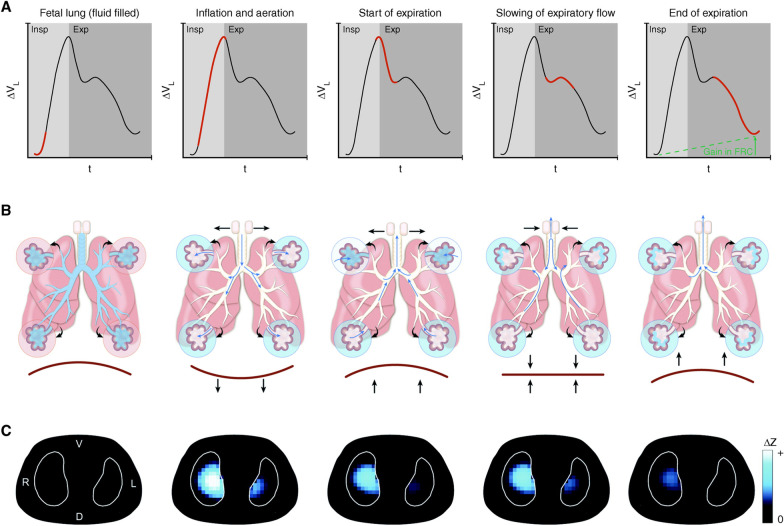
Fig. 8.
Five phases of a newborn infant transitioning from a collapsed fluid-filled state to full aeration. A Lung volume/time curve representing a single ‘cry’ during inspiration (Insp) and expiration (Exp). B Diagram of airways and acini. C Electrical impedance tomography (EIT) images. (1) Fetal lung (fluid filled): The beginning of the newborn’s first inspiration (red line) with the lung still collapsed and fluid filled (blue in airways) and no gas in the lung measured with EIT (no blue). (2) Inflation and aeration: A rapid inspiration (red line) with the glottis fully open (horizontal arrows pointing out) and contraction of the diaphragm (downward arrows) as the newborn rapidly fills the lung with gas to begin a cry. This high velocity inflow of air moves liquid in the airways and alveoli (blue changing to white) into the interstitial space (small blue arrows). EIT shows gas entering the lung (light blue). (3) Start of expiration: Expiration is active with diaphragm contraction (arrows) forcing gas rapidly out of the lungs (red steep slope, volume/time curve). Intra-alveolar pressure falls, allowing fluid to refill into some alveoli (upper alveoli going from white to blue) and EIT shows a loss of lung volume. (4) Slowing of expiratory flow: To prevent further lung collapse and flooding, the glottis briefly ‘brakes’ expiratory gas flow (horizontal arrows pointing inward), re-pressurizing the lungs. Pendelluft (blue arrows) redistributes gas into partially flooded alveoli. (5) End of expiration: The remainder of expiration (red line on volume/time curve) occurs with a partially closed glottis to maintain a PEEP to preserve FRC. EIT demonstrates that FRC is preserved (blue areas). Thus, the newborn uses a rapid inspiration to open flooded tissue and partially closes the glottis as a brake to prevent re-collapse and flooding. This method of rapid inspiration to open lung and closing the glottis to ‘brake’ expiratory flow and maintain airway pressure to prevent re-collapse ratchets open small volumes of lung tissue with each breath until the lung is fully inflated. The TCAV method uses a similar ratchet approach to open collapsed and fluid-filled lung of the ARDS patient. When expiratory flow is terminated (Fig. 4B, Gas Flow/Time curve, red arrowhead), the lung is rapidly re-inflated until the set CPAP Phase pressure is reached. This is analogous to the rapid inspiration before a cry in the newborn (Inflation and aeration). The brief Release Phase (0.2–0.5 s) acts as an expiratory ‘brake’ (Fig. 4B, red arrowhead), which does not allow the lung to depressurize, maintaining a time-controlled PEEP (Fig. 4B, TC-PEEP). This is similar to the newborn using the glottis as a ‘brake’ to slow expiratory flow (Slowing of expiratory flow). To summarize, both the newborn and the TCAV method use a rapid inspiration to open a small volume of lung with each breath. A ‘brake’ in expiratory flow is used to prevent re-collapse. Combined this ratchet approach opens small volumes with each breath and over time fully recruits the collapsed lung