Abstract
Introduction
Oral and maxillofacial injuries can be defined as injuries involving soft and hard tissue structures of the facial region and oral cavity, including the teeth and vital structures of the head and neck area as a result of trauma. The maxillofacial injuries are multifactorial and vary from one country to another and even from region to region. Despite, societal restrictions imposed by the government in the form of lockdowns and curfews, patients still experienced trauma and required significant healthcare services for management.
Methods
Patients of either gender reporting to the emergency department of Lata Mangeshkar Hospital with maxillofacial injuries, attended by residents of OMFS from October 2019 to August 2020 were included in the retrospective study. The demographic data about age, gender and status pertaining to under the influence of alcohol was recorded. The aim of this retrospective study was to evaluate the changing patterns of the maxillofacial injuries during the Covid-19 pandemic.
Results
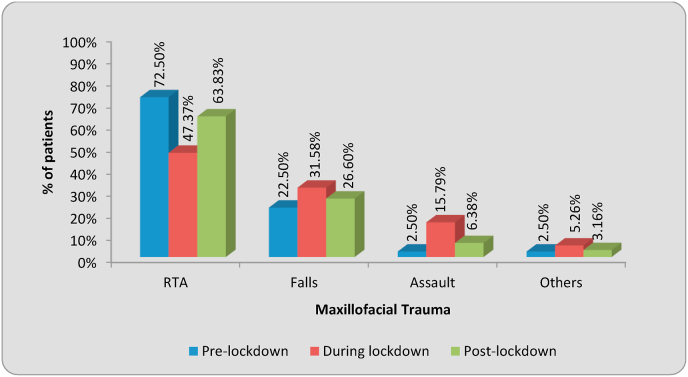
In the present study, the road traffic accidents were 72.50% pre-lockdown which reduced to 47.37% during the alcohol ban and nationwide lockdown and gradually increased to 63.83% post-lockdown. The second most common cause of maxillofacial injury was falls which showed a significant increase from 22.50% before the lockdown to 31.58% during the lockdown and decreased to 26.6% after lockdown during the pandemic. There was an increase in the number of assaults from 2.50% pre-lockdown to 15.79% during the lockdown and again a decrease to 6.38% post-lockdown.
Discussion
Our study demonstrates the impact of nationwide lockdown in the month of April and May 2020, may have an association with the significant statistical decrease in the monthly average number of trauma admissions. There was a significant decrease in the number of road traffic collisions and falls during the “lockdown period”.
Conclusion
The etiology and pattern of maxillofacial injuries reflect the trauma pattern within the community. We need more coordinated strategies of action to minimize maxillofacial injuries and its implication on physical and psychological wellbeing of patients.
Keywords: Changing patterns, Maxillofacial trauma, Etiology, COVID-19
1. Introduction
The latest infectious disease that has rapidly spread worldwide was caused by novel coronavirus strain in 2019 called COVID-19. It was not until the mid of March 2020 when an alarming situation was witnessed in India with a tremendous rise in patients of COVID-19. The rise in infection lead to a total lockdown imposed by the Government of India with closure of all commercial activities and restricting modes of transportation1. Oral and maxillofacial injuries can be defined as injuries involving soft and hard tissue structures of the facial region and oral cavity, including the teeth and vital structures of the head and neck area as a result of trauma2. The prominence of the face makes it prone to injuries due to fall. In cases of interpersonal violence or altercations the face is usually the target for injuries. The maxillofacial injuries are multifactorial and vary from one country to another and even from region to region. This change in etiology of maxillofacial injuries depends on the prevailing socio economic, cultural, and environmental factors. The cause of oral maxillofacial injuries has changed over the four decades and it continues to do so3.
The most common causes of maxillofacial injuries are road traffic accidents (RTAs) or vehicle motor accidents (VMAs), assaults, domestic abuse, falls, occupational trauma, sports injuries, and injuries to face due to seizures etc4. The major contribution to interpersonal violence (IPV) and motor vehicle accidents is consumption of alcohol that results in impaired judgement and inappropriate behavior5.
The outbreak of Corona virus disease 2019 (COVID-19) has made the Oral and Maxillofacial Surgical branch to adapt and modify to this global pandemic6. The COVID-19 pandemic has disrupted essential health services undoubtedly. Despite, societal restrictions imposed by the government in the form of lockdowns and curfews, patients still experienced trauma and required significant healthcare services for management.
With the reference to above context, the present study was undertaken to analyze the changing patterns in etiology of Oral & Maxillofacial cases before and during the COVID-19 pandemic. The objective of the study was to compare the etiological patterns with the recorded data of the patients reporting to the emergency department before and during the government-imposed lockdown. The primary hypothesis was that the government restrictions imposed during the pandemic would result in fewer trauma cases. The alternate hypothesis was that admissions due to assault may show a significant increase.
2. Methods
A comparative, retrospective study was conducted using the archived data of maxillofacial injury cases before and during the lockdown period. The study was conducted after approval from the Institutional Ethics Committee Reference no. IEC/VSPMDCRC/20/2020 and Institution Ethics Committee no. ECR/885/Inst/MH/2017.
The emergency department was selected by purposive sampling in order to secure maximum number of patients with maxillofacial injuries. Patients of either gender reporting to the emergency department of Lata Mangeshkar Hospital with maxillofacial injuries, attended by residents of OMFS from October 2019 to August 2020 were included in the retrospective study. The study was divided into two groups. Control Group (Group A) consisted of patients reporting to the emergency department of LMH from October 1, 2019 to March 15, 2020 while the Study group (Group B and C) consisted of patients from 16th March to August 31, 2020 (This included Pre-Lockdown Phase 1, Lockdown Phase 1–4 and Unlock 1.0–3.0)
Pre-Lockdown Phase 1 was from 16th March to 24th March which included Janta curfew imposed by government.
The Study group B included the months with
Phase 1: March 25, 2020–April 14, 2020 (21 days)
Phase 2: April 15, 2020–May 3, 2020 (19 days)
Phase 3: May 4, 2020–May 17, 2020 (14 days)
Phase 4: May 18, 2020–May 31, 2020 (14 days)
While the Group C included Unlock Phase:
Unlock 1.0: June 1, 2020–June 30, 2020 (30 days)
Unlock 2.0: July 1, 2020–July 31, 2020 (31 days)
Unlock 3.0: August 1, 2020–August 31, 2020 (31 days)
The demographic data about age, gender and status pertaining to under the influence of alcohol was recorded. A detailed history of the event causing maxillofacial injury was documented for each patient under the influence of alcohol or not. The history was either taken from the relative or the person who witnessed the injury if the patient was not in a condition to recall the events. These patients were referred to Oral and Maxillofacial Surgeons after the management of head injuries, if any. Patients with soft tissue injuries were managed either conservatively by placement of medicated dressings or by suturing the contused lacerated wounds followed by anti-biotic and analgesic coverage. The patients with suspected hard tissue injuries were followed with investigations, admitted if required and underwent Open Reduction with Internal Fixation (ORIF) under general or local anaesthesia.
The aim of this retrospective study was to evaluate the change in etiology of the maxillofacial injuries. Hence, we have collected the data spanning of equal months before and during this global pandemic. Patients were not given any sort of financial compensation to be a part of this study.
3. Results
The statistical analysis was done using descriptive and inferential statistics using chi square test and z-test for difference between single proportion and software used in the analysis were SPSS 27.0 version and GraphPad Prism 7.0 version, p < 0.05 is considered as level of significance and z > 1.96 is considered as significant.
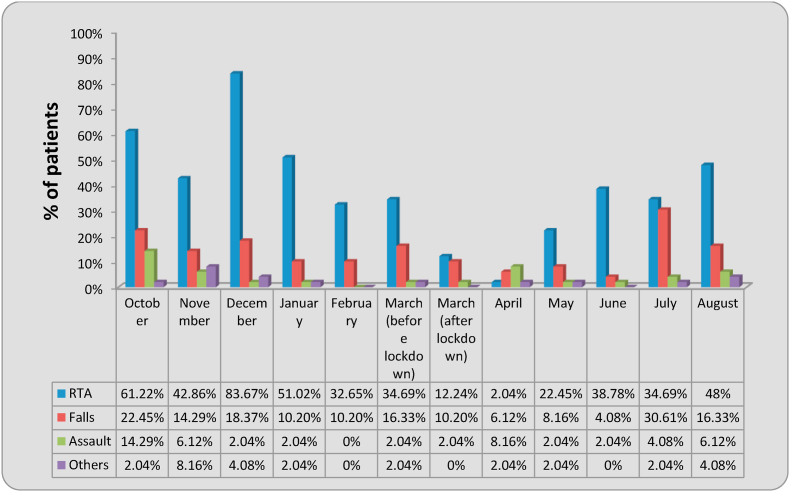
In the present study, a total of 349 cases were evaluated, out of which 283 were male and 66 were female. This clearly shows a male predilection towards maxillofacial trauma. The road traffic accidents were 72.50% in Group A which reduced to 47.37% in Group B which saw the nationwide lockdown imposed by the government and gradually increased to 63.83% in Group C during the Unlock Phase 1.0–3.0. The second most common cause of maxillofacial injury were falls which showed a significant increase from 22.50% in Group A to 31.58% in Group B and decreased to 26.6% in Group C. There was an increase in the number of assaults from 2.50% in Group A to 15.79% in Group B and again a decrease to 6.38% in Group C. In our study, the p value was 0.0001, which is significant thereby proving there was a significant change in etiology of maxillofacial trauma before and during the different Phases as shown in Table 1, Table 2, Table 3, Table 4 and Graph 1, Graph 2, Graph 3, Graph 4.
Table 1.
Month wise distribution of Maxillofacial Trauma.
| Maxillofacial trauma | RTA | Falls | Assault | Others | Total |
|---|---|---|---|---|---|
| October | 30(61.22%) | 11(22.45%) | 7(14.29%) | 1(2.04%) | 49 |
| November | 21(42.86%) | 7(14.29%) | 3(6.12%) | 4(8.16%) | 49 |
| December | 41(83.67%) | 9(18.37%) | 1(2.04%) | 2(4.08%) | 49 |
| January | 25(51.02%) | 5(10.20%) | 1(2.04%) | 1(2.04%) | 49 |
| February | 16(32.65%) | 5(10.20%) | 0(0%) | 0(0%) | 49 |
| March (before lockdown) | 17(34.69%) | 8(16.33%) | 1(2.04%) | 1(2.04%) | 49 |
| March (after lockdown) | 6(12.24%) | 5(10.20%) | 1(2.04%) | 0(0%) | 49 |
| April | 1(2.04%) | 3(6.12%) | 4(8.16%) | 1(2.04%) | 49 |
| May | 11(22.45%) | 4(8.16%) | 1(2.04%) | 1(2.04%) | 49 |
| June | 19(38.78%) | 2(4.08%) | 1(2.04%) | 0(0%) | 49 |
| July | 17(34.69%) | 15(30.61%) | 2(4.08%) | 1(2.04%) | 49 |
| August | 24(48%) | 8(16.33%) | 3(6.12%) | 2(4.08%) | 49 |
| χ2-value | 57.54, p-value = 0.0001, Significant | ||||
Table 2.
Distribution of cases at pre-lockdown, during lockdown and post-lockdown.
| RTA | Falls | Assault | Others | Total | χ2-value | |
|---|---|---|---|---|---|---|
| Pre-lockdown | 58(72.50%) | 18(22.50%) | 2(2.50%) | 2(2.50%) | 80 | |
| During lockdown | 8(47.37%) | 12(31.58%) | 6(15.79%) | 2(5.26%) | 38 | 10.65 p = 0.013,S |
| Post-lockdown | 60(63.83%) | 25(26.60%) | 6(6.38%) | 3(3.16%) | 94 | 21.43 p = 0.0003,S |
Table 3.
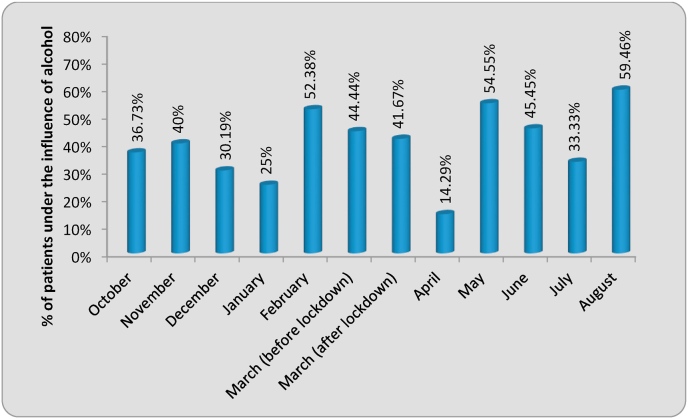
Month wise distribution of maxillofacial trauma cases who underwent under the influence of alcohol.
| Maxillofacial trauma | Total cases | Under the influence of alcohol | Percentage | z-value |
|---|---|---|---|---|
| October | 49 | 18 | 36.73 | 5.33,S |
| November | 35 | 14 | 40.00 | 4.83,S |
| December | 53 | 16 | 30.19 | 4.79,S |
| January | 32 | 8 | 25.00 | 3.27,S |
| February | 21 | 11 | 52.38 | 4.81,S |
| March (before lockdown) | 27 | 12 | 44.44 | 4.65,S |
| March (after lockdown) | 12 | 5 | 41.67 | 2.93,S |
| April | 7 | 1 | 14.29 | 1.08,NS |
| May | 11 | 6 | 54.55 | 3.63,S |
| June | 22 | 10 | 45.45 | 4.28,S |
| July | 36 | 12 | 33.33 | 4.24,S |
| August | 37 | 22 | 59.46 | 7.37,S |
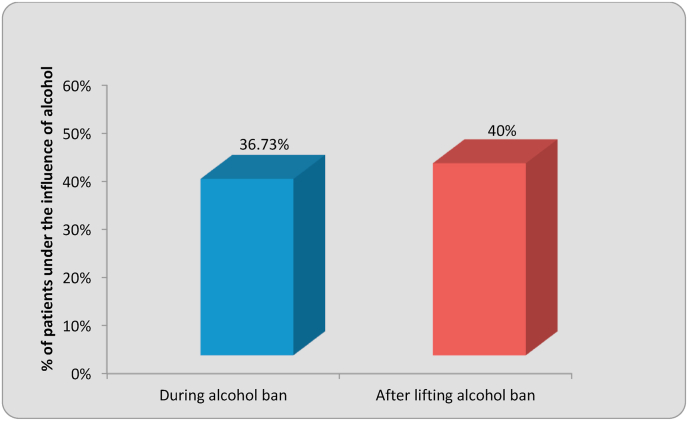
Table 4.
Distribution of cases under the influence of alcohol during and after lifting alcohol ban.
| Total cases | Under the influence of alcohol | Percentage | z-value | |
|---|---|---|---|---|
| During alcohol ban | 19 | 6 | 36.73 | 5.33,S |
| After lifting alcohol ban | 33 | 16 | 40 | 4.83,S |
Graph 1.
Month wise distribution of Maxillofacial Trauma.
Graph 2.
Distribution of cases at pre-lockdown, during lockdown and post-lockdown.
Graph 3.
Month wise distribution of maxillofacial trauma cases who underwent under the influence of alcohol.
Graph 4.
Distribution of cases under the influence of alcohol during and after lifting alcohol ban Statistical analysis was done by using descriptive and inferential statistics using chisquare test and z-test for difference between single proportion and software used in the analysis were SPSS 27.0 version and GraphPad Prism 7.0 version, p < 0.05 is considered as level of significance and z > 1.96 is considered as significant.
4. Discussion
With fewer people on the streets and the closure of restaurants and bars serving alcohol, the factors mostly associated with the altercations were significantly affected. Evaluating the factors involved in the etiologies of violent injuries involving the maxillofacial region enables the surgeon to approach service provision, resource allocation and emergency management in a comprehensive manner7.
Interpersonal violence (IPV) as a proportion of total maxillofacial trauma increased during the COVID-19 pandemic as observed in our study. Restrictions imposed by the government from mid-March 2020 to May 2020 have had an impact of paramount on the volume of maxillofacial injuries seen. Greater police presence on the streets with a ban on larger gatherings and curfews may have had a significant contribution in reduction of road traffic accidents and vehicle motor accidents at our center. However, household confinement during the months mid-March to May 2020 may have contributed to a significant increase in IPV in the form of domestic violence as observed in our study. With our present retrospective study, our department has noted fewer maxillofacial injuries arising on the street but, sudden societal restrictions may have pushed violence behind closed doors and domestic violence rose during the lockdown period.
RTAs are the main causative factor for maxillofacial trauma which accounts for approximately 68–73% in India which is confirmed by various studies8,9. Our study demonstrates the impact of nationwide lockdown in the month of April and May 2020, may have an association with the significant statistical decrease in the monthly average number of trauma admissions. There was a significant decrease in the number of road traffic collisions and falls during the ‘lockdown period’.
Maxillofacial injuries are more predominant in men than in women10. The least affected age group was above 60 years of age. The age group most prone to maxillofacial trauma was 21–30 years as they acquire social characteristics, that is, the beginning of working life, legal permission to drive cars and motorcycles and consumption of alcohol legally from 25 years of age. The road safety measures such as stringent use of seat belts and helmets, road traffic law enforcement and other traffic calming measures have played a significant role in reduction of road traffic accidents in developed countries. In a developing nation like India, traffic calming measures have also contributed to a greater extent, however the lack of discipline by a small section of people does contribute to RTAs. Given the large population burden of India, this extrapolates into a significant number. The causative factor generally recognized in the literature documented is alcohol which plays a prominent contributing factor in altercations and road traffic accidents. The male to female ratio in the study was found to be 4:1, lower as compared to other studies. This male predominance observed in the study can be related to the fact that young males are more prone to maxillofacial injuries due to contact sports, alcohol abuse and vehicular travel and IPV.
Various studies have shown that interpersonal violence is the most common etiology for maxillofacial injury in developing countries whereas RTAs are the most common etiology for maxillofacial trauma in developed countries11. It is well documented in the current literature that an increase in 40–50% cases of domestic violence was witnessed it Brazil, 25% increase in calls of help related to domestic violence in UK12. 10–27% increase in domestic violence at different parts of America was documented by Boserup in 202013.
An increase in reports and calls for help from victims of interpersonal violence have been reported by the specialized organizations worldwide during the COVID-19 pandemic. Increased incidence of IPV induced injuries illustrates the nature of isolated individuals with stagnation in life with a negative impact on the mental health of few individuals1. Interpersonal violence is a social, medical and legal problem that requires the combination of the same to address it. The COVID-19 pandemic also has an impact on the mental state and the healthcare professional can play a pivotal role to reduce the exacerbation of comorbid psychiatric disorders. It is well documented in the literature, children or adults witnessing or victimization have detrimental effect on mental and physical health. These witnesses within the family or victims of domestic violence can be associated with depression, anxiety, substance use. The impact of the pandemic still requires robust data that will help in reformulating the social policies which would minimize the overall effects.
5. Conclusion
The etiology and pattern of maxillofacial injuries reflect the trauma pattern within the community. We need more coordinated strategies of action to minimize maxillofacial injuries and its implication on physical and psychological wellbeing of patients. There were few limitations to the present study. A precise sub-classification of the etiology pertaining to maxillofacial injuries could be adopted.
The findings from the present study should alert the local authorities for enforcing stringent traffic laws and education of public vis-à-vis obeying traffic discipline to control excessive speed on highways and reckless driving. The better quality of roads as well as traffic engineering would significantly reduce the number of mishaps and evidently reduce injury to maxillofacial region. Drunken driving needs to be dealt with behavior refining laws as alcohol consumption plays a controversial role in maxillofacial trauma.
The study verified predominance of maxillofacial trauma among the young males irrespective of the pandemic. However, a shift towards assault related maxillofacial injuries due to domestic abuse especially during the ‘lockdown’ increased significantly. An Oral and Maxillofacial Surgeon needs to be prudent and vigilant while reporting the cases of IPV in the form of domestic abuse.
Declaration of patient consent
The study followed were in accordance with the ethical standards of the responsible committee and with Declaration of Helsinki. The authors certify that they have obtained all appropriate consent forms. In the form, the patients have given their consent for clinical information and images if any to be reported in the journal. The patients understand that their names and initials will be made to conceal identity.
Financial support and sponsorship
None.
Declaration of competing interest
None.
References
- 1.Prakash O., Prajapati V.K., Shahi A.K., Khaitan T. Incidence of maxillofacial trauma amid CoViD-19: a comparative study. J Maxillofacial Oral Surg. 2020 Nov 21:1–6. doi: 10.1007/s12663-020-01484-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Bokhamseen M., Al-Bodbaij M. Patterns of maxillofacial fractures in Hofuf, Saudi Arabia: a 10-year retrospective case series. Saudi Dental J. 2019 Jan 1;31(1):129–136. doi: 10.1016/j.sdentj.2018.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gandhi S., Ranganathan L.K., Solanki M., Mathew G.C., Singh I., Bither S. Pattern of maxillofacial fractures at a tertiary hospital in northern India: a 4‐year retrospective study of 718 patients. Dent Traumatol. 2011 Aug;27(4):257–262. doi: 10.1111/j.1600-9657.2011.00996.x. [DOI] [PubMed] [Google Scholar]
- 4.Malik S., Singh G., Kaur G., Yadav S., Mittal H.C. Orofacial trauma in rural India: a clinical study. Chin J Traumatol. 2017 Aug 1;20(4):216–221. doi: 10.1016/j.cjtee.2016.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee K.H., Snape L. Role of alcohol in maxillofacial fractures. N Z Med J. 2008 Apr 4;(1271):121. [PubMed] [Google Scholar]
- 6.Maffia F., Fontanari M., Vellone V., Cascone P., Mercuri L.G. Impact of COVID-19 on maxillofacial surgery practice: a worldwide survey. Int J Oral Maxillofac Surg. 2020 Jun 1;49(6):827–835. doi: 10.1016/j.ijom.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Olding J., Zisman S., Olding C., Fan K. Penetrating trauma during a global pandemic: changing patterns in interpersonal violence, self-harm and domestic violence in the Covid-19 outbreak. Surgeon. 2021 Feb 1;19(1):e9–13. doi: 10.1016/j.surge.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krishnaraj S., Chinnasamy R. A 4-year retrospective study of mandibular fractures in a South Indian City. J Craniofac Surg. 2007;18(4):776–780. doi: 10.1097/scs.0b013e318069005d. [DOI] [PubMed] [Google Scholar]
- 9.Barde D., Mudhol A., Madan R. Prevalence and pattern of mandibular fracture in Central India. Natl J Maxillofac Surg. 2014;5(2):153–156. doi: 10.4103/0975-5950.154818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kumar G.A., Dhupar V., Akkara F., Kumar S.P. Patterns of maxillofacial fractures in Goa. J Maxillofacial Oral Surg. 2015 Jun 1;14(2):138–141. doi: 10.1007/s12663-013-0583-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abhinav R.P., Selvarasu K., Gu Maheswari, Taltia A.A. The patterns and etiology of maxillofacial trauma in South India. Ann Maxillofacial Surg. 2019 Jan;9(1):114. doi: 10.4103/ams.ams_233_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sharma A., Borah S.B. Covid-19 and domestic violence: an indirect path to social and economic crisis. J Fam Violence. 2020 Jul 28:1–7. doi: 10.1007/s10896-020-00188-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boserup B., McKenney M., Elkbuli A. Alarming trends in US domestic violence during the COVID-19 pandemic. Am J Emerg Med. 2020;28(20):S0735–S6757. doi: 10.1016/j.ajem.2020.04.077. 30307–7. [DOI] [PMC free article] [PubMed] [Google Scholar]