Abstract
Gout is a chronic metabolic disease that seriously affects human health. It is also a major challenge facing the world, which has brought a heavy burden to patients and society. Hyperuricemia (HUA) is the most important risk factor for gout. In recent years, with the improvement of living standards and the change of dietary habits, the incidence of gout in the world has increased dramatically, and gradually tends to be younger. An increasing number of studies have shown that gene mutations may play an important role in the development of HUA and gout. Therefore, we reviewed the existing literature and summarized the susceptibility genes and research status of HUA and gout, in order to provide reference for the early diagnosis, individualized treatment and the development of new targeted drugs of HUA and gout.
Keywords: Hyperuricemia, Gout, Susceptibility gene, Single nucleotide polymorphism, Serum uric acid
Introduction
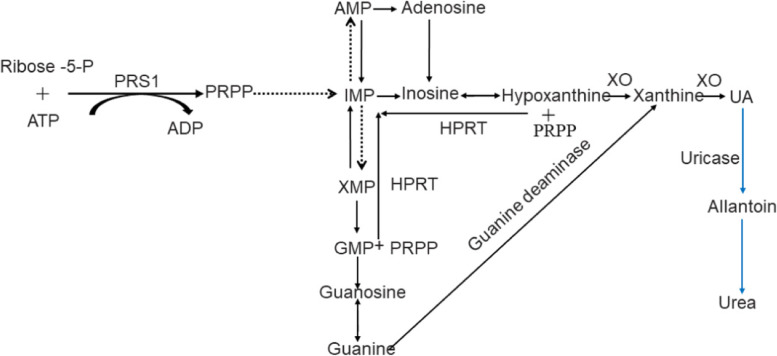
Gout is a common disease caused by purine metabolism disorder, which is primarily caused by the accumulation of uric acid (UA) crystals in joints and other tissues. It is typically characterized by recurrent episodes of acute inflammatory arthritis, and the metatarsophalangeal joint of the big toe is the most vulnerable part [1]. The occurrence of gout is often significantly correlated with the increase of serum uric acid (SUA) levels. In most mammals, UA is oxidized by uricase to a more water-soluble allantoin, which is excreted from the kidney (Fig. 1). However, in the process of human evolution, due to the silent mutation of the gene encoding uricase, UA becomes the final product of purine metabolism in humans, and its concentration is 3 to 10 times that of other mammals [2]. When the concentration of SUA in human exceeds 420 μmol/L (male) or 360 μmol/L(female) was defined as HUA. HUA plays a crucial role in the occurrence and development of gout. It has been reported that about a quarter of patients with HUA will develop gout [3]. Chronic gout can lead to lifelong disability. Moreover, studies have shown that the heritability of SUA is about 73% [4], which suggests that HUA and gout are largely determined by genetic factors. Therefore, it is significant to explore HUA and gout from the perspective of genetic variation.
Fig. 1.
Uric acid metabolism diagram. The solid line represents one-step reaction and the dotted line represents multi-step reaction, the blue part is mainly found in most mammals except humans
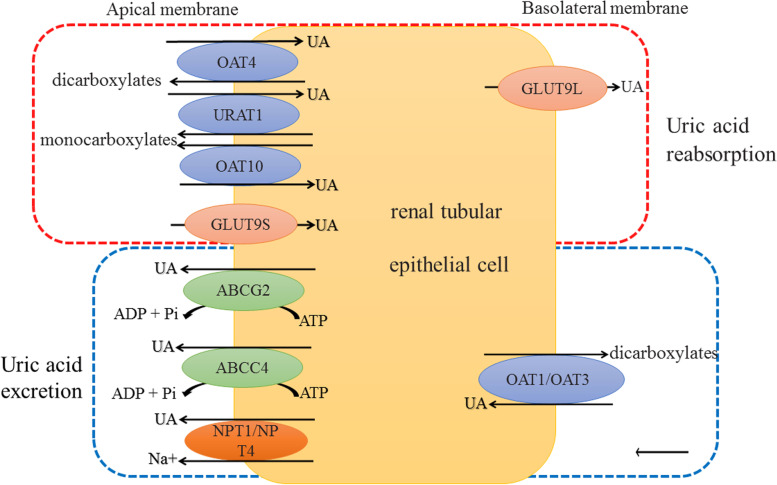
UA is mainly produced by the liver, two-thirds of which is excreted via the kidney and one-third via the intestine [5]. Among them, HPRT and PRS1 are the most important enzymes involved in liver UA production (Fig. 1); while GLUT9, ABCG2 and OATs, etc. are the main transporters involved in the reabsorption and excretion of UA in the kidney and intestine (Fig. 2). Studies have shown that HPRT and PRPS1 gene mutations seem to be the main cause of primary gout [6]; SLC22A11 gene mutation is associated with RUE (renal underexcretion) gout [7]; ABCG2 seems to be one of the reasons for the genetic heterogeneity of ROL (renal overload) and RUE gout [8]. It can be seen that any abnormality of enzymes or transporters involved in UA metabolism and their upstream genes will affect SUA levels. Consequently, this paper reviews the genes involved in HUA and gout mainly from three aspects (Table 1): UA production, UA reabsorption and UA excretion.
Fig. 2.
UA transport proteins on the membrane of renal tubular epithelial cells. In the red square frame are transport proteins involved in UA reabsorption. In the blue square frame are transport proteins involved in UA excretion
Table 1.
Susceptibility Genes of HUA and Gout
| Classification | Gene name | Gene product | Location (human) | Tissue distribution | Refs |
|---|---|---|---|---|---|
| Production | HPRT1 | HPRT1 | Xq26.2-q26.3 | Multi-tissue expression | NCBI, [9] |
| PRPS1 | PRS1 | Xq22.3 | Multi-tissue expression | NCBI, [10] | |
| ALDH16A1 | ALDH16A1 | 19q13.33 | High expression in kidney | NCBI, [11] | |
| Reabsorption | SLC22A11 | OAT4 | 11q13.1 | Kidney | NCBI, [12, 13] |
| SLC22A12 | URAT1 | 11q13.1 | Kidney | NCBI, [13] | |
| SLC22A13 | OAT10 | 3p22.2 | Kidney | NCBI, [14] | |
| SLC2A9 | GLUT9 | 4p16.1 | Liver and kidney | NCBI, [15] | |
| Excretion | ABCG2 | BCRP | 4q22.1 | Kidney and other tissues | NCBI, [16] |
| ABCC4 | MRP4 | 13q32.1 | Kidney and other tissues | NCBI, [17] | |
| SLC22A6 | OAT1 | 11q12.3 | Kidney and other tissues | NCBI, [13, 18] | |
| SLC22A8 | OAT3 | 11q12.3 | Kidney and other tissues | NCBI, [13, 18] | |
| SLC17A1 | NPT1 | 6p22.2 | Kidney and other tissues | NCBI, [12] | |
| SLC17A3 | NPT4 | 6p22.2 | Kidney and other tissues | NCBI, [12, 19] | |
| SLC17A4 | NPT5 | 6p22.2 | Kidney and other tissues | NCBI, [12, 20] | |
| SLC2A12 | GLUT12 | 6q23.2 | Kidney and other tissues | NCBI, [21] | |
| Other | PDZK1 | Various scaffold proteins | 1q21.1 | Liver, kidney and other tissues | NCBI, [22] |
| GCKR | GKRP | 2p23.3 | Liver | NCBI | |
| PKD2 | Polycytin-2 | 4q22.1 | Multi-tissue expression | NCBI, [23, 24] | |
| SLC16A9 | MCT9 | 10q21.2 | Kidneys and other tissues | NCBI, [12] | |
| CARMIL1 | CARMIL1 | 6p22.2 | Kidney and other epithelial tissues | NCBI, [25] | |
| SCGN | Secretagogin | 6p22.2 | Neuroendocrine tissue and pancreas | NCBI, [12] | |
| UMOD | THP | 16p12.3 | The major secretory protein in urine | NCBI, [26, 27] |
Genes related to UA production
HPRT
HPRT gene is located on human chromosome X (xq26.2-q26.3), with a total length of 44 kb, including 9 exons and 8 introns, encoding hypoxanthine guanine phosphoribosyltransferase (HPRT) [9]. As shown in Fig. 1, HPRT is the most important enzyme in the purine salvage pathway, which catalyzes the synthesis of hypoxanthine into hypoxanthine nucleotides and the conversion of guanine into guanine nucleotides. Its activity is regulated by the synergistic effect of guanine and IMP [28]. HPRT gene mutation can cause HPRT enzyme activity defect, then it will lead to the surplus of its substrates hypoxanthine and guanine, and these surplus purines will be converted into UA under the action of xanthine oxidase (XO) (Fig. 1), resulting in the increase of UA levels in the body [29], and finally cause gout. Clinically, the disease caused by HPRT deficiency belongs to X-linked genetic disease, which mainly affects men [30], and the severity of the disease is positively correlated with the degree of enzyme deficiency [31]. Moreover, diseases caused by HPRT gene mutations can be divided into three types according to the degree of enzyme deficiency: the most serious one is Lesch-Nyhan syndrome (LND) with enzyme activity less than 1.5%, mainly manifested in HUA, abnormal development of nervous system, involuntary movement, and self-injurious behavior; however, 1.5–2% of patients with enzyme activity showed HUA with neurological dysfunction; in addition, Keeley-seegmiller syndrome with enzyme activity of 8%—60% only shows HUA related symptoms [31]. Recently, studies have found that HPRT pathogenic mutants c.103G > A (p.V35M) [12], c.277-281delATTGC, c.299 (exon 3) T > A, c.468-470delGAT and loss (exon: 6) 84 bp are related to family juvenile gout. [6]. The interaction between HPRT gene mutants and β-amyloid precursor protein (APP) gene regulate the epigenetics of LND by affecting alternative APP pre-mRNA splicing [32]. The increase of SUA caused by HPRT deficiency is regulated by GLUT9 single nucleotide polymorphism (SNP) [5]. P53 up-regulates the expression of HPRT [33]; miR-181a down-regulates the expression of HPRT [34]. It can be seen that HPRT pathogenic mutants are significantly associated with familial juvenile gout. Therefore, it is particularly important to detect HPRT gene in these patients.
PRPS1
PRPS1 gene is located on human chromosome X (Xq22.3), encoding phosphoribosyl pyrophosphate synthase 1 (PRS1), which is involved in human nucleotide synthesis via catalyzing the synthesis of phosphoribosyl pyrophosphate (PRPP) by adenosine triphosphate (ATP) and 5-phosphoribosyl (R-5P) (Fig. 1) [10]. PRPS1 is transcriptionally regulated by miR-p376 [35], whose accelerated transcription will lead to the superactivity of PRS1 and eventually cause the increase of UA synthesis [36]. In general, pathogenic mutants of PRPS1 cause hereditary gout, Arts syndrome, Charcot-Marie-Tooth neuropathy type 5 (CMTX5) and X-linked deafness 1 (DFNX1), and mainly affect men [37]. Recently, Zikanova et al. [38] found a new mutation of PRPS1: c.520 G > A (p.G174R) leads to PRS1 hyperactivity, then resulting in severe HUA. In addition, Yang et al. [36] also found another missense mutation of PRPS1: c.521(exon)G > T, p. (Gly174Val) is associated with HUA and gout. However, studies have found that PRPS1 missense mutant c.359G > T (p.Gly120Val) causes a rare adult-onset cerebellar ataxia in female [37], and PRPS1 mutant c.82 G > C causes optic atrophy and deafness [39]. It can be seen that only the mutations that causes the superactivity of PRPS1 will increase the synthesis of UA. Therefore, the possibility of PRPS1 gene mutation cannot be ruled out when SUA levels is normal. Furthermore, the detection of PRPS1 activity is great significance for the early diagnosis of HUA and gout. PRPS1 may be a potential target for the treatment of HUA and gout in the future. Because this gene mutation is more likely to occur in early-onset gout, thus, young patients with simple HUA should be screened for PRPS1 mutation.
ALDH16A1
ALDH16A1 gene is located on human chromosome 19q13.33 and consists of 17 exons, encoding acetaldehyde dehydrogenase 16 family A1 (ALDH16A1) [11]. It is highly expressed in kidney [40] and catalyzes a variety of aldehyde reactions [11]. Leask et al. found that ALDH16A1 rs150414818 (Pro476Arg) mutation disrupted the interaction between ALDH16A1 and HPRT, thereby affecting purine metabolism, resulting in elevated UA [41]. In mice, knockdown of ALDH16A1 resulted in decreased SLC17A3 expression and increased SLC16A9 and ABCC4 expression [41]. Therefore, ALDH16A1 may be involved in the regulation of SUA via interacting with other UA transporters.
Genes related to UA reabsorption
Solute carrier family 22 (SLC22A)
SLC22A11
SLC22A11 gene is located on chromosome 11q13.1, encoding organic anion transporter 4 (OAT4) and is expressed in the apical membrane of renal proximal tubular epithelial cells. OAT4 is an asymmetric UA transporter with 53% homology with URAT1 [12]. It reabsorbs UA in the form of exchange between organic anions and dicarboxylate (Fig. 2) [12, 13]. The expression of OAT4 is regulated by PDZK1, NHERF1 and protein kinase C [13, 42]. IL-23 down-regulates OAT4 mRNA expression [43]. In addition, the inhibition of Wnt signaling pathway down-regulates the expression of OAT1, OAT3 and OAT4 [42]. GWAS have revealed that SLC22A11 rs17300741 was associated with SUA levels, while rs2078267, rs2186571, rs17299124 and rs17300741 were associated with gout [44]. Among them, rs17300741 is dramatically associated with RUE gout in Japanese population [7], but whether this association exists in other regions has not been confirmed.
SLC22A12
SLC22A12 gene is located on chromosome 11q13.1 and encodes urate transporter 1 (URAT1), which is expressed in the apical membrane of renal tubular epithelial cells. URAT1 is a high affinity UA transporter, which absorbs UA from raw urine and plays an important role in maintaining human UA homeostasis. Like OAT4, URAT1 is also an asymmetric UA transporter [13], which participates in the reabsorption of UA through monocarboxylate exchange (Fig. 2). SLC22A12 gene dysfunctional mutations cause URAT1 dysfunction, then leading to hereditary renal hypouricemia type 1 (RHUC1), which is characterized by decreased SUA levels and increased UA excretion [45]. Epidemiological investigation showed that 90% of hypouricemia (SUA ≤ 2.0 mg/dl) was caused by nonfunctional URAT1 mutations [46]. The rare variant of SLC22A12 gene is considered to have strong ethnic specificity [47]. SLC22A12 rs559946 is associated with a higher risk of gout in the Han population; rs3825017 is associated with gout risk in Czech population; rs75786299, rs7929627 and rs3825017 are associated with HUA in Korean population [37]; rs11231825 (p.H142H) is related to gout susceptibility in Vietnamese population [48]. SLC22A12 rs121907896(p.R90H) and rs121907892 (p.W258X) are the two most common variants leading to hypouricemia in the Japanese population [49, 50]. Sakiyama et al. [50] proved that these two variants were protective factor for HUA and gout. Consistent with previous studies, pavelcova et al. also found that SLC22A12 gene variant rs3825017 (p.N82N) increased the risk of gout [51]. However, Toyoda et al. [53] found that dysfunctional mutations of SLC22A12 gene have prominent anti-gout effect. Even in the presence of ABCG2 pathogenic mutations, these mutations still have a protective effect on gout. In addition, they found that the protective effect of SLC22A12 on gout exceeded the pathogenic effect of ABCG2 on gout. Meta-analysis showed that SLC22A12 rs3825016 and rs3825018 are risk factors for gout and HUA, while rs475688 is a protective factor for HUA [52]. It can be seen that the vast majority of SLC22A12 gene mutations inhibit the function of URAT1 and reduce the risk of gout. In addition, 27-Hydroxycholesterol (a metabolite of cholesterol) can activate SLC22A12 gene promoter via estrogen response elements (EREs), and then up-regulate the expression of SLC22A12 [53].
SLC22A13
SLC22A13 gene is located on chromosome 3p21.3, which encodes organic anion transporter 10 (OAT10). It is expressed in the apical membrane of proximal tubular epithelial cells [14]. In vitro analysis showed that OAT10 is a low affinity UA transporter, which has 44% homology with OAT1 and is mainly involved in the reabsorption of UA (Fig. 2) [54]. Insulin can selectively activate its UA transport function [55]. Bahn et al. [54] found that the expression of SLC22A13 in chickens was gender dependent, and the female was higher than the male. However, this gender dependent expression does not seem to exist in humans, because the SUA levels of men is higher than women. Recent studies have also shown that dysfunctional missense mutation of SLC22A13 gene reduced SUA levels and the risk of gout. Meta-analysis displayed that rs117371763 (R377C) variant of SLC22A13 gene has significant anti-gout effect [56]. It is certain that SLC22A13, like SLC22A12, can provide effective targets for the treatment of gout.
SLC2A9
SLC2A9 gene is located on chromosome 4p16.1 and has 13 exons, encoding glucose transporter 9 (GLUT9) with strong UA transport capacity, which is mainly expressed in liver and kidney [15]. Human GLUT9 has two subtypes: GLUT9L and GLUT9S. In proximal tubular epithelial cells, GLUT9L expressed in the basolateral membrane is the only UA efflux transporter [57](Fig. 2); GLUT9S expressed in the apical membrane regulates the reabsorption of UA together with URAT1 [58] (Fig. 2). Therefore, the loss of GLUT9 function will completely inhibit the outflow of UA, thus blocking the reabsorption of UA by the apical membrane UA transporter. It is well known that SLC2A9 gene mutation causes hereditary renal hypouricemia type 2 (RHUC2), which is characterized by severe hypouricemia and easy to be complicated with acute renal failure and renal calculi. Windpesl M et al. found that SLC2A9 gene mutation is a cause of RHUC2 in Austrian native families, especially homozygotes will have severe hypouricemia, and carriers have a higher risk of acute renal injury (AKI) [59]. Moreover, the CC genotype of SLC2A9 SNP rs1172228 in gout patients is significantly associated with renal calculi in Malaysian population [60]. However, consistent with previous results, two variants of SLC2A9 gene (p.V282I:rs16890979 and c.1002 + 78A > G:rs6823877) may be protective factors of gout [51]. Moreover, SLC2A9 SNP rs62293298 attenuates the risk of HUA [61]. In addition, SLC2A9 SNPs affect gout caused by HPRT deficiency and the therapeutic response of allopurinol [5]. Meta-analysis showed that SNP rs16890979, rs1014290and rs12510549 of SLC2A9 could prevent gout. Among them, rs16890979 was associated with lower gout risk in Caucasians and Asians, rs1014290 was associated with lower gout risk in Asians, and rs12510549 was associated with lower gout risk in Caucasians [62]. SLC2A9 rs3733591 (Arg265His) variant increases the risk of gout [45]. SLC2A9 rs 737267, rs6449213 and rs1014290 are associated with gout in the UK, German and Croatian populations, respectively [45]. SLC2A9 rs3775948G and rs13129697G alleles reduce the risk of HUA [63]. Therefore, SLC2A9 SNPs may have a protective effect on gout, but its severe hypouricemia and its complications may endanger the lives of patients. Non-additive genetic interaction between SLC2A9 and insulin related genes also affects SUA [55]. Moreover, this effect is most obvious in women, which is consistent with the greater effect of SLC2A9 on UA in women. Insulin promotes the activity of various UA transporters via activating MAPK p38, MAPK p44/42 and Akt pathways [55]. E4 promoter- binding protein 4 (E4BP4) gene directly binds P2 promoter to down-regulate the expression of SLC2A9 in mouse liver [64].
Genes related to UA excretion
ABCG2
ATP-binding cassette (ABC) transporters belong to the transmembrane protein family and are divided into seven subfamilies: A-G. At present, it is known that there are five members of ABCG subfamily: ABCG1, ABCG2, ABCG4, ABCG5 and ABCG8 [16]. Among them, the ABCG2 gene is located in chromosome 4q22.1, which consists of 16 exons and 15 introns, encoding ABC transporter G2(ABCG2), also known as breast cancer resistance protein (BCRP). ABCG2 is an ATP dependent exogenous transporter, which mediates the excretion of UA (Fig. 2) [65, 66]. Therefore, ABCG2 dysfunction will increase the risk of HUA and gout. Progesterone response factor down-regulates the expression of ABCG2, while estrogen response element up-regulates its expression [67]. GWAS showed that the genetic variation of ABCG2 seems to be one of the reasons for the genetic heterogeneity of ROL and RUE gout [8]. Its pathogenic mutants are considered to be the strongest genetic risk factor for RUE gout and HUA [68]. Among them, rs2231142 (Q141K) variant reduces its allele expression in the kidney and block the excretion of intestinal UA [41]. Furthermore, rs2231142 has gene dose effect on gout [61]. In Xenopus oocytes, insulin could up-regulate the transport activity of ABCG2, but does not affect the transport activity of Q141K variant [55]. In the mouse model, knock-in ABCG2 Q141K variant could down-regulate the expression of ABCG2 in male mice without affecting female mice [69]. ABCG2 rs372192400 (R147W), rs753759474 (T153M), rs752626614 (F373C) and rs200894058 (S572R) could down-regulate the expression of ABCG2 [68]. ABCG2 rs2054576 is related to HUA in the Korean population [70]; rs72552713 is associated with gout susceptibility in Vietnamese population [48]; c.725 T > C (p. I242T) is involved in the occurrence of early-onset HUA and gout [71]. Moreover, the more pathogenic variants carrying ABCG2, the earlier the onset of HUA and gout [68]. Interestingly, meta-analysis showed that ABCG2 SNP rs2231137 (p.V12M) was a protective factor for gout [72]. The genotype combination of mutants Q141K and Q126X can be used to evaluate ABCG2 activity [73]. The association of A1CF variation and BAZ1B variation with HUA and gout has also been concerned recently. Intriguingly, these two new variants appear to be associated with ABCG2 dysfunctional variants. In other words, when ABCG2 dysfunctional variation and A1CF variation exist at the same time, A1CF variation is significantly correlated with gout, but in the absence of ABCG2 variation, the correlation between A1CF variation and gout is no longer significant. However, the BAZ1B variation has a significant correlation with gout with or without ABCG2 dysfunctional variation [74]. It can be seen that ABCG2 gene variants and their SNPs are not only risk factors for HUA and gout, but also increase the risk of HUA and gout via interacting with other gene variants.
ABCC4
ABCC is the largest subfamily of ABC Family with 9 members. ABCC4 gene is located on chromosome13q32.1 [17]and encodes multidrug resistance protein 4 (MRP4) [75]. It is mainly expressed in the basolateral membrane of hepatocytes and apical membrane of proximal renal tubular epithelial cells [76]. MRP4 is an ATP dependent unidirectional efflux pump, which can participate in the excretion of UA in proximal tubules in coordination with BCRP [77] (Fig. 2). miR-124a and miR-506 down-regulate the expression of ABCC4 [78]. In poultry, knockdown of ABCC4 in proximal tubules reduced UA secretion by 80% [77]. It can be seen that ABCC4 is the key transporter of UA excretion in poultry kidney. Afterwards, Tanner et al. [79] repeated sequencing of ABCC4 in patients with HUA in New Zealand Māori and Pacific, identified a common variant SNP rs4148500 and a rare variant P1036L that were significantly associated with HUA and gout. They also found that the transport activity of MRP4 seemed to be affected by elevated UA levels, because the UA transport activity of MRP4 in individuals with P1036L mutation decreased by 30% compared with normal controls. Obviously, ABCC4 plays a key role in maintaining UA homeostasis.
SLC22A6 and SLC22A8
Human SLC22A6 and SLC22A8 genes are located on chromosome 11q12.3. The former encodes organic anion transporter 1 (OAT1) and the latter encodes organic anion transporter 3 (OAT3). In the kidney, immunohistochemistry showed that both OAT1 and OAT3 were located in the basolateral membrane of proximal tubular epithelial cells [13, 18]. OAT1 and OAT3 not only show overlapping substrate specificity, but also share transportation mode and driving force. They are famous multi-specific drug transporters [80]. The expression of OAT1 and OAT3 are regulated by protein kinase A and C [42]. Inhibition of Wnt signaling pathway down-regulates the expression of OAT1 and OAT3 [42]. Hepatocyte nuclear factor 1-α significantly up-regulates the expression of OAT1 in mouse kidney [81]. Estrogen receptor-α (ER-α) indirectly induces the transcriptional expression of OAT1 [82]. cAMP-response element(CRE) regulates the constitutive expression of human SLC22A8 gene [83]. Previous studies have shown that UA is the endogenous substrate of OATs [18]. OAT1 and OAT3 participate in the excretion of SUA through UA/dicarboxylate exchanger [84] (Fig. 2). Existing studies have shown that the expression of OAT1 and OAT3 is decreased in HUA. Recently, it was found that alcohol-soluble extract increases the expression of OAT1 and reduces the expression of URAT1, so it has significant anti-gout effect and does not affect renal function [85]. In addition, the study found that total flavonoids of S. glabra has a significant UA lowering effect in mice, because it can not only up-regulate the expression of OAT1 in kidney, but also inhibit xanthine oxidase [86]. Although SLC22A6 and SLC22A8 play a key role in UA transport, the specific mechanism of these two genes in HUA and gout still needs to be further studied, so as to provide new targets for the treatment of HUA and gout.
SLC17A
SLC17A family transporters are Na+ dependent phosphate transporters, which can mediate the transmembrane transport of organic anions and coordinate UA excretion [87]. Up to now, there are three major genes in SLC17A family involved in UA transport (Fig. 2): SLC17A1, SLC17A3 and SLC17A4, which all located on chromosome 6p22.2. Among them, sodium dependent phosphate transporter 1 (NPT1), encoded by SLC17A1, is located in the apical membrane of renal proximal tubular epithelial cells [12]. E4BP4 down-regulates the expression of SLC17A1 in mouse liver [64]. Sodium dependent phosphate transporter 4 (NPT4), encoded by SLC17A3, is mainly expressed in the liver and kidney and is involved in the secretion of UA (Fig. 2) and the elimination of various anionic drugs [19]. SLC17A4 encodes sodium dependent phosphate transporter 5 (NPT5), which is mainly expressed in pancreas, liver and intestine [20], but weakly expressed in kidney [12]. Recently, it was found that SLC17A1 and SLC17A3 SNPs are related to SUA levels, which may be involved in the occurrence of gout [65]. SLC17A1 rs1165196 significantly enhances UA secretion and reduces the risk of RUE gout; while rs9393672 and rs942379 are significantly correlated with female SUA [44].
SLC2A12
SLC2A12 encodes glucose transporter 12 (GLUT12), which belongs to the same family as GLUT9. It is a physiological UA transporter and is widely expressed in liver and kidney [21]. GLUT12 is a sodium independent bidirectional UA transporter, which may be involved in the transport of UA from blood to liver. In the mouse model of HUA, knockout of SLC2A12 gene causes SLC2A12 dysfunction, which leads to the increase of SUA levels [21]. It can be seen that SLC2A12 deletion mutations may increase the incidence of HUA and gout.
Other genes involved in UA regulation
PDZK1
PDZ domain-containing 1 (PDZK1) is a scaffold protein located on chromosome 1q21.1 that regulates SUA levels via participating in the assembly of renal UA transporter complex [22]. Although PDZK1 is not directly involved in UA transport, it interacts with C-terminal of various UA transporters, thereby regulating the expression of related proteins [41]. In human embryonic kidney 293 cells (HEK293 cells), co-expression of PDZK1 and URAT1 enhances the transport capacity of UA [77]. PDZK1 rs12129861 is considered as a risk allele for gout [88]. PDZK1 rs1967017 up-regulates the expression of PDZK1 via altering the transcription factor binding site of HNF4A [89]. Long noncoding RNA (lncRNA) PENG up-regulates the expression of PDZK1 via secreting miR-15b [90]. In addition, ABCG2 and PDZK1 gene-gender interactions are associated with gout risk in European populations [91].
PKD2
Like ABCG2, PKD2 gene is also located on chromosome 4q22.1 [23, 24], encoding ion channels of transient receptor potential superfamily (TRPP2, PKD2, PC2 or polycystin-2) [92]. It is related to the development, morphology and function of renal tubules and participates in the regulation of intracellular calcium homeostasis and other signal transduction pathways [93].Studies have confirmed that the epistatic interaction between PKD2 and ABCG2 is associated with the risk of HUA and gout [94]. The interaction between PKD2 SNP rs2725220 and nutritional factors increases the risk of HUA and gout in Koreans [95]. In addition, PKD2 expressed in B cells may be involved in B cell-mediated gout inflammation [96].
SLC16A9
SLC16A9 gene encodes monocarboxylic acid transporter 9 (MCT9), which is mainly expressed in kidney, parathyroid gland, trachea, spleen and adrenal gland [12]. MCT9 is mainly involved in the reabsorption of renal UA [41], and its activity is regulated by extracellular H+ and Na+ [97]. In addition, SLC16A9 SNPs are closely related to the occurrence and development of gout. Among them, rs2242206 reduces UA excretion in the intestine, which is significantly correlated with ROL gout, while rs550527563 is dramatically correlated with early-onset gout [98, 99]. Although it has been confirmed that there is a remarkable correlation between SLC16A9 gene and different types of gout, its specific regulatory mechanism is not clear. This suggests that if we can clearly clarify the specific mechanism of SLC16A9 on gout in future research, which may provide an effective target for the precise treatment of gout.
CARMIL(LRRC16A)
CARMIL gene is located on chromosome 6p22.2 and encodes myosin I connexin (CARMIL). It is expressed in kidney and other epithelial tissues and participates in the maintenance of cell shape [25]. CARMIL affect the activity of actin, which interacts with UA transporter and scaffold protein on renal apical membrane, so as to affect the function of UA transporter and indirectly cause the change of SUA levels [100]. A meta-analysis showed that LRRC16A was related to UA concentration [12]. Subsequently, Sakiyama et al. [100] found that LRRC16A SNP rs742132 was related to gout susceptibility in Japanese population. Sakiyama and others researchers believe that LRRC16A may participate in the occurrence and development of gout by affecting the function of UA transporter. However, there are few studies on the relationship between this gene and gout, and the specific regulatory mechanism is not clear.
SCGN
SCGN gene is located on chromosome 6p22.2. It encodes secretagogin,which is mainly expressed in neuroendocrine tissues and pancreatic β cells [12]. GWAS showed that SCGN was correlated with SUA levels [12]. In addition, studies on the change of SUA levels caused by this gene mutation have been reported [101]. However, the relationship between SCGN gene and gout has not been reported.
MAF
MAF is a transcription factor [102] involved in the regulation of SUA, which is highly expressed in human and mouse kidneys [103]. MAF gene expression is regulated by two independent upstream genetic signals, of which lncRNA is the most prominent [41]. It not only affects the structure and function of kidney, but also participates in the regulation of renal urate, and is related to SUA and gout susceptibility [104]. Recently, Higashino et al. [104] found that a common variant rs889472 of c-MAF was related to gout susceptibility in Japanese men through univariate logistic regression analysis.
UMOD
Uromodulin (UMOD) is encoded by UMOD gene located on chromosome 16p12.3, also known as Tamm-Horsfall protein (THP). It is the major protein secreted in normal urine [26, 27]. Its expression is regulated by transcription factors such as SP1, TP3, POU2F1, STAT3 and RARA [105]. Researchers found that more than 90% of UMOD gene mutations occurred in exons 3 and 4 [27]. This mutation causes autosomal dominant tubulointerstitial kidney disease (ADTKD-UMOD), also known as familial juvenile HUA nephropathy (FJHN) [27, 106]. This disease is an autosomal dominant disease, which is rare in children. It is mainly characterized by HUA, gout and chronic progressive nephropathy [107]. Interestingly, recently, ADTKD-UMOD caused by a new mutation of UMOD gene (c.1648G > A, p.V550I) was found in a 3-year-old Chinese boy [108], and the child showed persistent hematuria. On the contrary, a new UMOD gene mutation (c.163 g > A) was recently identified in the Brazilian family. Although it is related to ADTKD, the affected members do not seem to show HUA and gout [109]. In addition, homozygous mutations in UMOD gene seem to be more prone to early-onset gout [27]. The study found that the methylation level of UMOD in peripheral blood was related to the risk of gout, and its methylation evaluation could predict the risk of gout [110].
ALDH2
Aldehyde dehydrogenase 2 family member (ALDH2) gene is located on chromosome 12q24.12 and encodes aldehyde dehydrogenase 2 (ALDH2), which participates in alcohol metabolism. ALDH2 rs671 p.Glu504Lys pathogenic mutant reduces the activity of ALDH2, which is associated with reduced risk of gout [41].In addition, the rs671 GA + AA genotype was found to be associated with a lower risk of gout, while alcohol and BMI abnormalities were associated with a higher risk of gout in Taiwan population. Moreover, BMI and alcohol have a significant interaction on the risk of gout in patients with GG and GA + AA [111].
UA regulatory genes related to glycolysis
In humans, the disorder of glycometabolism can also indirectly affect purine metabolism, thus affecting SUA levels. For example, fructose can indirectly elevate SUA levels via increasing ATP degradation in the liver [112]. Moreover, many genes involved in glycometabolism (such as GCKR; PKLR; MLXIPL; PRKAG2; NFAT5; NF4G, etc.) indirectly affect SUA levels. Current studies have shown that among many genes involved in glycolysis, GCKR gene (located on chromosome 2p23.3) encoding glucokinase regulatory protein seems to be the most important gene affecting SUA levels. Its expression is regulated by lncRNAs ENST00000588707.1 and TCONS_00004187 [113]. Furthermore, GCKR gene mutations accelerate the transition from asymptomatic HUA to gout, and its SNP rs1260326 is associated with a higher risk of gout [114, 115]. Interestingly, GCKR interacts with alcohol to reduce the risk of gout [116].
Conclusion
This paper reviews the susceptibility genes and their variants involved in UA transport on HUA and gout. We found that SLC22A family, ABC family and SLC2A family are the most studied gene families among many susceptible genes at present. Interestingly, SLC22A family gene mutations can not only increase the risk of HUA and gout, but also reduce SUA levels and even cause severe hypouricemia. Moreover, some SNPs of SLC22A family (such as rs121907896 and rs121907892) also have significant anti-gout effects.
In summary, genomic studies on UA metabolism contribute to an in-depth understanding of the pathogenesis of HUA and gout. Generally speaking, gene level changes often precede protein level in the process of disease occurrence and development. Therefore, the study of HUA and gout at the gene level is still an important direction of our future research. If we can identify the highly specific and sensitive gene markers of elevated SUA levels, then, it will provide great help for the early diagnosis of HUA and the prevention and targeted treatment of gout patients.
Acknowledgements
Every step of this paper is completed under the guidance of my tutor Dr. You. Thank you very much for your guidance. I also thank my tutor Jiang Yao for her guidance and help in the revision of the review.
Abbreviations
- SUA
Serum uric acid
- UA
Uric acid
- HUA
Hyperuricemia
- PRS1
Phosphoribosyl pyrophosphate synthase1
- HPRT
Hypoxanthine–guanine phosophoribosyltransferase
- PRPP
5'-Phosphoribosyl-1'-pyrophosphate
- IMP
Inosine monophosphate
- GMP
Guanosine monophosphate
- XO
Xanthine oxidase
- LND
Lesch-Nyhan syndrome
- APP
β-Amyloid precursor protein
- ALDH16A1
Acetaldehyde dehydrogenase 16 family A1
- OAT1/3/4/10
Organic anion transporter 1/3/4/10
- SNP
Single nucleotide polymorphism
- GWAS
Genome-wide association studies
- RUE gout
Renal underexcretion gout
- URAT1
Urate transporter 1
- RHUC1
Hereditary renal hypouricemia type 1
- GLUT9/12
Glucose transporter 9/12
- RHUC2
Hereditary renal hypouricemia type 2
- E4BP4
E4 promoter-binding protein 4
- AKI
Acute renal injury
- BCRP
Breast cancer resistance protein
- MRP4
Multidrug resistance protein 4
- NPT1/4/5
Sodium dependent phosphate transporter 1/4/5
- PDZK1
PDZ domain-containing 1
- HEK293 cells
Human embryonic kidney 293 cells
- lncRNA
Long noncoding RNA
- MCT9
Monocarboxylic acid transporter 9
- ROL gout
Renal overload gout
- CARMIL
Myosin I connexin
- UMOD
Uromodulin
- THP
Tamm-Horsfall protein
- ADTKD-UMOD
Autosomal dominant tubulointerstitial kidney disease
- FJHN
Familial juvenile hyperuricemia nephropathy
Authors’ contributions
All authors are involved in the conception and drafting of the article and are responsible for its integrity.
Funding
This work was supported by the Science and Technology Plan Project of Gansu (21YF5FA126), and the Cuiying Scientific and Technological Innovation Program of Lanzhou University Second Hospital (CY2018-MS10).
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All of the named authors have agreed to submit the paper in its present form.
Competing interests
There is no conflict of interest between all authors.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yue-Li Nian, Email: nianyl21@lzu.edu.cn.
Chong-Ge You, Email: youchg@lzu.edu.cn.
References
- 1.Merriman TR. An update on the genetic architecture of hyperuricemia and gout. Arthritis Res Ther. 2015;17:98. doi: 10.1186/s13075-015-0609-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pillinger MH, Mandell BF. Therapeutic approaches in the treatment of gout. Semin Arthritis Rheum. 2020;50(3s):S24–s30. doi: 10.1016/j.semarthrit.2020.04.010. [DOI] [PubMed] [Google Scholar]
- 3.Campion EW, G R, DeLabry LO, Asymptomatic hyperuricemia Risks and consequences in the normative aging study. Am J Med. 1987;82(3):421–6. doi: 10.1016/0002-9343(87)90441-4. [DOI] [PubMed] [Google Scholar]
- 4.Yang Q, et al. Genome-wide search for genes affecting serum uric acid levels: the Framingham Heart Study. Metabolism. 2005;54(11):1435–1441. doi: 10.1016/j.metabol.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 5.Torres RJ, Puig JG. GLUT9 influences uric acid concentration in patients with Lesch-Nyhan disease. Int J Rheum Dis. 2018;21(6):1270–1276. doi: 10.1111/1756-185X.13323. [DOI] [PubMed] [Google Scholar]
- 6.Li L, et al. Description of the molecular and phenotypic spectrum of Lesch-Nyhan disease in eight chinese patients. Front Genet. 2022;13:868942. doi: 10.3389/fgene.2022.868942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sakiyama M, et al. A common variant of organic anion transporter 4 (OAT4/SLC22A11) gene is associated with renal underexcretion type gout. Drug Metab Pharmacokinet. 2014;29(2):208–210. doi: 10.2133/dmpk.DMPK-13-NT-070. [DOI] [PubMed] [Google Scholar]
- 8.Toyoda Y, et al. Genome-wide meta-analysis between renal overload type and renal underexcretion type of clinically defined gout in Japanese populations. Mol Genet Metab, 2022;136(3):186–189. [DOI] [PubMed]
- 9.Patel PI, et al. Fine structure of the human hypoxanthine phosphoribosyltransferase gene. Mol Cell Biol. 1986;6(2):393–403. doi: 10.1128/mcb.6.2.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Puusepp S, et al. Atypical presentation of arts syndrome due to a novel hemizygous loss-of-function variant in the PRPS1 gene. Mol Genet Metab Rep. 2020;25:100677. doi: 10.1016/j.ymgmr.2020.100677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marchitti Satori A , B C, Stagos Dimitrios, Vasiliou Vasilis. Non-P450 aldehyde oxidizing enzymes: the aldehyde dehydrogenase superfamily. Expert Opin Drug Metab Toxicol. 2008;4(6):697–720. doi: 10.1517/17425255.4.6.697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ichida K. What lies behind serum urate concentration? Insights from genetic and genomic studies. Genome Med. 2009. 10.1186/gm118. [DOI] [PMC free article] [PubMed]
- 13.Hagos Y, et al. Human renal organic anion transporter 4 operates as an asymmetric urate transporter. J Am Soc Nephrol. 2007;18(2):430–439. doi: 10.1681/ASN.2006040415. [DOI] [PubMed] [Google Scholar]
- 14.Higashino T, et al. Dysfunctional missense variant of OAT10/SLC22A13 decreases gout risk and serum uric acid levels. Ann Rheum Dis. 2020;79(1):164–166. doi: 10.1136/annrheumdis-2019-216044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wan Rohani WT, et al. Association of solute carrier family 2, member 9 (SLC2A9) genetic variant rs3733591 with gout in a Malay sample set. Med J Malaysia. 2018;73(5):307–310. [PubMed] [Google Scholar]
- 16.Woodward OM, Kottgen A, Kottgen M. ABCG transporters and disease. FEBS J. 2011;278(18):3215–3225. doi: 10.1111/j.1742-4658.2011.08171.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bawa PS, et al. A novel molecular mechanism for a long non-coding RNA PCAT92 implicated in prostate cancer. Oncotarget. 2018;9(65):32419–32434. doi: 10.18632/oncotarget.25940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nigam SK, Bush KT, Bhatnagar V. Drug and toxicant handling by the OAT organic anion transporters in the kidney and other tissues. Nat Clin Pract Nephrol. 2007;3(8):443–448. doi: 10.1038/ncpneph0558. [DOI] [PubMed] [Google Scholar]
- 19.Jutabha P, et al. Human sodium phosphate transporter 4 (hNPT4/SLC17A3) as a common renal secretory pathway for drugs and urate. J Biol Chem. 2010;285(45):35123–35132. doi: 10.1074/jbc.M110.121301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Togawa N, et al. A Na+-phosphate cotransporter homologue (SLC17A4 protein) is an intestinal organic anion exporter. Am J Physiol Cell Physiol. 2012;302(11):C1652–C1660. doi: 10.1152/ajpcell.00015.2012. [DOI] [PubMed] [Google Scholar]
- 21.Toyoda Y, et al. Identification of GLUT12/SLC2A12 as a urate transporter that regulates the blood urate level in hyperuricemia model mice. Proc Natl Acad Sci U S A. 2020;117(31):18175–18177. doi: 10.1073/pnas.2006958117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Prestin K, et al. Regulation of PDZ domain-containing 1 (PDZK1) expression by hepatocyte nuclear factor-1α (HNF1α) in human kidney. Am J Physiol Renal Physiol. 2017;313(4):F973–f983. doi: 10.1152/ajprenal.00650.2016. [DOI] [PubMed] [Google Scholar]
- 23.Ghata J, Cowley BD., Jr Polycystic kidney disease. Compr Physiol. 2017;7(3):945–975. doi: 10.1002/cphy.c160018. [DOI] [PubMed] [Google Scholar]
- 24.Lee MG, et al. Integrative genome-wide association studies of eQTL and GWAS data for gout disease susceptibility. Sci Rep. 2019;9(1):4981. doi: 10.1038/s41598-019-41434-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang C, et al. Mammalian CARMIL inhibits actin filament capping by capping protein. Dev Cell. 2005;9(2):209–221. doi: 10.1016/j.devcel.2005.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wu TH, et al. Tamm-Horsfall Protein is a potent immunomodulatory molecule and a disease biomarker in the urinary system. Molecules. 2018;23(1). 10.3390/molecules23010200. [DOI] [PMC free article] [PubMed]
- 27.Edwards N, et al. A novel homozygous UMOD mutation reveals gene dosage effects on uromodulin processing and urinary excretion. Nephrol Dial Transplant. 2017;32(12):1994–1999. doi: 10.1093/ndt/gfx066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ueda S, Hirata T, Sakasegawa SI. Hypoxanthine-guanine phosphoribosyltransferase is activated via positive cooperativity between guanine and IMP. FEBS Lett. 2022;596(8):1072–1080. doi: 10.1002/1873-3468.14306. [DOI] [PubMed] [Google Scholar]
- 29.Torres RJ, Puig JG. Hypoxanthine-guanine phosophoribosyltransferase (HPRT) deficiency: Lesch-Nyhan syndrome. Orphanet J Rare Dis. 2007;2:48. doi: 10.1186/1750-1172-2-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shields LBE, Peppas DS, Rosenberg E. Xanthine calculi in a patient with Lesch-Nyhan syndrome and factor V Leiden treated with allopurinol: case report. BMC Pediatr. 2018;18(1):231. doi: 10.1186/s12887-018-1197-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nanagiri A, Shabbir N. Lesch Nyhan Syndrome in StatPearls. 2022. StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC.: Treasure Island (FL). [PubMed]
- 32.Nguyen KV. Potential molecular link between the β-amyloid precursor protein (APP) and hypoxanthine-guanine phosphoribosyltransferase (HGprt) enzyme in Lesch-Nyhan disease and cancer. AIMS Neurosci. 2021;8(4):548–557. doi: 10.3934/Neuroscience.2021030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Townsend MH, et al. Overexpression and surface localization of HPRT in prostate cancer provides a potential target for cancer specific antibody mediated cellular cytotoxicity. Exp Cell Res. 2021;403(1):112567. doi: 10.1016/j.yexcr.2021.112567. [DOI] [PubMed] [Google Scholar]
- 34.Guibinga GH, et al. MicroRNA-mediated dysregulation of neural developmental genes in HPRT deficiency: clues for Lesch-Nyhan disease? Hum Mol Genet. 2012;21(3):609–622. doi: 10.1093/hmg/ddr495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu X, et al. Loss-of-function mutations in the PRPS1 gene cause a type of nonsyndromic X-linked sensorineural deafness, DFN2. Am J Hum Genet. 2010;86(1):65–71. doi: 10.1016/j.ajhg.2009.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yang BY, et al. A novel mutation in gene of PRPS1 in a young Chinese woman with X-linked gout: a case report and review of the literature. Clin Rheumatol. 2020;39(3):949–956. doi: 10.1007/s10067-019-04801-0. [DOI] [PubMed] [Google Scholar]
- 37.Rezende Filho FM, et al. PRPS1 gene mutation causes complex X-linked adult-onset cerebellar ataxia in women. Neurol Genet. 2021;7(2):e563. doi: 10.1212/NXG.0000000000000563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zikanova M, et al. Clinical manifestations and molecular aspects of phosphoribosylpyrophosphate synthetase superactivity in females. Rheumatology (Oxford) 2018;57(7):1180–1185. doi: 10.1093/rheumatology/key041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shirakawa S, et al. A Novel PRPS1 Mutation in a Japanese Patient with CMTX5. Intern Med. 2021;61(11):1749–51. [DOI] [PMC free article] [PubMed]
- 40.Charkoftaki G, et al. Transcriptomic analysis and plasma metabolomics in Aldh16a1-null mice reveals a potential role of ALDH16A1 in renal function. Chem Biol Interact. 2017;276:15–22. doi: 10.1016/j.cbi.2017.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Leask MP, Merriman TR. The genetic basis of urate control and gout: Insights into molecular pathogenesis from follow-up study of genome-wide association study loci. Best Pract Res Clin Rheumatol. 2021;35(4):101721. doi: 10.1016/j.berh.2021.101721. [DOI] [PubMed] [Google Scholar]
- 42.Ali Y, et al. Impaired Transport Activity of Human Organic Anion Transporters (OATs) and Organic Anion Transporting Polypeptides (OATPs) by Wnt Inhibitors. J Pharm Sci. 2021;110(2):914–924. doi: 10.1016/j.xphs.2020.10.009. [DOI] [PubMed] [Google Scholar]
- 43.Mirdamadi K, et al. Impact of Th-17 Cytokines on the Regulation of Transporters in Human Placental Explants. Pharmaceutics. 2021;13(6). 10.3390/pharmaceutics13060881. [DOI] [PMC free article] [PubMed]
- 44.Sun HL, et al. Function of Uric Acid Transporters and Their Inhibitors in Hyperuricaemia. Front Pharmacol. 2021;12:667753. doi: 10.3389/fphar.2021.667753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chung S, Kim GH. Urate transporters in the kidney: what clinicians need to know. Electrolyte Blood Press. 2021;19(1):1–9. doi: 10.5049/EBP.2021.19.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nakayama A, et al. Genetic epidemiological analysis of hypouricaemia from 4993 Japanese on non-functional variants of URAT1/SLC22A12 gene. Rheumatology (Oxford) 2022;61(3):1276–1281. doi: 10.1093/rheumatology/keab545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Misawa K, et al. Contribution of rare variants of the SLC22A12 gene to the missing heritability of serum urate levels. Genetics. 2020;214(4):1079–1090. doi: 10.1534/genetics.119.303006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Duong NT, et al. Polymorphisms of ABCG2 and SLC22A12 Genes Associated with Gout Risk in Vietnamese Population. Medicina (Kaunas). 2019;55(1). 10.3390/medicina55010008. [DOI] [PMC free article] [PubMed]
- 49.Nakayama A, et al. Clinical practice guideline for renal hypouricemia (1st edition) Hum Cell. 2019;32(2):83–87. doi: 10.1007/s13577-019-00239-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sakiyama M, et al. The effects of URAT1/SLC22A12 nonfunctional variants, R90H and W258X, on serum uric acid levels and gout/hyperuricemia progression. Sci Rep. 2016;6:20148. doi: 10.1038/srep20148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pavelcova K, et al. Evaluation of the Influence of Genetic Variants of SLC2A9 (GLUT9) and SLC22A12 (URAT1) on the Development of Hyperuricemia and Gout. J Clin Med. 2020;9(8). 10.3390/jcm9082510. [DOI] [PMC free article] [PubMed]
- 52.Zheng Q, et al. Genetic association between SLC22A12 variants and susceptibility to hyperuricemia: a meta-analysis. Genet Test Mol Biomarkers. 2022;26(2):81–95. doi: 10.1089/gtmb.2021.0175. [DOI] [PubMed] [Google Scholar]
- 53.Matsubayashi M, et al. 27-Hydroxycholesterol regulates human SLC22A12 gene expression through estrogen receptor action. Faseb j. 2021;35(1):e21262. doi: 10.1096/fj.202002077R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bahn A, et al. Identification of a new urate and high affinity nicotinate transporter, hOAT10 (SLC22A13) J Biol Chem. 2008;283(24):16332–16341. doi: 10.1074/jbc.M800737200. [DOI] [PubMed] [Google Scholar]
- 55.Mandal AK, et al. Genetic and physiological effects of insulin on human urate homeostasis. Front Physiol. 2021;12:713710. doi: 10.3389/fphys.2021.713710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Toyoda Y, et al. OAT10/SLC22A13 Acts as a renal urate re-absorber: clinico-genetic and functional analyses with pharmacological impacts. Front Pharmacol. 2022;13:842717. doi: 10.3389/fphar.2022.842717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Augustin R, et al. Identification and characterization of human glucose transporter-like protein-9 (GLUT9): alternative splicing alters trafficking. J Biol Chem. 2004;279(16):16229–16236. doi: 10.1074/jbc.M312226200. [DOI] [PubMed] [Google Scholar]
- 58.Auberson M, et al. SLC2A9 (GLUT9) mediates urate reabsorption in the mouse kidney. Pflugers Arch. 2018;470(12):1739–1751. doi: 10.1007/s00424-018-2190-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Windpessl M, et al. a novel homozygous SLC2A9 mutation associated with renal-induced Hypouricemia. Am J Nephrol. 2016;43(4):245–250. doi: 10.1159/000445845. [DOI] [PubMed] [Google Scholar]
- 60.Das Gupta E, et al. Clinical significance of SLC2A9/GLUT9 rs11722228 polymorphisms in gout. Int J Rheum Dis. 2018;21(3):705–709. doi: 10.1111/1756-185X.12918. [DOI] [PubMed] [Google Scholar]
- 61.Zhang W, et al. Effects of genetic and nongenetic factors on hyperuricemia in Chinese patients with coronary artery disease. Pharmacogenomics. 2021;22(13):821–831. doi: 10.2217/pgs-2021-0053. [DOI] [PubMed] [Google Scholar]
- 62.Lee YH, et al. Associations between SLC2A9 polymorphisms and gout susceptibility : a meta-analysis. Z Rheumatol. 2017;76(1):64–70. doi: 10.1007/s00393-016-0070-x. [DOI] [PubMed] [Google Scholar]
- 63.Chen Y, et al. Genetic risk of hyperuricemia in hypertensive patients associated with antihypertensive drug therapy: a longitudinal study. Clin Genet. 2022;101(4):411–420. doi: 10.1111/cge.14110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang Z, et al. E4BP4 regulates hepatic solute carrier family 2 member 9 and uric acid disposition in mice. Drug Metab Dispos. 2022;50(5):591–599. doi: 10.1124/dmd.121.000790. [DOI] [PubMed] [Google Scholar]
- 65.Nigam SK, Bhatnagar V. The systems biology of uric acid transporters: the role of remote sensing and signaling. Curr Opin Nephrol Hypertens. 2018;27(4):305–313. doi: 10.1097/MNH.0000000000000427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Huls M, et al. The breast cancer resistance protein transporter ABCG2 is expressed in the human kidney proximal tubule apical membrane. Kidney Int. 2008;73(2):220–225. doi: 10.1038/sj.ki.5002645. [DOI] [PubMed] [Google Scholar]
- 67.Kerr ID, et al. Mammalian ABCG-transporters, sterols and lipids: To bind perchance to transport? Biochim Biophys Acta Mol Cell Biol Lipids. 2021;1866(3):158860. doi: 10.1016/j.bbalip.2020.158860. [DOI] [PubMed] [Google Scholar]
- 68.Toyoda Y, et al. Functional Characterization of Clinically-Relevant Rare Variants in ABCG2 Identified in a Gout and Hyperuricemia Cohort. Cells. 2019. 8(4). 10.1016/j.bbalip.2020.158860. [DOI] [PMC free article] [PubMed]
- 69.Hoque KM, et al. The ABCG2 Q141K hyperuricemia and gout associated variant illuminates the physiology of human urate excretion. Nat Commun. 2020;11(1):2767. doi: 10.1038/s41467-020-16525-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Son CN, et al. ABCG2 polymorphism is associated with hyperuricemia in a study of a community-based korean cohort. J Korean Med Sci. 2017;32(9):1451–1459. doi: 10.1038/s41467-020-16525-w.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Toyoda Y, et al. Familial early-onset hyperuricemia and gout associated with a newly identified dysfunctional variant in urate transporter ABCG2. Arthritis Res Ther. 2019;21(1):219. doi: 10.1186/s13075-019-2007-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Stiburkova B, et al. Functional non-synonymous variants of ABCG2 and gout risk. Rheumatology (Oxford) 2017;56(11):1982–1992. doi: 10.1093/rheumatology/kex295. [DOI] [PubMed] [Google Scholar]
- 73.Fujita K, Ichida K. ABCG2 as a therapeutic target candidate for gout. Expert Opin Ther Targets. 2018;22(2):123–129. doi: 10.1080/14728222.2018.1420167. [DOI] [PubMed] [Google Scholar]
- 74.Kawaguchi M, et al. Both variants of A1CF and BAZ1B genes are associated with gout susceptibility: a replication study and meta-analysis in a Japanese population. Hum Cell. 2021;34(2):293–299. doi: 10.1007/s13577-021-00485-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chen ZS, Tiwari AK. Multidrug resistance proteins (MRPs/ABCCs) in cancer chemotherapy and genetic diseases. FEBS J. 2011;278(18):3226–3245. doi: 10.1111/j.1742-4658.2011.08235.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Slot AJ, Molinski SV, Cole SP. Mammalian multidrug-resistance proteins (MRPs) Essays Biochem. 2011;50(1):179–207. doi: 10.1042/bse0500179. [DOI] [PubMed] [Google Scholar]
- 77.Wang Z, et al. The effect of polymorphism of uric acid transporters on uric acid transport. J Nephrol. 2019;32(2):177–187. doi: 10.1007/s40620-018-0546-7. [DOI] [PubMed] [Google Scholar]
- 78.Markova SM, Kroetz DL. ABCC4 is regulated by microRNA-124a and microRNA-506. Biochem Pharmacol. 2014;87(3):515–522. doi: 10.1016/j.bcp.2013.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tanner C, et al. Population-specific resequencing associates the ATP-binding cassette subfamily C Member 4 gene with gout in New Zealand Maori and Pacific men. Arthritis Rheumatol. 2017;69(7):1461–1469. doi: 10.1002/art.40110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Burckhardt BC, Burckhardt G. Transport of organic anions across the basolateral membrane of proximal tubule cells. Rev Physiol Biochem Pharmacol. 2003;146:95–158. doi: 10.1007/s10254-002-0003-8. [DOI] [PubMed] [Google Scholar]
- 81.Saji T, et al. Transcriptional regulation of human and mouse organic anion transporter 1 by hepatocyte nuclear factor 1 alpha/beta. J Pharmacol Exp Ther. 2008;324(2):784–790. doi: 10.1124/jpet.107.128249. [DOI] [PubMed] [Google Scholar]
- 82.Euteneuer AM, et al. Estrogen receptor α (ERα) indirectly induces transcription of human renal organic anion transporter 1 (OAT1) Physiol Rep. 2019;7(21):e14229. doi: 10.14814/phy2.14229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ogasawara K, et al. Human organic anion transporter 3 gene is regulated constitutively and inducibly via a cAMP-response element. J Pharmacol Exp Ther. 2006;319(1):317–322. doi: 10.1124/jpet.106.108233. [DOI] [PubMed] [Google Scholar]
- 84.Tan PK, et al. Discovery and characterization of verinurad, a potent and specific inhibitor of URAT1 for the treatment of hyperuricemia and gout. Sci Rep. 2017;7(1):665. doi: 10.1038/s41598-017-00706-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Han S. Hypouricemic Effects of Extracts from Urtica hyperborea Jacq. ex Wedd. in Hyperuricemia Mice through XOD, URAT1, and OAT1. Biomed Res Int. 2020;2020:2968135. doi: 10.1155/2020/2968135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Huang L, et al. The anti-hyperuricemic effect of four astilbin stereoisomers in Smilax glabra on hyperuricemic mice. J Ethnopharmacol. 2019;238:111777. doi: 10.1016/j.jep.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 87.Reimer RJ, Edwards RH. Organic anion transport is the primary function of the SLC17/type I phosphate transporter family. Pflugers Arch. 2004;447(5):629–635. doi: 10.1007/s00424-003-1087-y. [DOI] [PubMed] [Google Scholar]
- 88.Butler F, Alghubayshi A, and Roman Y. The Epidemiology and Genetics of Hyperuricemia and Gout across Major Racial Groups: A Literature Review and Population Genetics Secondary Database Analysis. J Pers Med. 2021;11(3):629–35. [DOI] [PMC free article] [PubMed]
- 89.Ketharnathan S, et al. A non-coding genetic variant maximally associated with serum urate levels is functionally linked to HNF4A-dependent PDZK1 expression. Hum Mol Genet. 2018;27(22):3964–3973. doi: 10.1093/hmg/ddy295. [DOI] [PubMed] [Google Scholar]
- 90.Qi Y, et al. Long noncoding RNA PENG upregulates PDZK1 expression by sponging miR-15b to suppress clear cell renal cell carcinoma cell proliferation. Oncogene. 2020;39(22):3964–73. doi: 10.1038/s41388-020-1297-1. [DOI] [PubMed] [Google Scholar]
- 91.Narang RK, et al. Interactions between serum urate-associated genetic variants and sex on gout risk: analysis of the UK Biobank. Arthritis Res Ther. 2019;21(1):13. doi: 10.1186/s13075-018-1787-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hardy E, Tsiokas L. Polycystins as components of large multiprotein complexes of polycystin interactors. Cell Signal. 2020;72:109640. doi: 10.1016/j.cellsig.2020.109640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Koulen P, et al. Polycystin-2 is an intracellular calcium release channel. Nat Cell Biol. 2002;4(3):191–197. doi: 10.1038/ncb754. [DOI] [PubMed] [Google Scholar]
- 94.Dong Z, et al. Epistatic interaction between PKD2 and ABCG2 influences the pathogenesis of hyperuricemia and gout. Hereditas. 2020;157(1):2. doi: 10.1186/s41065-020-0116-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Yang HJ, et al. The haplotype of SLC2A9_rs3733591, PKD2_rs2725220 and ABCG2_rs2231142 increases the hyperuricaemia risk and alcohol, chicken and processed meat intakes and smoking interact with its risk. Int J Food Sci Nutr. 2021;72(3):391–401. doi: 10.1080/09637486.2020.1807474. [DOI] [PubMed] [Google Scholar]
- 96.Chen CJ, et al. ABCG2 contributes to the development of gout and hyperuricemia in a genome-wide association study. Sci Rep. 2018;8(1):3137. doi: 10.1038/s41598-018-21425-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Futagi Y, et al. Molecular characterization of the orphan transporter SLC16A9, an extracellular pH- and Na(+)-sensitive creatine transporter. Biochem Biophys Res Commun. 2020;522(2):539–544. doi: 10.1016/j.bbrc.2019.11.137. [DOI] [PubMed] [Google Scholar]
- 98.Huang XF, et al. Whole-exome sequencing reveals a rare missense variant in SLC16A9 in a pedigree with early-onset gout. Biomed Res Int. 2020;2020:4321419. doi: 10.1155/2020/4321419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Nakayama A, et al. Common missense variant of monocarboxylate transporter 9 (MCT9/SLC16A9) gene is associated with renal overload gout, but not with all gout susceptibility. Hum Cell. 2013;26(4):133–136. doi: 10.1007/s13577-013-0073-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sakiyama M, et al. Common variant of leucine-rich repeat-containing 16A (LRRC16A) gene is associated with gout susceptibility. Hum Cell. 2014;27(1):1–4. doi: 10.1007/s13577-013-0081-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Gonzalez-Aramburu I, et al. Genetic variability related to serum uric acid concentration and risk of Parkinson's disease. Mov Disord. 2013;28(12):1737–1740. doi: 10.1002/mds.25507. [DOI] [PubMed] [Google Scholar]
- 102.Leask M, et al. Functional urate-associated genetic variants influence expression of lincRNAs LINC01229 and MAFTRR. Front Genet. 2018;9:733. doi: 10.3389/fgene.2018.00733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Daassi D, et al. Differential expression patterns of MafB and c-Maf in macrophages in vivo and in vitro. Biochem Biophys Res Commun. 2016;473(1):118–124. doi: 10.1016/j.bbrc.2016.03.063. [DOI] [PubMed] [Google Scholar]
- 104.Higashino T, et al. A common variant of MAF/c-MAF, transcriptional factor gene in the kidney, is associated with gout susceptibility. Hum Cell. 2018;31(1):10–13. doi: 10.1007/s13577-017-0186-6. [DOI] [PubMed] [Google Scholar]
- 105.Srivastava R, et al. An intricate network of conserved DNA upstream motifs and associated transcription factors regulate the expression of uromodulin gene. J Urol. 2014;192(3):981–989. doi: 10.1016/j.juro.2014.02.095. [DOI] [PubMed] [Google Scholar]
- 106.Takemasa Y, et al. Familial juvenile hyperuricemia in early childhood in a boy with a novel gene mutation. CEN Case Rep. 2021;10(3):426–430. doi: 10.1007/s13730-020-00566-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ayasreh N, et al. Autosomal dominant tubulointerstitial kidney disease: clinical presentation of patients with ADTKD-UMOD and ADTKD-MUC1. Am J Kidney Dis. 2018;72(3):411–418. doi: 10.1053/j.ajkd.2018.03.019. [DOI] [PubMed] [Google Scholar]
- 108.Yang J, Zhang Y, Zhou J. UMOD gene mutations in Chinese patients with autosomal dominant tubulointerstitial kidney disease: a pediatric case report and literature review. BMC Pediatr. 2019;19(1):145. doi: 10.1186/s12887-019-1522-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lopes L.B, et al. Identification of a novel UMOD mutation (c.163G>A) in a Brazilian family with autosomal dominant tubulointerstitial kidney disease. Braz J Med Biol Res. 2018;51(3):e6560. doi: 10.1590/1414-431x20176560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Yang Y, et al. Elevated UMOD methylation level in peripheral blood is associated with gout risk. Sci Rep. 2017;7(1):11196. doi: 10.1038/s41598-017-11627-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Liu YR, et al. Risk of gout among Taiwanese adults with ALDH-2 rs671 polymorphism according to BMI and alcohol intake. Arthritis Res Ther. 2021;23(1):115. doi: 10.1186/s13075-021-02497-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kelley, B.I.t.-i.F.a.W.N., Studies on the Mechanism of Fructose-induced Hyperuricemia in Man. Metabolism, 1972. 21(8). [DOI] [PubMed]
- 113.Ma Q, et al. Association between lncRNA and GCKR gene in type 2 diabetes mellitus. Clin Chim Acta. 2020;501:66–71. doi: 10.1016/j.cca.2019.10.004. [DOI] [PubMed] [Google Scholar]
- 114.Sandoval-Plata G, Morgan K, Abhishek A. Variants in urate transporters, ADH1B, GCKR and MEPE genes associate with transition from asymptomatic hyperuricaemia to gout: results of the first gout versus asymptomatic hyperuricaemia GWAS in Caucasians using data from the UK Biobank. Ann Rheum Dis. 2021;80(9):1220–1226. doi: 10.1136/annrheumdis-2020-219796. [DOI] [PubMed] [Google Scholar]
- 115.Hutton J, et al. Mediation analysis to understand genetic relationships between habitual coffee intake and gout. Arthritis Res Ther. 2018;20(1):135. doi: 10.1186/s13075-018-1629-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Rasheed H, et al. Interaction of the GCKR and A1CF loci with alcohol consumption to influence the risk of gout. Arthritis Res Ther. 2017;19(1):161. doi: 10.1186/s13075-017-1369-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.