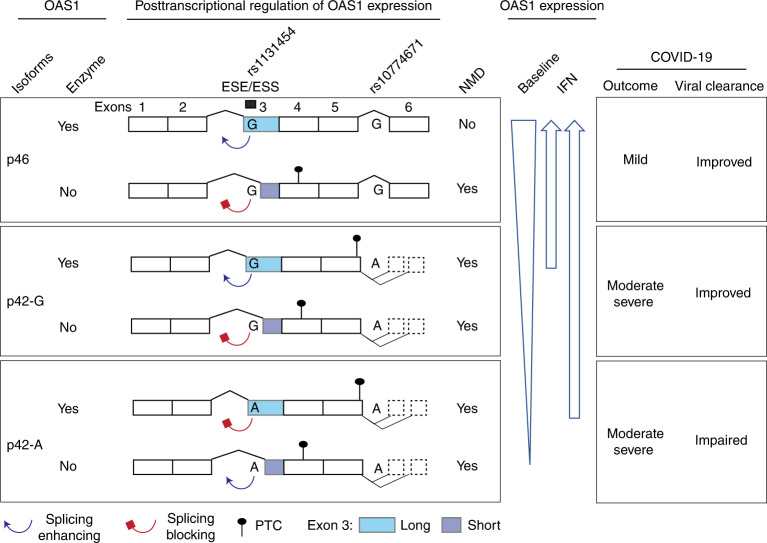
Fig. 8. Proposed model for mechanisms underlying association between OAS1 genetic variants and COVID-19 outcomes.
Two OAS1 variants, the splice site variant (rs10774671-A/G) and exon 3 missense variant (rs1131454-A/G, Gly162Ser), determine the structure and expression levels of OAS1 isoforms. Alleles of the splicing variant rs10774671 define the OAS1 isoforms OAS1-p42 (A allele) and OAS1-p46 (G allele). Alleles of rs1131454 create an ESE/ESS for splicing of the canonical/long versus alternative/short exon 3. Transcripts with short exon 3 are terminated by PTCs within exon 4 and efficiently targeted by NMD. The stop codon for OAS1-p42 is located within exon 5, followed by several additional exons creating OAS1-p44 and OAS1-p48 isoforms, making this stop codon a PTC. Thus, OAS1-p42 is also targeted by NMD, albeit less efficiently than transcripts with PTCs in exon 4. The combined splicing effects of rs10774671, which creates alternative OAS1 isoforms, and rs1131454, which regulates the inclusion of short or long exon 3 and thus the introduction of additional PTCs, result in variable degradation of OAS1 transcripts by NMD. At baseline, the expression is highest for OAS1-p46 and the lowest for OAS1-p42-A. However, treatment with interferons may compensate for NMD, allowing OAS1-p42 protein to reach expression levels comparable to OAS1-p46. Thus, the effects of genetic variants on OAS1 expression can be compensated by IFN treatment to overcome impaired viral clearance and prevent progression to severe COVID-19 requiring hospitalization.