Sir,
Brainstem as a location for neurocysticercosis (NCC) infection is considerably rare, and usually features third nerve involvement, internuclear ophthalmoplegia, and crossed brainstem syndromes.[1] Parinaud’s syndrome because of midbrain NCC has been rarely reported in literature, with most of these reports describing partial dorsal midbrain syndromes.[1,2,3] We present a case of midbrain NCC manifesting Parinaud’s syndrome with a few unusual features, including asymmetry and lack of pupillary involvement.
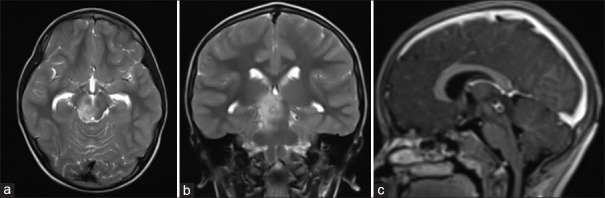
A previously healthy 12-year-old boy presented with 10 days’ history of vertical binocular diplopia, which was prominent on up gaze. He had no history of headache, fever, vomiting, anorexia, or weight loss. His older brother was also being managed at our center for focal epilepsy secondary to calcified intracranial neurocysticercosis. On examination, he was noted to have upgaze restriction with “V” pattern exotropia, impaired convergence, asymmetrical convergence-retraction nystagmus (CRN) (more prominent on the left), and Collier’s sign (lid retraction) on horizonal and up gaze [Video 1]. Light-near dissociation of pupillary reflex was not seen. Contrast-enhanced magnetic resonance imaging (MRI) of the brain revealed conglomerated ring-enhancing lesions in right paramedian dorsal midbrain with perilesional edema, with peripheral T2 hypointense rim and internal T2 hyperintense foci showing dot-like restricted diffusion, highly suggestive of neurocysticercosis [Figure 1].
Figure 1.
MRI brain showing (a) axial T2 weighted sequence and (b) coronal T2 weighted sequence showing a cyst with T2 hypointense rim and T2 hyperintense core edema in the right paramedian dorsal midbrain with surrounding edema; (c) contrast-enhanced sagittal sequence showing two conglomerate ring-enhancing lesions in the dorsal midbrain in the region of the superior colliculus
Routine blood tests including hemogram, hepatic and renal function, thyroid function, erythrocyte sedimentation rate, blood sugar, and chest X-ray were normal. Considering the radiological features of the lesion, including visualization of the scolex, and epidemiological evidence in the form of a household member with NCC, we made a diagnosis of probable midbrain NCC. As per the revised diagnostic criteria,[4] our patient offered one absolute criterion (presence of scolex), one major radiological criterion (enhancing lesions), and confirmative evidence in the form of resolution of the lesion. Clinical/exposure criterion was a residency in an endemic area.
The patient was treated with intravenous methylprednisolone pulse (500 mg once daily for 5 days) followed by oral prednisolone (1 mg/kg), which was administered in tapering doses over a period of 8 weeks. Due to the location of the lesions, antihelminthic therapy was not administered. With this treatment, he reported symptomatic improvement, and at a follow-up at 3 months, he reported continued improvement, with the resolution of diplopia on up gaze [Video 2]. MRI brain at the end of treatment also demonstrated resolution of the lesion and near-resolution edema [Supplementary Figure 1].
Isolated brainstem is a rare location for the development of neurocysticercosis.[1] In a literature review of 29 individual case reports of brainstem NCC, Del Brutto et al.[4] described midbrain to be the most frequent location. Brainstem cysts were usually small (less than 10 mm) and located close to the midline. As per reported literature, midbrain NCC usually leads to partial or complete third nerve involvement, although other midbrain syndromes such as Weber and Claude syndrome, and gaze disorders such as one-and-a-half syndrome have also been described. Parinaud’s syndrome due to midbrain neurocysticercosis is highly uncommon, and usually the full-blown syndrome is not seen, which comprises a triad of upgaze palsy, impaired convergence, and light-near dissociation.[5] However, isolated up gaze palsy or convergence deficits have been reported.[2,3] We have summarized these cases in Supplementary Table 1. Including our case, only two other cases have been reported of Parinaud’s syndrome with NCC.
Various therapeutic strategies have been described in literature in managing brainstem NCC, ranging from the use of cysticidal drugs to steroids alone, or even no treatment. Excellent clinical recovery has been documented, although the exact duration of steroid therapy may need to be individualized, as recurrence of symptoms on tapering steroids may occur.[6]
Our patient demonstrated certain unusual clinical findings; the asymmetry of the CRN demonstrated by our patient, which has not been observed previously, may be explained by the skewed burden of the cysticerci and surrounding edema toward the right side. We hypothesize that these likely impaired corrective saccades that could be generated due to the affectation of the third nerve fibers traversing to the medial rectus and other extraocular muscles on the right, which are necessary to produce CRN. This led to attenuation of the prominence of the CRN on the right side. The pathogenesis of CRN is not definitive, and it has variably been considered to be either a disorder of asynchronous opposing saccades, or of the vergence system. Asymmetry in our case points toward the former.[7]
This case highlights an unusual manifestation of an endemic disease due to its unusual location. It also highlights that Parinaud’s syndrome may present with a partial constellation of classical clinical features, which must not detract clinicians from classical localization to the dorsal midbrain.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos available on: www.annalsofian.org
Acknowledgements
We thank the patient and his parents for their co-operation.
REFERENCES
- 1.Del Brutto OH, Del Brutto VJ. Isolated brainstem cysticercosis: A review. Clin Neurol Neurosurg. 2013;115:507–11. doi: 10.1016/j.clineuro.2012.12.026. [DOI] [PubMed] [Google Scholar]
- 2.Shukla D. Midbrain cysticercal cyst. J Neurosci Rural Pract. 2012;3:93–4. doi: 10.4103/0976-3147.91974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lath R, Rajshekhar V. Solitary cysticercus granuloma of the brainstem.Report of four cases. J Neurosurg. 1998;89:1047–51. doi: 10.3171/jns.1998.89.6.1047. [DOI] [PubMed] [Google Scholar]
- 4.Del Brutto OH, Nash TE, White AC Jr, Rajshekhar V, Wilkins PP, Singh G, et al. Revised diagnostic criteria for neurocysticercosis. J Neurol Sci. 2017;372:202–10. doi: 10.1016/j.jns.2016.11.045. [DOI] [PubMed] [Google Scholar]
- 5.Keane JR. The pretectal syndrome: 206 patients. Neurology. 1990;40:684–90. doi: 10.1212/wnl.40.4.684. [DOI] [PubMed] [Google Scholar]
- 6.Kim JS, Jeong SM, Moon SY, Park SH. Third cranial nerve palsy from midbrain neurocysticercosis: Repeated exacerbation on tapering corticosteroids. J Neuroophthalmol. 2004;24:217–20. doi: 10.1097/00041327-200409000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Rambold H, Kömpf D, Helmchen C. Main sequence of convergence retraction nystagmus indicates a disorder of vergence. Ann N Y Acad Sci. 2002;956:592–4. doi: 10.1111/j.1749-6632.2002.tb02891.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.