FIGURE 1.
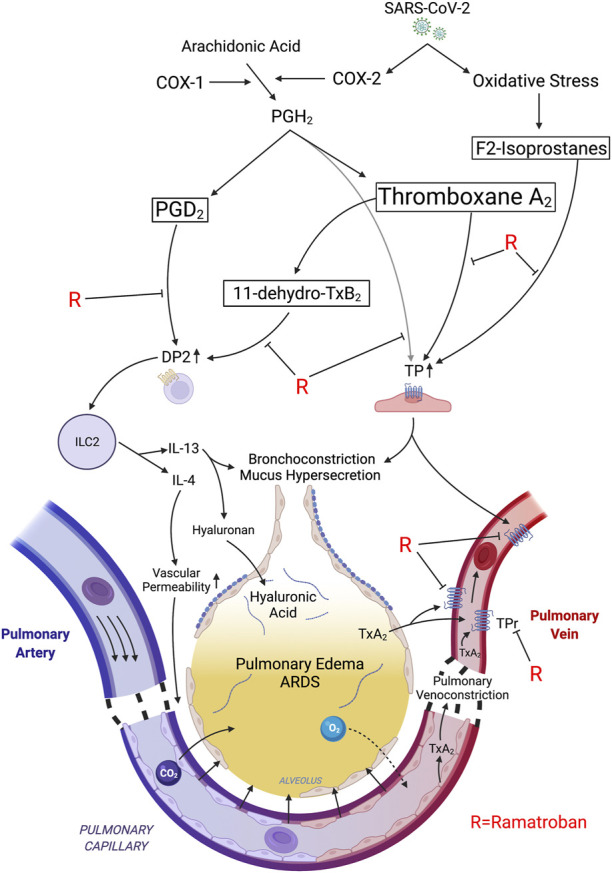
Proposed mechanisms of rapid relief in respiratory distress following ramatroban administration during acute SARS-CoV-2 infection. SARS-CoV-2 induced expression of COX-2 generates PGH2 which is converted into thromboxane A2 >> PGD2. Oxidative stress-associated free radicals initiate nonenzymatic peroxidation of arachidonic acid leading to F2-isoprostane generation. PGH2, TxA2, and F2-isoprostanes stimulate thromboxane prostanoid receptors (TP). TP stimulation induces pulmonary venoconstriction leading to an increase in transcapillary pressure in pulmonary microvasculature, and transudation of fluid into the alveoli, thereby causing impaired gas exchange and ARDS. The TxA2/TP axis also induces bronchoconstriction and mucus secretion. TxA2 is rapidly converted to 11-dehydro-TxB2 in the lungs. PGD2 and 11-dehydro-TxB2 stimulate the DP2 receptor on Th2 and ILC2 cells leading to release of type 2 cytokines, IL-4 and IL-13. Both TP activation and IL-4 promote vascular permeability thereby exacerbating fluid transudation, while IL-13 induces hyaluronic acid accumulation and mucus hypersecretion. Ramatroban inhibits the DP2 and TP receptors, thereby promoting pulmonary vasorelaxation and bronchorelaxation and improving capillary barrier function, while attenuating the maladaptive type 2 immune response and mucus secretion, thereby alleviating pulmonary edema and ARDS. Tx, thromboxane; PG, prostaglandin; TP, thromboxane prostanoid receptor; DP2; D-prostanoid receptor 2; Th2; T helper 2; ILC2; innate lymphoid class.
