptoms and the need for disease management strategies are likely to interfere with many aspects of the child's everyday life, may cause frustration and detrimentally affect the child's self‐esteem. Additionally, chronic illness may lead to problematic parental behaviours, ranging from overprotection to rejection, which may further impair the child's psychological health (Bennett, 1994). There was evidence of a trend for a similar association with a history of previous psychiatric or developmental disorder, which has not reached, however the level of statistical significance in our sample. The finding is in accordance with other findings showing that change in mental health symptoms was non‐significant in samples with pre‐existing mental health conditions (Robinson et al., 2022). On the other hand, multiple studies have pointed out a possibly higher vulnerability of individuals with pre‐existing mental illness that experience additional adverse events (Fiorillo & Gorwood, 2020; Nikolaidis et al., 2021).
Limitations
An important limitation of our study is the fact that we used an online, convenience sample, which is not representative of the population studied. It has been argued that non‐representative samples attract volunteers who are already well engaged, interested in the topic, who can access the internet, while those excluded, for instance individuals with severe mental illness, are often those most in need (Pierce et al., 2020). Therefore, our findings cannot be interpreted as an overall prevalence of psychopathology among children in the general population. However, our results indicate that individuals with various types of vulnerabilities are at higher risk for negative outcomes of the current crisis. Given the argument that vulnerable populations may have been excluded from our surveys, it could be expected that the real impact of COVID‐19 pandemic could be of greater magnitude for specific population sub‐groups.
Another limitation of our study is the fact that we used only parental reports. However, we collected our data during the lockdown and there were only limited opportunities to use more subjective measures of children's characteristics and difficulties. Additionally, the online nature of the design of our study presented significant difficulties for the use of children as informants, especially for younger children that were the majority in our sample.
In addition, the design of our study was cross‐sectional with no pre‐pandemic data, which means that causal inferences are not possible. A further limitation of our study is the lack of validated questionnaires as measures of children's mental health.
CONCLUSIONS
Our findings indicate that vulnerable individuals are at higher risk for experiencing negative outcomes during the course, and possibly also at the aftermath, of the COVID‐19 pandemic. Both family risk factors, such as parental unemployment, psychological distress or family conflict, and individual risk factors, such as pre‐existing physical health conditions, contribute substantially to the vulnerability of children and adolescents to the adverse effects of the new coronavirus outbreak and its containment measures. Well‐designed public health policies should focus on specific population groups with the aim of ameliorating risks, when possible, and enhancing resilience.
AUTHOR CONTRIBUTIONS
KM: Methodology, Writing ‐ Original draft, Formal analysis, Resources. HL: Conceptualization, Methodology, Review & Editing, Supervision, Resources. AB: Conceptualization, Methodology, Resources, Review & Editing. KP: Conceptualization, Methodology, Writing ‐ Review & Editing, Resources, Supervision. KF: Conceptualization, Methodology, Writing ‐ Original Draft, Formal analysis, Resources.
FUNDING INFORMATION
This research received no specific grant from any funding agency, commercial or not for‐profit sectors.
CONFLICTS OF INTEREST
The authors report no conflict of interest relevant to this study.
ETHICS STATEMENT
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committee on human experimentation with the Helsinki Declaration of 1975, as revised in 2008. The study protocol was approved by the ethics committee of the University of West Attica, Athens, Greece.
CONSENT STATEMENT
Participants were presented with an informed consent, consisting of a brief presentation of the research group and the purpose of the study. They were asked to read and provide their consent before proceeding to the questionnaire.
PERMISSION TO REPRODUCE MATERIAL FROM OTHER SOURCES
The authors declare that they have not reproduced any original material from other sources.
ACKNOWLEDGEMENTS
The authors would like to thank all parents and carers who participated in the survey.
Biographies
Konstantina Magklara is a child and adolescent psychiatrist at a university child and adolescent mental health centre in Athens, Greece.
Helen Lazaratou is a Full Professor of Child and Adolescent Psychiatry at the National and Kapodistrian University of Athens.
Anastasia Barbouni is a paediatrician and Professor of Public Health, Hygiene and Disease Prevention at the Department of Public and Community Health of the University of West Attica.
Konstantinos Poulas is an Associate Professor of Biochemistry at the Department of Pharmacy, University of Patras and the Director of BioHealth Hub, Science Park, Patras.
Konstantinos Farsalinos is a senior researcher at the University of Patras, the School of Public Health of the University of West Attica, as well as the King Abdulaziz University.
Magklara, K. , Lazaratou, H. , Barbouni, A. , Poulas, K. & Farsalinos, K. (2022). The impact of COVID‐19 lockdown on children's and adolescents' mental health in Greece. Children & Society, 00, 1–16. 10.1111/chso.12605
Konstantina Magklara, Helen Lazaratou, Anastasia Barbouni, Konstantinos Poulas and Konstantinos Farsalinos are contributed to the manuscript.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Araújo, F. , de Lima, L. , Cidade, P. , Nobre, C. B. , & Neto, M. (2020). Impact of Sars‐Cov‐2 and its reverberation in global higher education and mental health. Psychiatry Research, 288(112), 977. 10.1016/j.psychres.2020.112977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asmundson, G. J. G. , & Taylor, S. (2020). How health anxiety influences responses to viral outbreaks like COVID‐19: What all decision‐makers, health authorities, and health care professionals need to know. Journal of Anxiety Disorders, 71, 102211. 10.1016/j.janxdis.2020.102211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett, D. S. (1994). Depression among children with chronic medical problems: A meta‐analysis. Journal of Pediatric Psychology, 19(2), 149–169. 10.1093/jpepsy/19.2.149 [DOI] [PubMed] [Google Scholar]
- Brooks, S. K. , Webster, R. K. , Smith, L. E. , Woodland, L. , Wessely, S. , Greenberg, N. , & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet (London, England), 395(10227), 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins, D. (2003). Pretesting survey instruments: An overview of cognitive methods. Quality of Life Research, 12(3), 229–238. 10.1023/a:1023254226592 [DOI] [PubMed] [Google Scholar]
- Cummings, E. M. , & Schatz, J. N. (2012). Family conflict, emotional security, and child development: Translating research findings into a prevention program for community families. Clinical Child and Family Psychology Review, 15(1), 14–27. 10.1007/s10567-012-0112-0 [DOI] [PubMed] [Google Scholar]
- Duan, L. , Shao, X. , Wang, Y. , Huang, Y. , Miao, J. , Yang, X. , & Zhu, G. (2020). An investigation of mental health status of children and adolescents in china during the outbreak of COVID‐19. Journal of Affective Disorders, 275, 112–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elgar, F. J. , Pförtner, T. K. , Moor, I. , De Clercq, B. , Stevens, G. W. , & Currie, C. (2015). Socioeconomic inequalities in adolescent health 2002–2010: A time‐series analysis of 34 countries participating in the health behaviour in school‐aged children study. Lancet (London, England), 385(9982), 2088–2095. 10.1016/S0140-6736(14)61460-4 [DOI] [PubMed] [Google Scholar]
- Ellis, W. E. , Dumas, T. M. , & Forbes, L. M. (2020). Physically isolated but socially connected: Psychological adjustment and stress among adolescents during the initial COVID‐19 crisis. Canadian Journal of Behavioural Science, 52(3), 177. [Google Scholar]
- Fiorillo, A. , & Gorwood, P. (2020). The consequences of the COVID‐19 pandemic on mental health and implications for clinical practice. European Psychiatry: The Journal of the Association of European Psychiatrists, 63(1), e32. 10.1192/j.eurpsy.2020.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giannakopoulos, G. , Mylona, S. , Zisimopoulou, A. , Belivanaki, M. , Charitaki, S. , & Kolaitis, G. (2020). Perceptions, emotional reactions and needs of adolescent psychiatric inpatients during the COVID‐19 pandemic: A qualitative analysis of in‐depth interviews. BMC Psychiatry, 21(1), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giannopoulou, I. , Efstathiou, V. , Triantafyllou, G. , Korkoliakou, P. , & Douzenis, A. (2021). Adding stress to the stressed: Senior high school students' mental health amidst the COVID‐19 nationwide lockdown in Greece. Psychiatry Research, 295(113), 560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giannopoulou, I. , & Tsobanoglou, G. O. (2020). COVID‐19 pandemic: Challenges and opportunities for the Greek health care system. Irish Journal of Psychological Medicine, 37(3), 226–230. 10.1017/ipm.2020.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan, H. , Okely, A. D. , Aguilar‐Farias, N. , Del Pozo Cruz, B. , Draper, C. E. , El Hamdouchi, A. , Florindo, A. A. , Jáuregui, A. , Katzmarzyk, P. T. , Kontsevaya, A. , Löf, M. , Park, W. , Reilly, J. J. , Sharma, D. , Tremblay, M. S. , & Veldman, S. (2020). Promoting healthy movement behaviours among children during the COVID‐19 pandemic. The Lancet. Child & Adolescent Health, 4(6), 416–418. 10.1016/S2352-4642(20)30131-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiao, W. Y. , Wang, L. N. , Liu, J. , Fang, S. F. , Jiao, F. Y. , Pettoello‐Mantovani, M. , & Somekh, E. (2020). Behavioral and emotional disorders in children during the COVID‐19 epidemic. The Journal of Pediatrics, 221, 264–266.e1. 10.1016/j.jpeds.2020.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- John Hopkins Center for Systems Science and Engineering . (2020) https://systems.jhu.edu/research/public‐health/ncov/. Date accessed: 28 September 2020.
- Johnson, R. C. , Kalil, A. , & Dunifon, R. E. (2010). Mothers' work and children's lives: Low‐income families after welfare reform. WE Upjohn Institute. [Google Scholar]
- Kentikelenis, A. , Karanikolos, M. , Papanicolas, I. , Basu, S. , McKee, M. , & Stuckler, D. (2011). Health effects of financial crisis: Omens of a Greek tragedy. Lancet (London, England), 378(9801), 1457–1458. 10.1016/S0140-6736(11)61556-0 [DOI] [PubMed] [Google Scholar]
- Kılınçel, Ş. , Kılınçel, O. , Muratdağı, G. , Aydın, A. , & Usta, M. B. (2020). Factors affecting the anxiety levels of adolescents in home‐quarantine during COVID‐19 pandemic in Turkey. Asia‐Pacific Psychiatry, 13(2), e12406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolaitis, G. , & Giannakopoulos, G. (2015). Greek financial crisis and child mental health. Lancet (London, England), 386(9991), 335. 10.1016/S0140-6736(15)61402-7 [DOI] [PubMed] [Google Scholar]
- Liu, C. H. , Zhang, E. , Wong, G. , Hyun, S. , & Hahm, H. C. (2020). Factors associated with depression, anxiety, and PTSD symptomatology during the COVID‐19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Research, 290, 113172. 10.1016/j.psychres.2020.113172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loades, M. E. , Chatburn, E. , Higson‐Sweeney, N. , Reynolds, S. , Shafran, R. , Brigden, A. , Linney, C. , McManus, M. N. , Borwick, C. , & Crawley, E. (2020). Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID‐19. Journal of the American Academy of Child & Adolescent Psychiatry, 59(11), 1218–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo, M. , Guo, L. , Yu, M. , Jiang, W. , & Wang, H. (2020). The psychological and mental impact of coronavirus disease 2019 (COVID‐19) on medical staff and general public ‐ a systematic review and meta‐analysis. Psychiatry Research, 291(113), 190. 10.1016/j.psychres.2020.113190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lupien, S. J. , King, S. , Meaney, M. J. , & McEwen, B. S. (2000). Child's stress hormone levels correlate with mother's socioeconomic status and depressive state. Biological Psychiatry, 48(10), 976–980. [DOI] [PubMed] [Google Scholar]
- Mactavish, A. , Mastronardi, C. , Menna, R. , Babb, K. A. , Battaglia, M. , Amstadter, A. , & Rappaport, L. M. (2020). The acute impact of the COVID‐19 pandemic on Children's mental health in southwestern Ontario. 10.31234/osf.io/5cwb4. [DOI] [PMC free article] [PubMed]
- Magklara, K. , Skapinakis, P. , Niakas, D. , Bellos, S. , Zissi, A. , Stylianidis, S. , & Mavreas, V. (2010). Socioeconomic inequalities in general and psychological health among adolescents: A cross‐sectional study in senior high schools in Greece. International Journal for Equity in Health, 9, 3. 10.1186/1475-9276-9-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazza, M. , Marano, G. , Lai, C. , Janiri, L. , & Sani, G. (2020). Danger in danger: Interpersonal violence during COVID‐19 quarantine. Psychiatry Research, 289(113), 046. 10.1016/j.psychres.2020.113046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milligan, K. , & Stabile, M. (2011). Do child tax benefits affect the well‐being of children? Evidence from Canadian child benefit expansions. American Economic Journal: Economic Policy, 3(3), 175–205. [Google Scholar]
- Nikolaidis, A. , Paksarian, D. , Alexander, L. , Derosa, J. , Dunn, J. , Nielson, D. M. , Droney, I. , Kang, M. , Douka, I. , Bromet, E. , Milham, M. P. , Stringaris, A. , & Merikangas, K. R. (2021). The Coronavirus Health and Impact Survey (CRISIS) reveals reproducible correlates of pandemic‐related mood states across the Atlantic. Scientific Reports, 11(1), 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orgilés, M. , Morales, A. , Delvecchio, E. , Mazzeschi, C. , & Espada, J. P. (2020). Immediate psychological effects of the COVID‐19 quarantine in youth from Italy and Spain. Frontiers in Psychology, 11, 2986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papatheodorou, C. , & Papathanasiou, S. (2017). The state of the children in Greece report: The children of the crisis. Hellenic National Committee for UNICEF. [Google Scholar]
- Perlman, D. , & Peplau, L. A. (1981). Toward a social psychology of loneliness. Personal Relationships, 3, 31–56. [Google Scholar]
- Pierce, M. , McManus, S. , Jessop, C. , John, A. , Hotopf, M. , Ford, T. , Hatch, S. , Wessely, S. , & Abel, K. M. (2020). Says who? The significance of sampling in mental health surveys during COVID‐19. The Lancet. Psychiatry, 7(7), 567–568. 10.1016/S2215-0366(20)30237-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramchandani, P. , & Stein, A. (2003). The impact of parental psychiatric disorder on children: Avoiding stigma, improving care. BMJ, 327, 242–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravens‐Sieberer, U. , Kaman, A. , Erhart, M. , Devine, J. , Schlack, R. , & Otto, C. (2022). Impact of the COVID‐19 pandemic on quality of life and mental health in children and adolescents in Germany. European Child & Adolescent Psychiatry, 31, 879–889. 10.1007/s00787-021-01726-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raw, J. , Waite, P. , Pearcey, S. , Creswell, C. , Shum, A. , & Patalay, P. (2021). Examining changes in parent‐reported child and adolescent mental health throughout the UK's first COVID‐19 national lockdown. Journal of Child Psychology and Psychiatry, 62(12), 1391–1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiss, F. (2013). Socioeconomic inequalities and mental health problems in children and adolescents: A systematic review. Social Science & Medicine, 90, 24–31. [DOI] [PubMed] [Google Scholar]
- Robinson, E. , Sutin, A. R. , Daly, M. , & Jones, A. (2022). A systematic review and meta‐analysis of longitudinal cohort studies comparing mental health before versus during the COVID‐19 pandemic in 2020. Journal of Affective Disorders, 296, 567–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers, J. P. , Chesney, E. , Oliver, D. , Pollak, T. A. , McGuire, P. , Fusar‐Poli, P. , Zandi, M. S. , Lewis, G. , & David, A. S. (2020). Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta‐analysis with comparison to the COVID‐19 pandemic. The Lancet. Psychiatry, 7(7), 611–627. 10.1016/S2215-0366(20)30203-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roustit, C. , Campoy, E. , Chaix, B. , & Chauvin, P. (2010). Exploring mediating factors in the association between parental psychological distress and psychosocial maladjustment in adolescence. European Child & Adolescent Psychiatry, 19(7), 597–604. 10.1007/s00787-010-0094-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saurabh, K. , & Ranjan, S. (2020). Compliance and psychological impact of quarantine in children and adolescents due to Covid‐19 pandemic. Indian J Pediatr, 87(7), 532–536. 10.1007/s12098-020-03347-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- VandePol, B. (2020). Resilience during COVID‐19 on vimeo. Html. https://archive.hshsl.umaryland.edu/handle/10713/12579 date accessed: 28 September 2020.
- Vostanis, P. , Graves, A. , Meltzer, H. , Goodman, R. , Jenkins, R. , & Brugha, T. (2006). Relationship between parental psychopathology, parenting strategies and child mental health‐‐findings from the GB national study. Social Psychiatry and Psychiatric Epidemiology, 41(7), 509–514. 10.1007/s00127-006-0061-3 [DOI] [PubMed] [Google Scholar]
- Waite, P. , Pearcey, S. , Shum, A. , Raw, J. A. , Patalay, P. , & Creswell, C. (2021). How did the mental health symptoms of children and adolescents change over early lockdown during the COVID‐19 pandemic in the UK? JCPP Advances, 1(1), e12009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, G. , Zhang, Y. , Zhao, J. , Zhang, J. , & Jiang, F. (2020). Mitigate the effects of home confinement on children during the COVID‐19 outbreak. Lancet (London, England), 395(10228), 945–947. 10.1016/S0140-6736(20)30547-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whelan, C. T. (1992). The role of income, life‐style deprivation and financial strain in mediating the impact of unemployment on psychological distress: Evidence from the Republic of Ireland. Journal of Occupational and Organizational Psychology, 65(4), 331–344. 10.1111/j.2044-8325.1992.tb00509.x [DOI] [Google Scholar]
- Xiang, M. , Zhang, Z. , & Kuwahara, K. (2020). Impact of COVID‐19 pandemic on children and adolescents' lifestyle behavior larger than expected. Progress in Cardiovascular Diseases, 63(4), 531–532. 10.1016/j.pcad.2020.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie, X. , Xue, Q. , Zhou, Y. , Zhu, K. , Liu, Q. , Zhang, J. , & Song, R. (2020). Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatrics, 174(9), 898–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahn‐Waxler, C. , Duggal, S. , & Gruber, R. (2002). Parental psychopathology. In Bornstein M. H. (Ed.), Handbook of parenting: Vol. 4. Social conditions and applied parenting (2nd ed., pp. 295–327). Mahwah, NJ. [Google Scholar]
- Zhou, S. J. , Zhang, L. G. , Wang, L. L. , Guo, Z. C. , Wang, J. Q. , Chen, J. C. , Liu, M. , Chen, X. , & Chen, J. X. (2020). Prevalence and socio‐demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID‐19. European Child & Adolescent Psychiatry, 29(6), 749–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


